Pediatric Reconstruction of Full-Thickness Dog Bite Scalp Avulsion with a Combination of Acellular and Matrix Products: A Case Report
Abstract
1. Introduction
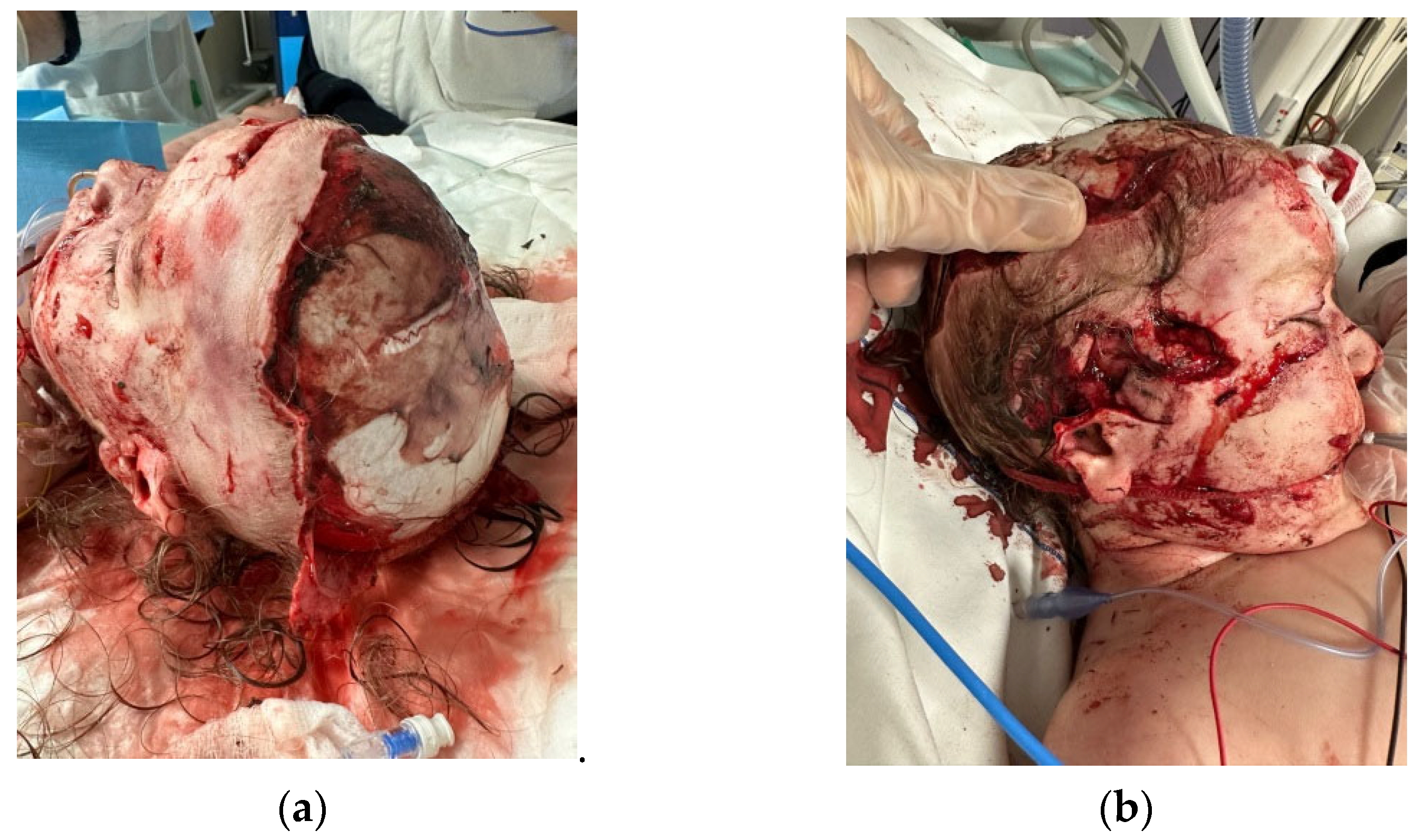
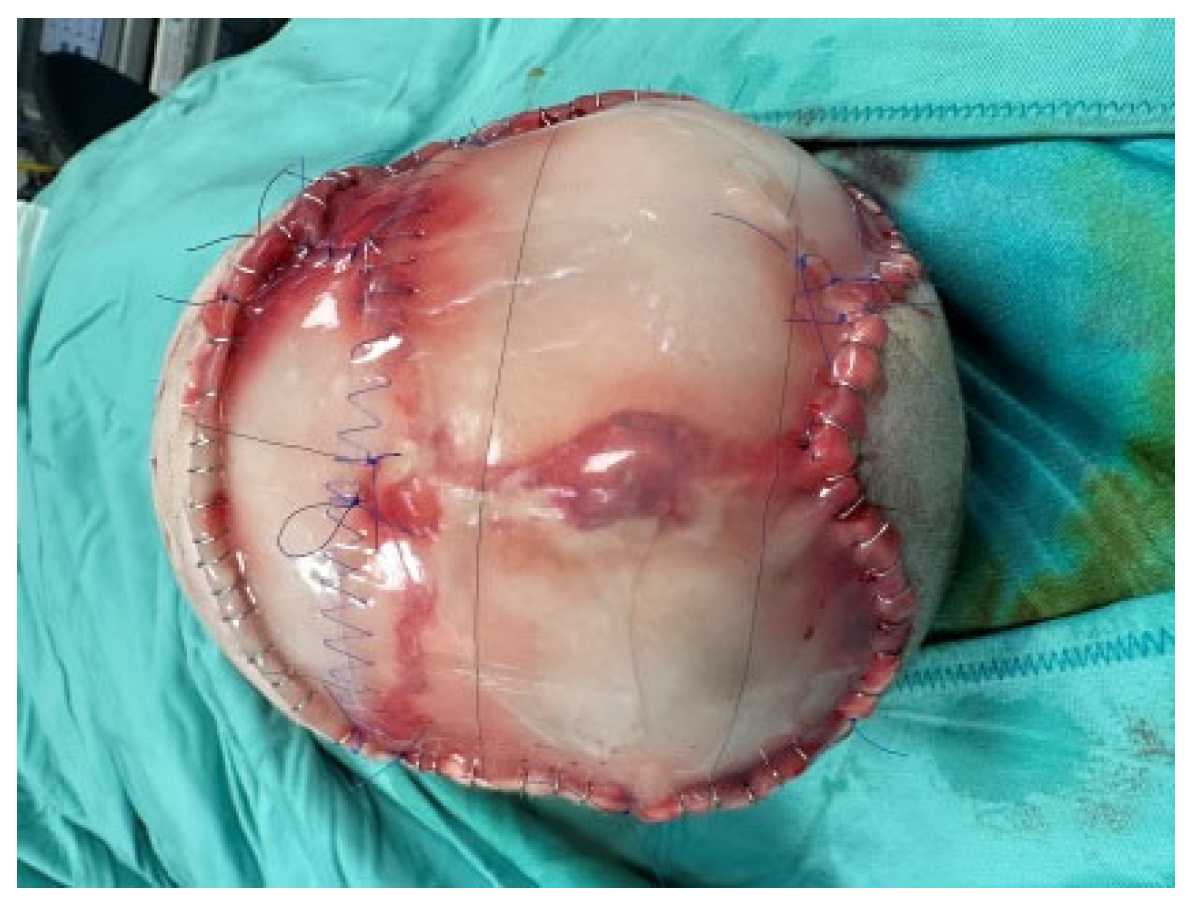
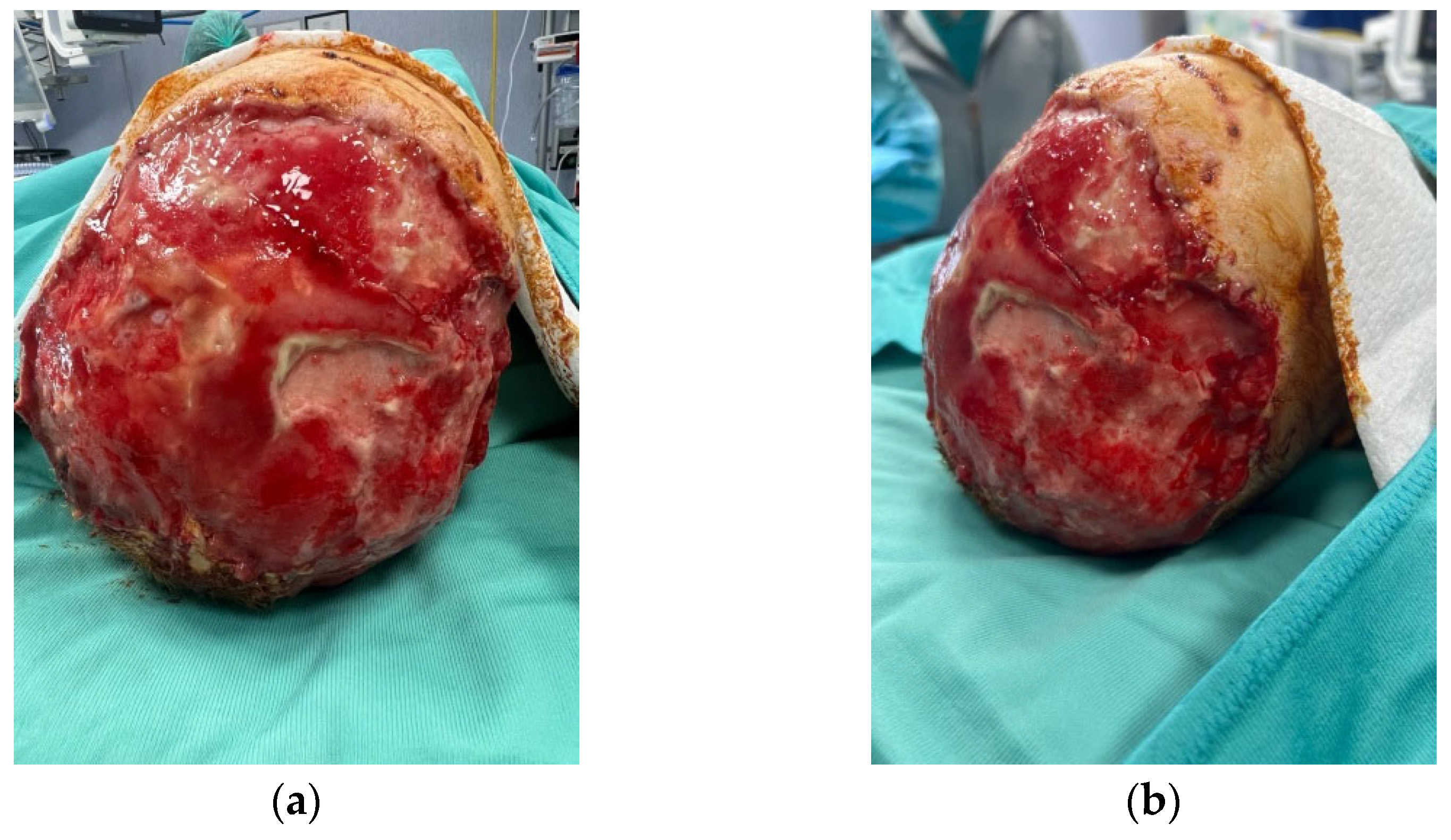
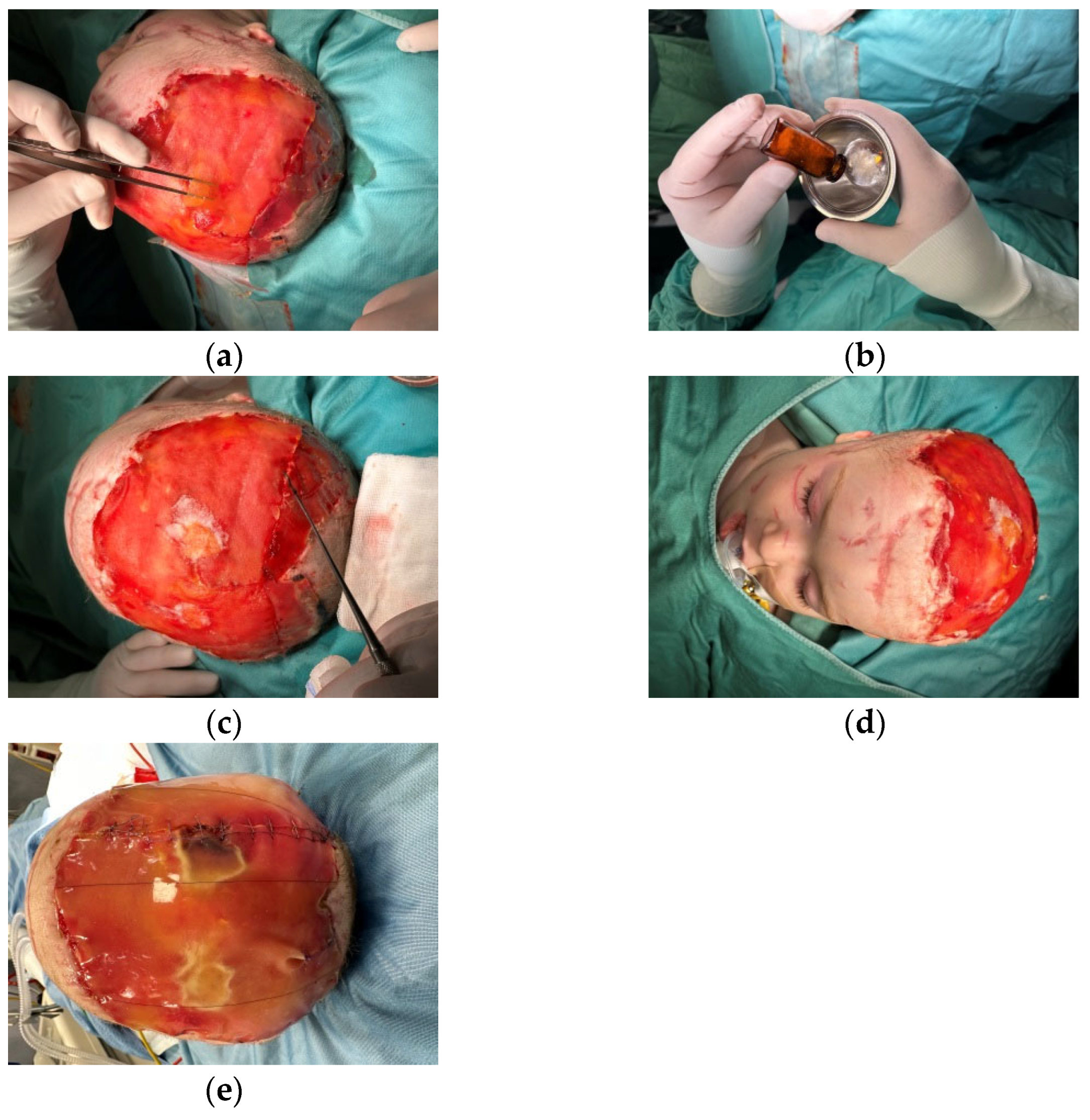
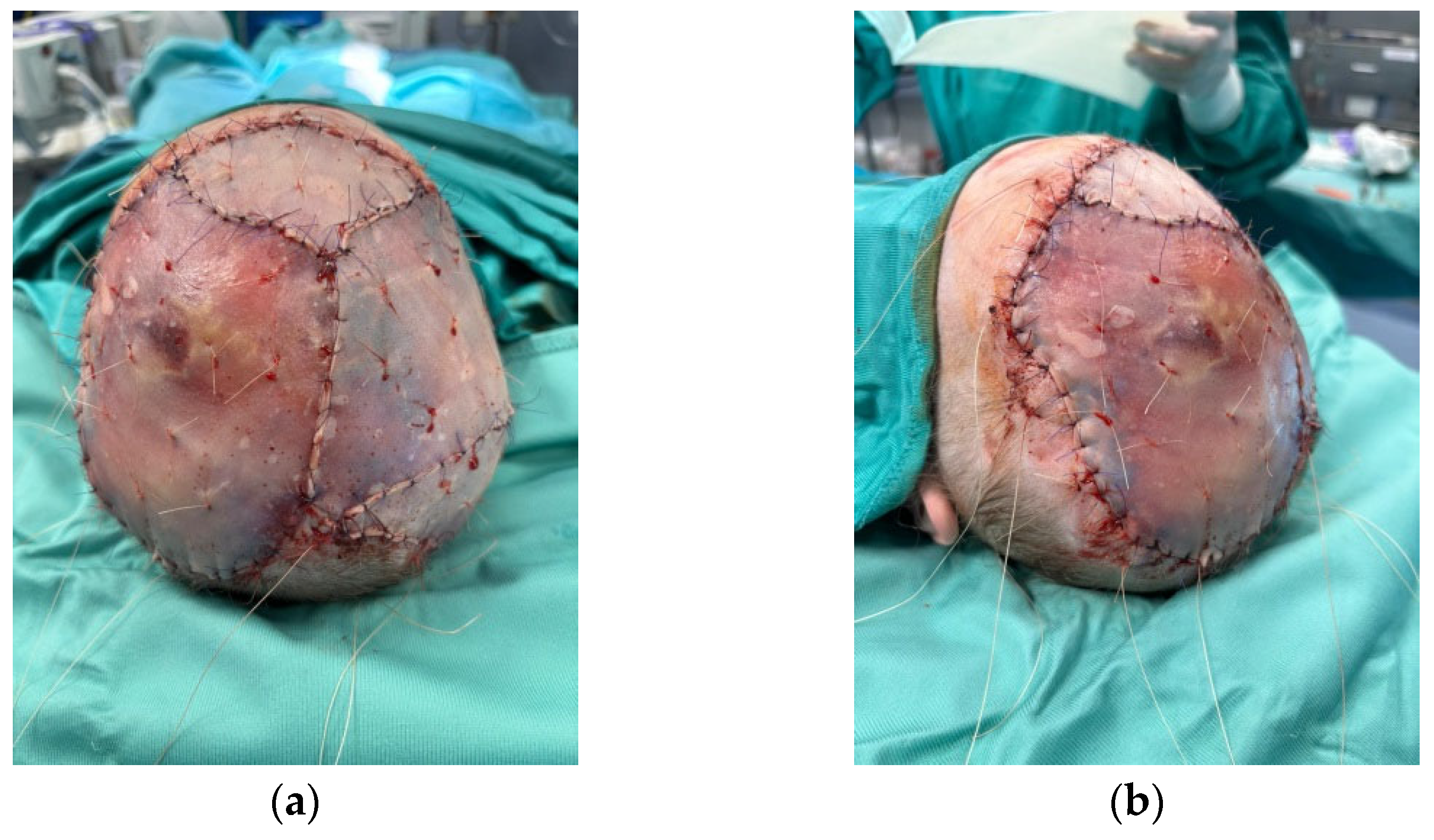
2. Clinical Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Bašković, M.; Pajić, A.; Barčot, Z. Massive Dog Bite Injury of the Scalp in One-year Old Boy. Prague Med. Rep. 2020, 121, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Konofaos, P.; Kashyap, A.; Wallace, R.D. Total Scalp Reconstruction Following a Dog Bite in a Pediatric Patient. J. Craniofac. Surg. 2014, 25, 1362–1364. [Google Scholar] [CrossRef] [PubMed]
- Macedo, J.L.S.; Rosa, S.C.; de Queiroz, M.N.; Gomes, T.G.A.C.B. Reconstruction of face and scalp after dog bites in children. Rev. Col. Bras. Cir. 2016, 43, 452–457. [Google Scholar] [CrossRef] [PubMed]
- McGuire, C.; Morzycki, A.; Simpson, A.; Williams, J.; Bezuhly, M. Dog bites in children: A descriptive analysis. Plast. Surg. 2018, 26, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Ng, Z.Y.; Eberlin, K.R.; Lin, T.; Masiakos, P.T.; Cetrulo, C.L., Jr. Reconstruction of Pediatric Scalp Avulsion Injuries After Dog Bites. J. Craniofac. Surg. 2017, 28, 1282–1285. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Walma, A.C.; Troulis, M.J.; August, M. Facial dog bites treated at the Massachusetts General Hospital over a 20-year period. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 130, 136–143. [Google Scholar] [CrossRef]
- Powell, M.S.M.; Osborn, T.; Mehta, S.T. Cultured Skin Autograft in Subtotal Pediatric Scalp Avulsion. Adv. Skin Wound Care 2023, 36, 1–6. [Google Scholar] [CrossRef]
- Anderson, S.R.; Gupta, N.B.; Johnson, R.M. Nonreplantable Total Scalp Avulsion Reconstruction with Acellular Biologic Matrix and Long-Term Outcome. J. Craniofac. Surg. 2022, 33, e445–e446. [Google Scholar] [CrossRef] [PubMed]
- Sofia, A.; Ellis, M.F. Hostile Scalp Wound Reconstruction Usingcellular Dermal Matrix for Soft Tissue Augmentation. J. Craniofac. Surg. 2020, 31, e309–e312. [Google Scholar]
- Patel, N.K.; Tipps, J.A.; Graham, E.M.; Taylor, J.A.; Mendenhall, S.D. Reconstruction of a near-total scalp avulsion with NovoSorb biodegradable temporizing matrix: Pediatric case report. Plast. Reconstr. Surg.–Glob. Open 2022, 10, e4717. [Google Scholar] [CrossRef] [PubMed]
- Amin, D.D.; Marwan, H.D.; Rowan, B.D.; Abramowicz, S.D.; Zaid, W.D. The Use of Urinary Bladder Matrix for Reconstructing Avulsed Traumatic Soft Tissue Injuries to the Maxillofacial Region. J. Craniofac. Surg. 2023, 34, 2317–2320. [Google Scholar] [CrossRef] [PubMed]
- Petrocelli, M.; Togo, G.; Ricci, S.; Zeneli, F.; Cutrupi, S.; Baietti, A.; Bonavolontà, P.; Califano, L.; Vaira, L.; Scarpa, A.; et al. Dermal Substitutes and Skin Grafts in the Reconstruction of Post-Traumatic Total Scalp Avulsion: A Case Series. J. Clin. Med. 2023, 12, 2167. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Li, F.; Yu, P.; Yu, C.; Han, C.; Wang, Y.; Yu, F.; Ye, L. Transcriptomic and cellular decoding of scaffolds-induced suture mesenchyme regeneration. Int. J. Oral Sci. 2024, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Othmana, A.; Lukowiakb, T.; Shakira, S.; Azourya, S.; Aizmanb, L.; Kliftoa, K.; Shinb, T.; Sobankob, J.; Millerb, C.; Etzkornb, J.; et al. Bilayer wound matrix-based cutaneous scalp reconstruction: A multidisciplinary case control analysis of factors associated with reconstructive success and failure. J. Plast. Reconstr. Aesthetic Surg. 2021, 74, 3008–3014. [Google Scholar] [CrossRef] [PubMed]
- Watts, V.; Attie, M.D.; McClure, S. Reconstruction of Complex Full-Thickness Scalp Defects After Dog-Bite Injuries Using Dermal Regeneration Template (Integra): Case Report and Literature Review. J. Oral Maxillofac. Surg. 2019, 77, 338–351. [Google Scholar] [CrossRef] [PubMed]
- Reece, M.; Walker, H.; Benintendi, I.; Ward, S.; Thatcher, A.; Johnson, M.; Kadakia, S. Delayed skin grafting protocol following IntegraTM application for non-radiated scalp reconstruction for decreased wound depth and improved contour. Head Neck 2023, 45, 2967–2974. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.; Atkin, L.; de Ceniga, M.V.; Weir, D.; Swanson, T.; Walker, A.; Mrozikiewicz-Rakowska, B.; Ciprandi, G.; Martínez, J.L.L.; Černohorská, J. Embedding Wound Hygiene into a proactive wound healing strategy. J. Wound Care 2022, 31, S1–S19. [Google Scholar] [CrossRef] [PubMed]
- Ciprandi, G.; Crucianelli, S.; Grussu, F.; Spuntarelli, G.; Marino, S.F.M.; Urbani, U.; Bernaschi, P.; Sisto, A.; Rizzo, M.I.; Zama, M. Meeting the Challenges in Pediatric Wound Care: Our 15-Year Experience with Dialkylcarbamoyl Chloride-Coated Dressing Technology in Acute and Chronic Wounds. Chronic Wound Care Manag. Res. 2022, 9, 23–33. [Google Scholar] [CrossRef]
- Komorowska-Timek, E.; Gabriel, A.; Bennett, D.C.; Miles, D.; Garberoglio, C.; Cheng, C.; Gupta, S. Artificial dermis as an alternative for coverage of complex scalp defects following excision of malignant tumors. Plast. Reconstr. Surg. 2005, 115, 1010–1017. [Google Scholar] [CrossRef] [PubMed]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grussu, F.; Ciprandi, G.; Lo Torto, F.; Ribuffo, D.; Zama, M. Pediatric Reconstruction of Full-Thickness Dog Bite Scalp Avulsion with a Combination of Acellular and Matrix Products: A Case Report. Medicina 2024, 60, 1838. https://doi.org/10.3390/medicina60111838
Grussu F, Ciprandi G, Lo Torto F, Ribuffo D, Zama M. Pediatric Reconstruction of Full-Thickness Dog Bite Scalp Avulsion with a Combination of Acellular and Matrix Products: A Case Report. Medicina. 2024; 60(11):1838. https://doi.org/10.3390/medicina60111838
Chicago/Turabian StyleGrussu, Francesca, Guido Ciprandi, Federico Lo Torto, Diego Ribuffo, and Mario Zama. 2024. "Pediatric Reconstruction of Full-Thickness Dog Bite Scalp Avulsion with a Combination of Acellular and Matrix Products: A Case Report" Medicina 60, no. 11: 1838. https://doi.org/10.3390/medicina60111838
APA StyleGrussu, F., Ciprandi, G., Lo Torto, F., Ribuffo, D., & Zama, M. (2024). Pediatric Reconstruction of Full-Thickness Dog Bite Scalp Avulsion with a Combination of Acellular and Matrix Products: A Case Report. Medicina, 60(11), 1838. https://doi.org/10.3390/medicina60111838






