Expanding the Minimally Invasive Approach towards the Ascending Aorta—A Practical Overview of the Currently Available Techniques
Abstract
:1. Introduction
2. Patient Selection
3. Preoperative Diagnostics and Planning
4. Operative Techniques
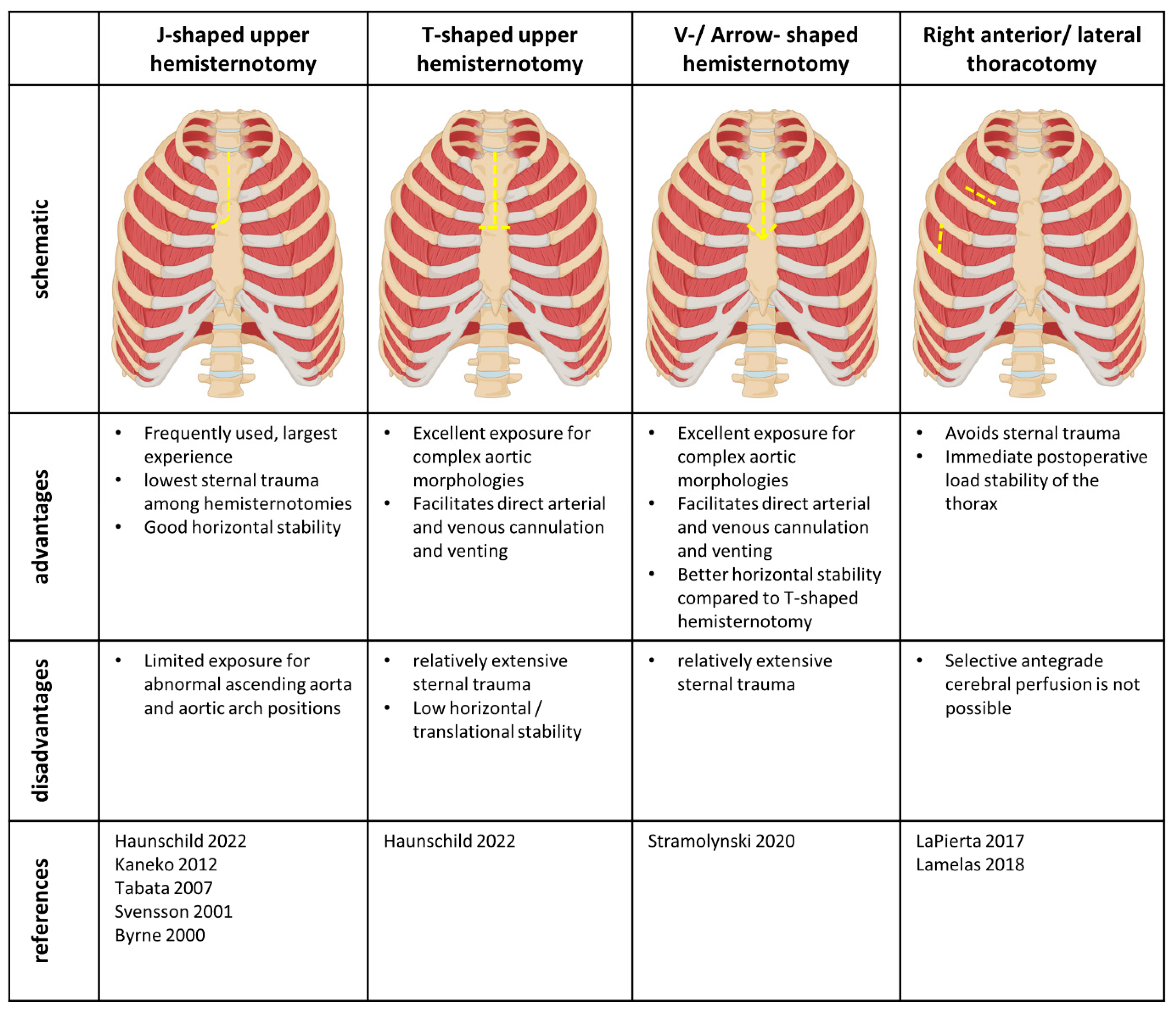
4.1. Access Sides
4.2. Cannulation
4.3. Venting and Cross-Clamping
4.4. Myocardial and Cerebral Protection
5. Outcome
6. Limitations
7. Conclusions and Future Perspective
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Iribarne, A.; Easterwood, R.M.; Chan, E.Y.; Yang, J.; Soni, L.; Russo, M.J.; Smith, C.R.; Argenziano, M.; Bostock, I.C.; Nammalwar, S.; et al. The golden age of minimally invasive cardiothoracic surgery: Current and future perspectives. Future Cardiol. 2011, 7, 333–346. [Google Scholar] [CrossRef]
- Monsefi, N.; Risteski, P.; Miskovic, A.; Moritz, A.; Zierer, A. Midterm Results of a Minimally Invasive Approach in David Procedure. Thorac. Cardiovasc. Surg. 2018, 66, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Jahangiri, M.; Hussain, A.; Akowuah, E. Minimally invasive surgical aortic valve replacement. Heart 2019, 105 (Suppl. 2), s10–s15. [Google Scholar] [CrossRef] [PubMed]
- Abu-Omar, Y.; Fazmin, I.T.; Ali, J.M.; Pelletier, M.P. Minimally invasive mitral valve surgery. J. Thorac. Dis. 2021, 13, 1960–1970. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Zheng, J.; Chang, Q.; Tang, Y.; Feng, J.; Sun, X.; Zhu, X. Aortic root replacement by ministernotomy: Technique and potential benefit. Ann. Thorac. Surg. 2000, 70, 1958–1961. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, M.; Kaufeld, T.; Shrestha, P.; Martens, A.; Rustum, S.; Rudolph, L.; Krüger, H.; Arar, M.; Haverich, A.; Beckmann, E. Valve-sparing David procedure via minimally invasive access does not compromise outcome. Front. Cardiovasc. Med. 2022, 9, 966126. [Google Scholar] [CrossRef]
- Staromłyński, J.; Kowalewski, M.; Sarnowski, W.; Smoczyński, R.; Witkowska, A.; Bartczak, M.; Drobiński, D.; Wierzba, W.; Suwalski, P. Midterm results of less invasive approach to ascending aorta and aortic root surgery. J. Thorac. Dis. 2020, 12, 6446–6457. [Google Scholar] [CrossRef]
- Byrne, J.G.; Karavas, A.N.; Cohn, L.H.; Adams, D.H. Minimal access aortic root, valve, and complex ascending aortic surgery. Curr. Cardiol. Rep. 2000, 2, 549–557. [Google Scholar] [CrossRef]
- Tabata, M.; Khalpey, Z.; Aranki, S.F.; Couper, G.S.; Cohn, L.H.; Shekar, P.S. Minimal access surgery of ascending and proximal arch of the aorta: A 9-year experience. Ann. Thorac. Surg. 2007, 84, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, T.; Couper, G.S.; Borstlap, W.A.; Nauta, F.J.; Wollersheim, L.; McGurk, S.; Cohn, L.H. Minimal-access aortic valve replacement with concomitant aortic procedure: A 9-year experience. Innovations 2012, 7, 368–371. [Google Scholar] [CrossRef]
- Lamelas, J.; Chen, P.C.; Loor, G.; LaPietra, A. Successful Use of Sternal-Sparing Minimally Invasive Surgery for Proximal Ascending Aortic Pathology. Ann. Thorac. Surg. 2018, 106, 742–748. [Google Scholar] [CrossRef]
- Haunschild, J.; van Kampen, A.; von Aspern, K.; Misfeld, M.; Davierwala, P.; Saeed, D.; Borger, M.A.; Etz, C.D. Supracommissural replacement of the ascending aorta and the aortic valve via partial versus full sternotomy-a propensity-matched comparison in a high-volume centre. Eur. J. Cardiothorac. Surg. 2022, 61, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Svensson, L.G. Progress in ascending and aortic arch surgery: Minimally invasive surgery, blood conservation, and neurological deficit prevention. Ann. Thorac. Surg. 2002, 74, S1786–S1799. [Google Scholar] [CrossRef] [PubMed]
- Svensson, L.G.; Nadolny, E.M.; Kimmel, W.A. Minimal access aortic surgery including re-operations. Eur. J. Cardiothorac. Surg. 2001, 19, 30–33. [Google Scholar] [CrossRef] [PubMed]
- LaPietra, A.; Santana, O.; Pineda, A.M.; Mihos, C.G.; Lamelas, J. Outcomes of aortic valve and concomitant ascending aorta replacement performed via a minimally invasive right thoracotomy approach. Innovations 2014, 9, 342. [Google Scholar] [PubMed]
- Deschka, H.; Erler, S.; Machner, M.; El-Ayoubi, L.; Alken, A.; Wimmer-Greinecker, G. Surgery of the ascending aorta, root remodelling and aortic arch surgery with circulatory arrest through partial upper sternotomy: Results of 50 consecutive cases. Eur. J. Cardiothorac. Surg. 2013, 43, 580–584. [Google Scholar] [CrossRef]
- Celmeta, B.; Viva, T.; Bisogno, A.; Bruno, V.D.; Miceli, A.; Glauber, M. Detachable Aortic Clamp for Minimally Invasive Cardiac Surgery. Surg. Technol. Int. 2023, 42, sti42/1675. [Google Scholar]
- Sansone, F.; Ceresa, F.; Patanè, F. Transcutaneous insertion of the Chitwood® clamp in case of minimally invasive cardiac surgery. Personal experience. Il G. Chir.-J. Ital. Surg. Assoc. 2013, 34, 278–279. [Google Scholar]
- Perrotta, S.; Lentini, S. Ministernotomy approach for surgery of the aortic root and ascending aorta. Interact. Cardiovasc. Thorac. Surg. 2009, 9, 849–858. [Google Scholar] [CrossRef]
- Zierer, A.; El-Sayed Ahmad, A.; Papadopoulos, N.; Moritz, A.; Diegeler, A.; Urbanski, P.P. Selective antegrade cerebral perfusion and mild (28 °C–30 °C) systemic hypothermic circulatory arrest for aortic arch replacement: Results from 1002 patients. J. Thorac. Cardiovasc. Surg. 2012, 144, 1042–1049. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Helms, F.; Schmack, B.; Weymann, A.; Hanke, J.S.; Natanov, R.; Martens, A.; Ruhparwar, A.; Popov, A.-F. Expanding the Minimally Invasive Approach towards the Ascending Aorta—A Practical Overview of the Currently Available Techniques. Medicina 2023, 59, 1618. https://doi.org/10.3390/medicina59091618
Helms F, Schmack B, Weymann A, Hanke JS, Natanov R, Martens A, Ruhparwar A, Popov A-F. Expanding the Minimally Invasive Approach towards the Ascending Aorta—A Practical Overview of the Currently Available Techniques. Medicina. 2023; 59(9):1618. https://doi.org/10.3390/medicina59091618
Chicago/Turabian StyleHelms, Florian, Bastian Schmack, Alexander Weymann, Jasmin Sarah Hanke, Ruslan Natanov, Andreas Martens, Arjang Ruhparwar, and Aron-Frederik Popov. 2023. "Expanding the Minimally Invasive Approach towards the Ascending Aorta—A Practical Overview of the Currently Available Techniques" Medicina 59, no. 9: 1618. https://doi.org/10.3390/medicina59091618
APA StyleHelms, F., Schmack, B., Weymann, A., Hanke, J. S., Natanov, R., Martens, A., Ruhparwar, A., & Popov, A.-F. (2023). Expanding the Minimally Invasive Approach towards the Ascending Aorta—A Practical Overview of the Currently Available Techniques. Medicina, 59(9), 1618. https://doi.org/10.3390/medicina59091618