Effectiveness of Acupotomy Combined with Epidural Steroid Injection for Lumbosacral Radiculopathy: A Randomized Controlled Pragmatic Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Randomization and Blinding
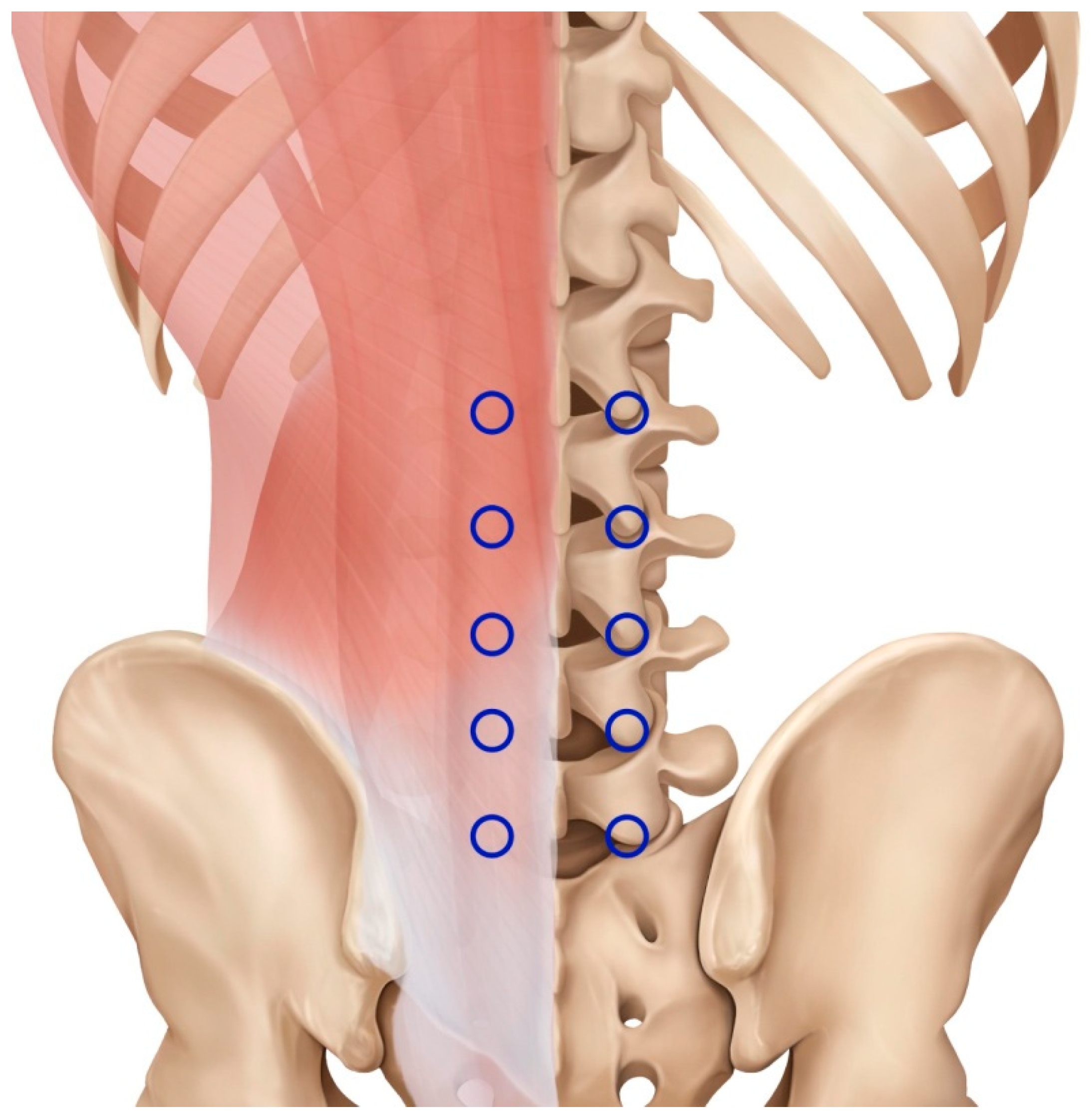
2.4. Interventions
2.5. Outcome Measures
2.6. Sample Size Calculation
2.7. Statistical Analysis
3. Results
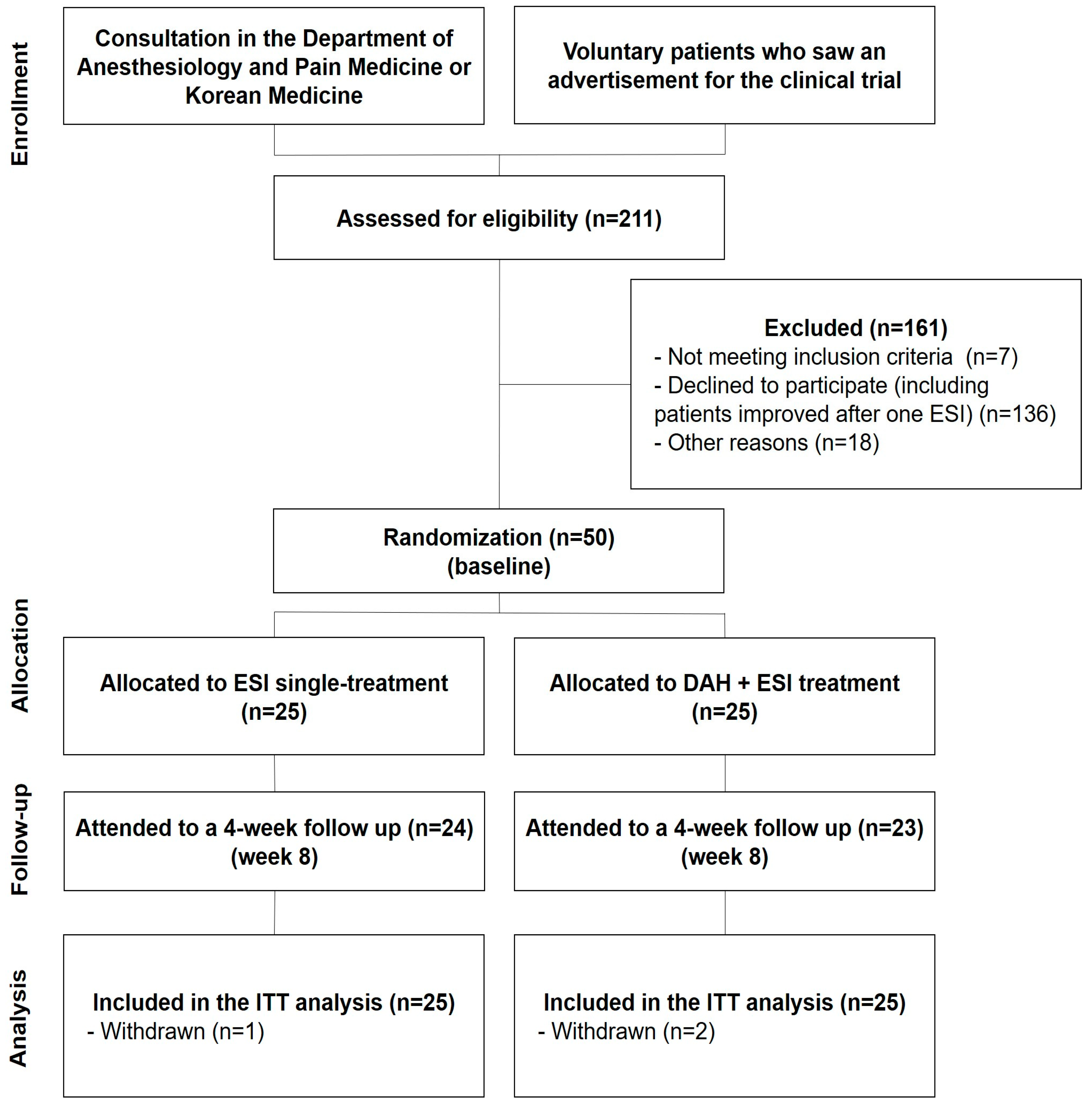
3.1. Participants
3.2. Baseline Characteristics
3.3. Outcomes
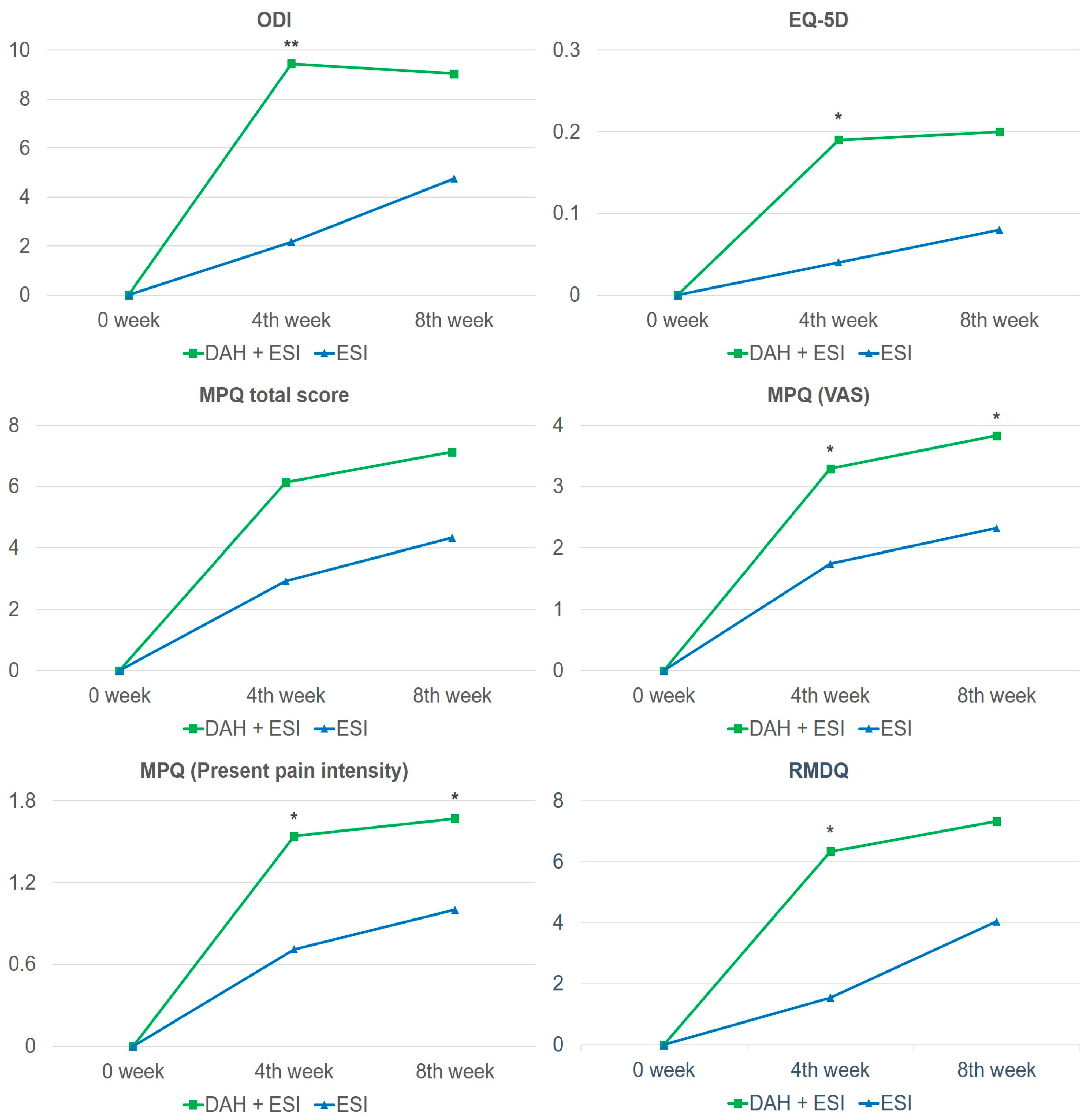
3.3.1. Primary Outcomes
3.3.2. Secondary Outcomes
3.3.3. Evaluation of Outcomes
3.3.4. Cost-Effectiveness
3.3.5. Safety and AEs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boxem, K.V.; Cheng, J.; Patjin, J.; Kleef, M.V.; Lataster, A.; Mekhail, N.; Zundert, J.V. Lumbosacral radicular pain. Pain Pract. 2010, 10, 339–358. [Google Scholar] [CrossRef] [PubMed]
- Cosamalón-Gan, I.; Cosamalón-Gan, T.; Mattos-Piaggio, G.; Villar-Suárez, V.; García-Cosamalón, J.; Vega-Álvarez, J.A. Inflammation in the intervertebral disc herniation. Neurocirugia 2021, 32, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Vanhoestenberghe, A. Chronic nerve root entrapment: Compression and degeneration. J. Neural. Eng. 2013, 10, 011001. [Google Scholar] [CrossRef] [PubMed]
- Kartha, S.; Ghimire, P.; Winkelstein, B.A. Inhibiting Spinal Secretory Phospholipase A2 After Painful Nerve Root Injury Attenuates Established Pain and Spinal Neuronal Hyperexcitability by Altering Spinal Glutamatergic Signaling. Mol. Pain 2021, 17, 17448069211066221. [Google Scholar] [CrossRef] [PubMed]
- Casey, E. Natural History of Radiculopathy. Phys. Med. Rehabil. Clin. N. Am. 2011, 22, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Berry, J.A.; Elia, C.; Saini, H.S.; Miulli, D.E. A Review of Lumbar Radiculopathy, Diagnosis, and Treatment. Cureus 2019, 11, e5934. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, H.; Kumar, A.; Kishen, T.J. Temporal Pattern of Pain and Disability Following the Administration of a Selective Nerve Root Block in Lumbar Disc Herniation with Radiculopathy. Int. J. Spine Surg. 2021, 15, 1090–1095. [Google Scholar] [CrossRef] [PubMed]
- William, J.; Roehmer, C.; Mansy, L.; Kennedy, D.J. Epidural Steroid Injections. Phys. Med. Rehabil. Clin. N. Am. 2022, 33, 215–231. [Google Scholar] [CrossRef]
- Friedly, J.L.; Comstock, B.A.; Turner, J.A.; Heagerty, P.J.; Deyo, R.A.; Sullivan, S.D.; Bauer, Z.; Bresnahan, B.W.; Avins, A.L.; Nedeljkovic, S.S.; et al. Randomized Trial of Epidural Glucocorticoid Injections for Spinal Stenosis. N. Engl. J. Med. 2014, 371, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Arun-Kumar, K.; Jayaprasad, S.; Senthil, K.; Lohith, H.; Jayaprakash, K.V. The Outcomes of Selective Nerve Root Block for Disc Induced Lumbar Radiculopathy. Malays. Orthop. J. 2015, 9, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Manchikanti, L.; Hirsch, J.A. Neurological Complications Associated with Epidural Steroid Injections. Curr. Pain Headache Rep. 2015, 19, 482. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.M.; Lee, E.Y.; Han, J.H.; Cho, K.H.; Kang, S.R.; Yoon, S.H. Effects of Wonli Acupuncture Procedure in Patients with LSS: A Clinical, Retrospective Study. Evid. Based Complement. Alternat. Med. 2014, 2014, 212098. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Kim, E.; Kwon, O.; Han, C.H.; Kim, Y.I. Effectiveness and Safety of Acupotomy for Lumbar Disc Herniation: A Randomized, Assessor-Blinded, Controlled Pilot Study. Evid. Based Complement. Alternat. Med. 2018, 2018, 5871657. [Google Scholar] [CrossRef]
- Zhong, Y.X.; Ding, Y.; Fu, B.S.; Ma, G.H.; Cui, H.P.; Chen, T.T.; Pan, L.Z.; Liu, Q.; Xu, H.C.; Li, C.X.; et al. Effect of Acupotomy on the Fat Infiltration Degree of Lumbar Multifidus Muscle in Patients with Lumbar Disc Herniation after Percutaneous Transforaminal Endoscopic Discectomy. Zhongguo Zhen Jiu 2023, 43, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Kwon, C.Y.; Yoon, S.H.; Lee, B.; Leem, J. Acupotomy for the Treatment of Lumbar Spinal Stenosis: A Systematic Review and Meta-Analysis. Medicine 2019, 98, e16662. [Google Scholar] [CrossRef]
- Ye, X.L.; Huang, X.L.; Ye, X.M. Meta-analysis on Curative Effect of Small-Needle-Knife Therapy on Lumbar Disc Herniation. China J. Trad. Chin. Med. Pharm. 2016, 07, 2784–2788. [Google Scholar]
- Yu, J.N.; Guo, C.Q.; Hu, B.; Liu, N.G.; Sun, H.M.; Xu, H.; Wu, H.X.; Guo, Y.; Liang, C.X.; Chen, Z.X.; et al. Effects of Acupuncture Knife on Inflammatory Factors and Pain in Third Lumbar Vertebrae Transverse Process Syndrome Model Rats. Evid. Based Complement. Alternat. Med. 2014, 2014, 892406. [Google Scholar] [CrossRef] [PubMed]
- Yanling, J. A clinical study on treating lumbar disc herniation by acupotomy plus awn needle acupuncture at Jiaji point at the waist. CJCM 2022, 14, 67–70. [Google Scholar]
- Zheng, C.L.; Jia, Y.; Zheng, G.Z. Clinical Trials of Slow-Rapid Reinforcing-Reducing Needling Manipulation at Jiaji (EX-B 2) Acupoint for Lumbar Intervertebral Disc Protrusion. Zhen Ci Yan Jiu 2015, 40, 242–246. [Google Scholar]
- Jing, H.T.; Peng, Y.Y.; Chen, M.; Huang, Y.S. Clinical Observation of Lumbar Spinal Stenosis Treated with Deep Puncture at Jiaji (EX-B 2). Zhongguo Zhen Jiu 2011, 31, 791–794. [Google Scholar]
- Rao, X.R.; Ma, Y.C. Deep Needling at Lumbar Jiaji (EX-B 2) Points with Inclined Pull Manipulation for 58 Cases of Prolapse of Lumbar Intervertebral Disc. Zhongguo Zhen Jiu 2013, 33, 253–254. [Google Scholar]
- Wang, H.; Zhang, L.H.; Ning, Z.Z.; Li, S.; Chen, W.; Yu, X.G.; Li, W. Clinical Observation on the Effectiveness and Safety of Deep Needling Jiaji Acupoint in the Treatment of Lumbar Disc Herniation: A Randomized Controlled Trial. Beijing J. Tradit. Chin. Med. 2022, 11, 1296–1299. [Google Scholar]
- Choi, S.; Park, S.; Lim, Y.S.; Park, T.Y.; Do, K.S.; Byun, S.H.; Yoon, S.H.; Lee, J.H. A Comparative Study of a Nerve Block Therapy with and Without a Deeply Inserted Acupotomy Applied to Hyeopcheok Points for Lumbosacral Radiculopathy: Safety, Effectiveness, Cost-Effectiveness (a Randomized Controlled, Two-Arm, Parallel Study, Pilot Study, Assessor-Blind). Medicine 2022, 101, e28983. [Google Scholar] [CrossRef]
- Choi, Y.J.; Lee, J.E.; Moon, W.K.; Cho, S.H. Does the Effect of Acupuncture Depend on Needling Sensation and Manipulation? Complement. Ther. Med. 2013, 21, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Wang, Y.; Zhang, Z.; Cao, H.; Wang, P.; Zhao, M.; Hu, N.; Wu, G.; Hu, S.; Meng, H.; et al. Effects of Needling Depth on Clinical Efficacy of Lumbar Disc Herniation: A Systematic Review. Zhongguo Zhen Jiu 2017, 37, 1015–1020. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.H.; Kim, S.A.; Lee, G.Y.; Kim, H.; Lee, J.H.; Leem, J. Using Magnetic Resonance Imaging to Measure the Depth of Acupotomy Points in the Lumbar Spine: A Retrospective Study. Integr. Med. Res. 2021, 10, 100679. [Google Scholar] [CrossRef] [PubMed]
- Jeon, C.H.; Kim, D.J.; Kim, S.K.; Kim, D.J.; Lee, H.M.; Park, H.J. Validation in the Cross-Cultural Adaptation of the Korean Version of the Oswestry Disability Index. J. Korean Med. Sci. 2006, 21, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Shim, S.Y.; Park, H.J.; Lee, J.M.; Lee, H.S. An Overview of Pain Measurements [Korean]. Korean J. Acupunct. 2007, 24, 77–97. [Google Scholar]
- Kim, T.H. Validity and Reliability Evaluation for EQ-5D in the General Population of South Korea. Ph.D. Thesis, University of Ulsan the Graduate School, Ulsan, Republic of Korea, 2012. [Google Scholar]
- Park, G.S. Validation of the Korean Versions of the Short-Form McGill Pain Questionnaire (SF-MPQ) and Neuropathic Pain Scale (NPS) in Neuropathic Pain Patients. Ph.D. Thesis, Seoul National University College of Medicine, Seoul, Republic of Korea, 2015. [Google Scholar]
- Lee, J.S.; Lee, D.H.; Suh, K.T.; Kim, J.I.; Lim, J.M.; Goh, T.S. Validation of the Korean Version of the Roland-Morris Disability Questionnaire. Eur. Spine J. 2011, 20, 2115–2119. [Google Scholar] [CrossRef]
- Maughan, E.F.; Lewis, J.S. Outcome measures in chronic low back pain. Eur. Spine J. 2010, 19, 1484–1494. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Yoon, J.; Kim, Y.; Oh, D.; Kim, S.J.; Ahn, J.; Suh, G.Y.; Nam, S.J.; Mitchell, S.A. Linguistic Validation of the US National Cancer Institute’s Patient-Reported Outcomes Version of the Common Terminology Criteria for Adverse Events in Korean. J. Glob. Oncol. 2019, 5, 1–10. [Google Scholar] [CrossRef]
- Jo, M.W.; Ahn, J.H.; Kim, S.H.; Shin, S.J.; Park, J.Y.; Ock, M.S.; Son, W.S.; Kim, S.O. The Valuation of EQ-5D-5L Health States in Korea; National Evidence-Based Healthcare Collaborating Agency: Seoul, Republic of Korea, 2013. [Google Scholar]
- Lim, J.H.; Lim, S.M. A Literature Study on Usage of and Satisfaction Levels with Combined Treatment Including Oriental and Western Medicine. J. Pharmacopunct. 2012, 15, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Fei, W. A Study on Collaborative Medical Care System of Korean Medicine and Western Medicine. Chung-Ang J. Legal Stud. 2021, 45, 207–242. [Google Scholar] [CrossRef]
- Jiang, L.L.; Zhang, B.Y.; Yu, H.L. Analysis on Adverse Event in Acupotomy Therapy Based on Literature Research. Zhongguo Zhen Jiu 2018, 38, 1007–1012. [Google Scholar] [PubMed]
- Yoon, S.H.; Kwon, C.Y.; Jo, H.G.; Sul, J.U.; Lee, H.; Won, J.; Jeong, S.J.; Lee, J.H.; Leem, J. Safety of Acupotomy in a Real-world Setting: A Prospective Pilot and Feasibility Study. J. Integr. Med. 2022, 20, 514–523. [Google Scholar] [CrossRef]
- Gao, C.Y.; Wang, B.J.; Jin, Z.F.; Yang, K.X.; Sun, W.; Wi, X.; Feng, M.S.; Yin, H.; Yin, X.L.; Ye, Y.Y. Clinical Study on the Treatment of Lumbar Disc Herniation by Acupotomy and Nerve Root Block. J. Basic Chin. Med. 2020, 26, 369–371. [Google Scholar]
- Gui, X.X.; Ou, Y.G.; Xiao, J.H. Observation of Nerve Block Combined with Acupotomy Surgery for the Treatment of Spinal Nerve Syndrome. J. Cervicodynia Lumbodynia 2017, 38, 153–156. [Google Scholar]
- Kim, S.Y.; Lee, H.; Chae, Y.; Park, H.J.; Lee, H. A Systematic Review of Cost-Effectiveness Analyses Alongside Randomised Controlled Trials of Acupuncture. Acupunct. Med. 2012, 30, 273–285. [Google Scholar] [CrossRef] [PubMed]
| ESI Single-Treatment Group | DAH + ESI Treatment Group | p-Value | |
|---|---|---|---|
| Sample size (n) | 25 | 25 | |
| Age (years) a | 63.2 ± 10.7 | 60.8 ± 13.1 | 0.4749 |
| Sex (n) b | |||
| Male | 13 (52) | 8 (32) | 0.1520 |
| Female | 12 (48) | 17 (68) | |
| Height (cm) a | 161.3 ± 8.6 | 159.4 ± 9.4 | 0.4573 |
| Body weight (kg) a | 64.9 ± 12.1 | 62.9 ± 14.8 | 0.5995 |
| BMI (kg/m2) a | 24.8 ± 3.8 | 24.4 ± 3.6 | 0.6902 |
| SBP (mmHg) a | 128.9 ± 15.6 | 131.2 ± 10.0 | 0.5419 |
| DBP (mmHg) a | 69.3 ± 14.8 | 74.9 ± 7.4 | 0.0996 |
| Pathology (n) c | |||
| Spinal stenosis | 11 (44) | 6 (24) | 0.4100 |
| Intervertebral disc disorder | 11 (44) | 14 (56) | |
| Others | 3 (12) | 5 (20) | |
| Duration of pain (days) | 255.0 (93.0, 949.0) | 106.0 (57.0, 454.0) | 0.2274 |
| Type of ESI—first (n) c | |||
| Caudal block | 4 (16) | 5 (20) | 1.0000 |
| Interlaminar approach | 21 (84) | 20 (80) | |
| Type of ESI—second (n) c | |||
| Caudal block | 6 (24) | 5 (20.83) | 0.7906 |
| Interlaminar approach | 19 (76) | 19 (79.17) |
| Outcomes | Changes from Baseline | |||||
|---|---|---|---|---|---|---|
| ESI Single-Treatment Group (n = 25) | DAH + ESI Treatment Group (n = 25) | p-Value | ESI Single-Treatment Group (n = 25) | DAH + ESI Treatment Group (n = 25) | p-Value c | |
| ODI score | ||||||
| Baseline | 27.64 (25.61, 29.67) | 29.24 (26.46, 32.02) | 0.3418 | |||
| Week 4 | 25.48 (22.17, 28.79) | 19.80 (16.62, 22.98) | 0.0139 a | −2.16 (−5.01, 0.69) | −9.44 (−12.71, −6.17) | 0.0021 b |
| Week 8 | 22.88 (19.66, 26.10) | 20.20 (17.74, 22.66) | 0.1791 | −4.76 (−7.68, −1.84) | −9.04 (−12.09, −5.99) | 0.0751 |
| NRS (back pain) | ||||||
| Baseline | 6.08 (5.13, 7.03) | 6.80 (5.71, 7.89) | 0.3087 | |||
| Week 4 | 5.28 (4.09, 6.47) | 4.16 (3.10, 5.22) | 0.1549 | −0.80 (−2.35, 0.75) | −2.64 (−3.85, −1.43) | 0.1144 |
| Week 8 | 5.12 (4.13, 6.11) | 4.20 (3.22, 5.18) | 0.1787 | −0.96 (−2.08, 0.16) | −2.60 (−3.70, −1.50) | 0.0673 |
| NRS (lower limb pain) | ||||||
| Baseline | 7.84 (7.06, 8.62) | 8.28 (7.74, 8.82) | 0.3425 | |||
| Week 4 | 6.04 (5.05, 7.03) | 5.04 (3.83, 6.25) | 0.1928 | −1.80 (−2.50, −1.10) | −3.24 (−4.60, −1.88) | 0.0942 |
| Week 8 | 5.48 (4.44, 6.52) | 4.80 (3.85, 5.75) | 0.3230 | −2.36 (−3.19, −1.53) | −3.48 (−4.62, −2.34) | 0.1776 |
| EQ-5D | ||||||
| Baseline | 0.63 (0.57, 0.69) | 0.58 (0.51, 0.65) | 0.2695 | |||
| Week 4 | 0.67 (0.60, 0.74) | 0.77 (0.70, 0.84) | 0.0210 a | 0.04 (−0.04, 0.11) | 0.19 (0.10, 0.28) | 0.0161 a |
| Week 8 | 0.71 (0.64, 0.78) | 0.78 (0.72, 0.83) | 0.0658 | 0.08 (0.02, 0.15) | 0.20 (0.12, 0.28) | 0.0511 |
| MPQ total score | ||||||
| Baseline | 26.44 (23.92, 28.96) | 27.12 (24.65, 29.59) | 0.6922 | |||
| Week 4 | 22.96 (19.49, 26.43) | 20.71 (18.23, 23.18) | 0.2808 | −2.92 (−5.44, −0.39) | −6.13 (−8.69, −3.56) | 0.0910 |
| Week 8 | 21.54 (18.97, 24.12) | 19.71 (17.75, 21.67) | 0.2476 | −4.33 (−6.40, −2.27) | −7.13 (−9.34, −4.91) | 0.0726 |
| MPQ (sense) | ||||||
| Baseline | 19.04 (17.12, 20.96) | 19.28 (17.62, 20.94) | 0.8461 | |||
| Week 4 | 17.17 (14.58, 19.75) | 15.38 (13.7, 17.05) | 0.2352 | −1.42 (−3.11, 0.28) | −3.71 (−5.26, −2.16) | 0.0520 |
| Week 8 | 16.33 (14.45, 18.22) | 14.79 (13.36, 16.22) | 0.1840 | −2.25 (−3.86, −0.64) | −4.29 (−5.62, −2.97) | 0.0477 a |
| MPQ (emotion) | ||||||
| Baseline | 7.40 (6.40, 8.40) | 7.84 (6.8, 8.88) | 0.5308 | |||
| Week 4 | 5.79 (4.83, 6.76) | 5.33 (4.39, 6.28) | 0.4862 | −1.50 (−2.64, −0.36) | −2.42 (−3.56, −1.28) | 0.3354 |
| Week 8 | 5.21 (4.40, 6.02) | 4.92 (4.19, 5.64) | 0.5808 | −2.08 (−3.06, −1.11) | −2.83 (−3.89, −1.77) | 0.3876 |
| MPQ (VAS) | ||||||
| Baseline | 8.21 (7.55, 8.87) | 8.40 (7.82, 8.98) | 0.6541 | |||
| Week 4 | 6.21 (5.24, 7.17) | 5.08 (4.13, 6.04) | 0.0933 | −1.74 (−2.62, −0.86) | −3.29 (−4.40, −2.18) | 0.0388 a |
| Week 8 | 5.48 (4.60, 6.35) | 4.54 (3.75, 5.33) | 0.1053 | −2.32 (−3.06, −1.58) | −3.83 (−4.83, −2.83) | 0.0257 a |
| MPQ (present pain intensity) | ||||||
| Baseline | 3.88 (3.63, 4.13) | 3.96 (3.61, 4.31) | 0.7002 | |||
| Week 4 | 3.13 (2.65, 3.60) | 2.46 (2.03, 2.89) | 0.0360 a | −0.71 (−1.13, −0.29) | −1.54 (−2.04, −1.04) | 0.0172 a |
| Week 8 | 2.83 (2.43, 3.24) | 2.33 (2.01, 2.65) | 0.0520 | −1.00 (−1.41, −0.59) | −1.67 (−2.11, −1.22) | 0.0372 a |
| RMDQ | ||||||
| Baseline | 11.12 (9.03, 13.21) | 12.24 (9.59, 14.89) | 0.4963 | |||
| Week 4 | 9.04 (6.65, 11.43) | 6.62 (3.42, 9.81) | 0.2070 | −1.54 (−4.05, 0.97) | −6.33 (−8.73, −3.93) | 0.0207 a |
| Week 8 | 6.74 (4.90, 8.57) | 5.84 (3.39, 8.29) | 0.5364 | −4.04 (−6.44, −1.64) | −7.32 (−9.88, −4.76) | 0.1939 |
| ESI Single-Treatment Group | DAH + ESI Treatment Group | Increment | |
|---|---|---|---|
| Cost (Won) | 978,817 | 788,467 | −190,350 |
| QALYs | 0.10271 | 0.11313 | 0.01042 |
| ICUR (Won/QALYs) | −18,267,754 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Lee, S.-H.; Suh, H.S.; Hwang, M.-S.; Jang, S.; Choi, S.; Lim, Y.-S.; Byun, S.H.; Yoon, S.-H.; Park, S.; et al. Effectiveness of Acupotomy Combined with Epidural Steroid Injection for Lumbosacral Radiculopathy: A Randomized Controlled Pragmatic Pilot Study. Medicina 2024, 60, 175. https://doi.org/10.3390/medicina60010175
Lee J-H, Lee S-H, Suh HS, Hwang M-S, Jang S, Choi S, Lim Y-S, Byun SH, Yoon S-H, Park S, et al. Effectiveness of Acupotomy Combined with Epidural Steroid Injection for Lumbosacral Radiculopathy: A Randomized Controlled Pragmatic Pilot Study. Medicina. 2024; 60(1):175. https://doi.org/10.3390/medicina60010175
Chicago/Turabian StyleLee, Jin-Hyun, Sang-Hyun Lee, Hae Sun Suh, Man-Suk Hwang, Semin Jang, Sooil Choi, Young-Soo Lim, Sang Hyun Byun, Sang-Hoon Yoon, Sukhee Park, and et al. 2024. "Effectiveness of Acupotomy Combined with Epidural Steroid Injection for Lumbosacral Radiculopathy: A Randomized Controlled Pragmatic Pilot Study" Medicina 60, no. 1: 175. https://doi.org/10.3390/medicina60010175
APA StyleLee, J.-H., Lee, S.-H., Suh, H. S., Hwang, M.-S., Jang, S., Choi, S., Lim, Y.-S., Byun, S. H., Yoon, S.-H., Park, S., & Park, T.-Y. (2024). Effectiveness of Acupotomy Combined with Epidural Steroid Injection for Lumbosacral Radiculopathy: A Randomized Controlled Pragmatic Pilot Study. Medicina, 60(1), 175. https://doi.org/10.3390/medicina60010175







