Prevalence of Malocclusions in Down Syndrome Population: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measures
- −
- malocclusion: the type of malocclusion was assessed by recording the molar class relationship based on Angle’s classification of malocclusion, and classified in Angle’s Class 1, Class 2 or Class 3 malocclusion [19].
- −
- maxillary transverse discrepancy: this was evaluated by evaluating the form, symmetry of the maxillary arch, palatal vault shape, predominant breathing mode (i.e., oral or nasal) and buccal corridor width when smiling [20]. The palatal transverse discrepancy was classified as posterior crossbite when the buccal cusps of the upper molars were in contact with the central fossae of the lower molars [21]. It was classified as scissor bite in the presence of a posterior discrepancy with or without contact between the palatal surface of the upper lingual cusp and the buccal surface of the lower buccal cusp [22].
- −
- sagittal discrepancy: anterior crossbite was defined as the presence of a negative horizontal overlap between upper and lower incisors, measured from the facial surface of the upper incisors to the middle of the incisal edge of the lower incisors [23].
- −
- dental crowding: this was measured using the Little’s irregularity index, a tool to estimate the difference between available and required space [24].
- −
- vertical discrepancy: the amount of vertical overlapping of upper and lower incisors was calculated, considering a value of 4 mm as the cut-off for presence of anterior deep bite [25]. Conversely, anterior open bite was defined as the presence of a negative vertical overlapping between upper and lower incisors [23].
- −
- facial profile: the patient’s profile was classified as concave, straight and convex based on the definition provided by Arnett and Bergman [26].
- −
- Finally, the presence of probable sleep bruxism was ascertained according to the grading system proposed by the international consensus [27]. As such, a positive response was assigned based on patient/guardian report and on the presence of at least one clinical sign (e.g., masticatory muscle hypertrophy, buccal linea alba, indentations on the tongue or lip, tooth wear) [27].
2.4. Statistical Analysis
3. Results
3.1. Children Population (<10 y.o.)
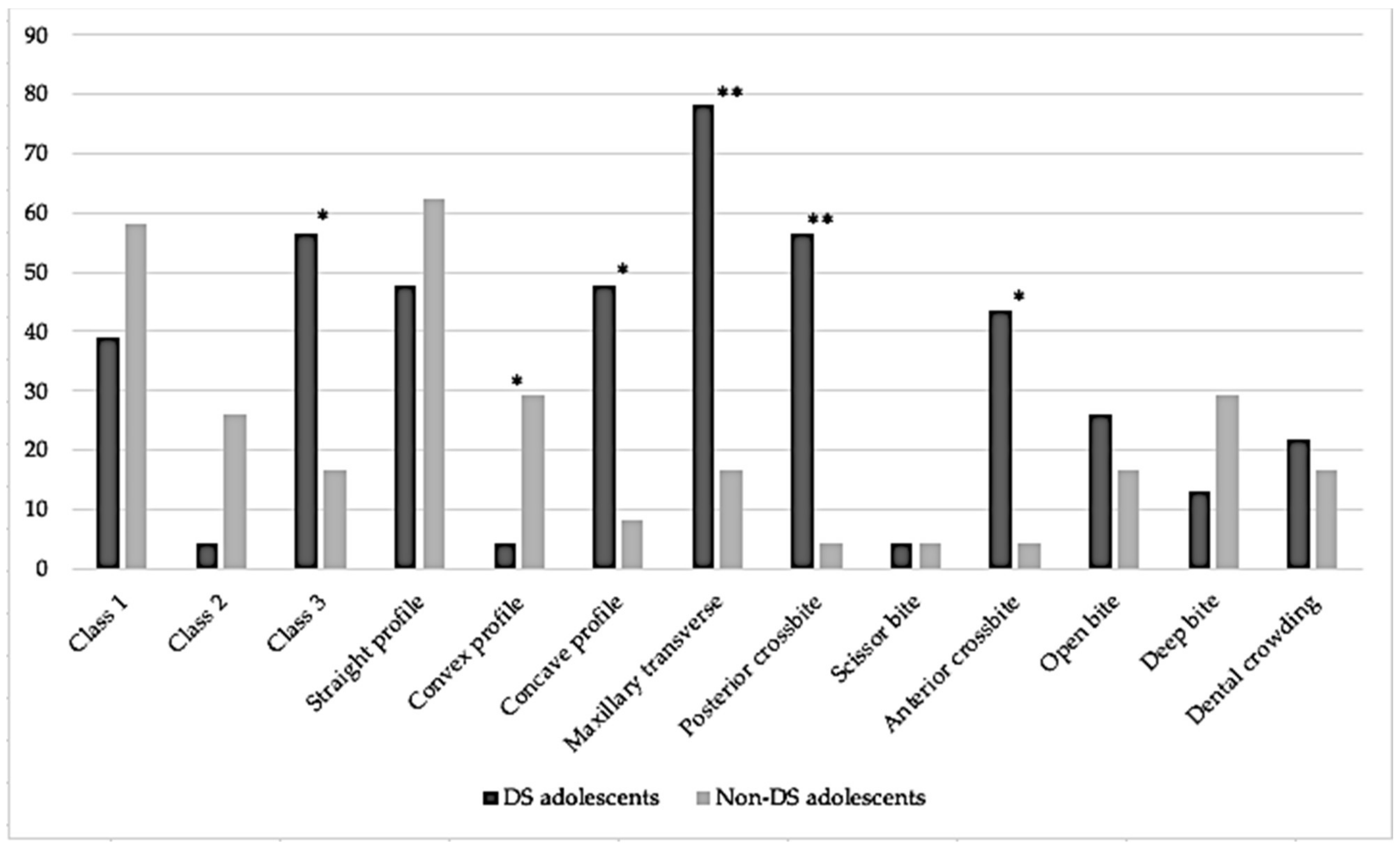
3.2. Adolescent Population (10–17 y.o.)
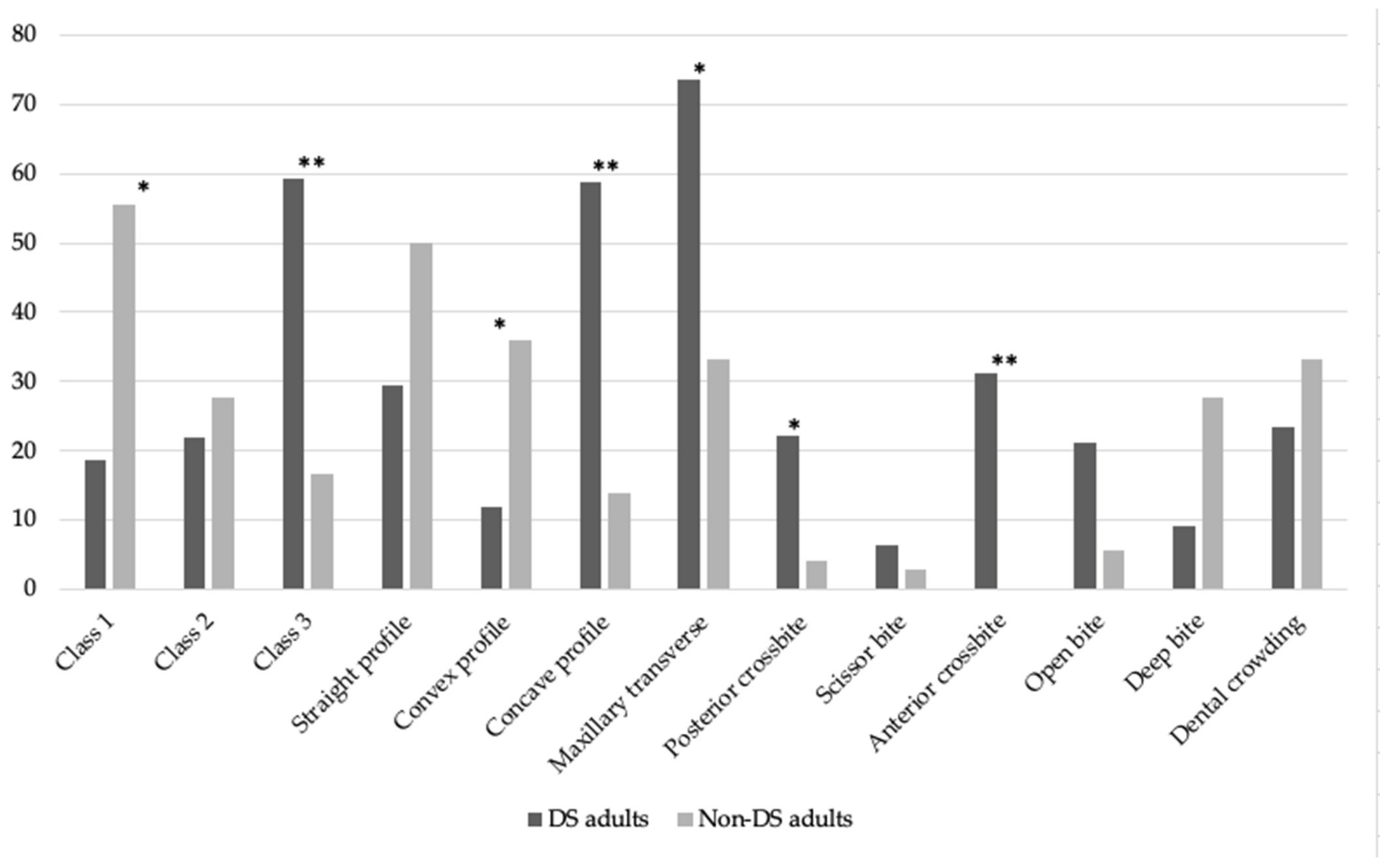
3.3. Adult Population (≥18 y.o.)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bull, M.J. Down Syndrome. N. Eng. J. Med. 2020, 382, 2344–2352. [Google Scholar] [CrossRef] [PubMed]
- Baburamani, A.A.; Patkee, P.A.; Arichi, T.; Rutherford, M.A. New approaches to studying early brain development in Down syndrome. Dev. Med. Child Neurol. 2019, 61, 867–879. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Quevedo, A.A.; Cstillo-Quispe, H.M.L.; Atoche-Socola, K.J.; Arriola-Guillén, L.E. Evaluation of the craniofacial and oral characteristics of individuals with Down syndrome: A review of the literature. Stomatol. Oral Maxillofac. Surg. 2021, 122, 583–587. [Google Scholar] [CrossRef] [PubMed]
- Valentini, D.; Di Camillo, C.; Mirante, N.; Vallogini, G.; Olivini, N.; Baban, A.; Buzzonetti, L.; Galeotti, A.; Raponi, M.; Villani, A. Medical conditions of children and young people with Down syndrome. J. Intellect. Disabil. Res. 2021, 65, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Schieve, L.; Boulet, S.; Boyle, C.; Rasmussen, S.; Schendel, D. Health of children 3 to 17 years of age with Down syndrome in the 1997–2005 National Health Interview Survey. Pediatrics 2009, 123, e253–e260. [Google Scholar] [CrossRef] [PubMed]
- Weijerman, M.E.; De Winter, J.P. Clinical practice: The care of children with Down syndrome. Eur. J. Pediatr. 2010, 169, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Bull, M.J.; Committee on Genetics. Clinical report—Health supervision for children with Down syndrome. Pediatrics 2011, 128, 393–406. [Google Scholar] [CrossRef]
- AL Ayoubi, A.; Madléna, M. Upper Airway Characteristics in Young Individuals with Class II Division 1 Malocclusion: A Retrospective Inter-Ethnic Cephalometric Comparison. J. Craniofacial Surg. 2021, 32, e761–e763. [Google Scholar] [CrossRef]
- Amr, N.H. Thyroid Disorders in Subjects with Down Syndrome: An Update. Acta Biomed. 2018, 89, 132–139. [Google Scholar]
- Vicente, A.; Bravo-Gonzáles, L.A.; López-Romero, A.; Munoz, C.S.; Sánchez-Meca, J. Craniofacial morphology in down syndrome: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 19895. [Google Scholar] [CrossRef]
- Lombardo, G.; Vena, F.; Negri, P.; Pagano, S.; Barilotti, C.; Paglia, L.; Colombo, S.; Orso, M.; Cianetti, S. Worldwide prevalence of malocclusion in the different stages of dentition: A systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020, 21, 115–122. [Google Scholar] [PubMed]
- Góis, E.G.; Vale, M.P.; Paiva, S.M.; Abreu, M.H.; Serra-Negra, J.M.; Pordeus, I.A. Incidence of malocclusion between primary and mixed dentitions among Brazilian children. A 5-year longitudinal study. Angle Orthod. 2012, 82, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Arora, A.; Valiathan, A. Age changes of jaws and soft tissue profile. Sci. World J. 2014, 2014, 301501. [Google Scholar] [CrossRef] [PubMed]
- Saheed, A. A comparative study of oral health amongst trisomy 21 children living in Riyadh, Saudi Arabia: Part 1 caries, malocclusion, trauma. Saudi Dent. J. 2015, 27, 220–223. [Google Scholar]
- De Ridder, L.; Aleksieva, A.; Willems, G.; Declerck, D.; de Cllano-Pérula, M.C. Prevalence of Orthodontic Malocclusions in Healthy Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7446. [Google Scholar] [CrossRef]
- Alexander, A.E.; McNamara, J.J.; Franchi, L.; Baccetti, T. Semilongitudinal cephalometric study of craniofacial growth in untreated Class III malocclusion. J. Orthod. Dentofac. Orthop. 2009, 135, 700.e1–700.e14. [Google Scholar] [CrossRef]
- Love, R.J.; Murray, J.M.; Mamandras, A.H. Facial growth in males 16 to 20 years of age. J. Orthod. Dentofac. Orthop. 1990, 97, 200–206. [Google Scholar] [CrossRef]
- Currie, K.; Sawchuk, D.; Saltaji, H.; Oh, H.; Flores-Mir, C.; Lagravere, M. Posterior cranial base natural growth and development: A systematic review. Angle Orthod. 2017, 676, 897–910. [Google Scholar] [CrossRef]
- Graber, L.W.; Vanarsdall, R.L.; Vig, K.W.L.; Huang, G.J. Orthodontics: Current Principles and Techniques, 6th ed.; Elsevier: St. Louis, MI, USA, 2017. [Google Scholar]
- Dakhil, N.B.; Salamah, F.B. The diagnosis methods and management modalities of maxillary transverse discrepancy. Cureus 2021, 13, e20482. [Google Scholar] [CrossRef]
- Mutinelli, S.; Cozzani, M. Rapid maxillary expansion in early-mixed dentition: Effectiveness of increasing arch dimension with anchorage on deciduous teeth. Eur. J. Paediatr. Dent. 2015, 16, 115–122. [Google Scholar]
- King, J.W.; Wallace, J.C. Unilateral Brodie bite treatment with distraction osteogenesis. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 500–509. [Google Scholar] [CrossRef]
- Borrie, F.; Bearn, D. Early correction of anterior crossbites: A systematic review. J. Orthod. 2011, 38, 175–184. [Google Scholar] [CrossRef]
- Little, R.M. The irregularity index: A quantitative score of mandibular anterior alignment. Am. J. Orthod. 1975, 68, 554–563. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.J.; Bates, S.B.; Ehlert, A.A.; Whiting, D.P.; Chen, S.S.; Bollen, A.M. Stability of deep-bite correction: A systematic review. J. World Fed. Orthod. 2012, 1, e89–e96. [Google Scholar] [CrossRef] [PubMed]
- Arnett, G.W.; Jelic, J.S.; Kim, J.; Cummings, D.R.; Beress, A.; Worley, C.M., Jr.; Chung, B.; Bergman, R.T. Soft tissue cephalometric analysis: Diagnosis and treatment planning of dentofacial deformity. J. Orthod. Dentofac. Orthop. 1999, 116, 239–253. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Y.; Yang, Y.; Zhang, L.; Hong, Z.; Ji, W.; Zhang, L. Clinical effects of maxillary protraction in different stages of dentition in skeletal class III children: A systematic review and meta-analysis. Orthod. Craniofacial Res. 2022, 25, 549–561. [Google Scholar] [CrossRef]
- Khda, M.; Likiaridis, S.; Antonarakis, G.S. Spontaneous correction and new development of posterior crossbite from the deciduous to the mixed dentition. Eur. J. Orthod. 2022, 7, cjac061. [Google Scholar] [CrossRef]
- Lee, C.F.; Lee, C.H.; Hsueh, W.Y.; Lin, M.T.; Kang, K.T. Prevalence of Obstructive Sleep Apnea in Children with Down Syndrome: A Meta-Analysis. J. Clin. Sleep Med. 2018, 14, 867–875. [Google Scholar] [CrossRef]
- de Miguel-Díez, J.; Villa-Asensi, J.; Alvarez-Sala, J.L. Prevalence of sleep-disordered breathing in children with Down syndrome: Polygraphic findings in 108 children. Sleep 2003, 26, 1006–1009. [Google Scholar] [CrossRef]
- Ohlmann, B.; Rathmann, F.; Bomickle, W.; Behnisch, R.; Rammelsberg, P.; Schmitter, M. Validity of patient self-reports and clinical signs in the assessment of sleep burxims based on home-recorded electromyographic/electrocardiographic data. J. Oral Rehabil. 2022, 49, 720–728. [Google Scholar] [CrossRef]
- Luconi, E.; Togni, L.; Mascitti, M.; Tesei, A.; Nori, A.; Barlattani, A.; Procaccini, M.; Santarelli, A. Bruxism in Children and Adolescents with Down Syndrome: A Comprehensive Review. Medicina 2021, 57, 224. [Google Scholar] [CrossRef]
- El-Attar, L.M.; Bahashwan, A.A.; Bakhsh, A.D.; Moshrif, Y.M. The prevalence and patterns of chromosome abnormalities in newborns with major congenital anomalies: A retrospective study from Saudi Arabia. Intractable Rare Dis. Res. 2021, 10, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press J. Orthod. 2019, 23, 40.e1–40.e10, Erratum in: Dent. Press J. Orthod. 2019, 24, 113. [Google Scholar] [CrossRef] [PubMed]
- Doriguêtto, P.V.T.; Carrada, C.F.; Scalioni, F.A.R.; Abreu, L.G.; Devito, K.L.; Paiva, S.M.; Ribeiro, R.A. Malocclusion in children and adolescents with Down syndrome: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2019, 29, 524–541. [Google Scholar] [CrossRef]
- Oliveira, A.C.; Paiva, S.M.; Campos, M.R.; Czeresnia, D. Factors associated with malocclusions in children and adolescents with Down syndrome. J. Orthod. Dentofac. Orthop. 2008, 133, 489.e1–489.e8. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.nih.gov/nih-style-guide/age (accessed on 1 September 2023).
- Available online: https://www.statcan.gc.ca/en/concepts/definitions/age2 (accessed on 1 September 2023).
- Naggara, O.; Raymond, J.; Guilbert, F.; Roy, D.; Weill, A.; Altman, D.G. Analysis by categorizing or dichotomizing continuous variables is inadvisable: An example from the natural history of unruptured aneurysms. AJNR Am. J. Neuroradiol. 2011, 32, 437–440. [Google Scholar] [CrossRef]
- Ramón, R.; Adanero, A.; Miegimolle, M. A new approach to diagnosis to posterior cross bite: Intraoral phtography and wala ridge. Int. J. Environ. Res. Public Health 2022, 19, 9443. [Google Scholar] [CrossRef]
- Hassan, A.H.; AlGhamdi, A.T.; Al-Fraidi, A.A.; Al-Hubail, A.; Hajrassy, M.K. Unilateral cross bite treated by corticotomy-assisted expansion: Two case reports. Head Face Med. 2010, 6, 6. [Google Scholar] [CrossRef]
- Suri, S.; Tompson, B.D.; Cornfoot, L. Cranial base, maxillary and mandibular morphology in Down syndrome. Angle Orthod. 2010, 80, 861–869. [Google Scholar] [CrossRef]
- Fink, G.B.; Madaus, W.K.; Walker, G.F. A quantitative study of the face in Down’s syndrome. Am. J. Orthod. 1975, 67, 540–553. [Google Scholar] [CrossRef]
- Guimaraes, C.V.; Donnelly, L.F.; Shott, S.R.; Amin, R.S.; Kalra, M. Relative rather than absolute macroglossia in patients with Down syndrome: Implications for treatment of obstructive sleep apnea. Pediatr. Radiol. 2008, 38, 1062–1067. [Google Scholar] [CrossRef] [PubMed]
- Grippaudo, C.; Paolantonio, E.G.; Antonini, G.; Saulle, R.; La Torre, G.; Deli, R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol. Ital. 2016, 36, 386–394. [Google Scholar] [CrossRef]
- Abate, A.; Cavagnetto, D.; Fama, A.; Maspero, C.; Farronato, G. Relationship between breastfeeding and malocclusion: A systematic review of the literature. Nutrients 2020, 12, 3688. [Google Scholar] [CrossRef] [PubMed]
- Moimaz, S.A.; Garbin, A.J.; Lima, A.M.; Lolli, L.F.; Saliba, O.; Garbin, C.A. Longitudinal study of habits leading to malocclusion development in childhood. BMC Oral Health 2014, 14, 96. [Google Scholar] [CrossRef] [PubMed]
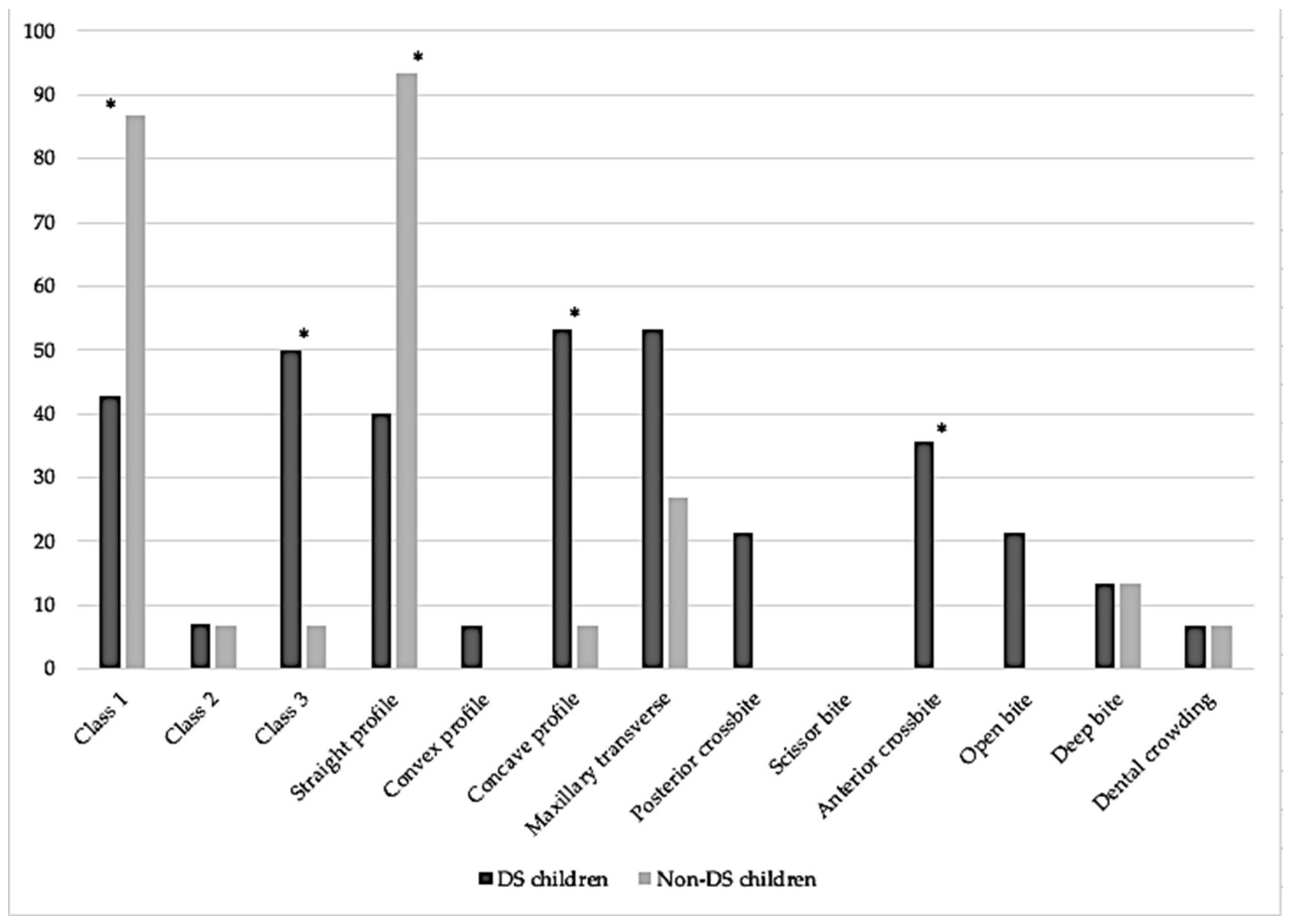
| DS Children (N = 15) | Non-DS Children (N = 15) | p Value | |
|---|---|---|---|
| Age (years) | 6.7 ± 2.0 | 7.0 ± 1.3 | |
| Male/female, N | 12/3 | 12/3 | |
| Angle’s malocclusion | |||
| Angle’s Class 1 | 42.9% | 86.7% | 0.021 * |
| Angle’s Class 2 | 7.1% | 6.7% | 0.742 |
| Angle’s Class 3 | 50.0% | 6.7% | 0.014 * |
| Facial profile | |||
| Straight | 40.0% | 93.3% | 0.005 * |
| Convex | 6.7% | 0.0% | 0.500 |
| Concave | 53.3% | 6.7% | 0.014 * |
| Tranverse discrepancy | |||
| Maxillary transverse discrepancy | 53.3% | 26.7% | 0.264 |
| Posterior crossbite | 21.4% | 0.0% | 0.100 |
| Scissor bite | 0.0% | 0.0% | 1.000 |
| Sagittal discrepancy | |||
| Anterior crossbite | 35.7% | 0.0% | 0.017 * |
| Vertical discrepancy | |||
| Open bite | 21.4% | 0.0% | 0.100 |
| Deep bite | 13.3% | 13.3% | 1.000 |
| Dental crowding | 6.7% | 6.7% | 1.000 |
| Probable sleep bruxism | 60.0% | 33.3% | 0.272 |
| DS Adolescents (N = 23) | Non-DS Adolescents (N = 24) | p Value | |
|---|---|---|---|
| Age (years) | 13.1 ± 2.3 | 13.2 ± 1.9 | |
| Male/female, N | 11/12 | 13/11 | |
| Angle’s malocclusion | |||
| Angle’s Class 1 | 39.1% | 58.3% | 0.248 |
| Angle’s Class 2 | 4.3% | 26.0% | 0.097 |
| Angle’s Class 3 | 56.6% | 16.7% | 0.006 * |
| Facial profile | |||
| Straight | 47.8% | 62.5% | 0.385 |
| Convex | 4.3% | 29.2% | 0.048 * |
| Concave | 47.8% | 8.3% | 0.003 * |
| Transverse discrepancy | |||
| Maxillary transverse discrepancy | 78.3% | 16.7% | <0.001 * |
| Posterior crossbite | 56.5% | 4.2% | <0.001 * |
| Scissor bite | 4.3% | 4.2% | 1.000 |
| Sagittal discrepancy | |||
| Anterior crossbite | 43.5% | 4.2% | 0.002 * |
| Vertical discrepancy | |||
| Open bite | 26.1% | 16.7% | 0.494 |
| Deep bite | 13.0% | 29.2% | 0.286 |
| Dental crowding | 21.7% | 16.7% | 0.724 |
| Probable sleep bruxism | 43.5% | 16.7% | 0.060 |
| DS Adults (N = 34) | Non-DS Adults (N = 36) | p Value | |
|---|---|---|---|
| Age (years) | 28.1 ± 9.0 | 28.3 ± 9.0 | |
| Male/female, N | 23/11 | 20/16 | |
| Angle’s malocclusion | |||
| Angle’s Class 1 | 18.8% | 55.6% | 0.003 * |
| Angle’s Class 2 | 21.9% | 27.8% | 0.780 |
| Angle’s Class 3 | 59.4% | 16.7% | <0.001 * |
| Facial profile | |||
| Straight | 29.4% | 50.% | 0.093 |
| Convex | 11.8% | 36.1% | 0.025 * |
| Concave | 58.8% | 13.9% | <0.001 * |
| Transverse discrepancy | |||
| Maxillary transverse discrepancy | 73.5% | 33.3% | 0.001 * |
| Posterior crossbite | 22.2% | 4.2% | 0.001 * |
| Scissor bite | 6.3% | 2.8% | 0.598 |
| Sagittal discrepancy | |||
| Anterior crossbite | 31.3% | 0.0% | <0.001 * |
| Vertical discrepancy | |||
| Open bite | 21.2% | 5.6% | 0.076 |
| Deep bite | 9.1% | 27.8% | 0.066 |
| Dental crowding | 23.5% | 33.3% | 0.433 |
| Probable sleep bruxism | 60.6% | 22.2% | 0.002 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alessandri-Bonetti, A.; Guglielmi, F.; Mollo, A.; Sangalli, L.; Gallenzi, P. Prevalence of Malocclusions in Down Syndrome Population: A Cross-Sectional Study. Medicina 2023, 59, 1657. https://doi.org/10.3390/medicina59091657
Alessandri-Bonetti A, Guglielmi F, Mollo A, Sangalli L, Gallenzi P. Prevalence of Malocclusions in Down Syndrome Population: A Cross-Sectional Study. Medicina. 2023; 59(9):1657. https://doi.org/10.3390/medicina59091657
Chicago/Turabian StyleAlessandri-Bonetti, Anna, Federica Guglielmi, Antongiulia Mollo, Linda Sangalli, and Patrizia Gallenzi. 2023. "Prevalence of Malocclusions in Down Syndrome Population: A Cross-Sectional Study" Medicina 59, no. 9: 1657. https://doi.org/10.3390/medicina59091657
APA StyleAlessandri-Bonetti, A., Guglielmi, F., Mollo, A., Sangalli, L., & Gallenzi, P. (2023). Prevalence of Malocclusions in Down Syndrome Population: A Cross-Sectional Study. Medicina, 59(9), 1657. https://doi.org/10.3390/medicina59091657







