Monitored Anesthesia Care in Minimally Invasive Spine Surgery—A Retrospective Case Series Study
Abstract
:1. Introduction
2. Materials and Methods
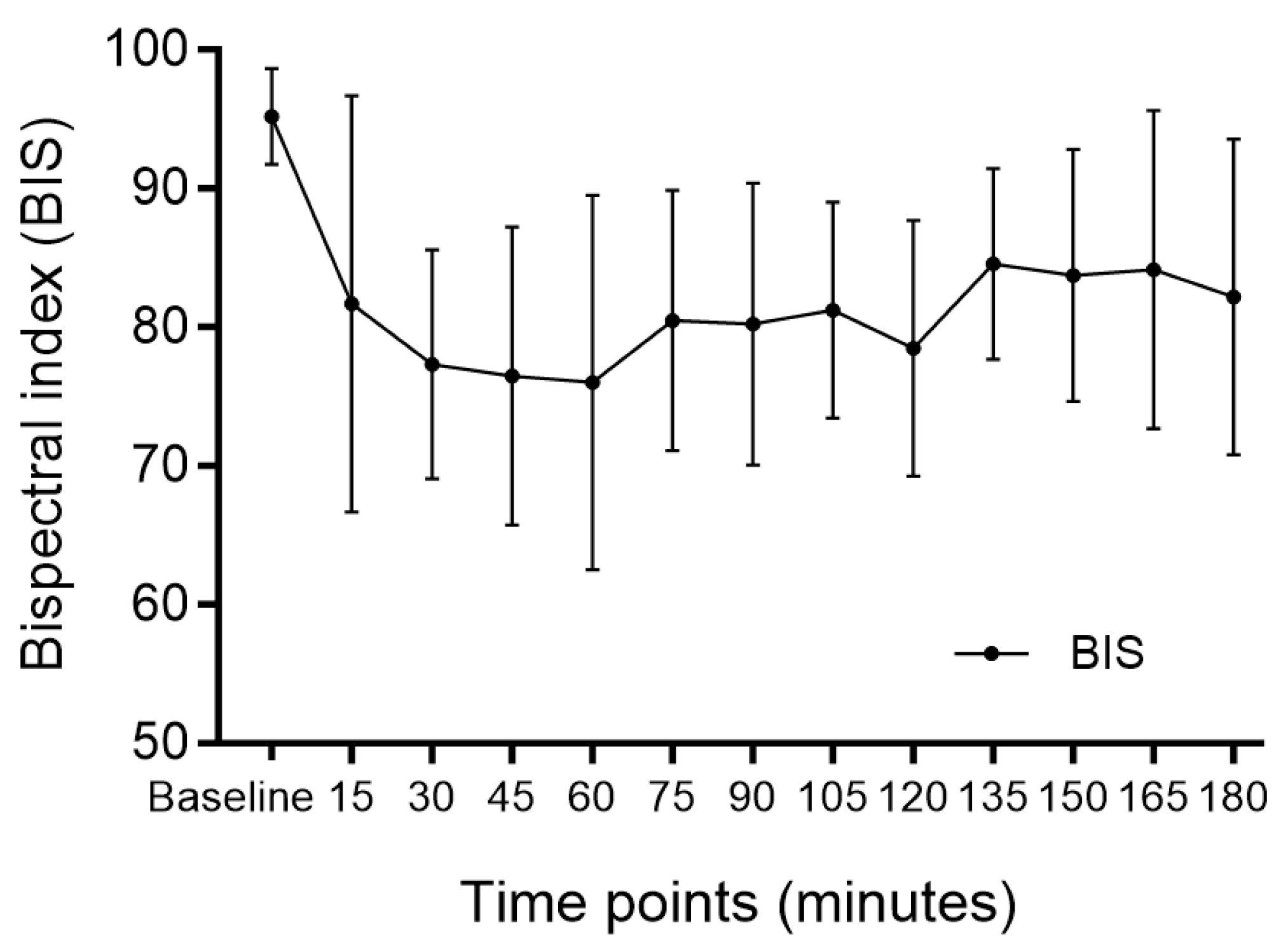
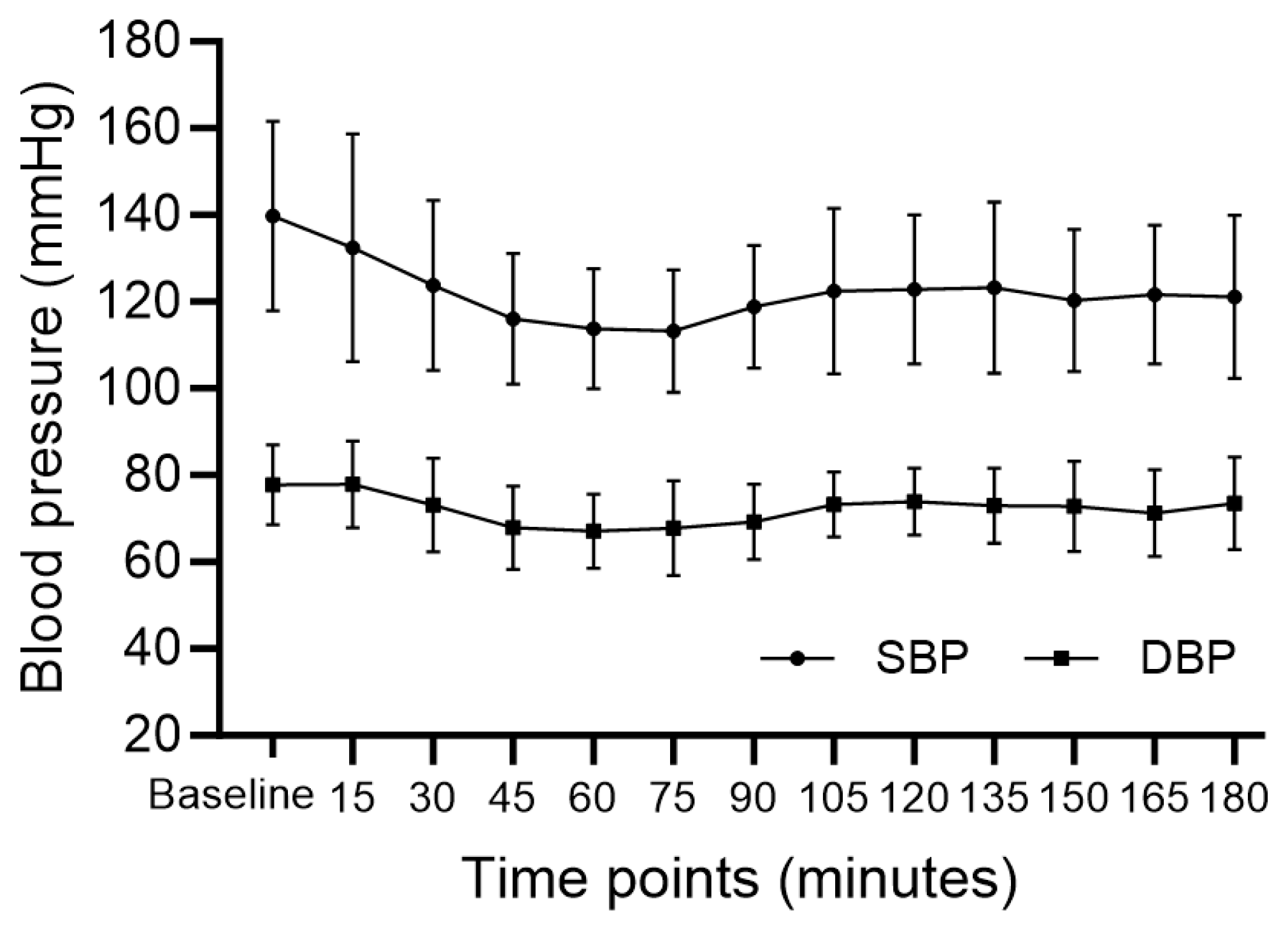
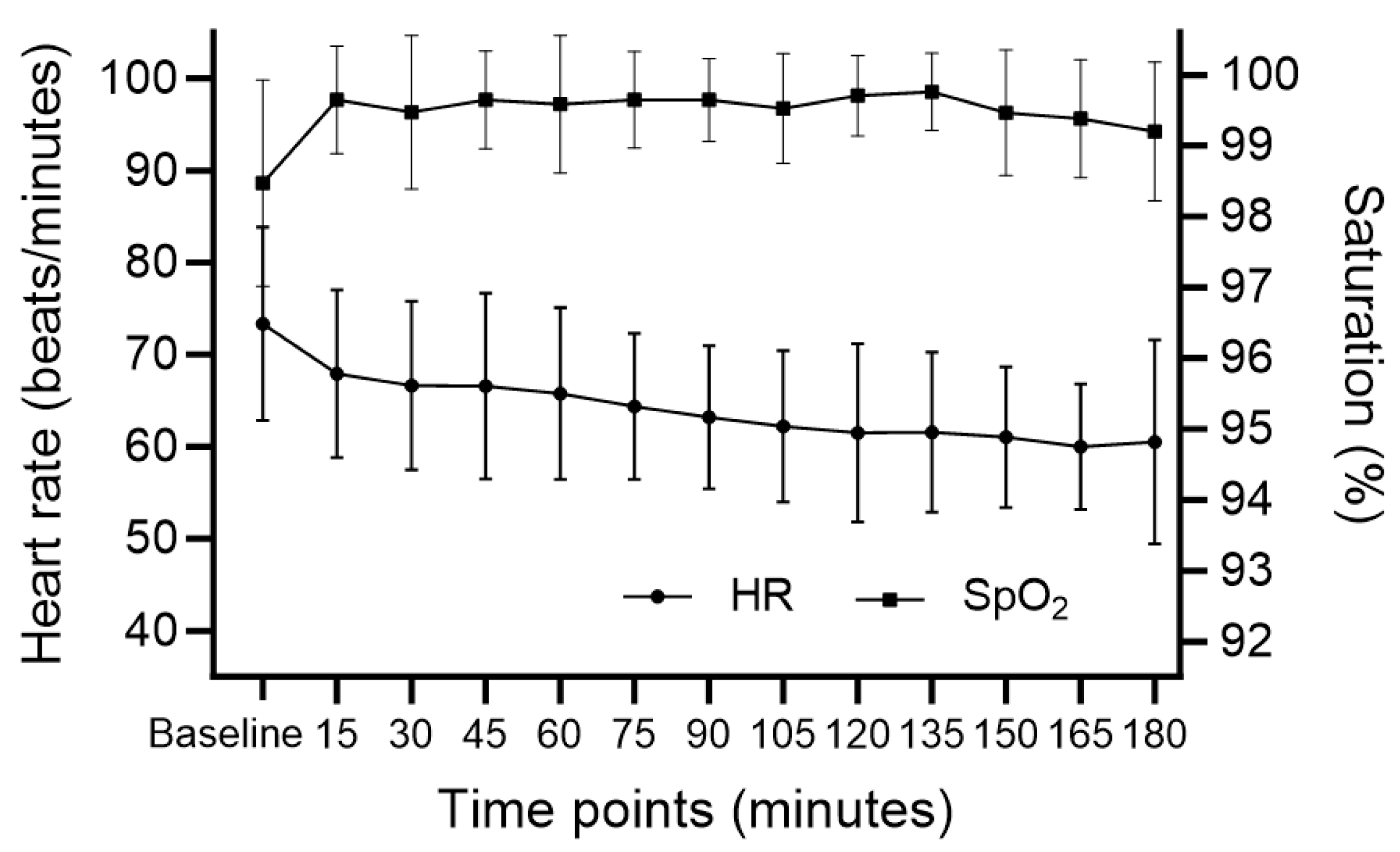
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deyo, R.A.; Mirza, S.K.; Martin, B.I.; Kreuter, W.; Goodman, D.C.; Jarvik, J.G. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. Jama 2010, 303, 1259–1265. [Google Scholar] [CrossRef] [PubMed]
- Johnson, W.C.; Seifi, A. Trends of the neurosurgical economy in the United States. J. Clin. Neurosci. 2018, 53, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Rajaee, S.S.; Bae, H.W.; Kanim, L.E.; Delamarter, R.B. Spinal fusion in the United States: Analysis of trends from 1998 to 2008. Spine 2012, 37, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.D.; Canseco, J.A.; Houlihan, N.; Gabay, A.; Grasso, G.; Vaccaro, A.R. Overview of minimally invasive spine surgery. World Neurosurg. 2020, 142, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Kolcun, J.P.G.; Brusko, G.D.; Basil, G.W.; Epstein, R.; Wang, M.Y. Endoscopic transforaminal lumbar interbody fusion without general anesthesia: Operative and clinical outcomes in 100 consecutive patients with a minimum 1-year follow-up. Neurosurg. Focus 2019, 46, E14. [Google Scholar] [CrossRef]
- Chan, A.K.; Bisson, E.F.; Bydon, M.; Foley, K.T.; Glassman, S.D.; Shaffrey, C.I.; Wang, M.Y.; Park, P.; Potts, E.A.; Shaffrey, M.E. A comparison of minimally invasive and open transforaminal lumbar interbody fusion for grade 1 degenerative lumbar spondylolisthesis: An analysis of the prospective quality outcomes database. Neurosurgery 2020, 87, 555–562. [Google Scholar] [CrossRef]
- Debono, B.; Wainwright, T.W.; Wang, M.Y.; Sigmundsson, F.G.; Yang, M.M.; Smid-Nanninga, H.; Bonnal, A.; Huec, J.-C.L.; Fawcett, W.J.; Ljungqvist, O. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery after Surgery (ERAS®) Society recommendations. Spine J. 2021, 21, 729–752. [Google Scholar] [CrossRef]
- Raw, D.A.; Beattie, J.K.; Hunter, J.M. Anaesthesia for spinal surgery in adults. BJA Br. J. Anaesth. 2003, 91, 886–904. [Google Scholar] [CrossRef]
- Ghisi, D.; Fanelli, A.; Tosi, M.; Nuzzi, M.; Fanelli, G. Monitored anesthesia care. Minerva Anestesiol. 2005, 71, 533–538. [Google Scholar]
- Nelson, L.E.; Lu, J.; Guo, T.; Saper, C.B.; Franks, N.P.; Maze, M. The α2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects. J. Am. Soc. Anesthesiol. 2003, 98, 428–436. [Google Scholar] [CrossRef]
- Basil, G.W.; Wang, M.Y. Trends in outpatient minimally invasive spine surgery. J. Spine Surg. 2019, 5, S108. [Google Scholar] [CrossRef] [PubMed]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R. The Richmond Agitation–Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- An Updated Report by the American Society of Anesthesiologists Task Force on, S.; Analgesia by, N.-A. Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists. Anesthesiology 2002, 96, 1004–1017. [CrossRef]
- Doo, A.R.; Lee, H.; Baek, S.J.; Lee, J. Dexmedetomidine-induced hemodynamic instability in patients undergoing orthopedic upper limb surgery under brachial plexus block: A retrospective study. BMC Anesthesiol. 2021, 21, 207. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Cheng, X.; Chen, B. Comparison of 270-degree percutaneous transforaminal endoscopic decompression under local anesthesia and minimally invasive transforaminal lumbar interbody fusion in the treatment of geriatric lateral recess stenosis associated with degenerative lumbar spondylolisthesis. J. Orthop. Surg. Res. 2023, 18, 183. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, S.M.; Rajaei, S.; Falsafi, M.; Golmakani, E.; Behnaz, F.; Zali, A.; Asgari, S. S1 Transforaminal Epidural Anesthesia in Percutaneous Transforaminal Endoscopic Discectomy: A Case-Series Study. Anesth. Pain Med. 2023, 13, e131746. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zheng, L.; Ma, J.X.; Wang, H.; Wang, K.Q.; Chen, Y.; Yu, H.L.; Xiang, L.B. Comparison of 2 Anesthetic Methods for Transforaminal Endoscopic Lumbar Discectomy: A Prospective Randomized Controlled Study. Glob. Spine J. 2023, 21925682231220550. [Google Scholar] [CrossRef]
- Lu, V.M.; Brusko, G.D.; Urakov, T.M. Defining the Time Benefit of Awake versus General Anesthesia for Single-Level Lumbar Spine Surgery. World Neurosurg. 2022, 158, e793–e798. [Google Scholar] [CrossRef]
- Mazur, M.D.; Dailey, A.T. Reducing the burden of spine fusion. Neurosurg. Focus 2019, 46, E15. [Google Scholar] [CrossRef]
- Sohn, H.-m.; Ryu, J.-H. Monitored anesthesia care in and outside the operating room. Korean J. Anesthesiol. 2016, 69, 319–326. [Google Scholar] [CrossRef]
- Candiotti, K.A.; Bergese, S.D.; Bokesch, P.M.; Feldman, M.A.; Wisemandle, W.; Bekker, A.Y.; Group, M.S. Monitored anesthesia care with dexmedetomidine: A prospective, randomized, double-blind, multicenter trial. Anesth. Analg. 2010, 110, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.-J.; Koo, B.-W.; Bang, S.-U.; Kim, J.-H.; Hwang, J.-W.; SH, D.; Na, H.-S. Intraoperative dexmedetomidine sedation reduces the postoperative agitated behavior in elderly patients undergoing orthopedic surgery compared to the propofol sedation. Minerva Anestesiol. 2017, 83, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Vaishnav, A.S.; Othman, Y.A.; Virk, S.S.; Gang, C.H.; Qureshi, S.A. Current state of minimally invasive spine surgery. J. Spine Surg. 2019, 5, S2. [Google Scholar] [CrossRef] [PubMed]
- Donatiello, V.; Alfieri, A.; Napolitano, A.; Maffei, V.; Coppolino, F.; Pota, V.; Passavanti, M.B.; Pace, M.C.; Sansone, P. Opioid sparing effect of intravenous dexmedetomidine in orthopaedic surgery: A retrospective analysis. J. Anesth. Analg. Crit. Care 2022, 2, 49. [Google Scholar] [CrossRef]
- Soffin, E.M.; Wetmore, D.S.; Beckman, J.D.; Sheha, E.D.; Vaishnav, A.S.; Albert, T.J.; Gang, C.H.; Qureshi, S.A. Opioid-free anesthesia within an enhanced recovery after surgery pathway for minimally invasive lumbar spine surgery: A retrospective matched cohort study. Neurosurg. Focus 2019, 46, E8. [Google Scholar] [CrossRef]
- Montano, N.; Cogliati, C.; Porta, A.; Pagani, M.; Malliani, A.; Narkiewicz, K.; Abboud, F.M.; Birkett, C.; Somers, V.K. Central vagotonic effects of atropine modulate spectral oscillations of sympathetic nerve activity. Circulation 1998, 98, 1394–1399. [Google Scholar] [CrossRef]
- Chin, K.; Seow, S. Atrioventricular conduction block induced by low-dose atropine. Anaesthesia 2005, 60, 935–936. [Google Scholar] [CrossRef]
| Value | |
|---|---|
| Age, years | 67 [63–80] |
| Sex | |
| Male | 12 (70.6%) |
| Female | 5 (29.4%) |
| Height, cm | 161.9 [158.3–168.2] |
| Weight, kg | 66.6 [58.0–71.8] |
| BMI, kg/m2 | 25.1 [22.1–26.5] |
| ASA PS | |
| 1 | 5 (29.4%) |
| 2 | 11 (64.7%) |
| 3 | 1 (5.9%) |
| Previous medical history | |
| Hypertension | 6 (35.3%) |
| Diabetes | 3 (17.6%) |
| Arrhythmia | 2 (11.8%) |
| Coronary artery disease | 1 (5.9%) |
| Asthma | 1 (5.9%) |
| Liver disease | 1 (5.9%) |
| Diagnosis | |
| Spinal stenosis | 12 (70.6%) |
| HIVD | 3 (17.6%) |
| Facet joint syndrome | 1 (5.9%) |
| Compression fracture | 1 (5.9%) |
| Value | |
|---|---|
| No. of operated spine levels | |
| 1 | 14 (82.6%) |
| 2 | 2 (11.8%) |
| 3 | 1 (5.9%) |
| Type of surgery | |
| Dome laminoplasty | 14 (82.4%) |
| PELD | 3 (17.6%) |
| Duration of surgery, mins | 140 [130–155] |
| Duration of anesthesia, mins | 185 [170–200] |
| Recovery time, mins | 62.0 [47.0–72.0] |
| Premedication | |
| Midazolam | 7 (41.2%) |
| Glycopyrrolate | 2 (11.8%) |
| None | 8 (47.0%) |
| Dexmedetomidine | |
| Loading dose, mcg/kg | 0.70 [0.67–0.82] |
| Maintenance dose, mcg/kg/hr | 0.40 [0.40–0.60] |
| Total infused dose, mcg/kg | 1.93 [1.72–2.37] |
| Need for rescue sedative | 4 (23.6%) |
| Value | |
|---|---|
| Hypotension (SBP < 90 mmHg) | 6 (35.3%) |
| Bradycardia (HR < 45 bpm) | 3 (17.6%) |
| Need for continuous infusion of phenylephrine | 3 (17.6%) |
| Conversion to general anesthesia | 0 (0%) |
| Postoperative nausea and vomiting | 3 (17.6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.J.; Park, S.; Lim, Y.; Bang, S.R. Monitored Anesthesia Care in Minimally Invasive Spine Surgery—A Retrospective Case Series Study. Medicina 2024, 60, 43. https://doi.org/10.3390/medicina60010043
Kim HJ, Park S, Lim Y, Bang SR. Monitored Anesthesia Care in Minimally Invasive Spine Surgery—A Retrospective Case Series Study. Medicina. 2024; 60(1):43. https://doi.org/10.3390/medicina60010043
Chicago/Turabian StyleKim, Hyo Jin, Seongho Park, Yunhee Lim, and Si Ra Bang. 2024. "Monitored Anesthesia Care in Minimally Invasive Spine Surgery—A Retrospective Case Series Study" Medicina 60, no. 1: 43. https://doi.org/10.3390/medicina60010043
APA StyleKim, H. J., Park, S., Lim, Y., & Bang, S. R. (2024). Monitored Anesthesia Care in Minimally Invasive Spine Surgery—A Retrospective Case Series Study. Medicina, 60(1), 43. https://doi.org/10.3390/medicina60010043







