Oral Health Survey in Burundi; Evaluation of the Caries Experience in Schoolchildren Using the DMFT Index
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Methods
2.3. Data Collection and Analysis
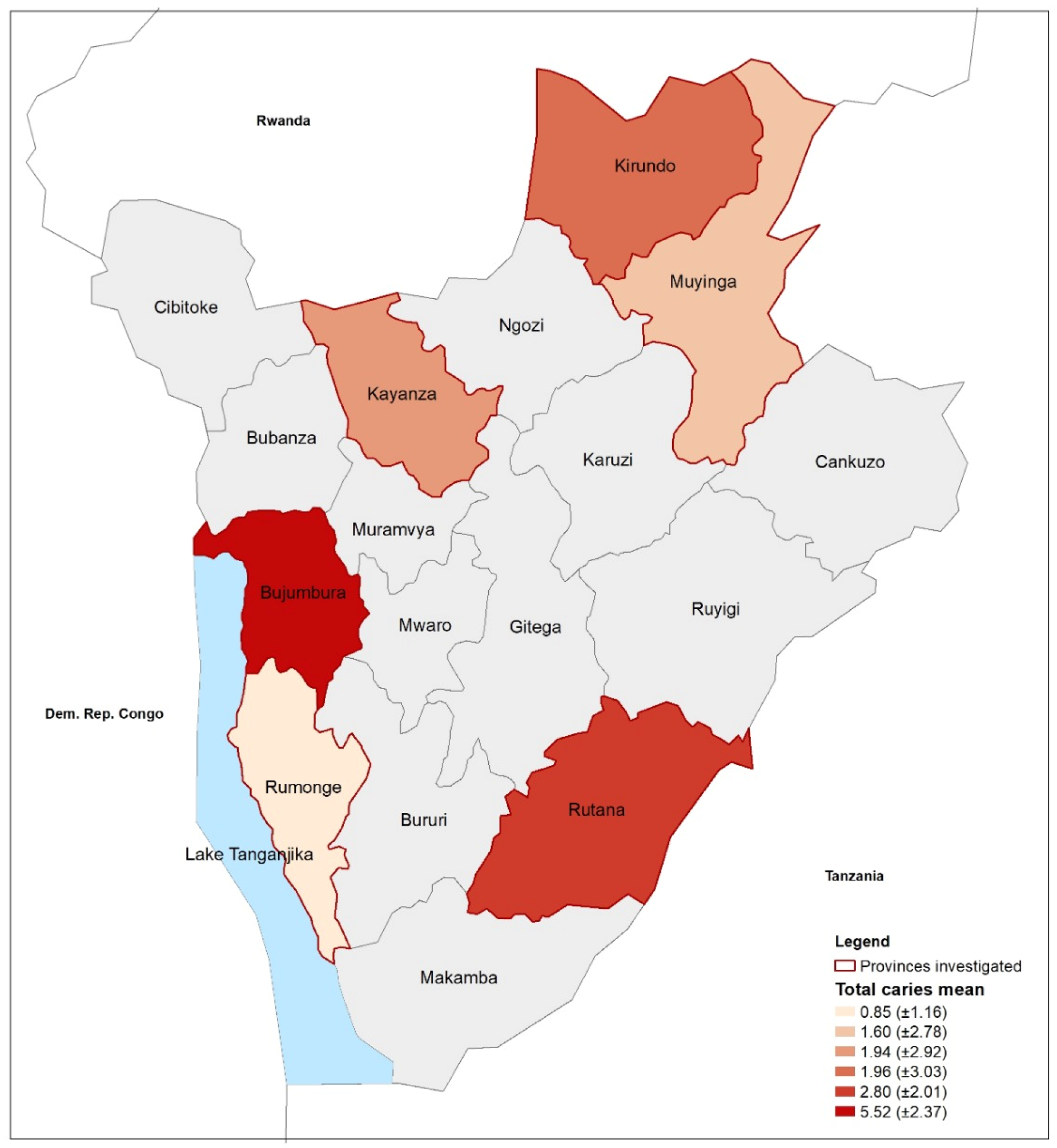
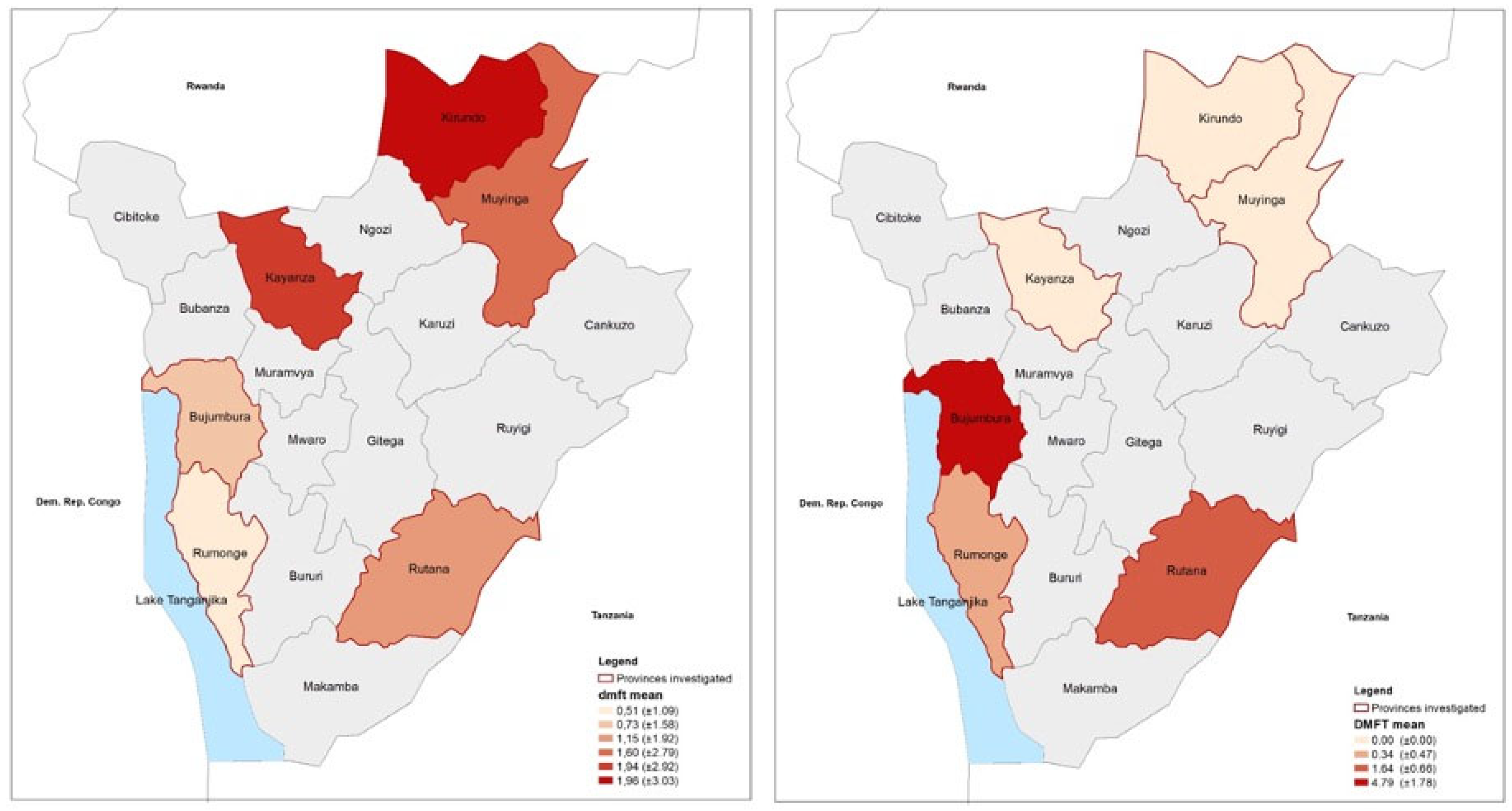
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Çolak, H.; Dülgergil, Ç.T.; Dalli, M.; Hamidi, M.M. Early Childhood Caries Update: A Review of Causes, Diagnoses, and Treatments. J. Nat. Sci. Biol. Med. 2013, 4, 29–38. [Google Scholar] [CrossRef]
- Elamin, A.; Garemo, M.; Mulder, A. Determinants of dental caries in children in the Middle East and North Africa region: A systematic review based on literature published from 2000 to 2019. BMC Oral Health 2021, 21, 237. [Google Scholar] [CrossRef]
- Teshome, A.; Muche, A.; Girma, B. Prevalence of Dental Caries and Associated Factors in East Africa, 2000-2020: Systematic Review and Meta-Analysis. Front. Public Health 2021, 9, 645091. [Google Scholar] [CrossRef] [PubMed]
- Lagerweij, M.D.; van Loveren, C. Declining Caries Trends: Are We Satisfied? Curr. Oral Health Rep. 2015, 2, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Bernabé, E.; Sheiham, A. Age, Period and Cohort Trends in Caries of Permanent Teeth in Four Developed Countries. Am. J. Public Health 2014, 104, e115–e121. [Google Scholar] [CrossRef] [PubMed]
- Yee, R.; Sheiham, A. The Burden of Restorative Dental Treatment for Children in Third World Countries. Int. Dent. J. 2002, 52, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tinanoff, N.; Kanellis, M.J.; Vargas, C.M. Current Understanding of the Epidemiology Mechanisms, and Prevention of Dental Caries in Preschool Children. Pediatr. Dent. 2002, 24, 543–551. [Google Scholar]
- Ayele, F.A.; Taye, B.W.; Ayele, T.A.; Gelaye, K.A. Predictors of Dental Caries among Children 7–14 Years Old in Northwest Ethiopia: A Community Based Cross-Sectional Study. BMC Oral Health 2013, 13, 7. [Google Scholar] [CrossRef]
- Petersen, P.E.; Bourgeois, D.; Ogawa, H.; Estupinan-Day, S.; Ndiaye, C. The Global Burden of Oral Diseases and Risks to Oral Health. Bull. World Health Organ. 2005, 83, 661–669. [Google Scholar]
- Zewdu, T.; Abu, D.; Agajie, M.; Sahilu, T. Dental caries and associated factors in Ethiopia: Systematic review and meta-analysis. Environ. Health Prev. Med. 2021, 26, 21. [Google Scholar] [CrossRef]
- Clauss, A.; Sie, A.; Zabre, P.; Schmoll, J.; Sauerborn, R.; Listl, S. Population-Based Prevalence of Oral Conditions as a Basis for Planning Community-Based Interventions: An Epidemiological Study from Rural Burkina Faso. Front. Public Health 2021, 9, 697498. [Google Scholar] [CrossRef]
- Mbawalla, H.S.; Nyamuryekung’e, K.K.; Mtaya-Mlangwa, M.; Masalu, J.R. Dental Caries Pattern Amongst Tanzanian Children: National Oral Health Survey. Int. Dent. J. 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Hewlett, S.A.; Blankson, P.K.; Aheto, J.M.K.; Anto, F.; Danso-Appiah, T.; Sackeyfio, J.; Koram, K.; Amoah, A.G.B. Assessment of oral health status in a Ghanaian population: Rationale, methods, and population characteristics. BMC Oral Health 2022, 22, 67. [Google Scholar] [CrossRef] [PubMed]
- Chikte, U.; Pontes, C.C.; Karangwa, I.; Kimmie-Dhansay, F.; Erasmus, R.; Kengne, A.P.; Matsha, T.E. Dental caries in a South African adult population: Findings from the Cape Town Vascular and Metabolic Health Study. Int. Dent. J. 2020, 70, 176–182. [Google Scholar] [CrossRef]
- World Bank GDP per Capita (Current US$)—Burundi|Data. Available online: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=BI (accessed on 6 April 2021).
- United Nations Development Programme—UNDP Human Development Index (HDI) Ranking|Human Development Reports. Available online: http://hdr.undp.org/en/content/latest-human-development-index-ranking (accessed on 6 April 2021).
- Burundi Ministry of Health République Du Burundi, Politique National de Santé 2016–2025. Available online: https://www.ilo.org/dyn/natlex/docs/ELECTRONIC/110854/138027/F1656560762/BDI-110854.pdf (accessed on 6 April 2021).
- Iyer, H.S.; Chukwuma, A.; Mugunga, J.C.; Manzi, A.; Ndayizigiye, M.; Anand, S. A Comparison of Health Achievements in Rwanda and Burundi. Health Hum. Rights 2018, 20, 199–211. [Google Scholar]
- Ahinkorah, B.O.; Seidu, A.-A.; Hagan, J.E.; Budu, E.; Mohammed, A.; Adu, C.; Ameyaw, E.K.; Adoboi, F.; Schack, T. Barriers to Healthcare Access and Healthcare Seeking for Childhood Illnesses among Childbearing Women in Burundi. PLoS ONE 2022, 17, e0274547. [Google Scholar] [CrossRef]
- Lambert-Evans, S.; Ponsar, F.; Reid, T.; Bachy, C.; Van Herp, M.; Philips, M. Financial Access to Health Care in Karuzi, Burundi: A Household-Survey Based Performance Evaluation. Int. J. Equity Health 2009, 8, 36. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.E.; Mattos Savage, G.C.; Crummey, S.C.; Sabbah, W.; Varenne, B.; Makino, Y. Oral Health Workforce in Africa: A Scarce Resource. Int. J. Environ. Res. Public Health 2023, 20, 2328. [Google Scholar] [CrossRef]
- Menegaz, A.M.; Silva, A.E.R.; Cascaes, A.M. Educational Interventions in Health Services and Oral Health: Systematic Review. Rev. Saude Publica 2018, 52, 52. [Google Scholar] [CrossRef] [PubMed]
- Kanoute, A.; Faye, D.; Bourgeois, D. Current Status of Oral Health Research in Africa: An Overview. Int. Dent. J. 2020, 62, 301–307. [Google Scholar] [CrossRef]
- Ramphoma, K.; Rampersad, N.; Singh, N.; Mukhari-Baloyi, N.; Naidoo, S. The Proposed Need for Integrated Maternal and Child Oral Health Policy: A Case of South Africa. Front. Oral Health 2022, 3, 1023268. [Google Scholar] [CrossRef] [PubMed]
- Hescot, P.; China, E.; Bourgeois, D.; Maina, S.; Monteiro da Silva, O.; Luc Eiselé, J.; Simpson, C.; Horn, V. The FDI African Strategy for Oral Health: Addressing the Specific Needs of the Continent. Int. Dent. J. 2020, 63, 113–120. [Google Scholar] [CrossRef]
- Global Health Observatory. Available online: https://www.who.int/data/gho (accessed on 12 July 2023).
- Lwanga, S.K.; Lemeshow, S.; World Health Organization. Sample Size Determination in Health Studies: A Practical Manual; World Health Organization: Geneva, Switzerland, 1991. [Google Scholar]
- Daniel, W.W.; Cross, C.L. Biostatistics: A Foundation for Analysis in the Health Sciences, 10th ed.; Wiley: Hoboken, NJ, USA, 2019; Available online: https://www.wiley.com/en-us/Biostatistics%3A+A+Foundation+for+Analysis+in+the+Health+Sciences%2C+10th+Edition-p-9781119625506 (accessed on 19 July 2023).
- World Health Organization. Oral Health Surveys: Basic Methods, 5th ed.; WHO: Geneva, Switzerland, 2013; Available online: https://www.who.int/publications-detail-redirect/9789241548649 (accessed on 12 July 2023).
- Teshome, A.; Yitayeh, A.; Gizachew, M. Prevalence of Dental Caries and Associated Factors Among Finote Selam Primary School Students Aged 12-20 Years, Finote Selam Town, Ethiopia. Oral Health Dent. Manag. 2016, 15, 36–41. [Google Scholar]
- Rwakatema, D.S.; Ananduni, K.N.; Katiti, V.W.; Msuya, M.; Chugulu, J.; Kapanda, G. Oral Health in Nursing Students at Kilimanjaro Christian Medical Centre Teaching Hospital in Moshi, Tanzania. BMC Oral Health 2015, 15, 23. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, M.; Vieira, A.R. Explaining Gender Differences in Caries: A Multifactorial Approach to a Multifactorial Disease. Int. J. Dent. 2010, 2010, 649643. [Google Scholar] [CrossRef]
- Pujar, P.; Subbareddy, V.V. Evaluation of the Tooth Brushing Skills in Children Aged 6–12 Years. Eur. Arch. Paediatr. Dent. 2013, 14, 213–219. [Google Scholar] [CrossRef]
- Ogunbodede, E.O.; Kida, I.A.; Madjapa, H.S.; Amedari, M.; Ehizele, A.; Mutave, R.; Sodipo, B.; Temilola, S.; Okoye, L. Oral Health Inequalities between Rural and Urban Populations of the African and Middle East Region. Adv. Dent. Res. 2015, 27, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Varenne, B.; Petersen, P.E.; Ouattara, S. Oral Health Behaviour of Children and Adults in Urban and Rural Areas of Burkina Faso, Africa. Int. Dent. J. 2006, 56, 61–70. [Google Scholar] [CrossRef]
- Kikwilu, E.N.; Frencken, J.E.; Mulder, J. Utilization of Toothpaste and Fluoride Content in Toothpaste Manufactured in Tanzania. Acta Odontol. Scand. 2008, 66, 293–299. [Google Scholar] [CrossRef]
- Mafuvadze, B.T.; Mahachi, L.; Mafuvadze, B. Dental Caries and Oral Health Practice among 12 Year Old School Children from Low Socio-Economic Status Background in Zimbabwe. Pan Afr. Med. J. 2013, 14, 164. [Google Scholar] [CrossRef] [PubMed]
- Simangwa, L.D.; Åstrøm, A.N.; Johansson, A.; Minja, I.K.; Johansson, A.-K. Oral Diseases and Oral Health Related Behaviors in Adolescents Living in Maasai Population Areas of Tanzania: A Cross-Sectional Study. BMC Pediatr. 2019, 19, 275. [Google Scholar] [CrossRef]
- Fantaye, W.; Bjorvatn, K.; Bårdsen, A. The Relationship between Dental Caries and Dental Fluorosis in Areas with Moderate-High Fluoride Drinking Water in Ethiopia. Community Dent. Oral Epidemiol. 2004, 32, 337–344. [Google Scholar] [CrossRef]
- Mwakayoka, H.; Masalu, J.R.; Namakuka Kikwilu, E. Dental Caries and Associated Factors in Children Aged 2–4 Years Old in Mbeya City, Tanzania. J. Dent. 2017, 18, 104–111. [Google Scholar]
- Diop, M.; Kanouté, A.; Diouf, M.; Ndiaye, A.D.; Lo, C.M.M.; Faye, D.; Cissé, D. The Role of Health Insurance in the Coverage of Oral Health Care in Senegal. J. Public Health Afr. 2018, 9, 772. [Google Scholar] [CrossRef]
- Eze, P.; Lawani, L.O.; Agu, U.J.; Acharya, Y. Catastrophic Health Expenditure in Sub-Saharan Africa: Systematic Review and Meta-Analysis. Bull. World Health Organ. 2022, 100, 337J–351J. [Google Scholar] [CrossRef]
- Uguru, N.; Onwujekwe, O.; Ogu, U.U.; Uguru, C. Access to Oral Health Care: A Focus on Dental Caries Treatment Provision in Enugu Nigeria. BMC Oral Health 2020, 20, 145. [Google Scholar] [CrossRef] [PubMed]
- Bhayat, A.; Chikte, U. Human Resources for Oral Health Care in South Africa: A 2018 Update. Int. J. Environ. Res. Public Health 2019, 16, 1668. [Google Scholar] [CrossRef]
- Kaguru, G.; Ayah, R.; Mutave, R.; Mugambi, C. Integrating Oral Health into Primary Health Care: A Systematic Review of Oral Health Training in Sub-Saharan Africa. J. Multidiscip. Healthc. 2022, 15, 1361–1367. [Google Scholar] [CrossRef]
- Friedman, J.W.; Mathu-Muju, K.R. Dental Therapists: Improving Access to Oral Health Care for Underserved Children. Am. J. Public Health 2014, 104, 1005–1009. [Google Scholar] [CrossRef]
- Yang, Y.T.; Chen, B.; Wanchek, T. Dental Therapists: A Solution to a Shortage of Dentists in Underserved Communities? Public Health Rep. 2017, 132, 285–288. [Google Scholar] [CrossRef]
- Edelstein, B.L. Examining Whether Dental Therapists Constitute a Disruptive Innovation in US Dentistry. Am. J. Public Health 2011, 101, 1831–1835. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Dörfer, C.E.; Schlattmann, P.; Foster Page, L.; Thomson, W.M.; Paris, S. Socioeconomic Inequality and Caries: A Systematic Review and Meta-Analysis. J. Dent. Res. 2015, 94, 10–18. [Google Scholar] [CrossRef]
- Abid, A.; Maatouk, F.; Berrezouga, L.; Azodo, C.; Uti, O.; El-Shamy, H.; Oginni, A. Prevalence and Severity of Oral Diseases in the Africa and Middle East Region. Adv. Dent. Res. 2015, 27, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Kiguli, J.; Alvesson, H.M.; Mayega, R.W.; Kasujja, F.X.; Muyingo, A.; Kirunda, B.; Ekirapa Kiracho, E.; Kayemba Nalwadda, C.; Naggayi, G.; Peterson, S.; et al. Dietary Patterns and Practices in Rural Eastern Uganda: Implications for Prevention and Management of Type 2 Diabetes. Appetite 2019, 143, 104409. [Google Scholar] [CrossRef]
- Steyn, N.P.; McHiza, Z.J. Obesity and the Nutrition Transition in Sub-Saharan Africa. Ann. N. Y. Acad. Sci. 2014, 1311, 88–101. [Google Scholar] [CrossRef] [PubMed]

| Sex | |||
|---|---|---|---|
| Males n (%) | Females n (%) | Total n (%) | |
| 6-year-olds | 476 (47.27) | 531 (52.73) | 1007 (52.94) |
| 12-year-olds | 430 (48.04) | 465 (51.96) | 895 (47.06) |
| Pearson χ2(1) = 0.11 p = 0.74 | |||
| Urban | 286 (46.89) | 324 (53.11) | 610 (32.07) |
| Rural | 620 (47.99) | 672 (52.01) | 1292 (67.93) |
| Pearson χ2(1) = 0.20 p = 0.65 | |||
| Kayanza | 125 (41.39) | 177 (58.61) | 302 (15.88) |
| Muyinga | 247 (49.30) | 254 (50.70) | 501 (26.34) |
| Kirundo | 152 (50.84) | 147 (49.16) | 299 (15.72) |
| Northern provinces | 524 (47.55) | 578 (52.45) | 1102 (57.94) |
| Rumonge | 149 (49.67) | 151 (50.33) | 300 (15.77) |
| Rutana | 136 (45.33) | 164 (54.67) | 300 (15.77) |
| Bujumbura | 97 (48.50) | 103 (51.50) | 200 (10.52) |
| Southern provinces | 382 (47.75) | 418 (52.25) | 800 (42.06) |
| Pearson χ2(5) = 7.70 p = 0.17 | |||
| (A) Primary Dentition | (B) Permanent Dentition | |||||||
| Males mean ± SD (range) | Females mean ± SD (range) | One-way ANOVA p-value | Sex | Males mean ± SD (range) | Females mean ± SD (range) | One-way ANOVA p-value | ||
| d | 1.25 ± 2.33 (0–13) | 1.33 ± 2.37 (0–16) | 0.51 | D | 0.71 ± 1.46 (0–9) | 0.89 ± 1.74 (0–12) | 0.01 | |
| m | 0.1 ± 0.43 (0–4) | 0.09 ± 0.48 (0–6) | 0.70 | M | 0.01 ± 0.13 (0–2) | 0.01 ± 0.12 (0–2) | 0.71 | |
| f | 0.01 ± 0.17 (0–5) | 0.00 ± 0.07 (0–2) | 0.66 | F | -- | 0.00 ± 0.03 (0–1) | -- | |
| dmft | 1.35 ± 2.47 (0–13) | 1.42 ± 2.50 (0–16) | 0.55 | DMFT | 0.72 ± 1.46 (0–9) | 0.90 ± 1.75 (0–12) | 0.02 | |
| 6-year-olds mean ± SD (range) | 12-year-olds mean ± SD (range) | One-way ANOVA p-value | Age groups | 6-year-olds mean ± SD (range) | 12-year-olds mean ± SD (range) | One-way ANOVA p-value | ||
| d | 2.28 ± 2.83 (0–16) | 0.18 ± 0.67 (0–7) | <0.01 | D | 0.28 ± 0.77 (0–6) | 1.39 ± 2.05 (0–12) | <0.01 | |
| m | 0.17 ± 0.59) (0–6) | 0.01 ± 0.17 (0–3) | <0.01 | M | 0.01 ± 0.10 (0–2) | 0.02 ± 0.15 (0–2) | 0.25 | |
| f | 0.01 ± 0.17 (0–5) | -- | -- | F | -- | 0.00 ± 0.03 (0–1) | -- | |
| dmft | 2.45 ± 2.97 (0–16) | 0.19 ± 0.70 (0–7) | <0.01 | DMFT | 0.29 ± 0.78 (0–6) | 1.41 ± 2.06 (0–12) | <0.01 | |
| Urban mean ± SD (range) | Rural mean ± SD (range) | One-way ANOVA p-value | Living Area | Urban mean ± SD (range) | Rural mean ± SD (range) | One-way ANOVA p-value | ||
| d | 1.03 ± 1.86 (0–11) | 1.41 ± 2.55 (0–16) | <0.01 | D | 0.35 ± 0.91 (0–7) | 1.02 ± 1.82 (0–12) | <0.01 | |
| m | 0.10 ± 0.51 (0–6) | 0.09 ± 0.42 (0–4) | 0.59 | M | 0.01 ± 0.09 (0–1) | 0.01 ± 0.14 (0–2) | 0.36 | |
| f | 0.01 ± 0.22 (0–5) | -- | -- | F | 0.00 ± 0.04 (0–1) | -- | -- | |
| dmft | 1.13 ± 2.02 (0–12) | 1.50 ± 2.68 (0–16) | <0.01 | DMFT | 0.36 ± 0.92 (0–7) | 1.03 ± 1.82 (0–12) | <0.01 | |
| Northern regions mean ± SD (range) | Southern regions mean ± SD (range) | One-way ANOVA p-value | Geographical regions | Northern regions mean ± SD (range) | Southern regions mean ± SD (range) | One-way ANOVA p-value | ||
| d | 1.70 ± 2.77 (0–16) | 0.73 ± 1.45 (0–10) | <0.01 | D | 1.17 ± 1.94 (0–12) | 0.30 ± 0.75 (0–6) | <0.01 | |
| m | 0.10 ± 0.48 (0–6) | 0.09 ± 0.42 (0–4) | 0.67 | M | 0.00 ± 0.05 (0–1) | 0.03 ± 0.19 (0–2) | <0.01 | |
| f | -- | 0.01 ± 0.19 (0–5) | F | -- | 0.00 ± 0.04 (0–1) | -- | ||
| dmft | 1.80 ± 2.89 (0–16) | 0.81 ± 1.60 (0–11) | <0.01 | DMFT | 1.17 ± 1.94 (0–12) | 0.32 ± 0.80 (0–6) | <0.01 | |
| Total Caries Experience | Bivariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Sex (females) | 1.19 (1.00–1.42) | 0.07 | 1.20 (1.00–1.47) | 0.06 |
| Age groups (12-year-olds) | 0.62 (0.52–0.75) | <0.01 | 0.52 (0.43–0.64) | <0.01 |
| Living area (Rural) | 1.76 (1.45–2.14) | <0.01 | 1.20 (0.96–1.49) | 0.104 |
| Geographical regions (Southern) | 0.26 (0.22–0.32) | <0.01 | 0.26 (0.21–0.32) | <0.01 |
| Living area/geographical provinces (Rural/Southern) | 0.48 (0.43–0.55) | <0.01 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamloum, D.; Dettori, M.; La Corte, P.; Agnoli, M.R.; Cappai, A.; Viarchi, A.; Arghittu, A.; Wolf, T.G.; Castiglia, P.; Campus, G. Oral Health Survey in Burundi; Evaluation of the Caries Experience in Schoolchildren Using the DMFT Index. Medicina 2023, 59, 1538. https://doi.org/10.3390/medicina59091538
Lamloum D, Dettori M, La Corte P, Agnoli MR, Cappai A, Viarchi A, Arghittu A, Wolf TG, Castiglia P, Campus G. Oral Health Survey in Burundi; Evaluation of the Caries Experience in Schoolchildren Using the DMFT Index. Medicina. 2023; 59(9):1538. https://doi.org/10.3390/medicina59091538
Chicago/Turabian StyleLamloum, Demetrio, Marco Dettori, Pino La Corte, Maria Ruth Agnoli, Andrea Cappai, Arianna Viarchi, Antonella Arghittu, Thomas Gerhard Wolf, Paolo Castiglia, and Guglielmo Campus. 2023. "Oral Health Survey in Burundi; Evaluation of the Caries Experience in Schoolchildren Using the DMFT Index" Medicina 59, no. 9: 1538. https://doi.org/10.3390/medicina59091538
APA StyleLamloum, D., Dettori, M., La Corte, P., Agnoli, M. R., Cappai, A., Viarchi, A., Arghittu, A., Wolf, T. G., Castiglia, P., & Campus, G. (2023). Oral Health Survey in Burundi; Evaluation of the Caries Experience in Schoolchildren Using the DMFT Index. Medicina, 59(9), 1538. https://doi.org/10.3390/medicina59091538









