Intradiscal Condoliase Injection Therapy for Recurrent Lumbar Disc Herniation: Case Series and Literature Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Case Series
2.1.1. Participants
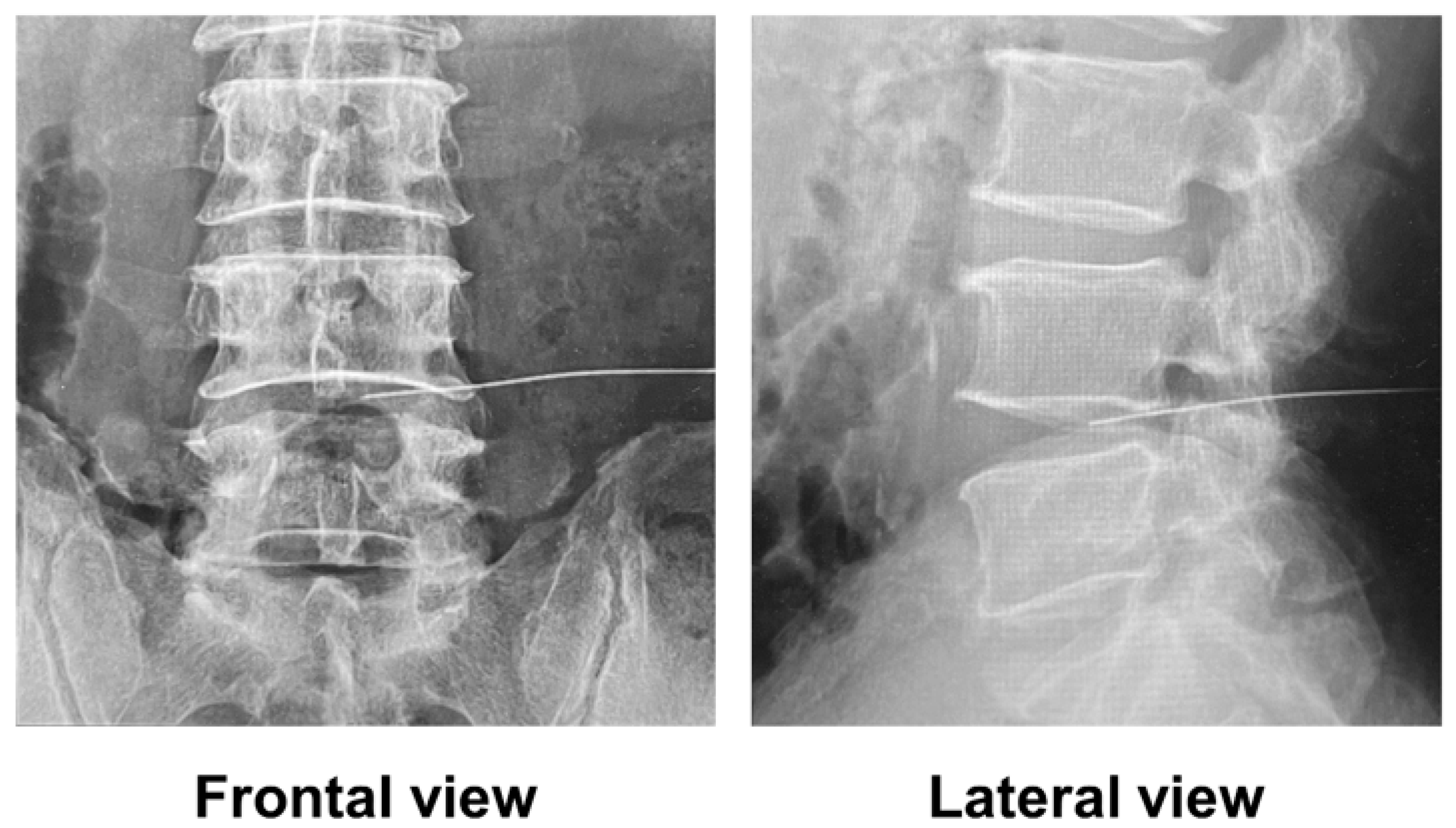
2.1.2. Condoliase Treatment
2.1.3. Evaluations
2.1.4. Statistical Analysis
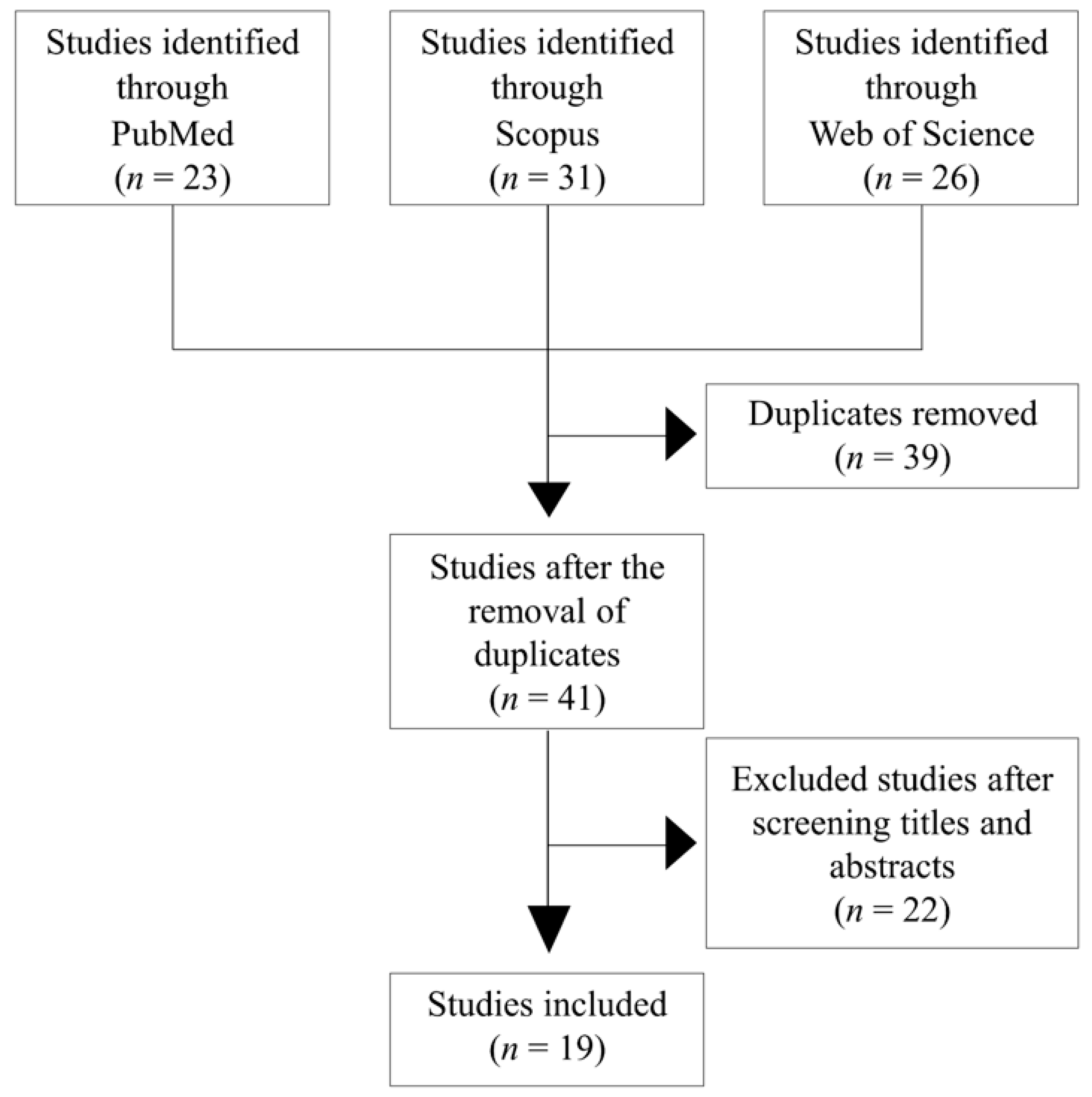
2.2. Literature Review
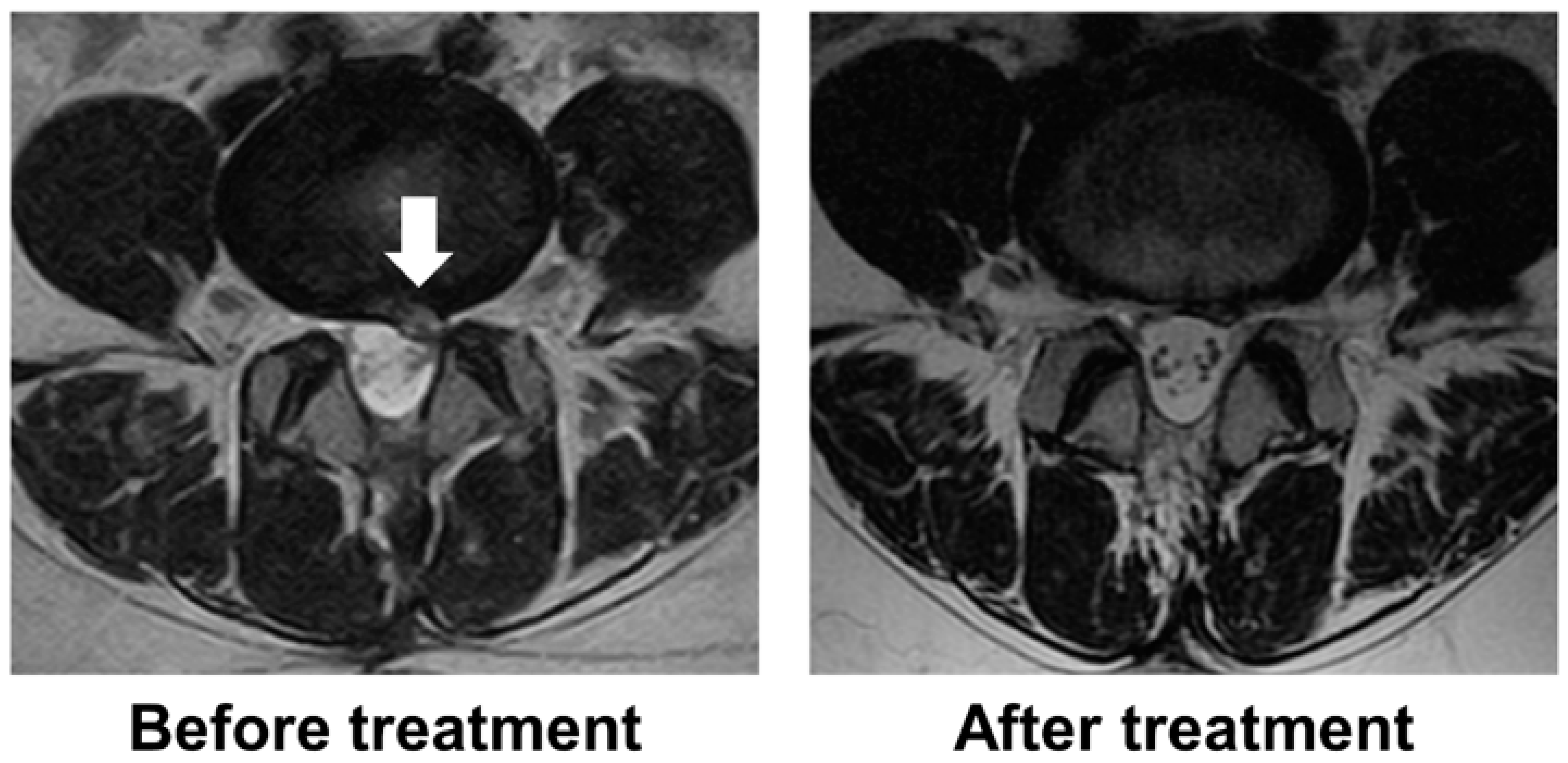
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lurie, J.D.; Tosteson, T.D.; Tosteson, A.N.; Zhao, W.; Morgan, T.S.; Abdu, W.A.; Herkowitz, H.; Weinstein, J.N. Surgical versus nonoperative treatment for lumbar disc herniation: Eight-year results for the spine patient outcomes research trial. Spine 2014, 39, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Fjeld, O.R.; Grovle, L.; Helgeland, J.; Smastuen, M.C.; Solberg, T.K.; Zwart, J.A.; Grotle, M. Complications, reoperations, readmissions, and length of hospital stay in 34 639 surgical cases of lumbar disc herniation. Bone Joint J. 2019, 101-B, 470–477. [Google Scholar] [CrossRef]
- Nykvist, F.; Hurme, M.; Alaranta, H.; Kaitsaari, M. Severe sciatica: A 13-year follow-up of 342 patients. Eur. Spine J. 1995, 4, 335–338. [Google Scholar] [CrossRef]
- Swartz, K.R.; Trost, G.R. Recurrent lumbar disc herniation. Neurosurg. Focus. 2003, 15, E10. [Google Scholar] [CrossRef] [PubMed]
- Yuce, I.; Kahyaoglu, O.; Cavusoglu, H.; Aydin, Y. Surgical outcome and efficacy of lumbar microdiscectomy technique with preserving of ligamentum flavum for recurrent lumbar disc herniations. J. Clin. Neurosci. 2019, 63, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.Y.; Zhou, Q.; Yao, W.F.; Shen, L. Recurrent lumbar disc herniation after discectomy: Outcome of repeat discectomy. Surg. Neurol. 2005, 64, 226–231, discussion 231. [Google Scholar] [CrossRef] [PubMed]
- Nolte, M.T.; Basques, B.A.; Louie, P.K.; Khan, J.M.; Varthi, A.; Paul, J.; An, H.S. Patients Undergoing Revision Microdiskectomy for Recurrent Lumbar Disk Herniation Experience Worse Clinical Outcomes and More Revision Surgeries Compared with Patients Undergoing a Primary Microdiskectomy. J. Am. Acad. Orthop. Surg. 2019, 27, e796–e803. [Google Scholar] [CrossRef]
- Miwa, S.; Yokogawa, A.; Kobayashi, T.; Nishimura, T.; Igarashi, K.; Inatani, H.; Tsuchiya, H. Risk factors of recurrent lumbar disk herniation: A single center study and review of the literature. J. Spinal Disord. Tech. 2015, 28, E265–E269. [Google Scholar] [CrossRef]
- Chiba, K.; Matsuyama, Y.; Seo, T.; Toyama, Y. Condoliase for the Treatment of Lumbar Disc Herniation: A Randomized Controlled Trial. Spine 2018, 43, E869–E876. [Google Scholar] [CrossRef]
- Matsuyama, Y.; Chiba, K.; Iwata, H.; Seo, T.; Toyama, Y. A multicenter, randomized, double-blind, dose-finding study of condoliase in patients with lumbar disc herniation. J. Neurosurg. Spine 2018, 28, 499–511. [Google Scholar] [CrossRef]
- Funayama, T.; Setojima, Y.; Shibao, Y.; Noguchi, H.; Miura, K.; Eto, F.; Sato, K.; Kono, M.; Asada, T.; Takahashi, H.; et al. A Case of Postoperative Recurrent Lumbar Disc Herniation Conservatively Treated with Novel Intradiscal Condoliase Injection. Case Rep. Orthop. 2022, 2022, 3656753. [Google Scholar] [CrossRef]
- Nakajima, H.; Kubota, A.; Maezawa, Y.; Watanabe, S.; Honjoh, K.; Ohmori, H.; Matsumine, A. Short-Term Outcome and Predictors of Therapeutic Effects of Intradiscal Condoliase Injection for Patients with Lumbar Disc Herniation. Spine Surg. Relat. Res. 2020, 5, 264–271. [Google Scholar] [CrossRef]
- Banno, T.; Hasegawa, T.; Yamato, Y.; Yoshida, G.; Yasuda, T.; Arima, H.; Oe, S.; Ushirozako, H.; Yamada, T.; Ide, K.; et al. Clinical outcome of condoliase injection treatment for lumbar disc herniation: Indications for condoliase therapy. J. Orthop. Sci. 2021, 26, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Pfirrmann, C.W.; Metzdorf, A.; Zanetti, M.; Hodler, J.; Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001, 26, 1873–1878. [Google Scholar] [CrossRef] [PubMed]
- Udby, P.M.; Modic, M.; Elmose, S.; Carreon, L.Y.; Andersen, M.O.; Karppinen, J.; Samartzis, D. The Clinical Significance of the Modic Changes Grading Score. Global Spine J. 2022, 21925682221123012. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Kim, Y.T.; Lee, C.S.; Shin, M.J. MRI classification of lumbar herniated intervertebral disc. Orthopedics 1992, 15, 493–497. [Google Scholar] [CrossRef]
- Matsuyama, Y.; Seo, T.; Chiba, K. Condoliase chemonucleolysis for lumbar disc herniation: A post-hoc follow-up study of patients in previous clinical trials. J. Orthop. Sci. 2023, in press.
- Ishibashi, K.; Fujita, M.; Takano, Y.; Iwai, H.; Inanami, H.; Koga, H. Chemonucleolysis with Chondroitin Sulfate ABC Endolyase for Treating Lumbar Disc Herniation: Exploration of Prognostic Factors for Good or Poor Clinical Outcomes. Medicina 2020, 56, 627. [Google Scholar] [CrossRef]
- Okada, E.; Suzuki, S.; Nori, S.; Tsuji, O.; Nagoshi, N.; Yagi, M.; Fujita, N.; Nakamura, M.; Matsumoto, M.; Watanabe, K. The effectiveness of chemonucleolysis with condoliase for treatment of painful lumbar disc herniation. J. Orthop. Sci. 2021, 26, 548–554. [Google Scholar] [CrossRef]
- Inoue, M.; Sainoh, T.; Kojima, A.; Yamagata, M.; Morinaga, T.; Mannoji, C.; Ataka, H.; Yamashita, M.; Takahashi, H.; Saito, J.; et al. Efficacy and Safety of Condoliase Disc Administration as a New Treatment for Lumbar Disc Herniation. Spine Surg. Relat. Res. 2021, 6, 31–37. [Google Scholar] [CrossRef]
- Hirai, T.; Takahashi, T.; Tanaka, T.; Motoyoshi, T.; Matsukura, Y.; Yuasa, M.; Inose, H.; Yoshii, T.; Okawa, A. Intradiscal Injection with Condoliase (Chondroitin Sulfate ABC Endolyase) for Painful Radiculopathy Caused by Lumbar Disc Herniation. Spine Surg. Relat. Res. 2021, 6, 252–260. [Google Scholar] [CrossRef]
- Banno, T.; Hasegawa, T.; Yamato, Y.; Yoshida, G.; Arima, H.; Oe, S.; Mihara, Y.; Yamada, T.; Ide, K.; Watanabe, Y.; et al. Disc degeneration could be recovered after chemonucleolysis with condoliase.-1 year clinical outcome of condoliase therapy. J. Orthop. Sci. 2022, 27, 767–773. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Sato, K.; Ando, T. Factors associated with disc degeneration based on Pfirrmann criteria after condoliase treatment for lumbar disc herniation. J. Orthop. Sci. 2022. [Google Scholar] [CrossRef] [PubMed]
- Oshita, Y.; Matsuyama, D.; Sakai, D.; Schol, J.; Shirasawa, E.; Emori, H.; Segami, K.; Takahashi, S.; Yagura, K.; Miyagi, M.; et al. Multicenter Retrospective Analysis of Intradiscal Condoliase Injection Therapy for Lumbar Disc Herniation. Medicina 2022, 58, 1284. [Google Scholar] [CrossRef] [PubMed]
- Banno, T.; Hasegawa, T.; Yamato, Y.; Yoshida, G.; Arima, H.; Oe, S.; Ide, K.; Yamada, T.; Kurosu, K.; Nakai, K.; et al. Condoliase therapy for lumbar disc herniation -2 year clinical outcome. J. Orthop. Sci. 2023, in press.
- Takeuchi, S.; Hanakita, J.; Takahashi, T.; Inoue, T.; Minami, M.; Suda, I.; Nakamura, S.; Kanematsu, R. Predictive Factors for Poor Outcome following Chemonucleolysis with Condoliase in Lumbar Disc Herniation. Medicina 2022, 58, 1868. [Google Scholar] [CrossRef] [PubMed]
- Takaki, S.; Miyama, H.; Iwasaki, M. Cost-effectiveness analysis of intradiscal condoliase injection vs. surgical or conservative treatment for lumbar disc herniation. J. Med. Econ. 2023, 26, 233–242. [Google Scholar] [CrossRef]
- Ohtonari, T.; Torii, R.; Noguchi, S.; Kitagawa, T.; Nishihara, N. Short-term clinical and radiographic outcomes of chemonucleolysis with condoliase for painful lumbar disc herniation and analysis regarding intradiscal injection area. Neurosurg. Rev. 2023, 46, 59. [Google Scholar] [CrossRef]
- Kobayashi, K.; Sato, K.; Ando, T.; Ando, K. MRI characteristics of disc degeneration after condoliase injection in young patients: A consecutive case series. J. Orthop. Sci. 2023, in press.
- Funayama, T.; Mataki, K.; Murakami, K.; Mataki, Y.; Noguchi, H.; Miura, K.; Shibao, Y.; Eto, F.; Kono, M.; Abe, T.; et al. Two Cases of Lateral Lumbar Disc Herniation Successfully Treated with Intradiscal Condoliase Injection. Spine Surg. Relat. Res. 2020, 5, 437–441. [Google Scholar] [CrossRef]

| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Age (years) | 82 | 61 | 51 | 48 | 76 | 70 | ||
| Sex | Male | Male | Male | Female | Male | Female | ||
| Location | L5-S | L5-S | L5-S | L4-5 | L4-5 | L5-S | ||
| Time to recurrence (month) | 24 | 15 | 6 | 12 | 24 | 48 | ||
| Time to treatment (week) | 16 | 52 | 20 | 1 | 8 | 28 | ||
| Follow-up time (month) | 12 | 24 | 7 | 12 | 12 | 12 | ||
| VAS score forback pain (mm) | Pre | 56 | 71 | 86 | 85 | 72 | 50 | |
| 1 M | 22 | 25 | 81 | 21 | 55 | 31 | 0.058 | |
| 3 M | 67 | 54 | 75 | 23 | 54 | 18 | 0.233 | |
| 6 M | 48 | 52 | 73 | 19 | 28 | 11 | 0.052 | |
| VAS score forleg pain (mm) | Pre | 78 | 74 | 84 | 85 | 82 | 48 | |
| 1 M | 31 | 26 | 81 | 11 | 58 | 14 | 0.049 | |
| 3 M | 35 | 55 | 81 | 0 | 53 | 5 | 0.059 | |
| 6 M | 50 | 52 | 75 | 0 | 29 | 10 | 0.044 | |
| JOS score | Pre | 20 | 18 | 15 | 14 | 13 | 17 | |
| 1 M | 17 | 24 | 16 | 20 | 18 | 26 | 0.191 | |
| 3 M | 19 | 24 | 16 | 19 | 17 | 24 | 0.247 | |
| 6 M | 21 | 23 | 20 | 18 | 11 | 24 | 0.315 | |
| Disc height (mm) | Pre | 8.7 | 9.6 | 5.5 | 7.6 | 9.7 | 9.0 | <0.001 |
| 6 M | 6.9 | 8.1 | 3.7 | 6.4 | 9.0 | 7.4 | ||
| T2 signal intensity of disc herniation | High | High | High | High | Low | High | ||
| Pfirrmann grade | Pre | IV | III | V | III | IV | V | |
| 6 M | IV | IV | V | III | IV | V | ||
| Type of disc herniation | PT | SL | SL | PT | PT | SL | ||
| Size of disc herniation | No change | Reduced | No change | Disappeared | Reduced | Disappeared | ||
| Time to reoperation (month) | 12 | - | 7 | - | - | - | ||
| Number of patients | 26–228 | |
| Mean age (years) | 21.1–53.1 | |
| Sex (percentage of women) | 20.8–42.6 | |
| Location (%) | L1–2 | 0–1.9 |
| L2–3 | 0–6.1 | |
| L3–4 | 0–11.9 | |
| L4–5 | 40.6–73.5 | |
| L5–S1 | 26.5–48.3 | |
| Pfirrmann grade (%) | I | 0–1.2 |
| II | 3.1–38.2 | |
| III | 32.7–80.8 | |
| IV | 2.9–53.8 | |
| V | 0–4.4 | |
| Type of LDH (%) | Protrusion | 0–16.9 |
| Subligamentous | 43.8–72.3 | |
| Transligamentous | 0–56.3 | |
| Efficacy rate (%) | 61.8–85.4 | |
| Surgery rate (%) | 5.8–13.1 | |
| Mean decrease in disc height (%) | 10.1–20.0 | |
| Percentage of cases showing a change in Pfirrmann grade (%) | 38.6–61.5 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukui, H.; Kamei, N.; Fujiwara, Y.; Nakamae, T.; Ohta, R.; Kotaka, S.; Adachi, N. Intradiscal Condoliase Injection Therapy for Recurrent Lumbar Disc Herniation: Case Series and Literature Review. Medicina 2023, 59, 1561. https://doi.org/10.3390/medicina59091561
Fukui H, Kamei N, Fujiwara Y, Nakamae T, Ohta R, Kotaka S, Adachi N. Intradiscal Condoliase Injection Therapy for Recurrent Lumbar Disc Herniation: Case Series and Literature Review. Medicina. 2023; 59(9):1561. https://doi.org/10.3390/medicina59091561
Chicago/Turabian StyleFukui, Hiroki, Naosuke Kamei, Yasushi Fujiwara, Toshio Nakamae, Ryo Ohta, Shinji Kotaka, and Nobuo Adachi. 2023. "Intradiscal Condoliase Injection Therapy for Recurrent Lumbar Disc Herniation: Case Series and Literature Review" Medicina 59, no. 9: 1561. https://doi.org/10.3390/medicina59091561
APA StyleFukui, H., Kamei, N., Fujiwara, Y., Nakamae, T., Ohta, R., Kotaka, S., & Adachi, N. (2023). Intradiscal Condoliase Injection Therapy for Recurrent Lumbar Disc Herniation: Case Series and Literature Review. Medicina, 59(9), 1561. https://doi.org/10.3390/medicina59091561





