Trends for Percutaneous Tracheostomy in Italian Acute Care Setting over a 5-Year Period
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Statistical Analysis
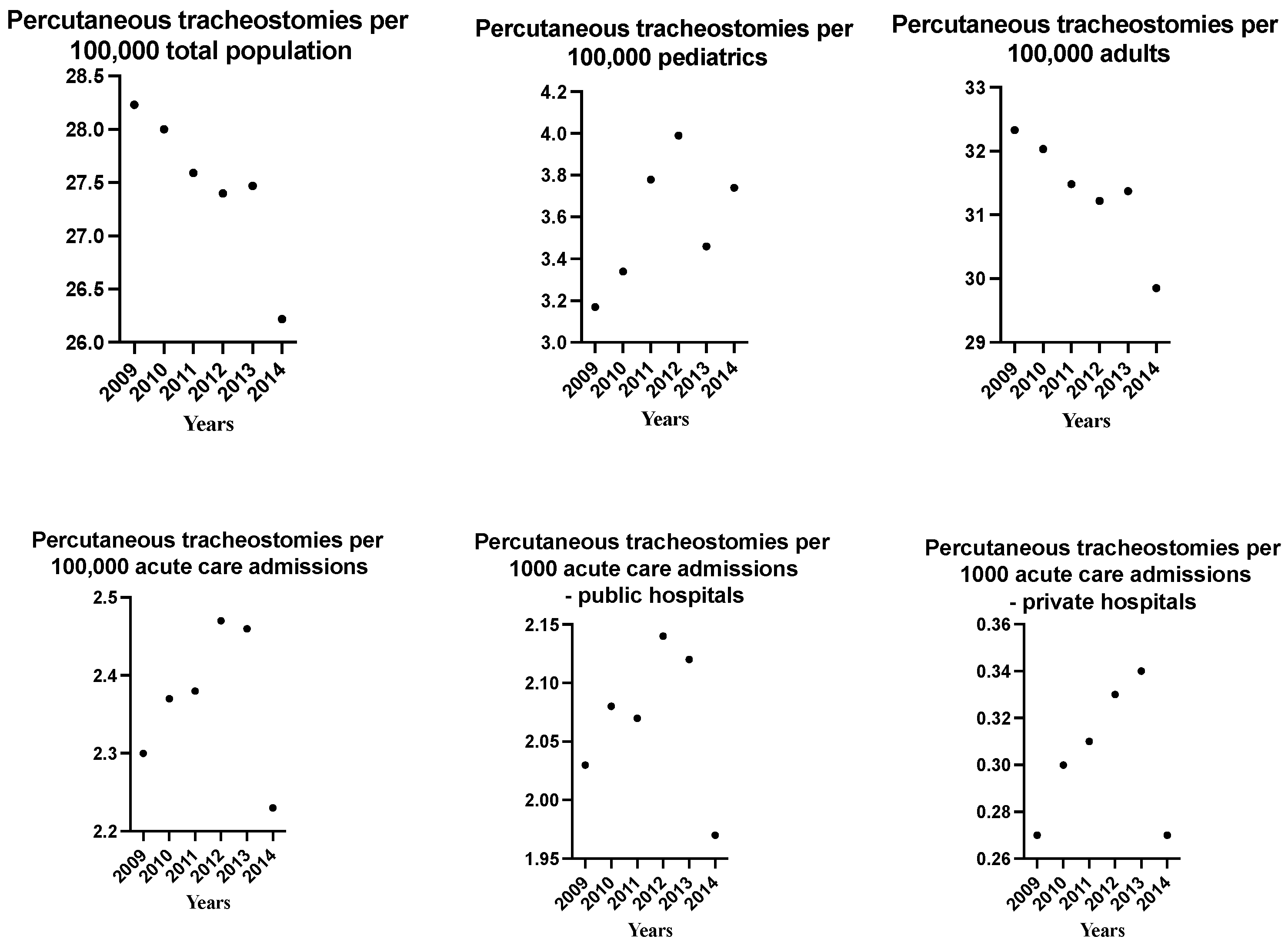
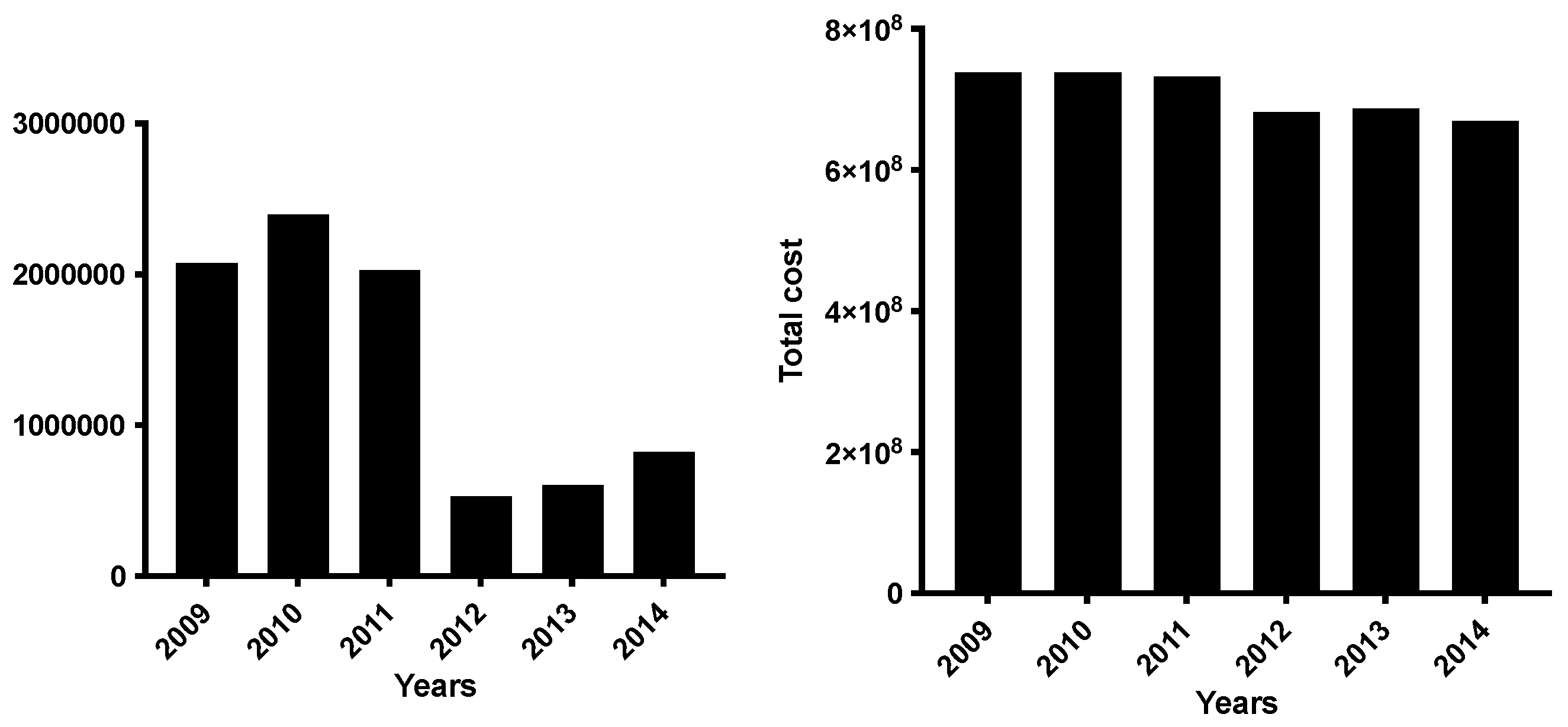
3. Results
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mahmood, K.; Wahidi, M.M. The changing role for tracheostomy in patients requiring mechanical ventilation. Clin. Chest Med. 2016, 37, 741–751. [Google Scholar] [CrossRef] [PubMed]
- Vargas, M.; Pelosi, P.; Tessitore, G.; Aloj, F.; Brunetti, I.; Arditi, E.; Salami, D.; Kacmarek, R.M.; Servillo, G. Percutaneous dilatational tracheostomy with a double-lumen endotracheal tube: A comparison of feasibility, gas exchange, and airway pressures. Chest 2015, 147, 1267–1274. [Google Scholar] [CrossRef] [PubMed]
- Langerman, A.; Patel, R.M.; Cohen, E.E.; Blair, E.A.; Stenson, K.M. Airway management before chemoradiation for advanced head and neck cancer. Head Neck 2012, 34, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Hashemain, S.M.R.; Digaleh, H.A. A prospective randomized study comparing mini-surgical percutaneous dilatational tracheostomy with surgical and classical percutaneous approach. Medicine 2015, 47, e2015. [Google Scholar] [CrossRef] [PubMed]
- McGrath, B.A.; Wilkinson, K. The NCEPOD study: On the right trach? Lessons for the anesthetist. Br. J. Anaesth. 2015, 115, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, K.A.; Martin, I.C.; Freeth, H.; Kelly, K.; Mason, M. NCEPOD. On the Right Trach? 2014. Available online: www.ncepod.org.uk/2014tc.htm (accessed on 30 July 2023).
- Mehta, A.B.; Syeda, S.N.; Bajpayee, L.; Cooke, C.R.; Walkey, A.J.; Wiener, R.S. Trends in tracheostomy for mechanically ventilated patients in the United States, 1993–2012. Am. J. Respir. Crit. Care Med. 2015, 192, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Diagnosis Related Groups Classification. Version 24. Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_1094_allegato.pdf (accessed on 30 July 2023).
- Annual Discharge Report. Italian Ministry of Health. Available online: http://www.salute.gov.it/ (accessed on 30 July 2023).
- Vargas, M.; Servillo, G.; Tessitore, G.; Aloj, F.; Brunetti, I.; Arditi, E.; Salami, D.; Kacmarek, R.M.; Pelosi, P. Double lumen endotracheal tube for percutaneous tracheostomy. Respir. Care 2014, 59, 1652–1659. [Google Scholar] [CrossRef] [PubMed]
- Nyanzi, D.J.; Atwine, D.; Kamoga, R.; Birungi, C.; Nansubuga, C.A.; Nyaiteera, V.; Nakku, D. Tracheostomy-related indications, early complications and their predictors among patients in low resource settings: A prospective cohort study in the pre-COVID-19 era. BMC Surg. 2023, 23, 59. [Google Scholar] [CrossRef] [PubMed]
- Vargas, M.; Servillo, G.; Arditi, E.; Brunetti, I.; Pecunia, L.; Salami, D.; Putensen, C.; Antonelli, M.; Pelosi, P. Tracheostomy in Intensive Care Unit: A national survey in Italy. Minerva Anestesiol. 2013, 79, 156–164. [Google Scholar] [PubMed]
- Mehta, A.B.; Cooke, C.R.; Soylemez, R.W.; Walkey, A.J. Hospital variation in early tracheostomy in the United States: A population based study. Crit. Care Med. 2016, 44, 1506–1514. [Google Scholar] [CrossRef] [PubMed]
- Cheung, N.H.; Napolitano, L.M. Tracheostomy: Epidemiology, indications, timing, technique, and outcomes. Respir. Care 2014, 59, 895–919. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, R.; Tizon, A.I.; Gnzales, J.; Monedero, P.; Garcia-Sanchez, M.; De-la-Torre, M.V.; Ibenez, P.; Frutos, F.; De-nogal, F.; Gomez, M.J.; et al. Intensive care unit discharge to the ward with a tracheostomy cannula as a risk factors for mortality: A prospective, multicenter propensity analysis. Crit. Care Med. 2011, 39, 2240–2245. [Google Scholar] [CrossRef] [PubMed]
- El Solh, A.A.; Ramadan, F.H. Overview of respiratory failure in older adults. J. Intensive Care Med. 2006, 21, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Vargas, M.; Sutherasan, Y.; Brunetti, I.; Micalizzi, C.; Insorsi, A.; Ball, L.; Folentino, M.; Sileo, R.; De Lucia, A.; Cerana, M.; et al. Mortality and long-term quality of life after percutaneous tracheotomy in Intensive Care Unit: A prospective observational study. Minerva Anestesiol. 2018, 84, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Kerlin, M.P.; Cooke, C.R. Understanding costs when seeking value in critical care. Ann. Am. Thorac. Soc. 2015, 12, 1743–1744. [Google Scholar] [CrossRef] [PubMed]
- Halpern, S.D.; Becker, D.; Curtis, J.R.; Fowler, R.; Hyzy, R.; Kapln, L.J.; Rawat, N.; Sessler, C.N.; Wunsch, H.; Kahn, J.M. An Official American Thoracic Society/American Association of Critical-Care Nurses/American College of Chest Physicians/Society of Critical Care Medicine Policy Statement: The Choosing Wisely® Top 5 List in Critical Care Medicine. Am. J. Respir. Crit. Care Med. 2014, 7, 818–826. [Google Scholar] [CrossRef]
- Cox, E.C.; Carson, S.S.; Holmes, G.M.; Howard, A.; Carey, T.S. Increase in tracheostomy for prolonged mechanical ventilation in North Carolina, 1993–2002. Crit. Care Med. 2004, 32, 2219–2226. [Google Scholar] [CrossRef]
- Altman, K.W.; Banoff, K.M.; Tong, C.C.L. Medical economic impact of tracheostomy patients on hospital system. J. Med. Econ. 2015, 18, 28–62. [Google Scholar] [CrossRef] [PubMed]
| Year | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | p |
|---|---|---|---|---|---|---|---|
| Percutaneous Tracheostomies (n) | 16,953 | 16,893 | 16,726 | 16,274 | 16,394 | 15,938 | 6.6 × 10−11 |
| Age, | 1.38 × 10−6 | ||||||
| Mean (SD) | 65 (24) | 65 (18) | 64 (19) | 64 (18) | 64 (17) | 64 (17) | |
| ≤65 yr % | 79.87 | 79.77 | 79.71 | 79.17 | 78.82 | 78.59 | |
| 66–84 yr % | 17.60 | 17.59 | 17.53 | 17.95 | 18.18 | 18.35 | |
| ≥85 yr % | 2.53 | 2.64 | 2.76 | 2.88 | 3.00 | 3.06 | |
| Gender % | |||||||
| M | 62.3 | 62.0 | 62.6 | 62.6 | 62.6 | 63.2 | 0.0544 |
| F | 37.7 | 38.0 | 37.4 | 37.4 | 37.4 | 36.8 | |
| Length of ICU stay | |||||||
| ≤20 ds % | 25.3 | 25.0 | 25.5 | 26.7 | 26.9 | 26.6 | 5.52 × 10−5 |
| 21–39 ds % | 32.8 | 32.5 | 32.7 | 33.6 | 33.6 | 33.7 | 0.0161 |
| ≥40 ds % | 41.9 | 42.5 | 41.8 | 39.7 | 39.5 | 39.7 | 7.56 × 10−8 |
| Hospital type, | |||||||
| Public % | 88.11 | 88.31 | 87.54 | 87.21 | 86.62 | 86.21 | 0.0221 |
| Private with reimbursement % | 11.84 | 11.67 | 12.44 | 12.77 | 13.35 | 13.73 | 1.03 × 10−10 |
| Private without reimbursement % | 0.05 | 0.02 | 0.02 | 0.012 | 0.03 | 0.06 | 0.705 |
| Hospital region, | |||||||
| North % | 50.8 | 49.2 | 49.4 | 48.7 | 46.6 | 46.7 | 2.22 × 10−10 |
| Mid % | 21.3 | 22.5 | 22.4 | 22.7 | 23.1 | 23.1 | 0.000313 |
| South % | 27.9 | 28.3 | 28.2 | 28.6 | 30.3 | 30.2 | 4.47 × 10−7 |
| Year | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | p |
|---|---|---|---|---|---|---|---|
| LOS, mean (SD) | 43 (35) | 43 (36) | 43 (40) | 42 (38) | 42 (39) | 41 (36) | <2 × 10−16 * |
| Total duration of stay, days | 724,713 | 732,025 | 727,954 | 684,119 | 684,226 | 661,277 | <2 × 10−16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vargas, M.; Buonanno, P.; De Simone, S.; Russo, G.; Iacovazzo, C.; Servillo, G. Trends for Percutaneous Tracheostomy in Italian Acute Care Setting over a 5-Year Period. Medicina 2023, 59, 1444. https://doi.org/10.3390/medicina59081444
Vargas M, Buonanno P, De Simone S, Russo G, Iacovazzo C, Servillo G. Trends for Percutaneous Tracheostomy in Italian Acute Care Setting over a 5-Year Period. Medicina. 2023; 59(8):1444. https://doi.org/10.3390/medicina59081444
Chicago/Turabian StyleVargas, Maria, Pasquale Buonanno, Stefania De Simone, Gennaro Russo, Carmine Iacovazzo, and Giuseppe Servillo. 2023. "Trends for Percutaneous Tracheostomy in Italian Acute Care Setting over a 5-Year Period" Medicina 59, no. 8: 1444. https://doi.org/10.3390/medicina59081444
APA StyleVargas, M., Buonanno, P., De Simone, S., Russo, G., Iacovazzo, C., & Servillo, G. (2023). Trends for Percutaneous Tracheostomy in Italian Acute Care Setting over a 5-Year Period. Medicina, 59(8), 1444. https://doi.org/10.3390/medicina59081444






