Evaluation of Gait Parameters on Subjects with Hallux Limitus Using an Optogait Sensor System: A Case–Control Study
Abstract
1. Introduction
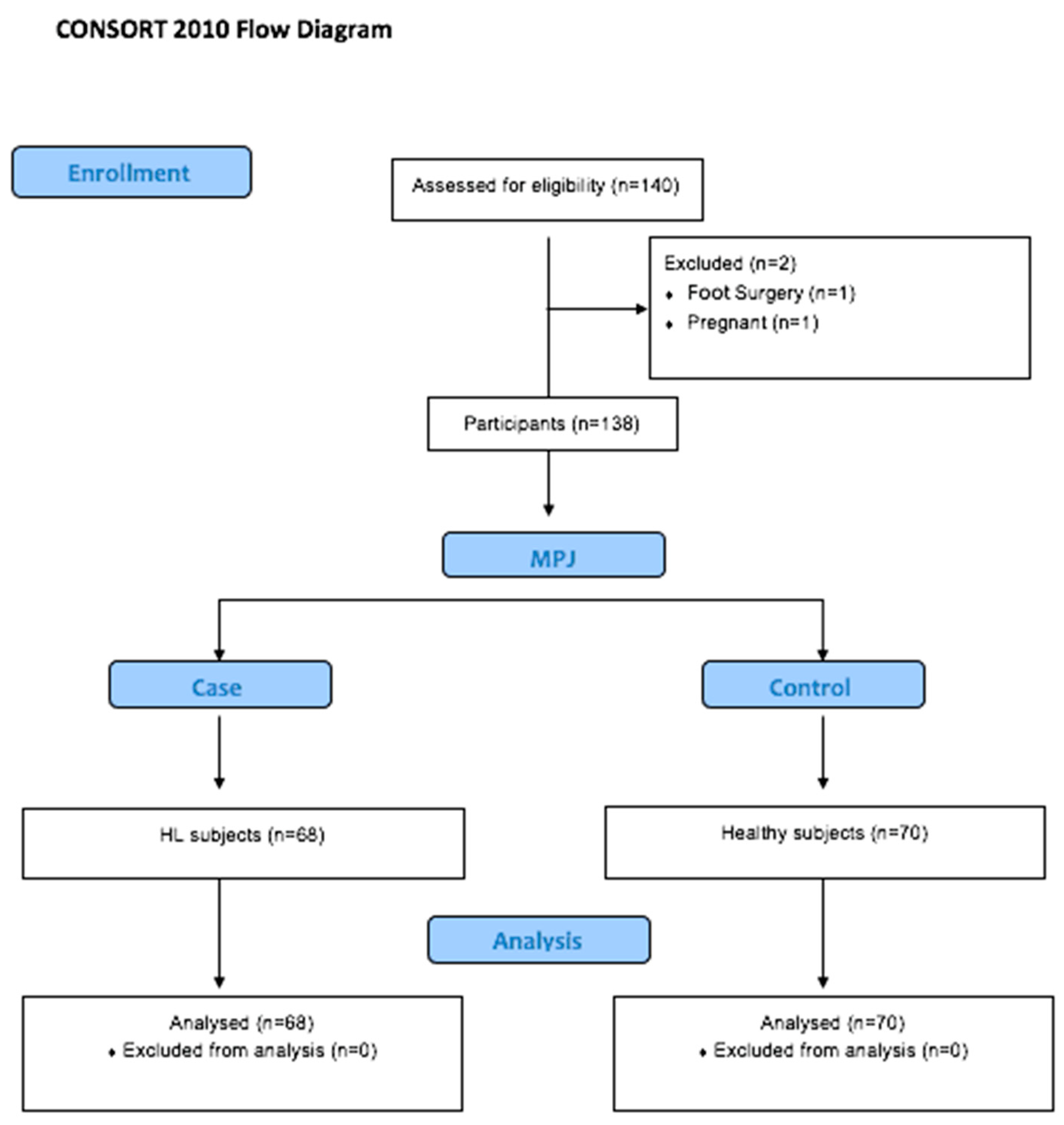
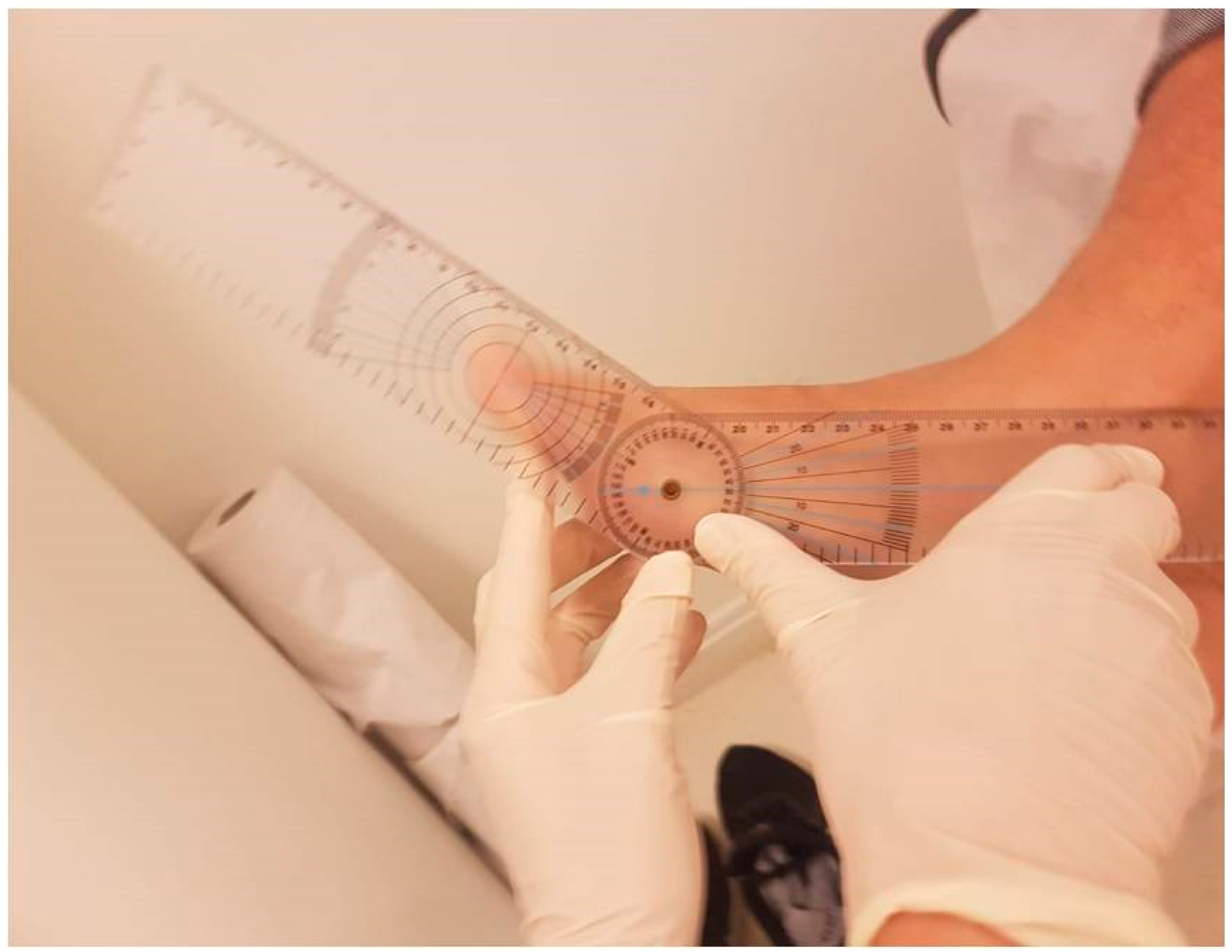
2. Materials and Methods
3. Results
Description of the Total Sample and by Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cuevas-Martínez, C.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Casado-Hernández, I.; Navarro-Flores, E.; Pérez-Palma, L.; Martiniano, J.; Gómez-Salgado, J.; López-López, D. Hallux Limitus Influence on Plantar Pressure Variations during the Gait Cycle: A Case-Control Study. Bioengineering 2023, 10, 772. [Google Scholar] [CrossRef] [PubMed]
- Dananberg, H.J. Gait style as an etiology to chronic postural pain. Part I. Functional hallux limitus. J. Am. Podiatr. Med. Assoc. 1993, 83, 433–441. [Google Scholar] [PubMed]
- Van Gheluwe, B.; Dananberg, H.J.; Hagman, F.; Vanstaen, K. Effects of hallux limitus on plantar foot pressure and foot kinematics during walking. J. Am. Podiatr. Med. Assoc. 2006, 96, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, M.J.; Shurnas, P.S. Hallux rigidus: Demographics, etiology, and radiographic assessment. Foot Ankle Int. 2003, 24, 731–743. [Google Scholar] [CrossRef] [PubMed]
- Senga, Y.; Nishimura, A.; Ito, N.; Kitaura, Y.; Sudo, A. Prevalence of and risk factors for hallux rigidus: A cross-sectional study in Japan. BMC Musculoskelet. Disord. 2021, 22, 786. [Google Scholar] [CrossRef]
- Cobos-Moreno, P.; Astasio-Picado, Á.; Gómez-Martín, B. Epidemiological Study of Foot Injuries in the Practice of Sport Climbing. Int. J. Environ. Res. Public. Health 2022, 19, 4302. [Google Scholar] [CrossRef]
- Roddy, E.; Thomas, M.J.; Marshall, M.; Rathod, T.; Myers, H.; Menz, H.B.; Thomas, E.; Peat, G. The population prevalence of symptomatic radiographic foot osteoarthritis in community-dwelling older adults: The clinical assessment study of the foot. Ann. Rheum. Dis. 2015, 74, 156–163. [Google Scholar] [CrossRef]
- Zlotoff, H.J.; Christensen, J.C.; Mendicino, R.W.; Schuberth, J.M.; Schwartz, N.H.; Thomas, J.L.; Weil, L.S. ACFAS Universal Foot and Ankle Scoring System: First Metatarsophalangeal Joint and First Ray (module 1). J. Foot Ankle Surg. 2002, 41, 2–5. [Google Scholar] [CrossRef]
- Hopson, M.M.; McPoil, T.G.; Cornwall, M. Motion of the first metatarsophalangeal joint. Reliability and validity of four measurement techniques. J. Am. Podiatr. Med. Assoc. 1995, 85, 198–204. [Google Scholar]
- Maceira, E.; Monteagudo, M. Functional hallux rigidus and the Achilles-calcaneus-plantar system. Foot Ankle Clin. 2014, 19, 669–699. [Google Scholar] [CrossRef]
- Halstead, J.; Turner, D.E.; Redmond, A.C. The relationship between hallux dorsiflexion and ankle joint complex frontal plane kinematics: A preliminary study. Clin. Biomech. 2005, 20, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Beeson, P.; Phillips, C.; Corr, S.; Ribbans, W.J. Hallux rigidus: A cross-sectional study to evaluate clinical parameters. Foot 2009, 19, 80–92. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zammit, G.V.; Menz, H.B.; Munteanu, S.E. Structural factors associated with hallux limitus/rigidus: A systematic review of case control studies. J. Orthop. Sports Phys. Ther. 2009, 39, 733–742. [Google Scholar] [CrossRef]
- Rudisch, J.; Jöllenbeck, T.; Vogt, L.; Cordes, T.; Klotzbier, T.J.; Vogel, O.; Wollesen, B. Agreement and consistency of five different clinical gait analysis systems in the assessment of spatiotemporal gait parameters. Gait Posture 2021, 85, 55–64. [Google Scholar] [CrossRef]
- Núñez-Trull, A.; Alvarez-Medina, J.; Jaén-Carrillo, D.; Roche-Seruendo, L.E.; Gómez-Trullén, E. Absolute agreement and consistency of the OptoGait system and Freemed platform for measuring walking gait. Med. Eng. Phys. 2022, 110, 103912. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.M.; Song, C.H.; Lee, K.J.; Jung, S.W.; Shin, D.C.; Shin, S.H. Concurrent Validity and Test-retest Reliability of the OPTOGait Photoelectric Cell System for the Assessment of Spatio-temporal Parameters of the Gait of Young Adults. J. Phys. Ther. Sci. 2014, 26, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Gomez Bernal, A.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E. Reliability of the OptoGait portable photoelectric cell system for the quantification of spatial-temporal parameters of gait in young adults. Gait Posture 2016, 50, 196–200. [Google Scholar] [CrossRef]
- Goss, D.A.; Long, J.; Carr, A.; Rockwell, K.; Cheney, N.A.; Law, T.D. Clinical Implications of a One-hand Versus Two-hand Technique in the Silfverskiöld Test for Gastrocnemius Equinus. Cureus 2020, 12, 6555. [Google Scholar] [CrossRef]
- Redmond, A.C.; Crosbie, J.; Ouvrier, R.A. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clin. Biomech. 2006, 21, 89–98. [Google Scholar] [CrossRef]
- Requelo-Rodríguez, I.; Castro-Méndez, A.; Jiménez-Cebrián, A.M.; González-Elena, M.L.; Palomo-Toucedo, I.C.; Pabón-Carrasco, M. Assessment of Selected Spatio-Temporal Gait Parameters on Subjects with Pronated Foot Posture on the Basis of Measurements Using OptoGait. A Case-Control Study. Sensors 2021, 21, 2805. [Google Scholar] [CrossRef]
- Herssens, N.; Verbecque, E.; Hallemans, A.; Vereeck, L.; Van Rompaey, V.; Saeys, W. Do spatiotemporal parameters and gait variability differ across the lifespan of healthy adults? A systematic review. Gait Posture 2018, 64, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Agner, S.; Bernet, J.; Brülhart, Y.; Radlinger, L.; Rogan, S. Spatiotemporal gait parameters during dual task walking in need of care elderly and young adults. A cross-sectional study. Z. Gerontol. Geriatr. 2015, 48, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Fung, J.; Sherman, A.; Stachura, S.; Eckles, R.; Doucette, J.; Chusid, E. Nonoperative Management of Hallux Limitus Using a Novel Forefoot Orthosis. J. Foot Ankle Surg. 2020, 59, 1192–1196. [Google Scholar] [CrossRef] [PubMed]
- Becerro-de-Bengoa Vallejo, R.; Sanchez Gómez, R.; Losa-Iglesias, M.E. Clinical improvement in functional hallux limitus using a cut-out orthosis. Prosthet. Orthot. Int. 2016, 40, 215–223. [Google Scholar] [CrossRef]
- Gordillo-Fernández, L.; Órtíz-Romero, M.; Valero-Salas, J.; Salcini-Macías, J.L.; Benhamu-Benhamu, S.; García-de-la-Peña, R.; Cervera-Marin, J.A. Effect by custom-made foot orthoses with added support under the first metatarso-phalangeal joint in hallux limitus patients: Improving on first metatarso-phalangeal joint extension. Orth. Prosthet. Int. 2016, 40, 668–674. [Google Scholar] [CrossRef]
- Menz, H.B.; Auhl, M.; Tan, J.M.; Levinger, P.; Roddy, E.; Munteanu, S.E. Biomechanical Effects of Prefabricated Foot Orthoses and Rocker-Sole Footwear in Individuals with First Metatarsophalangeal Joint Osteoarthritis. Arthritis Care Res. 2016, 68, 603–611. [Google Scholar] [CrossRef]
- Vallotton, J. Hallux limitus fonctionnel: Le pied qui fatigue et qui use [Functional hallux limitus (Fhl): A new explanation for overuse pathologies]. Rev. Med. Suisse 2014, 10, 2333–2337. [Google Scholar]
- Taranto, J.; Taranto, M.J.; Bryant, A.R.; Singer, K.P. Analysis of dynamic angle of gait and radiographic features in subjects with hallux abducto valgus and hallux limitus. J. Am. Podiatr. Med. Assoc. 2007, 97, 175–188. [Google Scholar] [CrossRef]
- Canseco, K.; Long, J.; Marks, R.; Khazzam, M.; Harris, G. Quantitative characterization of gait kinematics in patients with hallux rigidus using the Milwaukee foot model. J. Orthop. Res. 2008, 26, 419–427. [Google Scholar] [CrossRef]
- Galois, L.; Girard, D.; Martinet, N.; Delagoutte, J.P.; Mainard, D. Analyse opto-électronique de la marche après arthrodèsemétatarso-phalangienne de l’hallux: À propos de 15 cas [Optoelectronic gait analysis after metatarsophalangeal arthrodesis of the hallux: Fifteen cases]. Rev. Chir. Orthop. Reparatrice. Appar. Mot. 2006, 92, 52–59. [Google Scholar] [CrossRef]
- Allan, J.; McClelland, J.A.; Munteanu, S.E.; Buldt, A.K.; Landorf, K.B.; Roddy, E.; Auhl, M.; Menz, H.B. First metatarsophalangeal joint range of motion is associated with lower limb kinematics in individuals with first metatarsophalangeal joint osteoarthritis. J. Foot Ankle Res. 2020, 13, 33. [Google Scholar] [CrossRef] [PubMed]
- Muchna, A.; Najafi, B.; Wendel, C.S.; Schwenk, M.; Armstrong, D.G.; Mohler, J. Foot Problems in Older Adults Associations with Incident Falls, Frailty Syndrome, and Sensor-Derived Gait, Balance, and Physical Activity Measures. J. Am. Podiatr. Med. Assoc. 2018, 108, 126–139. [Google Scholar] [CrossRef] [PubMed]
| Sample n = 138 | Group | |||
|---|---|---|---|---|
| Case n = 68 | Control n = 70 | p-Value | ||
| Gender Female | 92 (66.7%) | 44 (64.70%) | 48 (68.6%) | p = 0.630 a |
| BMI (kg/m2) | 22.20 (5.12) | 21.90 (5.20) | 22.80 (3.50) | p = 0.436 b |
| Age | 25.86 (10.95) | 23.03 (8.86) | 28.60 (12.08) | p = 0.001 b |
| ROM MPJ right foot (degrees) | 67.00 (38.00) | 52.00 (10.00) | 90.00 (14.50) | p = 0.001 b |
| ROM MPJ left foot (degrees) | 75.00 (30.00) | 60.00 (11.00) | 90.00 (24.00) | p = 0.001 b |
| FPI right foot | 6.00 (3.00) | 7.00 (1.00) | 6.00 (3.00) | p = 0.012 a |
| FPI left foot | 5.00 (1.00) | 5.00 (3.00) | 6.00 (3.00) | p = 0.590 b |
| ROM right ankle (degrees) | 11.50 (12.00) | 9.00 (7.00) | 15.00 (9.00) | p = 0.001 b |
| ROM left ankle (degrees) | 11.00 (12.00) | 8.00 (4.00) | 15.00 (8.00) | p = 0.001 b |
| Sample N = 138 | Group | |||
|---|---|---|---|---|
| Case n = 68 | Control n = 70 | p-Value | ||
| Right foot stride length (cm) | 61.20 (6.90) | 64.50 (5.40) | 59.20 (6.02) | p = 0.001 * |
| Left foot stride length (cm) | 61.15 (6,60) | 62.95 (5.20) | 58.20 (6.58) | p = 0.001 * |
| Ground contact time (loading time) | ||||
| right foot sec Step (%) | 0.55 (0.05) 70.90 (6.63) | 0.57 (0.04) 69.30 (3.30) | 0.53 (0.06) 69.00 (3.03) | p = 0.041 * p = 0.460 |
| Ground contact time (loading time) | ||||
| left foot sec Step (%) Gait cycle sec Gait cadence | 0.55 (0.05) 70.60 (6.00) 1.10 (0.10) 108.50 (8.83) | 0.57 (0.04) 69.80 (2.40) 1.14 (0.09) 106.40 (13.20) | 0.53 (0.06) 68.65 (2.90) 1.07 (0.05) 112.20 (3.70) | p = 0.003 * p = 0.081 p = 0.001 * p = 0.001 * |
| Passage time difference | 0.32 (3.75) | 0.30 (4.25) | 0.45 (3.52) | p = 0.040 * |
| Step length difference (cm) | 0.45 (6.00) | 0.40 (8.25) | 0.50 (5.35) | p = 0.255 |
| Total stride (cm) | 123.00 (11.50) | 127.80 (8.75) | 118.40 (12.03) | p = 0.001 * |
| Difference load response | −1.40 (6.32) | 0.30 (4.75) | 2.20 (9.43) | p = 0.027 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro-Méndez, A.; Canca-Sánchez, F.J.; Pabón-Carrasco, M.; Jiménez-Cebrián, A.M.; Córdoba-Fernández, A. Evaluation of Gait Parameters on Subjects with Hallux Limitus Using an Optogait Sensor System: A Case–Control Study. Medicina 2023, 59, 1519. https://doi.org/10.3390/medicina59091519
Castro-Méndez A, Canca-Sánchez FJ, Pabón-Carrasco M, Jiménez-Cebrián AM, Córdoba-Fernández A. Evaluation of Gait Parameters on Subjects with Hallux Limitus Using an Optogait Sensor System: A Case–Control Study. Medicina. 2023; 59(9):1519. https://doi.org/10.3390/medicina59091519
Chicago/Turabian StyleCastro-Méndez, Aurora, Francisco Javier Canca-Sánchez, Manuel Pabón-Carrasco, Ana María Jiménez-Cebrián, and Antonio Córdoba-Fernández. 2023. "Evaluation of Gait Parameters on Subjects with Hallux Limitus Using an Optogait Sensor System: A Case–Control Study" Medicina 59, no. 9: 1519. https://doi.org/10.3390/medicina59091519
APA StyleCastro-Méndez, A., Canca-Sánchez, F. J., Pabón-Carrasco, M., Jiménez-Cebrián, A. M., & Córdoba-Fernández, A. (2023). Evaluation of Gait Parameters on Subjects with Hallux Limitus Using an Optogait Sensor System: A Case–Control Study. Medicina, 59(9), 1519. https://doi.org/10.3390/medicina59091519






