The Impact of COVID-19 Pandemic on Weight Loss, Eating Behaviour and Quality of Life after Roux-en-Y Gastric Bypass
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Surgical Procedure
2.3. Ethics
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Zachary, Z.; Brianna, F.; Brianna, L.; Garrett, P.; Jade, W.; Alyssa, D.; Mikayla, K. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes. Res. Clin. Pract. 2020, 14, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, D.; Gill, T. Impact of COVID-19 lockdown on self-managed weight loss journeys. Obes. Res. Clin. Pract. 2020, 14, 386–387. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 15 March 2023).
- Schwartz, M.W.; Seeley, R.J.; Zeltser, L.M.; Drewnowski, A.; Ravussin, E.; Redman, L.M.; Leibel, R.L. Obesity Pathogenesis: An Endocrine Society Scientific Statement. Endocr. Rev. 2017, 38, 267–296. [Google Scholar] [CrossRef] [PubMed]
- Aghili, S.M.M.; Ebrahimpur, M.; Arjmand, B.; Shadman, Z.; Pejman Sani, M.; Qorbani, M.; Larijani, B.; Payab, M. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: A review and meta-analysis. Int. J. Obes. 2021, 45, 998–1016. [Google Scholar] [CrossRef] [PubMed]
- Bauraitė, K.; Mikuckytė, D.; Gudaitytė, R.; Petereit, R.; Maleckas, A. Factors associated with quality of life and weight regain 12 years after Roux-en-Y gastric bypass. Surg. Endosc. 2022, 36, 4333–4341. [Google Scholar] [CrossRef]
- Sjöström, L. Bariatric surgery and reduction in morbidity and mortality: Experiences from the SOS study. Int. J. Obes. 2008, 32 (Suppl. S7), S93–S97. [Google Scholar] [CrossRef]
- Hasnain, N.; Moeed, A.; Waqar, E.; Farhan, S.A.; Amreek, F. Efficacy of bariatric surgery in COVID-19 patients: An updated systematic review and meta-analysis. Surg. Pract. Sci. 2022, 11, 100140. [Google Scholar] [CrossRef]
- American Society for Metabolic and Bariatric Surgery. Estimate of Bariatric Surgery Numbers, 2011–2020. Available online: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers (accessed on 15 March 2023).
- Murtha, J.A.; Alagoz, E.; Breuer, C.R.; Eierman, L.; Jawara, D.; Farrar-Edwards, D.; Voils, C.I.; Funk, L.M. Impact of COVID-19 on the Postoperative Bariatric Surgery Patient Experience. Ann. Surg. 2023, 277, e745–e751. [Google Scholar] [CrossRef]
- Haghighat, N.; Foroutan, H.; Hesameddini, I.; Amini, M.; Hosseini, B.; Moeinvaziri, N.; Hosseini, S.V.; Kamran, H. Impact of the COVID-19 Pandemic on the Success of Bariatric Surgeries in Patients with Severe Obesity. Obes. Facts 2023, 16, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, A.; Berardi, G.; Velotti, N.; Schiavone, V.; Musella, M. Impact of COVID-19 Lockdown on Short-term Weight Loss in a Single Italian Institution. Obes. Surg. 2021, 31, 3365–3368. [Google Scholar] [CrossRef] [PubMed]
- Talledo, O.; Carroll, R.; Worden, E.; Greenwood, A.M.; Alexander, H.; Karlsdottir, B.; Lehmann, R.; Peoples, R.; Smith, J.; Thompson, D.; et al. The impact of COVID-19 on medium term weight loss and comorbidities in patients undergoing bariatric surgery and its association with psychological wellbeing. Surg. Endosc. 2023, 37, 1537–1542. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.Y.; Grunvald, E.; Blitzer, R.R.; Lee, A.M.; Broderick, R.C.; Li, J.Z.; Cheverie, J.N.; Sandler, B.J.; Horgan, S.; Jacobsen, G.R. Despite regression of healthy lifestyle habits, weight loss after bariatric surgery is not affected during the COVID-19 pandemic. Surg. Endosc. 2023, 37, 607–612. [Google Scholar] [CrossRef]
- Ayuso, M.C.; Jimenez, P.P.; Orduña, P.C.; Carretero, J.I.B.; Alvarez, J.G. Impact of COVID-19 Lockdown on Short-Term Weight Loss After Bariatric Surgery. Obes. Surg. 2023, 33, 961–964. [Google Scholar] [CrossRef]
- Pereira, X.; Romero-Velez, G.; Skendelas, J.P.; Rodriguez-Quintero, J.H.; Grosser, R.; Lima, D.L.; Moran-Atkin, E.; Choi, J.; Camacho, D. The COVID-19 Pandemic Did Not Affect Target Weight Loss 1 Year Post Bariatric Surgery. Obes. Surg. 2021, 31, 4926–4932. [Google Scholar] [CrossRef]
- Hu, A.; Harvey, A.; Rogers, A.M.; Rigby, A.; Butt, M. Associations of COVID-19 Lockdowns on Eating Behaviors and Body Mass Index in Patients with a History of Bariatric Surgery: A Cross-Sectional Analysis. Obes. Surg. 2023, 33, 1099–1107. [Google Scholar] [CrossRef]
- Youssef, A.; Cassin, S.E.; Wnuk, S.; Leung, S.; Jackson, T.; Sockalingam, S. The impact of COVID-19 pandemic on bariatric patients’ self-management post-surgery. Appetite 2021, 162, 105166. [Google Scholar] [CrossRef]
- Petereit, R.; Jonaitis, L.; Kupčinskas, L.; Maleckas, A. Gastrointestinal symptoms and eating behavior among morbidly obese patients undergoing Roux-en-Y gastric bypass. Medicina 2014, 50, 118–123. [Google Scholar] [CrossRef]
- Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee; World Health Organ Technical Report Series 854; World Health Organization: Geneva, Switzerland, 1995; pp. 1–452. [Google Scholar]
- Karlsson, J.; Persson, L.O.; Sjöström, L.; Sullivan, M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1715–1725. [Google Scholar] [CrossRef]
- Kolotkin, R.L.; Crosby, R.D.; Gress, R.E.; Hunt, S.C.; Adams, T.D. Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg. Obes. Relat. Dis. 2009, 5, 250–256. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ware, J.; Snow, K.; Kosinski, M.; Gandek, B. SF-36 Health Survey: Manual and Interpretation Guide; The Health Institute, New England Medical Center: Boston, UK, 1993. [Google Scholar]
- Elmacıoğlu, F.; Emiroğlu, E.; Ülker, M.T.; Özyılmaz Kırcali, B.; Oruç, S. Evaluation of nutritional behaviour related to COVID-19. Public. Health Nutr. 2021, 24, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Costa, M.L.; Costa, M.G.O.; de Souza, M.F.C.; da Silva, D.G.; Dos Santos Vieira, D.A.; Mendes-Netto, R.S. Cognitive restraint, emotional eating and uncontrolled eating: Exploring factors associated with the cycle of behaviors during the COVID-19 pandemic. Food Qual. Prefer. 2022, 100, 104579. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.T.; Kannan, T.M. Comparison of eating behaviour by relative weight change status of young adults throughout the COVID-19 pandemic. Dialogues Health 2023, 2, 100094. [Google Scholar] [CrossRef]
- Athanasiadis, D.I.; Hernandez, E.; Hilgendorf, W.; Roper, A.; Embry, M.; Selzer, D.; Stefanidis, D. How are bariatric patients coping during the coronavirus disease 2019 (COVID-19) pandemic? Analysis of factors known to cause weight regain among postoperative bariatric patients. Surg. Obes. Relat. Dis. 2021, 17, 756–764. [Google Scholar] [CrossRef]
- Kubo, K.Y.; Iinuma, M.; Chen, H. Mastication as a Stress-Coping Behavior. Biomed. Res. Int. 2015, 2015, 876409. [Google Scholar] [CrossRef]
- Andreu, A.; Flores, L.; Molero, J.; Mestre, C.; Obach, A.; Torres, F.; Moizé, V.; Vidal, J.; Navinés, R.; Peri, J.M.; et al. Patients Undergoing Bariatric Surgery: A Special Risk Group for Lifestyle, Emotional and Behavioral Adaptations During the COVID-19 Lockdown. Lessons from the First Wave. Obes. Surg. 2022, 32, 441–449. [Google Scholar] [CrossRef]
- Conceição, E.; de Lourdes, M.; Ramalho, S.; Félix, S.; Pinto-Bastos, A.; Vaz, A.R. Eating behaviors and weight outcomes in bariatric surgery patients amidst COVID-19. Surg. Obes. Relat. Dis. 2021, 17, 1165–1174. [Google Scholar] [CrossRef]
- Roser, K.; Baenziger, J.; Ilic, A.; Mitter, V.R.; Mader, L.; Dyntar, D.; Michel, G.; Sommer, G. Health-related quality of life before and during the COVID-19 pandemic in Switzerland: A cross-sectional study. Qual. Life Res. 2023, 32, 2695–2706. [Google Scholar] [CrossRef]
- Fernández-Abascal, E.G.; Martín-Díaz, M.D. One Year of COVID-19 in Spain, Longitudinal Study on Mental and Physical Health. Behav. Med. 2022, 1–13. [Google Scholar] [CrossRef]
- Cheng, Z.; Gao, X.; Yang, C.; Brytek-Matera, A.; He, J. Effects of Online and Face-to-Face Intuitive Eating Interventions on Body Image and Eating Behaviors among Women in China: A Feasibility Study. Nutrients 2022, 14, 1761. [Google Scholar] [CrossRef] [PubMed]

| Group S * (n = 72) | Group C (n = 87) | p Value | |
|---|---|---|---|
| Age before the surgery, yr., mean (SD) | 44.31 (11.95) | 41.91 (10.98) | 0.189 |
| Sex F/M | 51/21 | 62/25 | 0.107 |
| BMI before the surgery, mean (SD) | 46.07 (8.42) | 44.95 (6.57) | 0.359 |
| %EBMIL one yr. post-surgery, %, (SD) | 77.88 (26.33) | 76.21 (19.98) | 0.663 |
| Cardiovascular diseases ** (%) | 32.20 1 | 12.99 | 0.005 |
| Hypertension ** (%) | 69.49 1 | 65.52 | 0.618 |
| Diabetes ** (%) | 28.81 1 | 10.34 | 0.004 |
| Musculoskeletal disorders ** (%) | 37.29 1 | 17.24 | 0.007 |
| Gastrointestinal diseases ** (%) | 27.12 1 | 1.15 | <0.0001 |
| Respiratory disease ** (%) | 20.34 1 | 6.90 | 0.016 |
| Depression ** (%) | 25.00 2 | 35.63 | 0.173 |
| Work style ** (%): | |||
| Not working | 6.78 1 | 0.00 | 0.014 |
| Sedentary | 50.85 1 | 40.23 | 0.207 |
| Variable | 19.00 1 | 37.93 | 0.015 |
| Not sedentary | 10.17 1 | 18.39 | 0.175 |
| Intense physical work | 0.00 1 | 3.45 | 0.121 |
| Before RYGB | One Year after RYGB | Change from Baseline to Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Group S * | Group C | p Value | Group S | Group C | p Value | Delta | Delta Group C | p Value |
| (n = 60) | (n = 87) | (n = 72) | (n = 87) | Group S | |||||
| TFEQ (mean, (SD)) | |||||||||
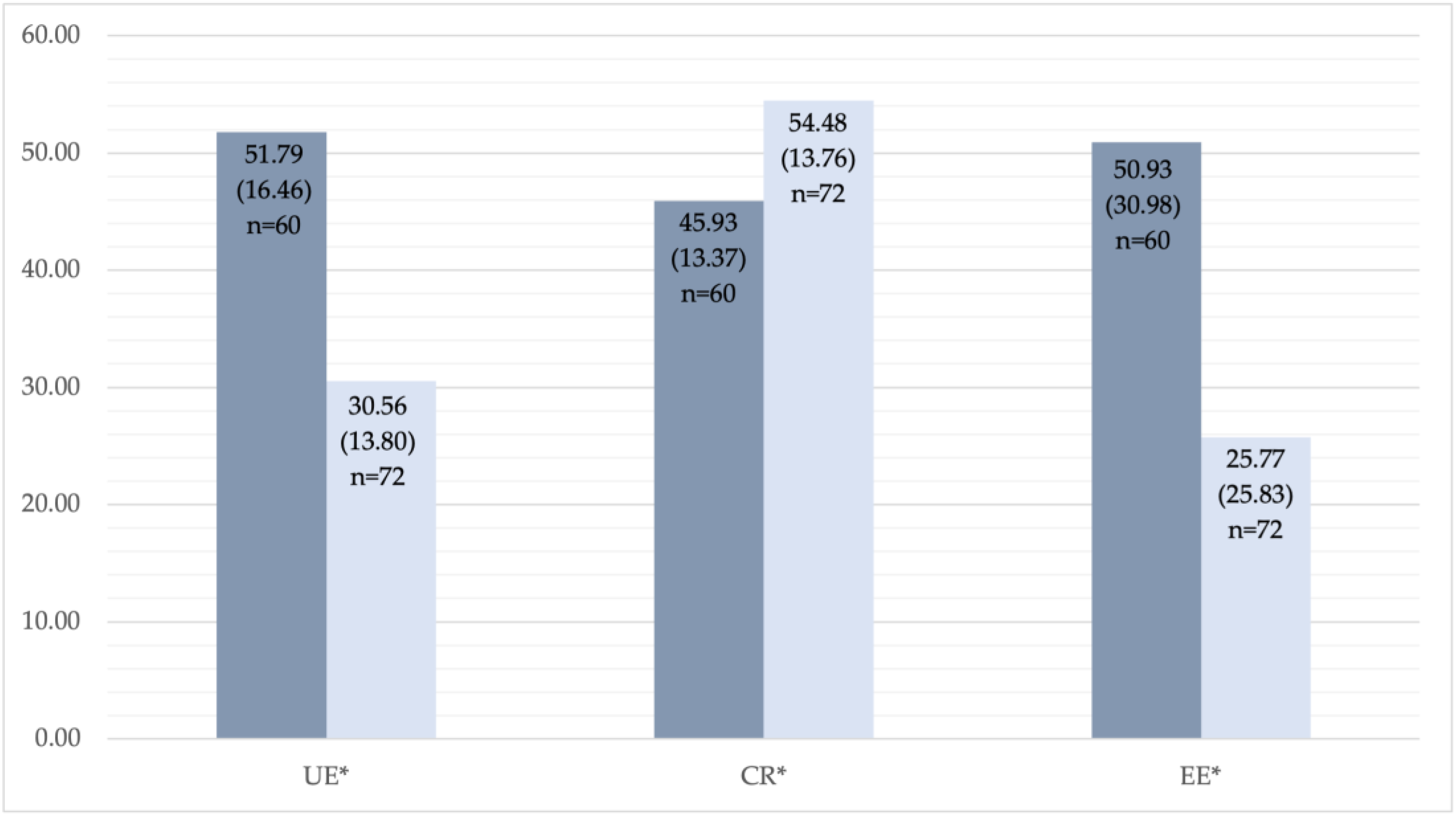
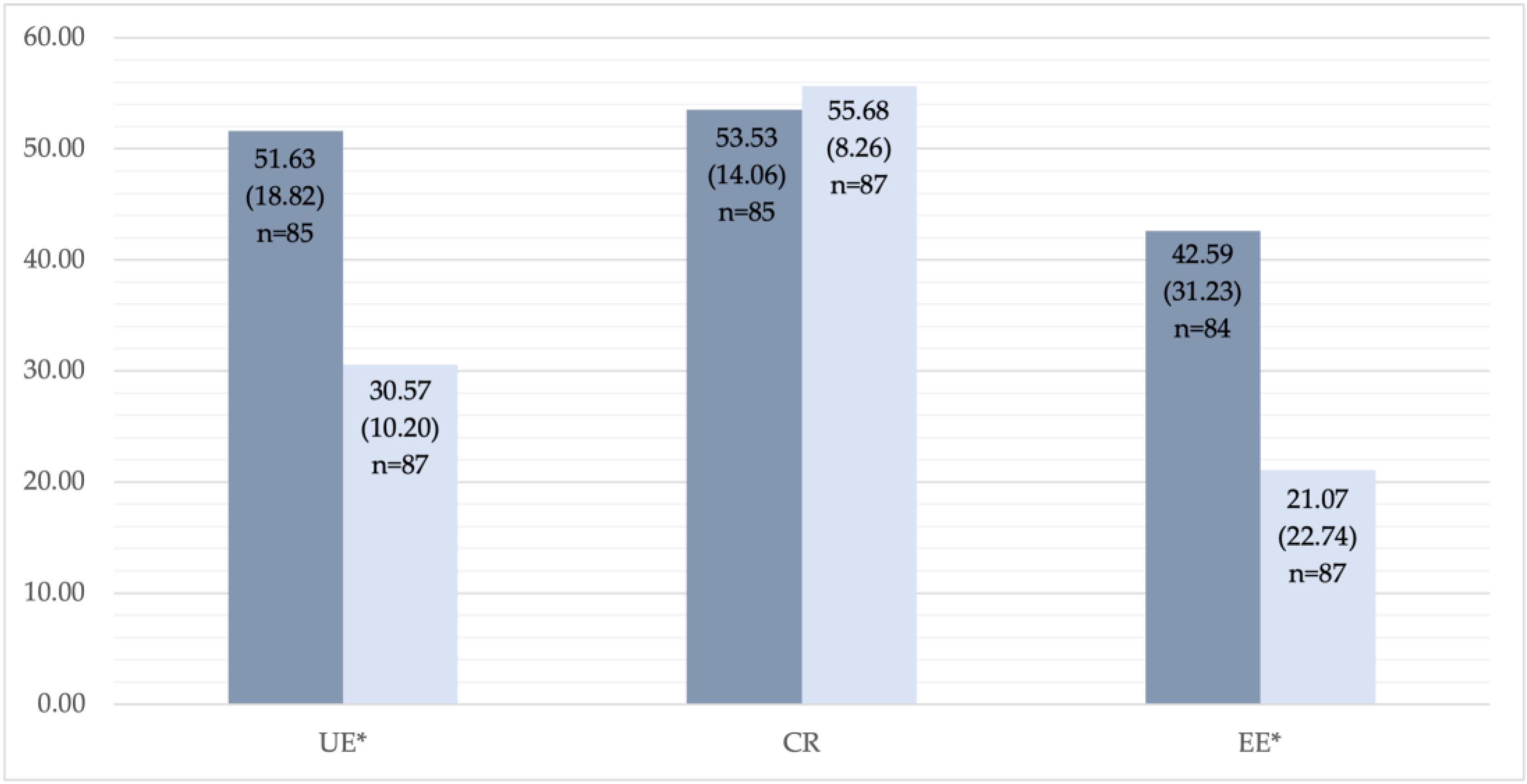
| Uncontrolled eating | 51.8 (16.5) | 51.6 (18.8) 1 | 0.959 | 30.6 (13.8) | 30.6 (10.2) | 0.996 | −20.9 (20.0) | −21.0 (20.3) | 0.978 |
| Cognitive restraint | 45.9 (13.4) | 53.5 (14.1) 1 | 0.001 | 54.5 (13.8) | 55.7 (8.3) | 0.515 | 7.4 (20.6) | 2.2 (15.7) | 0.099 |
| Emotional eating | 50.9 (31.0) | 42.6 (31.2) 2 | 0.115 | 25.8 (25.8) | 21.1 (22.7) | 0.225 | −26.7 (31.7) | −21.2 (35.0) | 0.335 |
| SF-36 (mean, (SD)) | |||||||||
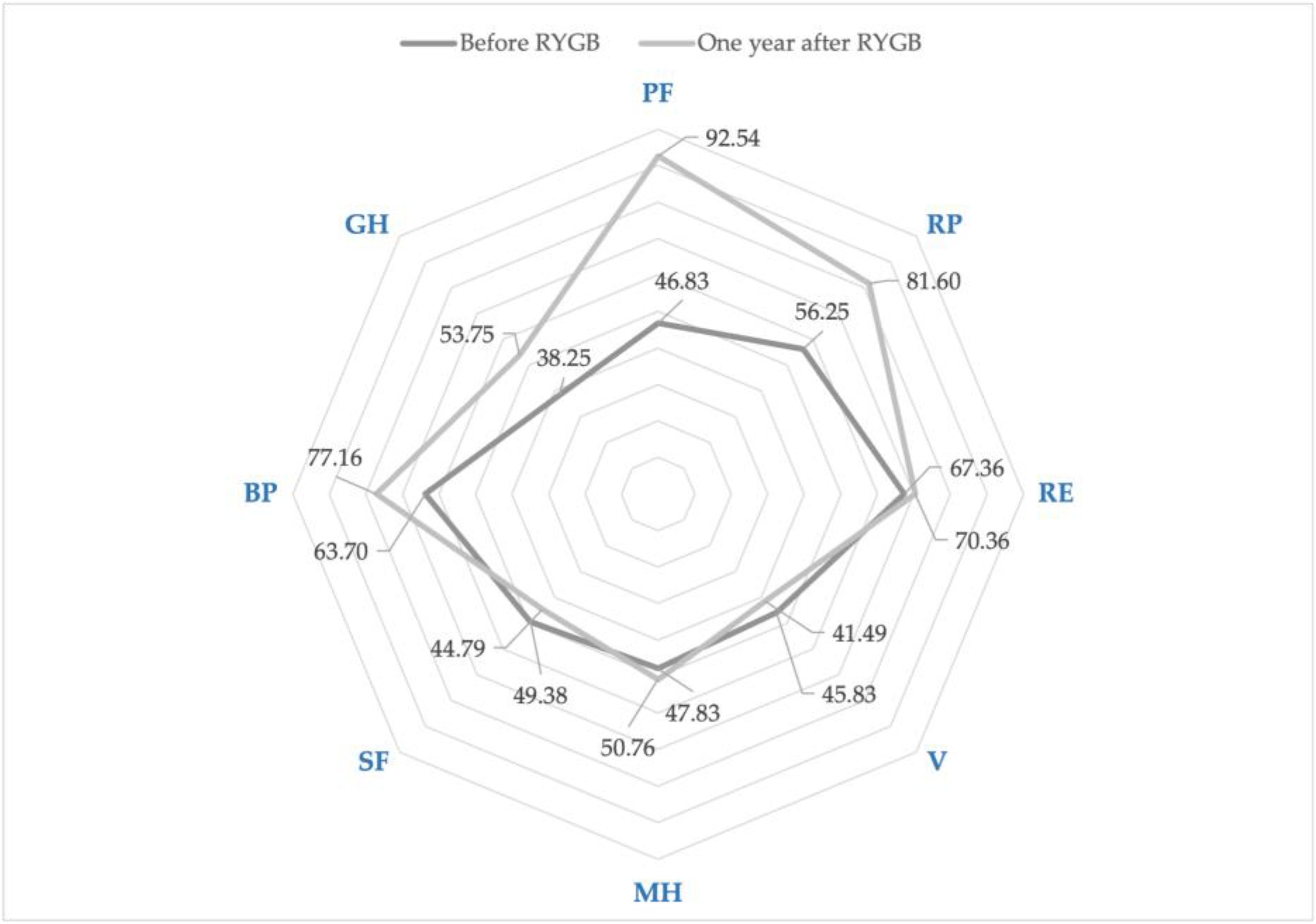
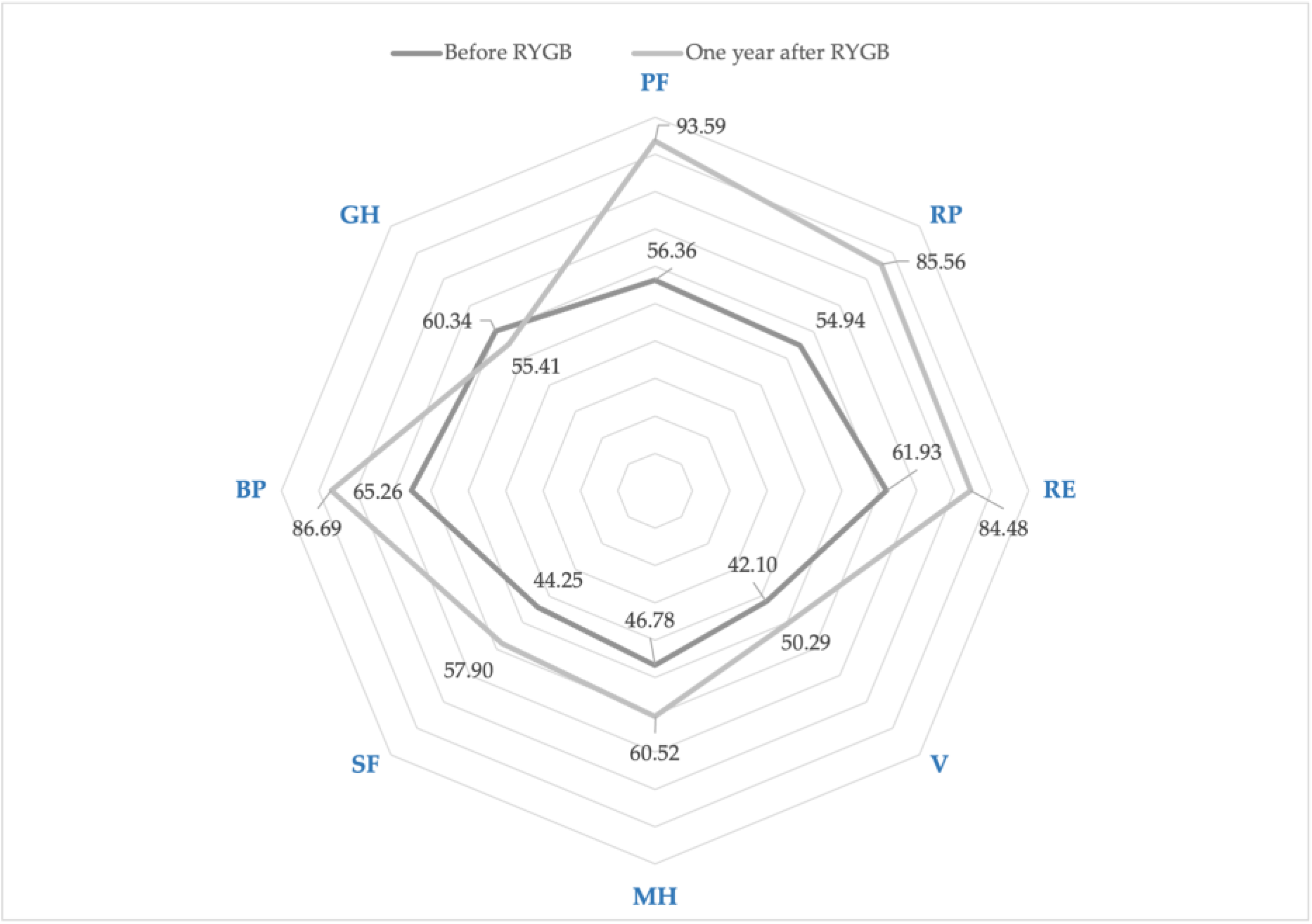
| Physical functioning | 46.8 (32.3) | 56.4 (26.2) 3 | 0.064 | 92.5 (12.0) 4 | 93.6 (14.5) 1 | 0.627 | 46.1 (31.9) | 37.8 (27.4) | 0.102 |
| Role limitations due to physical health | 56.3 (30.5) | 54.9 (23.4) 3 | 0.781 | 81.6 (24.7) 4 | 85.6 (23.1) | 0.300 | 27.5 (34.2) | 29.9 (27.9) | 0.660 |
| Role limitations due to emotional problems | 67.4 (32.3) | 61.9 (23.7) 3 | 0.273 | 70.4 (27.5) 5 | 84.5 (24.3) | 0.001 | 3.9 (42.0) | 21.9 (31.5) | 0.007 |
| Vitality | 45.8 (9.6) | 42.1 (14.0) | 0.057 | 41.5 (13.9) | 50.3 (12.5) | <0.0001 | −4.6 (15.8) | 8.2 (20.0) | <0.0001 |
| Mental health | 47.8 (10.8) | 46.8 (14.6) | 0.616 | 50.8 (11.3) | 60.5 (14.2) | <0.0001 | 3.3 (16.6) | 13.7 (21.1) | 0.001 |
| Social functioning | 49.4 (10.9) | 44.3 (15.9) | 0.022 | 44.8 (12.2) | 57.9 (17.8) | <0.0001 | −5.0 (16.8) | 13.7 (25.8) | <0.0001 |
| Body pain | 63.7 (32.9) | 65.3 (27.1) | 0.762 | 77.2 (26.4) | 86.7 (20.8) | 0.014 | 14.6 (36.0) | 21.5 (27.4) 6 | 0.218 |
| General health | 38.3 (14.7) | 60.3 (17.0) | <0.0001 | 53.8 (14.4) | 55.4 (11.0) 6 | 0.424 | 16.9 (18.9) | −5.1 (19.8) 6 | <0.0001 |
| PCS | 50.2 (16.6) | 56.0 (12.9) | 0.025 | 69.3 (11.0) | 74.0 (11.6) | 0.009 | 20.0 (16.9) | 18.1 (14.1) | 0.456 |
| MCS | 49.7 (8.2) | 50.7 (9.5) | 0.542 | 52.1 (8.7) | 61.7 (11.1) | <0.0001 | 2.6 (11.7) | 11.1 (15.3) | 0.0002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bauraitė, K.; Gudaitytė, R.; Maleckas, A. The Impact of COVID-19 Pandemic on Weight Loss, Eating Behaviour and Quality of Life after Roux-en-Y Gastric Bypass. Medicina 2023, 59, 1597. https://doi.org/10.3390/medicina59091597
Bauraitė K, Gudaitytė R, Maleckas A. The Impact of COVID-19 Pandemic on Weight Loss, Eating Behaviour and Quality of Life after Roux-en-Y Gastric Bypass. Medicina. 2023; 59(9):1597. https://doi.org/10.3390/medicina59091597
Chicago/Turabian StyleBauraitė, Karolina, Rita Gudaitytė, and Almantas Maleckas. 2023. "The Impact of COVID-19 Pandemic on Weight Loss, Eating Behaviour and Quality of Life after Roux-en-Y Gastric Bypass" Medicina 59, no. 9: 1597. https://doi.org/10.3390/medicina59091597
APA StyleBauraitė, K., Gudaitytė, R., & Maleckas, A. (2023). The Impact of COVID-19 Pandemic on Weight Loss, Eating Behaviour and Quality of Life after Roux-en-Y Gastric Bypass. Medicina, 59(9), 1597. https://doi.org/10.3390/medicina59091597




