A Comparative Analysis of Pain Assessment Methods in the Initial Postoperative Phase Following Different Pilonidal Cyst Surgeries
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
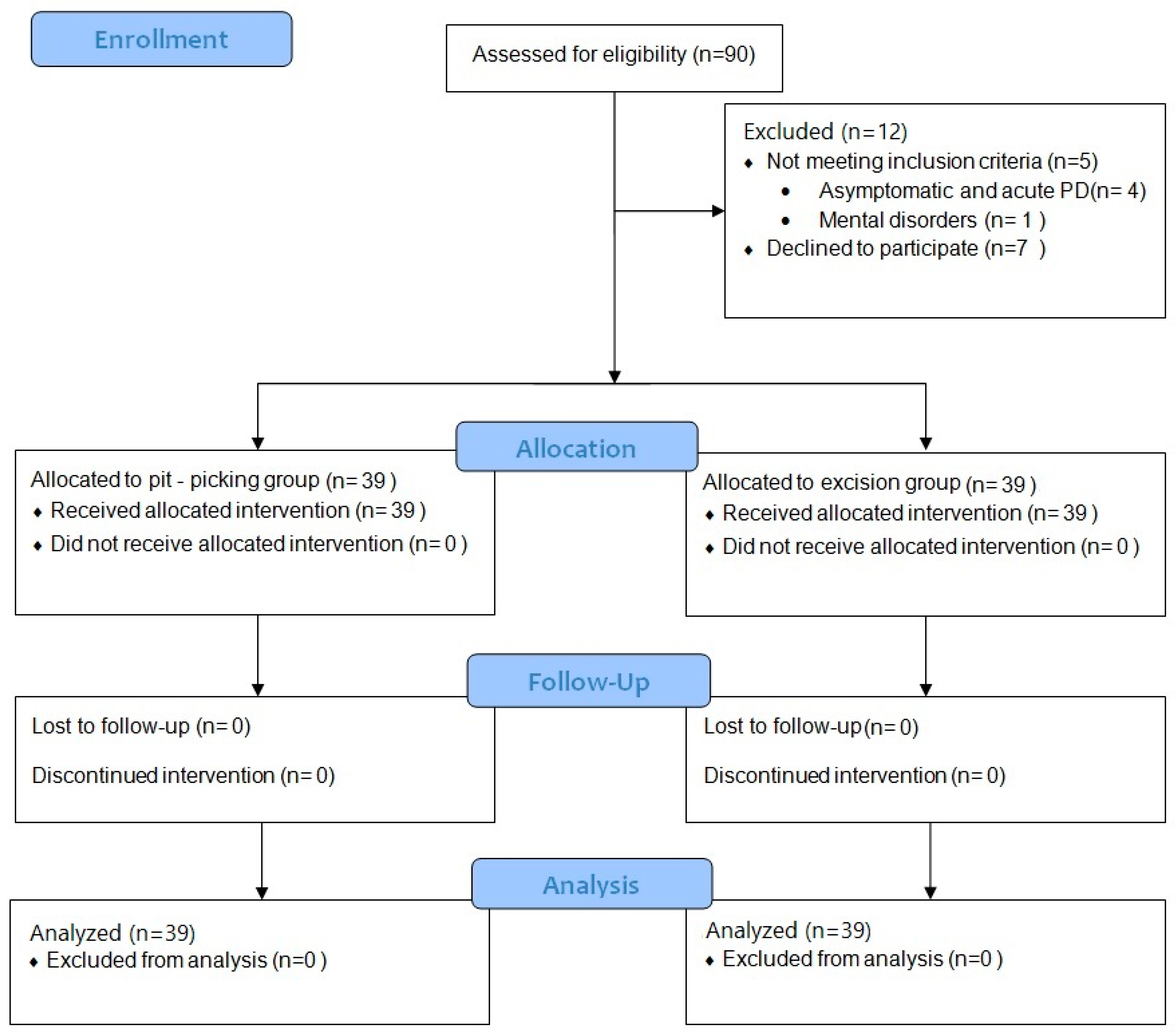
2.2. Participants
2.3. Sample Size
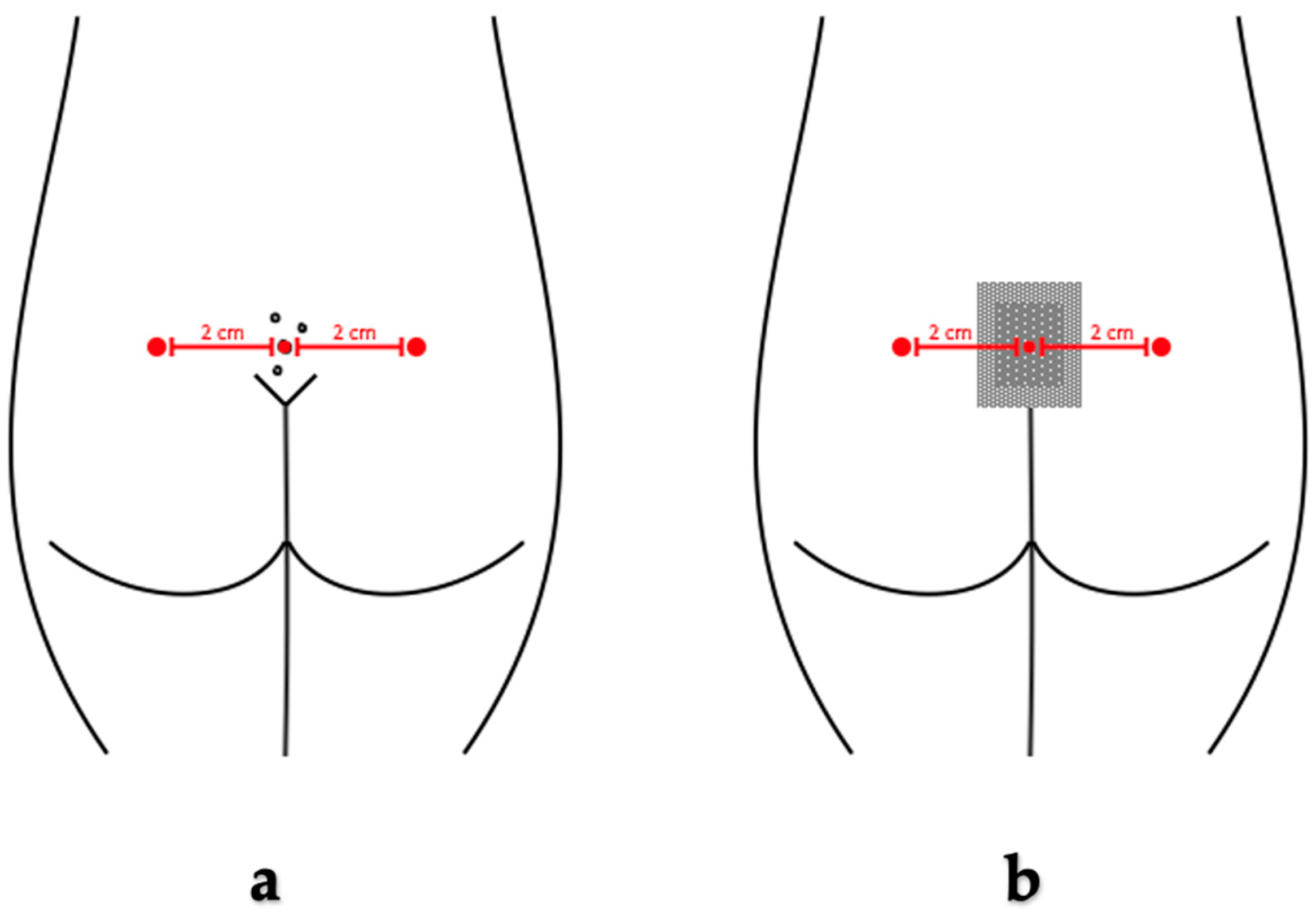
2.4. Surgical Procedures
2.5. Study Design
2.6. Pain Management
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients and Peculiarities of Pilonidal Disease
3.2. Pain Intensity Levels Measured by Visual Analogue Scale
3.3. Pain Intensity Levels Measured by Pressure Algometry
3.4. Correlation between VAS and Pressure Algometry
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The Revised IASP definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef] [PubMed]
- Begum, M.R.; Hossain, M.A. Validity and Reliability of Visual Analogue Scale (VAS) for Pain Measurement. J. Med. Case Rep. Rev. 2019, 2, 394–402. [Google Scholar]
- Reed, M.D.; van Nostran, W. Assessing pain intensity with the visual analog scale: A plea for uniformity. J. Clin. Pharmacol. 2014, 54, 241–244. [Google Scholar] [CrossRef] [PubMed]
- Breivik, H.; Borchgrevink, P.C.; Allen, S.M.; Rosseland, L.A.; Romundstad, L.; Breivik Hals, E.K.; Kvarstein, G.; Stubhaug, A. Assessment of pain. Br. J. Anaesth. 2008, 101, 17–24. [Google Scholar] [CrossRef]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of Digital Visual Analog Scale Pain Scoring with a Traditional Paper-based Visual Analog Scale in Adults. J. Am. Acad. Surg. Glob. Res. Rev. 2018, 2, e088. [Google Scholar] [CrossRef]
- Pelfort, X.; Torres-Claramunt, R.; Sánchez-Soler, J.F.; Hinarejos, P.; Leal-Blanquet, J.; Valverde, D.; Monllau, J.C. Pressure algometry is a useful tool to quantify pain in the medial part of the knee: An intra- and inter-reliability study in healthy subjects. Orthop. Traumatol. Surg. Res. 2015, 101, 559–563. [Google Scholar] [CrossRef]
- Więckiewicz, W.; Woźniak, K.; Piątkowska, D.; Szyszka-Sommerfeld, L.; Lipski, M. The Diagnostic Value of Pressure Algometry for Temporomandibular Disorders. BioMed Res. Int. 2015, 2015, 575038. [Google Scholar] [CrossRef]
- Alfonsin, M.M.; Chapon, R.; De Souza, C.A.B.; Genro, V.K.; Mattia, M.M.C.; Cunha-Filho, J.S. Correlations among algometry, the visual analogue scale, and the numeric rating scale to assess chronic pelvic pain in women. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2019, 3, 100037. [Google Scholar] [CrossRef]
- Sansone, P.; Caterina Pace, M.; Beatrice Passavanti, M.; Pota, V.; Colella, U.; Aurilio, C. Post-surgical pain. Epidemiology and Incidence of Acute and Chronic Post-Surgical Pain. Ann. Ital. Chir 2015, 86, 285–292. [Google Scholar]
- Mitra, S.; Carlyle, D.; Kodumudi, G.; Kodumudi, V.; Vadivelu, N. New Advances in Acute Postoperative Pain Management. Curr. Pain Headache Rep. 2018, 22, 35. [Google Scholar] [CrossRef]
- Beloeil, H.; Sulpice, L. Peri-operative pain and its consequences. J. Visc. Surg. 2016, 153, S15–S18. [Google Scholar] [CrossRef] [PubMed]
- Harries, R.L.; Alqallaf, A.; Torkington, J.; Harding, K.G. Management of sacrococcygeal pilonidal sinus disease. Int. Wound J. 2019, 16, 370–378. [Google Scholar] [CrossRef] [PubMed]
- De Parades, V.; Bouchard, D.; Janier, M.; Berger, A. Pilonidal sinus disease. J. Visc. Surg. 2013, 150, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Iesalnieks, I.; Ommer, A.; Herold, A.; Doll, D. German National Guideline on the management of pilonidal disease: Update 2020. Langenbeck’s Arch. Surg. 2021, 406, 2569–2580. [Google Scholar] [CrossRef]
- Al-Salamah, S.M.; Hussain, M.I.; Mahmood Mirza, S.; Al-Salamah, S.M. Excision with or without primary closure for Pilonidal sinus disease. Artic. J. Pak. Med. Assoc. 2007, 57, 388–391. [Google Scholar]
- Colov, E.P.; Bertelsen, C.A. Short convalescence and minimal pain after out-patient Bascom’s pit-pick operation. Dan. Med. Bull. 2011, 58, A4348. [Google Scholar]
- Ogilvie, J.W.; Ricciardi, R. Complications of Perineal Surgery. Clin. Colon Rectal Surg. 2009, 22, 51–59. [Google Scholar] [CrossRef][Green Version]
- Tazreean, R.; Nelson, G.; Twomey, R. Early mobilization in enhanced recovery after surgery pathways: Current evidence and recent advancements. J. Comp. Eff. Res. 2022, 11, 121–129. [Google Scholar] [CrossRef]
- Käser, S.A.; Zengaffinen, R.; Uhlmann, M.; Glaser, C.; Maurer, C.A. Primary wound closure with a Limberg flap vs. secondary wound healing after excision of a pilonidal sinus: A multicentre randomised controlled study. Int. J. Color. Dis. 2014, 30, 97–103. [Google Scholar] [CrossRef]
- Ehrl, D.; Choplain, C.; Heidekrueger, P.; Erne, H.C.; Rau, H.-G.; Niclas Broer, P. Treatment Options for Pilonidal Disease. Am. Surg. 2017, 83, 453–457. [Google Scholar] [CrossRef]
- Mohamed, H.A.; Kadry, I.; Adly, S. Comparison between three therapeutic modalities for non-complicated pilonidal sinus disease. Surgeon 2005, 3, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Dainius, E.; Vaiciute, M.K.; Parseliunas, A.; Latkauskas, T.; Venskutonis, D. Surgical treatment of pilonidal disease-Short-term follow up results of minimally invasive pit-picking surgery versus radical excision without suturing: A prospective randomised trial. Heliyon 2024, 10, e31497. [Google Scholar] [CrossRef] [PubMed]
- Stewart, A.; Donoghue, J.; Mitten-Lewis, S. Pilonidal sinus: Healing rates, pain and embarrassment levels. J. Wound Care 2013, 17, 468–474. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Brennan, T.J. Mechanisms of postoperative pain. Anesth. Pain Med. 2016, 11, 236–248. [Google Scholar] [CrossRef]
- Sterling, M. Pressure Algometry: What Does It Really Tell Us? J. Orthop. Sports Phys. Ther. 2011, 41, 623–624. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, K. Abdominal examination using pressure pain threshold algometer reflecting clinical characteristics of complementary and alternative medicine in Korea: A systematic review and a brief proposal. Medicine 2022, 101, E31417. [Google Scholar] [CrossRef]
- Parseliunas, A.; Paskauskas, S.; Kubiliute, E.; Vaitekunas, J.; Venskutonis, D. Transcutaneous Electric Nerve Stimulation Reduces Acute Postoperative Pain and Analgesic Use after Open Inguinal Hernia Surgery: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Pain 2021, 22, 533–544. [Google Scholar] [CrossRef]
| Baseline Characteristic Item | Excision Group (N = 39) | Pit-Picking Group (N = 39) | p Value |
|---|---|---|---|
| Male sex, n (%) | 33 (84.6%) | 35 (89.7%) | 0.46 |
| Age * | 26 (26.44–32.13) | 26 (26.46–33.28) | 0.83 |
| BMI * | 26.47 (25.87–29.82) | 27.31 (26.19–28.71) | 0.43 |
| Smoking, n (%) | 18 (46.2%) | 23 (59.0%) | 0.28 |
| Duration of symptoms, months * | 6 (9.38–25.59) | 12 (11.20–24.69) | 0.56 |
| ASA class, n (%) | I—33 (84.6%) II—6 (15.4%) | I—36 (92.3%) II—3 (7.7%) | 0.28 |
| Primary PD, n (%) | 29 (74.4%) | 32 (82.1%) | 0.41 |
| Size of PD—cm * | 5.5 (4.65–6.24) | 5.2 (4.97–6.83) | 0.46 |
| Count of grown follicles * | 3 (2.25–3.13) | 3 (2.58–3.79) | 0.29 |
| Fistula n (%) | 28 (71.8%) | 24 (61.5%) | 0.23 |
| Excision Group (N = 39) | Pit-Picking Group (N = 39) | p Value | |
|---|---|---|---|
| VAS before surgery * | 2 (4.72–11.84) | 4 (5.45–15.01) | 0.29 |
| VAS during anesthesia * | 40 (37.3–48.4) | 35 (27.8–40.4) | 0.06 |
| VAS I day after surgery * | 13 (14.36–28.46) | 15 (15.02–27.23) | 0.62 |
| Excision Group (N = 39) * | Pit-Picking Group (N = 39) * | p Value | |
|---|---|---|---|
| PPT right before surgery (kg/cm2) | 3.17 ± 1.33 | 3.38 ± 1.21 | 0.46 |
| MTPP right before surgery (kg/cm2) | 4.45 ± 1.26 | 4.74 ± 1.30 | 0.32 |
| IPPT right before surgery (kg/cm2) | 1.26 ± 0.68 | 1.41 ± 0.70 | 0.34 |
| PPT left before surgery (kg/cm2) | 2.94 ± 1.22 | 2.94 ± 1.22 | 0.98 |
| MTPP left before surgery (kg/cm2) | 4.19 ± 1.20 | 4.28 ± 1.22 | 0.76 |
| IPPT left before surgery (kg/cm2) | 1.32 ± 0.78 | 1.43 ± 0.92 | 0.57 |
| PPT center before surgery (kg/cm2) | 2.08 ± 1.15 | 2.07 ± 1.02 | 0.96 |
| MTPP center before surgery (kg/cm2) | 3.01 ± 1.35 | 3.00 ± 1.28 | 0.98 |
| IPPT center before surgery (kg/cm2) | 0.91 ± 0.57 | 0.93 ± 0.57 | 0.86 |
| Excision Group (N = 39) * | Pit-Picking Group (N = 39) * | p Value | |
|---|---|---|---|
| PPT right I day after surgery (kg/cm2) | 1.99 ± 1.06 | 2.23 ± 1.02 | 0.31 |
| MTPP right I day after surgery (kg/cm2) | 3.23 ± 1.34 | 3.49 ± 1.23 | 0.39 |
| IPPT right I day after surgery (kg/cm2) | 1.29 ± 0.71 | 1.24 ± 0.62 | 0.91 |
| PPT left I day after surgery (kg/cm2) | 2.05 ± 1.46 | 1.42 ± 0.73 | 0.02 |
| MTPP left I day after surgery (kg/cm2) | 2.91 ± 1.33 | 2.32 ± 1.14 | 0.04 |
| IPPT left I day after surgery (kg/cm2) | 0.86 ± 1.31 | 0.90 ± 0.66 | 0.83 |
| PPT center I day after surgery (kg/cm2) | 1.50 ± 0.67 | 1.32 ± 0.68 | 0.23 |
| MTPP center I day after surgery (kg/cm2) | 2.51 ± 1.07 | 1.91 ± 0.91 | 0.01 |
| IPPT center I day after surgery (kg/cm2) | 0.98 ± 0.62 | 0.59 ± 0.39 | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dainius, E.; Garnyte, J.; Juskeviciute, E.; Parseliunas, A.; Latkauskas, T.; Burzinskiene, G.; Venskutonis, D.; Tamelis, A. A Comparative Analysis of Pain Assessment Methods in the Initial Postoperative Phase Following Different Pilonidal Cyst Surgeries. Medicina 2024, 60, 1710. https://doi.org/10.3390/medicina60101710
Dainius E, Garnyte J, Juskeviciute E, Parseliunas A, Latkauskas T, Burzinskiene G, Venskutonis D, Tamelis A. A Comparative Analysis of Pain Assessment Methods in the Initial Postoperative Phase Following Different Pilonidal Cyst Surgeries. Medicina. 2024; 60(10):1710. https://doi.org/10.3390/medicina60101710
Chicago/Turabian StyleDainius, Edvinas, Julija Garnyte, Egle Juskeviciute, Audrius Parseliunas, Tadas Latkauskas, Guoda Burzinskiene, Donatas Venskutonis, and Algimantas Tamelis. 2024. "A Comparative Analysis of Pain Assessment Methods in the Initial Postoperative Phase Following Different Pilonidal Cyst Surgeries" Medicina 60, no. 10: 1710. https://doi.org/10.3390/medicina60101710
APA StyleDainius, E., Garnyte, J., Juskeviciute, E., Parseliunas, A., Latkauskas, T., Burzinskiene, G., Venskutonis, D., & Tamelis, A. (2024). A Comparative Analysis of Pain Assessment Methods in the Initial Postoperative Phase Following Different Pilonidal Cyst Surgeries. Medicina, 60(10), 1710. https://doi.org/10.3390/medicina60101710






