Knowledge, Attitudes and Practices Survey of Recombinant Zoster Vaccine among Cardiologists and Cardiac Nurses in Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Survey Instrument
2.3. Statistical Analysis
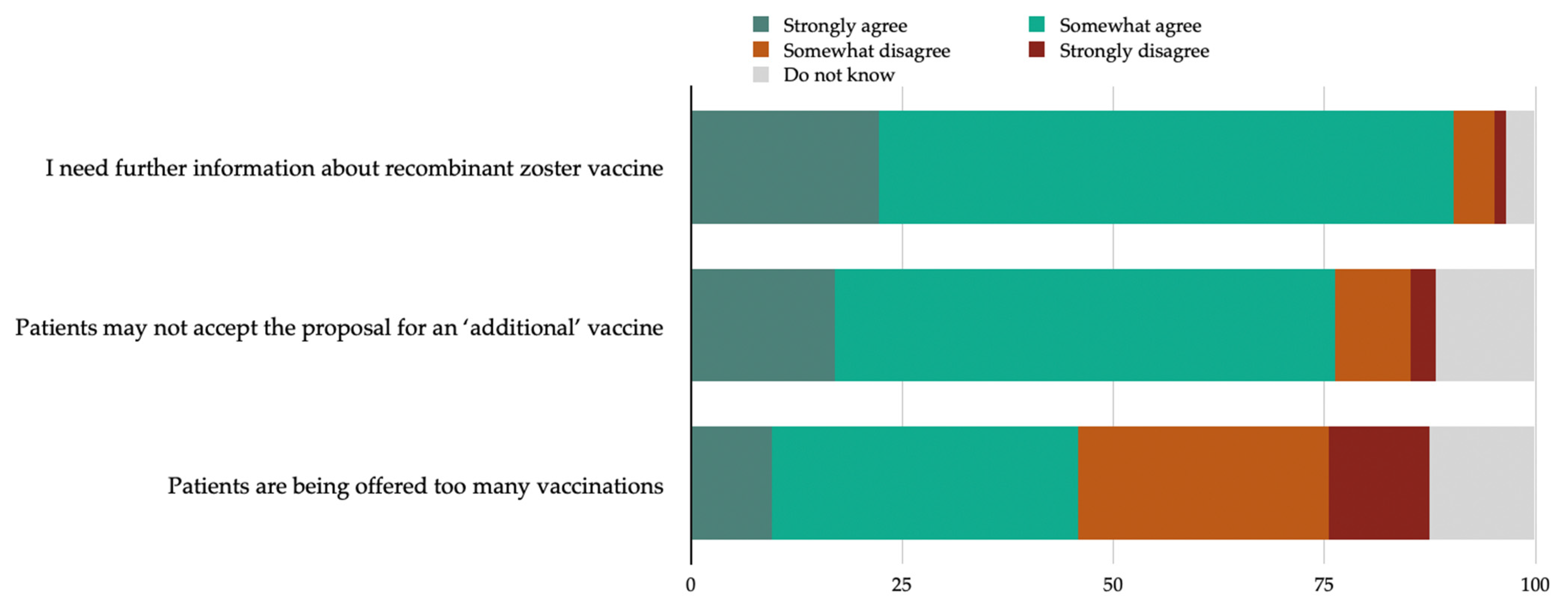
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sampathkumar, P.; Drage, L.A.; Martin, D.P. Herpes Zoster (Shingles) and Postherpetic Neuralgia. Mayo Clin. Proc. 2009, 84, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.I. Herpes Zoster. N. Engl. J. Med. 2013, 369, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.X.; Lee, M.S.; Nambudiri, V.E. Global Herpes Zoster Incidence, Burden of Disease, and Vaccine Availability: A Narrative Review. Ther. Adv. Vaccines Immunother. 2022, 10, 25151355221084535. [Google Scholar] [CrossRef]
- Van Oorschot, D.; Vroling, H.; Bunge, E.; Diaz-Decaro, J.; Curran, D.; Yawn, B. A Systematic Literature Review of Herpes Zoster Incidence Worldwide. Hum. Vaccines Immunother. 2021, 17, 1714–1732. [Google Scholar] [CrossRef] [PubMed]
- Kawai, K.; Gebremeskel, B.G.; Acosta, C.J. Systematic Review of Incidence and Complications of Herpes Zoster: Towards a Global Perspective. BMJ Open 2014, 4, e004833. [Google Scholar] [CrossRef] [PubMed]
- Curran, D.; Callegaro, A.; Fahrbach, K.; Neupane, B.; Vroling, H.; Van Oorschot, D.; Yawn, B.P. Meta-Regression of Herpes Zoster Incidence Worldwide. Infect. Dis. Ther. 2022, 11, 389–403. [Google Scholar] [CrossRef]
- Marra, F.; Parhar, K.; Huang, B.; Vadlamudi, N. Risk Factors for Herpes Zoster Infection: A Meta-Analysis. Open Forum Infect. Dis. 2020, 7, ofaa005. [Google Scholar] [CrossRef]
- Hata, A.; Kuniyoshi, M.; Ohkusa, Y. Risk of Herpes Zoster in Patients with Underlying Diseases: A Retrospective Hospital-Based Cohort Study. Infection 2011, 39, 537–544. [Google Scholar] [CrossRef]
- Wu, P.-H.; Lin, Y.-T.; Lin, C.-Y.; Huang, M.-Y.; Chang, W.-C.; Chang, W.-P. A Nationwide Population-Based Cohort Study to Identify the Correlation between Heart Failure and the Subsequent Risk of Herpes Zoster. BMC Infect. Dis. 2015, 15, 17. [Google Scholar] [CrossRef]
- Esteban-Vasallo, M.D.; Domínguez-Berjón, M.F.; Gil-Prieto, R.; Astray-Mochales, J.; Gil De Miguel, Á. Sociodemographic Characteristics and Chronic Medical Conditions as Risk Factors for Herpes Zoster: A Population-Based Study from Primary Care in Madrid (Spain). Hum. Vaccines Immunother. 2014, 10, 1650–1660. [Google Scholar] [CrossRef]
- Guignard, A.P.; Greenberg, M.; Lu, C.; Rosillon, D.; Vannappagari, V. Risk of Herpes Zoster among Diabetics: A Matched Cohort Study in a US Insurance Claim Database before Introduction of Vaccination, 1997–2006. Infection 2014, 42, 729–735. [Google Scholar] [CrossRef]
- Curhan, S.G.; Kawai, K.; Yawn, B.; Rexrode, K.M.; Rimm, E.B.; Curhan, G.C. Herpes Zoster and Long-Term Risk of Cardiovascular Disease. J. Am. Heart Assoc. 2022, 11, e027451. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.-H.; Chuang, Y.-S.; Lin, Y.-T. Does Herpes Zoster Increase the Risk of Stroke and Myocardial Infarction? A Comprehensive Review. J. Clin. Med. 2019, 8, 547. [Google Scholar] [CrossRef] [PubMed]
- Parameswaran, G.I.; Drye, A.F.; Wattengel, B.A.; Carter, M.T.; Doyle, K.M.; Mergenhagen, K.A. Increased Myocardial Infarction Risk Following Herpes Zoster Infection. Open Forum Infect. Dis. 2023, 10, ofad137. [Google Scholar] [CrossRef] [PubMed]
- Horev, A.; Horev, A.; Gordon-Irshai, A.; Gordon, M.; Andre, N.; Ifergane, G. Herpes Zoster and Long-Term Vascular Risk: A Retrospective Cohort Study. Sci. Rep. 2023, 13, 2364. [Google Scholar] [CrossRef] [PubMed]
- Ministero della Salute. Piano Nazionale Prevenzione Vaccinale. 2023. Available online: https://www.salute.gov.it/portale/vaccinazioni/dettaglioContenutiVaccinazioni.jsp?lingua=italiano&id=4828&area=vaccinazioni&menu=vuoto (accessed on 1 December 2023).
- Cataldi, J.R.; Kerns, M.E.; O’Leary, S.T. Evidence-Based Strategies to Increase Vaccination Uptake: A Review. Curr. Opin. Pediatr. 2020, 32, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Loftus, R.; Sahm, L.J.; Fleming, A. A Qualitative Study of the Views of Healthcare Professionals on Providing Vaccines Information to Patients. Int. J. Clin. Pharm. 2021, 43, 1683–1692. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, P.; Stromillo, L.; Albano, L. Awareness, Attitudes, and Practices Toward Meningococcal B Vaccine among Pediatricians in Italy. Medicina 2018, 54, 100. [Google Scholar] [CrossRef]
- Kuehn, B.M. Health Care Professionals’ Advice Can Increase COVID-19 Vaccination. JAMA 2022, 327, 518. [Google Scholar] [CrossRef]
- Ianni, A.; Tedeschi, R.; Marchetti, A. The Role of Nurses in Health Education about Vaccines: Analysis of Style and Communication Models of Institutional Vaccination Campaigns. Ig Sanita Pubbl. 2019, 75, 355–369. [Google Scholar]
- Cassidy, C.; Langley, J.; Steenbeek, A.; Taylor, B.; Kennie-Kaulbach, N.; Grantmyre, H.; Stratton, L.; Isenor, J. A Behavioral Analysis of Nurses’ and Pharmacists’ Role in Addressing Vaccine Hesitancy: Scoping Review. Hum. Vaccines Immunother. 2021, 17, 4487–4504. [Google Scholar] [CrossRef] [PubMed]
- Hurley, L.P.; O’Leary, S.T.; Dooling, K.; Anderson, T.C.; Crane, L.A.; Cataldi, J.R.; Brtnikova, M.; Beaty, B.L.; Gorman, C.; Guo, A.; et al. Survey of Physician Practices, Attitudes, and Knowledge Regarding Recombinant Zoster Vaccine. J. Gen. Intern. Med. 2023, 38, 986–993. [Google Scholar] [CrossRef] [PubMed]
- Yawn, B.P.; Merrill, D.D.; Martinez, S.; Callen, E.; Cotton, J.; Williams, D.; Loskutova, N.Y. Knowledge and Attitudes Concerning Herpes Zoster among People with COPD: An Interventional Survey Study. Vaccines 2022, 10, 420. [Google Scholar] [CrossRef] [PubMed]
- Hurley, L.P.; Allison, M.A.; Dooling, K.L.; O’Leary, S.T.; Crane, L.A.; Brtnikova, M.; Beaty, B.L.; Allen, J.A.; Guo, A.; Lindley, M.C.; et al. Primary Care Physicians’ Experience with Zoster Vaccine Live (ZVL) and Awareness and Attitudes Regarding the New Recombinant Zoster Vaccine (RZV). Vaccine 2018, 36, 7408–7414. [Google Scholar] [CrossRef] [PubMed]
- Vezzosi, L.; Riccò, M.; Agozzino, E.; Odone, A.; Signorelli, C. Knowledge, Attitudes, and Practices of General Practitioners from the Province of Parma (Northern Italy) towards Vaccinations in Adults ≥ 65 Year-Old. Acta Bio Medica Atenei Parm. 2019, 90, 71–75. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 18. 2023. Available online: https://www.stata.com (accessed on 1 December 2023).
- Choudhry, N.K.; Fletcher, R.H.; Soumerai, S.B. Systematic Review: The Relationship between Clinical Experience and Quality of Health Care. Ann. Intern. Med. 2005, 142, 260. [Google Scholar] [CrossRef] [PubMed]
- Yamashiro, H.; Cutcliffe, N.; Dobson, S.; Fisman, D.; Gold, R. The Role of Pediatricians as Key Stakeholders in Influencing Immunization Policy Decisions for the Introduction of Meningitis B Vaccine in Canada: The Ontario Perspective. Can. J. Infect. Dis. Med. Microbiol. 2015, 26, 183–190. [Google Scholar] [CrossRef]
- Morrone, T.; Napolitano, F.; Albano, L.; Di Giuseppe, G. Meningococcal Serogroup B Vaccine: Knowledge and Acceptability among Parents in Italy. Hum. Vaccines Immunother. 2017, 13, 1921–1927. [Google Scholar] [CrossRef]
- Baalbaki, N.A.; Fava, J.P.; Ng, M.; Okorafor, E.; Nawaz, A.; Chiu, W.; Salim, A.; Cha, R.; Kilgore, P.E. A Community-Based Survey to Assess Knowledge, Attitudes, Beliefs and Practices Regarding Herpes Zoster in an Urban Setting. Infect. Dis. Ther. 2019, 8, 687–694. [Google Scholar] [CrossRef]
- Teeter, B.S.; Garza, K.B.; Stevenson, T.L.; Williamson, M.A.; Zeek, M.L.; Westrick, S.C. Factors Associated with Herpes Zoster Vaccination Status and Acceptance of Vaccine Recommendation in Community Pharmacies. Vaccine 2014, 32, 5749–5754. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, L.; Li, L.; Liu, C.; Jin, H.; Lin, L. Willingness to Vaccinate Against Herpes Zoster and Its Associated Factors Across WHO Regions: Global Systematic Review and Meta-Analysis. JMIR Public Health Surveill. 2023, 9, e43893. [Google Scholar] [CrossRef] [PubMed]
- Kizmaz, M.; Kumtepe Kurt, B.; Çetin Kargin, N.; Döner, E. Influenza, Pneumococcal and Herpes Zoster Vaccination Rates among Patients over 65 Years of Age, Related Factors, and Their Knowledge and Attitudes. Aging Clin. Exp. Res. 2020, 32, 2383–2391. [Google Scholar] [CrossRef] [PubMed]
- Lu, P.-J.; Hung, M.-C.; Srivastav, A.; Grohskopf, L.A.; Kobayashi, M.; Harris, A.M.; Dooling, K.L.; Markowitz, L.E.; Rodriguez-Lainz, A.; Williams, W.W. Surveillance of Vaccination Coverage Among Adult Populations—United States, 2018. MMWR Surveill. Summ. 2021, 70, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Wood, J.G.; Bernardo, C.; Stocks, N.P.; Liu, B. Herpes Zoster Vaccine Coverage in Australia before and after Introduction of a National Vaccination Program. Vaccine 2020, 38, 3646–3652. [Google Scholar] [CrossRef] [PubMed]
- Leung, S.O.A.; Akinwunmi, B.; Elias, K.M.; Feldman, S. Educating Healthcare Providers to Increase Human Papillomavirus (HPV) Vaccination Rates: A Qualitative Systematic Review. Vaccine X 2019, 3, 100037. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.U.; Cheong, H.J.; Choi, W.S.; Song, J.Y.; Noh, J.Y.; Kim, W.J. Physician Attitudes toward the Herpes Zoster Vaccination in South Korea. Infect. Chemother. 2014, 46, 194. [Google Scholar] [CrossRef]
- Joon Lee, T.; Hayes, S.; Cummings, D.M.; Cao, Q.; Carpenter, K.; Heim, L.; Edwards, H. Herpes Zoster Knowledge, Prevalence, and Vaccination Rate by Race. J. Am. Board Fam. Med. 2013, 26, 45–51. [Google Scholar] [CrossRef]
- Prieto-Campo, Á.; Batista, A.D.; Magalhães Silva, T.; Herdeiro, M.T.; Roque, F.; Figueiras, A.; Zapata-Cachafeiro, M. Understanding Vaccination Hesitation among Health Professionals: A Systematic Review of Qualitative Studies. Public Health 2024, 226, 17–26. [Google Scholar] [CrossRef]
- Guillari, A.; Polito, F.; Pucciarelli, G.; Serra, N.; Gargiulo, G.; Esposito, M.R.; Botti, S.; Rea, T.; Simeone, S. Influenza Vaccination and Healthcare Workers: Barriers and Predisposing Factors.: A Literature Review. Acta Biomed. 2021, 92 (Suppl. S2), e2021004. [Google Scholar] [CrossRef]
- Calculator.net. Sample Size Calculator. 2023. Available online: https://www.calculator.net/sample-size-calculator.html?type=1&cl=95&ci=5&pp=90&ps=&x=Calculate (accessed on 1 December 2023).
| Characteristic | N | Percentage |
|---|---|---|
| Gender | ||
| Male | 58 | 37.7 |
| Female | 96 | 62.3 |
| Age ^ | 45.7 ± 11.3 | |
| Educational level | ||
| Master’s degree or higher | 62 | 40.3 |
| Other | 92 | 59.7 |
| Professional role | ||
| Nurse | 99 | 64.3 |
| Physician | 55 | 35.7 |
| Hospital unit | ||
| Cardiology | 18 | 12.0 |
| Interventional cardiology | 23 | 15.3 |
| Electrophysiology | 10 | 6.7 |
| Cardiac surgery | 21 | 14.0 |
| Post-surgery intensive care | 18 | 12.0 |
| Cardiac intensive care | 15 | 10.0 |
| Cardio-pulmonology | 14 | 9.3 |
| More than one unit | 16 | 10.7 |
| Others/non-cardiology unit | 15 | 10.0 |
| Previous professional update on vaccination | ||
| Yes | 61 | 41.2 |
| No | 87 | 58.8 |
| Experience in managing patients with herpes zoster | ||
| Yes | 59 | 38.3 |
| No | 95 | 61.7 |
| Item * | N | Percentage |
|---|---|---|
| HZ risk factors | ||
| Age > 50 years | ||
| Yes | 59 | 38.3 |
| No | 95 | 61.7 |
| Immunosuppression | ||
| Yes | 116 | 75.3 |
| No | 38 | 24.7 |
| Malignancy | ||
| Yes | 33 | 21.4 |
| No | 121 | 78.6 |
| Multiple chronic conditions | ||
| Yes | 57 | 37.0 |
| No | 97 | 63.0 |
| Major HZ consequences and complications | ||
| Post-herpetic neuralgia | ||
| Yes | 82 | 53.2 |
| No | 72 | 46.8 |
| Recurrence | ||
| Yes | 65 | 42.2 |
| No | 89 | 57.8 |
| Major cardiovascular events | ||
| Yes | 55 | 35.7 |
| No | 99 | 64.3 |
| Knowledge that HZ vaccines are included in the National Vaccination Plan | ||
| Yes | 16 | 10.9 |
| No | 131 | 89.1 |
| Knowledge that zoster vaccine live (ZVL) uses a one-dose schedule | ||
| Yes | 72 | 48.0 |
| No | 78 | 72.0 |
| Knowledge of RZV vaccination schedule (i.e., two doses and timing) | ||
| Yes | 43 | 29.1 |
| No | 105 | 70.9 |
| Knowledge about the possibility of RZV administration in immunocompromised individuals | ||
| Yes | 87 | 57.6 |
| No | 64 | 42.4 |
| Attitude toward RZV safety ^ | 7.4 ± 2.2 | |
| Attitude toward RZV effectiveness ^ | 7.4 ± 2.1 | |
| Have you previously recommended or suggested vaccination to a patient at risk of HZ (either ZVL or RZV)? | ||
| Yes | 69 | 46.3 |
| No | 80 | 53.7 |
| Will you recommend or suggest HZ vaccination to your patients? | ||
| Yes | 116 | 78.9 |
| No | 31 | 21.1 |
| Model 1: Knowledge about the possibility of RZV administration in immunocompromised individuals (N = 137) | ||||
| Variable | Odds ratio | SE | 95%CI | p-value |
| Log likelihood = −67.68; χ2 = 45.53 (5 df); p-value < 0.0001 | ||||
| Having a master’s degree or higher | 4.42 | 2.15 | 1.70–11.47 | 0.002 |
| Professional update on vaccinations | 3.86 | 1.85 | 1.51–9.87 | 0.005 |
| Awareness that HZ could cause major CV events | 4.23 | 2.23 | 1.50–11.91 | 0.006 |
| Awareness that HZ could cause PHN | 2.56 | 1.17 | 1.05–6.25 | 0.04 |
| Needing further information about RZV | 6.43 | 4.94 | 1.42–29.98 | 0.02 |
| Model 2: Attitude toward RZV effectiveness (N = 132) | ||||
| Variable | Coefficient | SE | 95%CI | p-value |
| F (5,126) = 42.67; R2 = 0.63; adjusted R2 = 0.61; p-value < 0.0001 | ||||
| Positive attitude toward RZV safety (≥8 vs. <8/10) | 2.92 | 0.22 | 2.49–3.36 | <0.001 |
| Age (continuous, in years) | −0.02 | 0.01 | −0.04–−0.01 | 0.02 |
| Experience in managing patients with HZ | 0.45 | 0.21 | 0.03–0.88 | 0.04 |
| Awareness that HZ could recur | 0.33 | 0.22 | −0.09–0.76 | 0.13 |
| Awareness that HZ could cause major CV events | 0.45 | 0.22 | −0.70–0.15 | 0.20 |
| Model 3: Willingness to recommend/suggest HZ vaccination to patients (N = 117) | ||||
| Variable | Odds ratio | SE | 95%CI | p-value |
| Log likelihood = −35.92; χ2 = 31.97 (4 df); p-value < 0.0001 | ||||
| Positive attitude toward RZV effectiveness (≥8 vs. <8/10) | 7.17 | 5.24 | 1.71–30.03 | 0.007 |
| Having a master’s degree or higher | 7.21 | 5.92 | 1.44–36.08 | 0.02 |
| Age (continuous, in years) | 0.94 | 0.03 | 0.89–0.99 | 0.04 |
| Having recommended HZ vaccine in the past | 4.03 | 2.70 | 1.08–14.96 | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ponticelli, D.; Antonazzo, I.C.; Losa, L.; Zampella, A.; Di Marino, F.; Mottola, G.; Fede, M.N.; Gallucci, F.; Magliuolo, R.; Rainone, A.; et al. Knowledge, Attitudes and Practices Survey of Recombinant Zoster Vaccine among Cardiologists and Cardiac Nurses in Italy. Medicina 2024, 60, 93. https://doi.org/10.3390/medicina60010093
Ponticelli D, Antonazzo IC, Losa L, Zampella A, Di Marino F, Mottola G, Fede MN, Gallucci F, Magliuolo R, Rainone A, et al. Knowledge, Attitudes and Practices Survey of Recombinant Zoster Vaccine among Cardiologists and Cardiac Nurses in Italy. Medicina. 2024; 60(1):93. https://doi.org/10.3390/medicina60010093
Chicago/Turabian StylePonticelli, Domenico, Ippazio Cosimo Antonazzo, Lorenzo Losa, Anna Zampella, Fabio Di Marino, Gaetano Mottola, Mara Noemi Fede, Fortuna Gallucci, Roberto Magliuolo, Antonio Rainone, and et al. 2024. "Knowledge, Attitudes and Practices Survey of Recombinant Zoster Vaccine among Cardiologists and Cardiac Nurses in Italy" Medicina 60, no. 1: 93. https://doi.org/10.3390/medicina60010093
APA StylePonticelli, D., Antonazzo, I. C., Losa, L., Zampella, A., Di Marino, F., Mottola, G., Fede, M. N., Gallucci, F., Magliuolo, R., Rainone, A., Del Giudice, C., Arcari, A., & Ferrara, P. (2024). Knowledge, Attitudes and Practices Survey of Recombinant Zoster Vaccine among Cardiologists and Cardiac Nurses in Italy. Medicina, 60(1), 93. https://doi.org/10.3390/medicina60010093








