Analysis of Complications of a Neglected Disease: 13 Years of Experience with Liver Hydatid Cysts in a High-Volume Hospital
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Groups
2.2. Ethical Approval
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Definition of the Grade of CE
2.6. Clinical Monitoring
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mirabile, E.; Solomon, N.; Fields, P.J.; Macpherson, C.N.L. Progress towards international adoption of the World Health Organization ultrasound classification of cystic echinococcosis. Acta Trop. 2019, 189, 6–9. [Google Scholar] [CrossRef]
- Agudelo Higuita, N.I.; Brunetti, E.; McCloskey, C. Cystic Echinococcosis. J. Clin. Microbiol. 2016, 54, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Giorgio, A.; Di Sarno, A.; de Stefano, G.; Farella, N.; Matteucci, P.; Scognamiglio, U.; Giorgio, V. Percutaneous treatment of Hydatid Liver Cyst. Recent Pat. Anti-Infect. Drug Discov. 2009, 4, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Stojkovic, M.; Junghanss, T. Cystic and alveolar echinococcosis. Handb. Clin. Neurol. 2013, 114, 327–334. [Google Scholar]
- McManus, D.P.; Zhang, W.; Li, J.; Bartley, P.B. Echinococcosis. Lancet Lond. Engl. 2003, 362, 1295–1304. [Google Scholar] [CrossRef]
- Yilmaz, L.; Bulut, A.; Aytekin, A.; Baskonus, I.; Yildiz, F.; Coban, S.; Balik, A.A. A Novel Technique for the Management of Persistent Biliary Fistulas Developing After Liver Hydatid Cyst Surgeries: Drain Clamping Technique. Dig. Dis. Sci. 2024, 69, 961–968. [Google Scholar] [CrossRef]
- Orue-Echebarria, M.I.; Vaquero, J.; Vara, E.; Rancan, L.; Lozano, P.; Lisbona, C.J.; Laso, J.; Fernández-Mena, C.; Olmedilla, L.; Peligros, I.; et al. Mechanisms of regenerative preconditioning in pigs with subtotal hepatectomies. Cir. Cir. 2022, 90, 61–69. [Google Scholar]
- Martínez-Mier, G.; Esquivel-Torres, S.; Alvarado-Arenas, R.; Moreno-Ley, P.I.; Lajud-Barquin, F.A. Application and validation of a surgical risk calculator in a liver surgery cohort of patients in Veracruz, Mexico. Cir. Cir. 2022, 90, 359–364. [Google Scholar] [CrossRef]
- Atay, G.; Erdogan, S.; Tugrul, H.C.; Dur, S.M.S. Anaphylaxis during puncture of a hepatic hydatid cyst. North. Clin. Istanb. 2023, 10, 813–815. [Google Scholar] [CrossRef]
- Dehkordi, A.B.; Sanei, B.; Yousefi, M.; Sharafi, S.M.; Safarnezhad, F.; Jafari, R.; Darani, H.Y. Albendazole and Treatment of Hydatid Cyst: Review of the Literature. Infect. Disord. Drug Targets 2019, 19, 101–104. [Google Scholar] [CrossRef]
- Ran, B.; Shao, Y.; Yimiti, Y.; Aji, T.; Jiang, T.; Cheng, L.; Li, W.; Zhang, W.; Wen, H. Surgical Procedure Choice for Removing Hepatic Cysts of Echinococcus granulosus in Children. Eur. J. Pediatr. Surg. Off. J. Austrian Assoc. Pediatr. Surg. Z. Kinderchir. 2016, 26, 363–367. [Google Scholar] [CrossRef]
- McManus, D.P.; Gray, D.J.; Zhang, W.; Yang, Y. Diagnosis, treatment, and management of echinococcosis. BMJ 2012, 344, e3866. [Google Scholar] [CrossRef] [PubMed]
- Halezeroglu, S.; Okur, E.; Tanyü, M.O. Surgical management for hydatid disease. Thorac. Surg. Clin. 2012, 22, 375–385. [Google Scholar] [CrossRef] [PubMed]
- Sen, P.; Demirdal, T.; Nemli, S.A. Evaluation of clinical, diagnostic and treatment aspects in hydatid disease: Analysis of an 8-year experience. Afr. Health Sci. 2019, 19, 2431–2438. [Google Scholar] [CrossRef] [PubMed]
- García-Redondo, M.; González Sánchez, D.; Cabañó-Muñoz, D.; del Mar Rico-Morales, M.; Rodriguez-Perdomo, M.; Lopez-Fernandez, J.; Torres-Melero, J.; Reina-Duarte, A. Management of a hydatid cyst in a center with high prevalence. Descriptive series. Rev. Esp. Enferm. Dig. 2023, 115, 747–748. [Google Scholar]
- WHO Informal Working Group. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003, 85, 253–261. [Google Scholar] [CrossRef]
- Brunetti, E.; Kern, P.; Vuitton, D.A.; Writing Panel for the WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010, 114, 1–16. [Google Scholar] [CrossRef]
- Oral, A.; Yigiter, M.; Yildiz, A.; Yalcin, O.; Dikmen, T.; Eren, S.; Kantarci, M.; Salman, A.B. Diagnosis and management of hydatid liver disease in children: A report of 156 patients with hydatid disease. J. Pediatr. Surg. 2012, 47, 528–534. [Google Scholar] [CrossRef]
- Mihetiu, A.; Bratu, D.; Sabau, D.; Nastase, O.; Sandu, A.; Tanasescu, C.; Boicean, A.; Ichim, C.; Todor, S.B.; Serban, D.; et al. Optimized Strategies for Managing Abdominal Hydatid Cysts and Their Complications. Diagnostics 2024, 14, 1346. [Google Scholar] [CrossRef]
- Öztorun, C.İ.; Demir, S.; Güney, D.; Ertürk, A.; Ilıkan, G.B.; Karabulut, B.; Azılı, M.N.; Şenel, E. An unsolved problem in developing countries: Hydatid cysts in children. Pediatr. Surg. Int. 2021, 37, 1235–1241. [Google Scholar] [CrossRef]
- Sheves, A.; Fuxman, Y.; Gazer, B.; Shmueli, M.; Van Buren, J.; Ben-Shimol, S.; Assi, Z. Treatment of Cystic Echinococcosis in Children: A Single Center Experience. Pediatr. Infect. Dis. J. 2023, 42, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Mandal, K.C.; Halder, P.; Mondal, G.; Debnath, B.; Mitra, D.; Mukhopadhyay, B. Atypical presentations of hydatid cyst in children and their management. Indian J. Gastroenterol. Off. J. Indian Soc. Gastroenterol. 2022, 41, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, H.; Öztürk, H.; Otçu, S.; Önen, A.; Duran, H. Çocuklarda hidatik hastalık: 49 olgunun analizi. Turk. J. Surg. 2006, 22, 017–020. [Google Scholar]
- Pradhan, A.; Mallick, B.; Dash, A.; Nanda, D. Clinical presentation and outcome of children with hydatid disease: A retrospective cross-sectional study from a tertiary care hospital in eastern India. J. Parasit. Dis. Off. Organ. Indian. Soc. Parasitol. 2022, 46, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Tüz, A.E.; Ekemen Keleş, Y.; Şahin, A.; Üstündağ, G.; Taşar, S.; Öncel, E.K.; Aksay, A.K.; Öztan, M.O.; Köylüoğlu, G.; Çapar, A.E.; et al. Hydatid Disease in Children from Diagnosis to Treatment: A 10-year Single Center Experience. Turk. Parazitolojii Derg. 2022, 46, 189–194. [Google Scholar] [CrossRef]
- Masood, P.F.; Mufti, G.N.; Wani, S.A.; Sheikh, K.; Baba, A.A.; Bhat, N.A.; Hamid, R. Comparison of laparoscopic and open surgery in hepatic hydatid disease in children: Feasibility, efficacy and safety. J. Minimal Access Surg. 2022, 18, 360–365. [Google Scholar] [CrossRef]
- Aygun, D.; Yıldırım, T.; Öner, Ö.; Kuzdan, Ö.; Özaydın, S.; Erbaş, M.; Şiraneci, R. Hydatid Disease in Childhood: A Single Center Experience. J. Pediatr. Infect. 2020, 14, 80–86. [Google Scholar] [CrossRef]
- Tural Kara, T.; Ozdemir, H.; Karbuz, A.; Yahşi, A.; Erat, T.; Bingöl-Koloğlu, M.; Fitöz, S.; Tutar, E.; Çiftçi, E.; Ince, E. Clinical characteristics of childhood hydatid disease: A single tertiary centre experience from Turkey. Hong Kong J. Paediatr. 2018, 23, 162–168. [Google Scholar]
- Czermak, B.V.; Akhan, O.; Hiemetzberger, R.; Zelger, B.; Vogel, W.; Jaschke, W.; Rieger, M.; Kim, S.Y.; Lim, J.H. Echinococcosis of the liver. Abdom. Imaging 2008, 33, 133–143. [Google Scholar] [CrossRef]
- Khan, A.; Ahmed, H.; Khan, H.; Saleem, S.; Simsek, S.; Brunetti, E.; Afzal, M.S.; Manciulli, T.; Budke, C.M. Cystic Echinococcosis in Pakistan: A Review of Reported Cases, Diagnosis, and Management. Acta Trop. 2020, 212, 105709. [Google Scholar] [CrossRef]
- Kaman, A.; Tanır, G.; Çakmakçı, E.; Demir, P.; Öz, F.N.; Teke, T.A.; Metin, Ö.; Gayretli-Aydın, Z.G.; Karaman, A. Characteristics, diagnosis, and treatment modality of pediatric patients with cystic echinococcosis: A single centre experience. Turk. J. Pediatr. 2019, 61, 704–713. [Google Scholar] [CrossRef] [PubMed]
- Yücesan, B.; Babür, C.; Kılıç, S.; Dikmen, A.U. Evaluation of Echinococcosis Pre-Diagnosis Patients Admitted to the National Parasitology Reference Laboratory of Turkey from 2014–2019. Iran. J. Parasitol. 2022, 17, 250–258. [Google Scholar] [CrossRef]
- Karabulut, B.; Bayram, G.; Azılı, M.N.; Özcan, F.; Şenaylı, A.; Akbıyık, F.; Mambet, E.; Şenel, E.; Livanelioğlu Yz Tiryaki, T. Karaciğer Kist Hidatiğinin Cerrahi ve Perkütan Tedavi Sonuçlarının Karşılaştırılması. J. Pediatr. Dis. 2014, 8, 141–145. [Google Scholar]

| WHO-IWGE | Definition | Gharbi | Stage | n (%) |
|---|---|---|---|---|
| CE1 | Unilocular unechoic cystic lesion with double line sign | I | Active | 99 (46%) |
| CE2 | Multiseptated, rosette-like, honeycomb cyst | III | Active | 23 (11%) |
| CE3A | Cyst with detached membranes (water-lily-sign) | II | Transitional | 32 (15%) |
| CE3B | Cyst with daughter cysts in solid matrix | III | Transitional | 26 (12%) |
| CE4 | Cyst with heterogenous hypoechoic/hyperechoic contents. No daughter cysts | IV | Inactive | 24 (11%) |
| CE5 | =CE4 plus calcified wall | V | Inactive | 10 (5%) |
| Cyst Localization | n | % |
|---|---|---|
| Isolated Liver | 184 | 86% |
| Liver + Lung | 20 | 9.3% |
| Right | 14 | |
| Left | 4 | |
| Bilateral | 2 | |
| Liver + Spleen | 5 | 2.3% |
| Liver + Intraabdominal | 2 | 0.9% |
| Liver + Kidney | 1 | 0.5% |
| Liver + Rectus Muscle | 1 | 0.5% |
| Liver + Kidney + Brain | 1 | 0.5% |
| Total | 214 | 100% |
| n | % * | % ^ | |
|---|---|---|---|
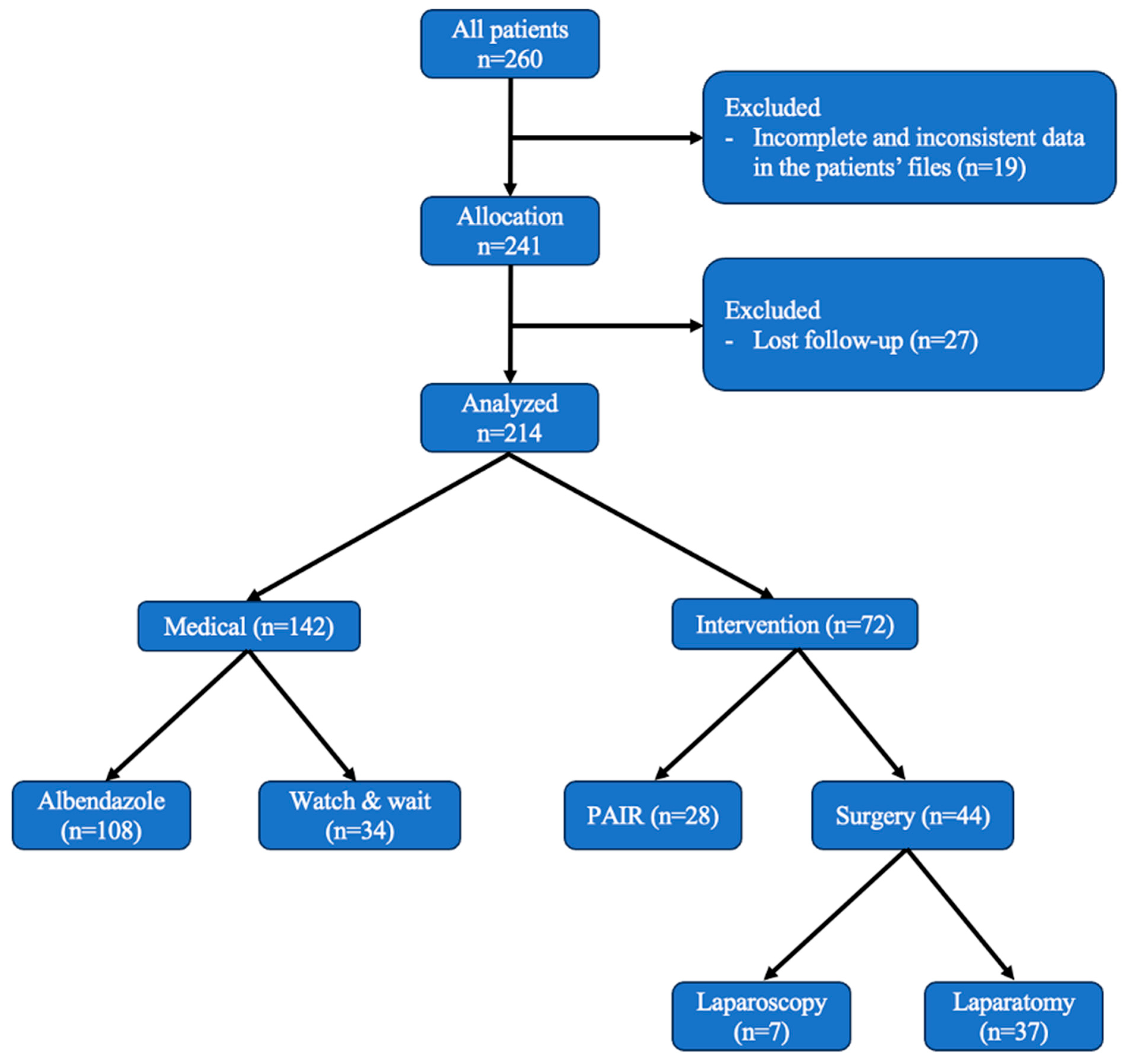
| Non-operative | 142 | 66% | 100% |
| Medical treatment (Albendazole) | 108 | 50% | 76% |
| Observation without treatment | 34 | 16% | 24% |
| Operative (+Albendazole) | 72 | 34% | 100% |
| PAIR | 28 | 13% | 39% |
| Surgery | 44 | 21% | 61% |
| Laparoscopy | 7 | 16% | |
| Laparotomy | 37 | 84% | |
| Conversion to laparotomy | 1 |
| * (μ ± σ), # (n, %) | Group 1 (n = 142) | Group 2 (n = 72) | Total (n = 214) | p | ||||
|---|---|---|---|---|---|---|---|---|
| Demographics | Age (year) * | 10.8 ± 3.8 | 12.03 ± 3.53 | 11.05 ± 3.83 | >0.05 | |||
| Gender # | >0.05 | |||||||
| Female | 80 | 56% | 42 | 58% | 122 | 56% | ||
| Male | 62 | 44% | 30 | 42% | 92 | 44% | ||
| Laboratory results | Eosinophil (1 × 103/uL) * | 1.27 ± 0.93 | 1.28 ± 0.89 | 1.27 ± 0.93 | >0.05 | |||
| Bilirubin (mg/dL) * | 0.35 ± 0.21 | 0.37 ± 0.21 | 0.35 ± 0.21 | >0.05 | ||||
| Amylase (U/L) * | 72.22 ± 29.65 | 76.35 ± 33.34 | 73.24 ± 31.13 | >0.05 | ||||
| ALT (U/L) * | 34.47 ± 29.81 | 40.31 ± 32.65 | 36.65 ± 31.57 | >0.05 | ||||
| AST (U/L) * | 44.86 ± 36.33 | 45.12 ± 37.98 | 44.97 ± 37.12 | >0.05 | ||||
| GGT (U/L) * | 56.88 ± 32.37 | 58.36 ± 33.03 | 57.13 ± 32.94 | >0.05 | ||||
| Feature of the cysts | Localization # | >0.05 | ||||||
| Right lobe | 95 | 67% | 48 | 66% | 143 | 67% | ||
| Left lobe | 30 | 21% | 15 | 21% | 45 | 21% | ||
| Bilateral | 17 | 12% | 9 | 13% | 26 | 12% | ||
| Organ Involvement # | >0.05 | |||||||
| Isolated in liver | 119 | 84% | 65 | 90% | 184 | 86% | ||
| Multiple organs | 23 | 16% | 7 | 10% | 30 | 14% | ||
| Number of Cysts # | >0.05 | |||||||
| Single | 95 | 67% | 50 | 69% | 145 | 68% | ||
| Multiple | 47 | 33% | 22 | 31% | 69 | 32% | ||
| Cyst Diameter # | 0.000 | |||||||
| <5 cm | 72 | 51% | 0 | 0% | 72 | 34% | ||
| 5–10 cm | 64 | 45% | 33 | 46% | 97 | 45% | ||
| >10 cm | 6 | 4% | 39 | 54% | 45 | 21% | ||
| Cyst diameter (mm) * | 60.1 ± 30.8 | 100 ± 30.5 | 66.9 ± 34.2 | 0.000 | ||||
| Cyst Rupture # | >0.05 | |||||||
| No | 135 | 95% | 66 | 92% | 201 | 94% | ||
| Yes | 7 | 5% | 6 | 8% | 13 | 6% | ||
| Recurrence # | >0.05 | |||||||
| No | 140 | 99% | 70 | 97% | 210 | 98% | ||
| Yes | 2 | 1% | 2 | 3% | 4 | 2% | ||
| Complications | n | % |
|---|---|---|
| Anaphylaxis | 1 | 2% |
| Cysto-biliary fistula | 8 | 11% |
| Need for ERCP | 2 | 3% |
| Nasobiliary catheter insertion | 1 | 2% |
| Clavien–Dindo classification (≥3) | 4 | 6% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azizoğlu, M.; Aydogdu, B.; Kamci, T.O.; Arslan, S.; Basuguy, E.; Bilici, S.; Okur, M.H. Analysis of Complications of a Neglected Disease: 13 Years of Experience with Liver Hydatid Cysts in a High-Volume Hospital. Medicina 2024, 60, 1696. https://doi.org/10.3390/medicina60101696
Azizoğlu M, Aydogdu B, Kamci TO, Arslan S, Basuguy E, Bilici S, Okur MH. Analysis of Complications of a Neglected Disease: 13 Years of Experience with Liver Hydatid Cysts in a High-Volume Hospital. Medicina. 2024; 60(10):1696. https://doi.org/10.3390/medicina60101696
Chicago/Turabian StyleAzizoğlu, Mustafa, Bahattin Aydogdu, Tahsin Onat Kamci, Serkan Arslan, Erol Basuguy, Salim Bilici, and Mehmet Hanifi Okur. 2024. "Analysis of Complications of a Neglected Disease: 13 Years of Experience with Liver Hydatid Cysts in a High-Volume Hospital" Medicina 60, no. 10: 1696. https://doi.org/10.3390/medicina60101696
APA StyleAzizoğlu, M., Aydogdu, B., Kamci, T. O., Arslan, S., Basuguy, E., Bilici, S., & Okur, M. H. (2024). Analysis of Complications of a Neglected Disease: 13 Years of Experience with Liver Hydatid Cysts in a High-Volume Hospital. Medicina, 60(10), 1696. https://doi.org/10.3390/medicina60101696





