Polymicrobial Bacterial Meningitis in a Patient with Chronic Suppurative Otitis Media: Case Report and Literature Review
Abstract
1. Introduction
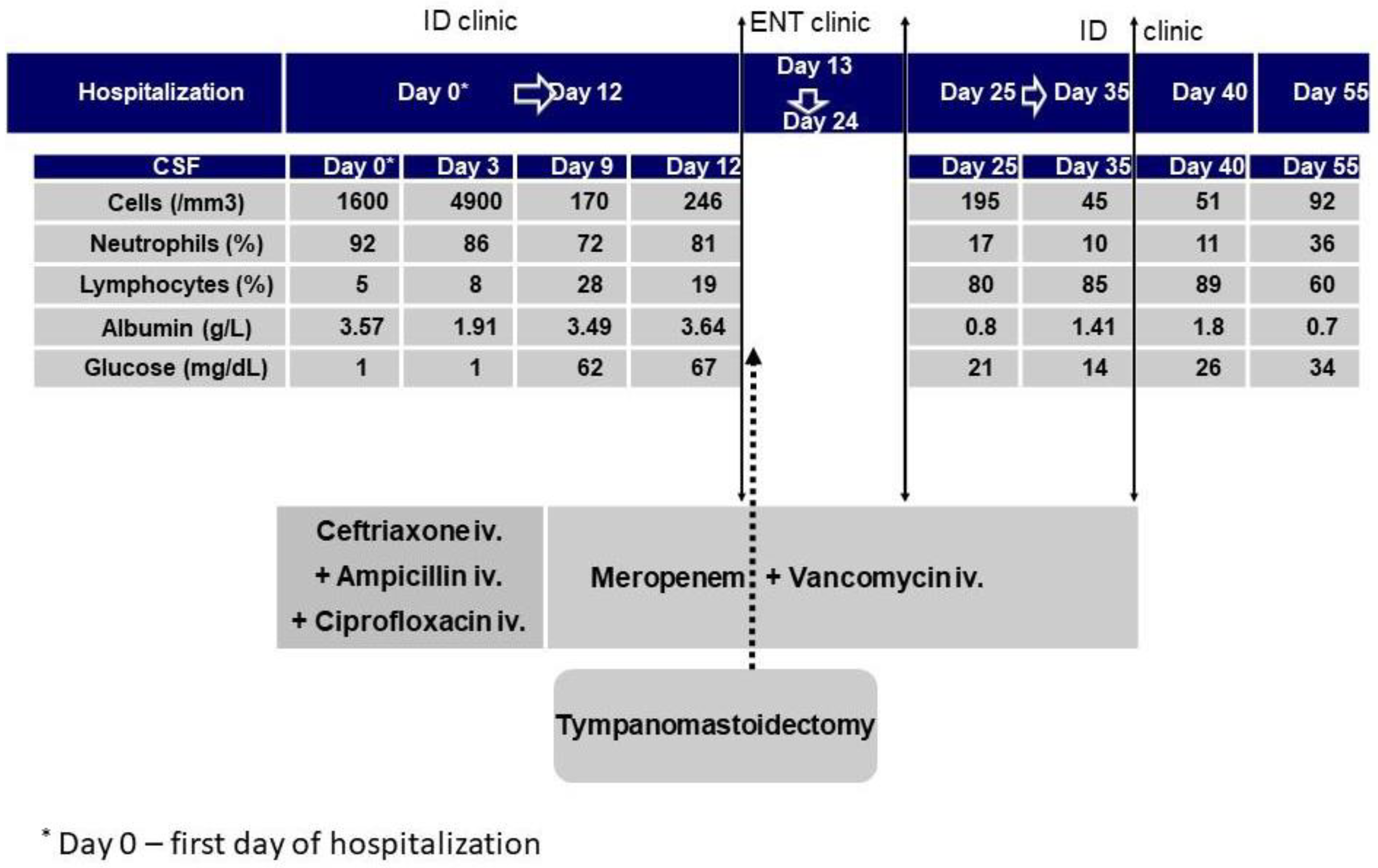
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, X.; Du, H.; Song, Z.; Wang, H.; Long, X. Polymicrobial Anaerobic Meningitis Detected by Next-Generation Sequencing: Case Report and Review of the Literature. Front. Med. 2022, 9, 840910. [Google Scholar] [CrossRef]
- Al Qahtani, H.M.; Aljoqiman, K.S.; Arabi, H.; Al Shaalan, H.; Singh, S. Fatal Meningitis in a 14-Month-Old with Currarino Triad. Case Rep. Radiol. 2016, 2016, 1346895. [Google Scholar] [CrossRef]
- Gutierrez, M.; Emmanuel, P.J. Expanding Molecular Diagnostics for Central Nervous System Infections. Adv. Pediatr. 2018, 65, 209–227. [Google Scholar] [CrossRef]
- Sharma, N.; Jaiswal, A.A.; Banerjee, P.K.; Garg, A.K. Complications of Chronic Suppurative Otitis Media and Their Management: A Single Institution 12 Years Experience. Indian J. Otolaryngol. Head Neck Surg. 2015, 67, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-J.; Lien, C.-Y.; Chien, C.-C.; Huang, C.-R.; Tsai, N.-W.; Chang, C.-C.; Lu, C.-H.; Chang, W.-N. Anaerobic bacterial meningitis in adults. J. Clin. Neurosci. 2018, 50, 45–50. [Google Scholar] [CrossRef]
- Heintz, E.; Pettengill, M.A.; Gangat, M.A.; Hardy, D.J.; Bonnez, W.; Sobhanie, M.M. Oral flora meningoencephalitis diagnosis by next-generation DNA sequencing. Access Microbiol. 2019, 1, e000056. [Google Scholar] [CrossRef]
- Neal, T.W.; Schlieve, T. Complications of Severe Odontogenic Infections: A Review. Biology 2022, 11, 1784. [Google Scholar] [CrossRef]
- Woodhouse, A. Bacterial meningitis and brain abscess. Medicine 2021, 49, 667–674. [Google Scholar] [CrossRef]
- Wang, S.; Peng, L.; Gai, Z.; Zhang, L.; Jong, A.; Cao, H.; Huang, S.-H. Pathogenic Triad in Bacterial Meningitis: Pathogen Invasion, NF-κB Activation, and Leukocyte Transmigration that Occur at the Blood-Brain Barrier. Front. Microbiol. 2016, 7, 148. [Google Scholar] [CrossRef] [PubMed]
- Vata, L. Ghrelin effects on local renin angiotensin from pulmonary vessels. Acta Endocrinol. 2010, 6, 295–304. [Google Scholar] [CrossRef]
- McGill, F.; Heyderman, R.S.; Panagiotou, S.; Tunkel, A.R.; Solomon, T. Acute bacterial meningitis in adults. Lancet 2016, 388, 3036–3047. [Google Scholar] [CrossRef]
- Morrison, A.; Weir, I.; Silber, T. Otogenic Fusobacterium Meningitis, Sepsis, and Mastoiditis in an Adolescent. South. Med. J. 2004, 97, 416–418. [Google Scholar] [CrossRef] [PubMed]
- Glimåker, M.; Naucler, P.; Sjölin, J. Etiology, clinical presentation, outcome and the effect of initial management in immunocompromised patients with community acquired bacterial meningitis. J. Infect. 2020, 80, 291–297. [Google Scholar] [CrossRef]
- Van de Beek, D.; Cabellos, C.; Dzupova, O.; Esposito, S.; Klein, M.; Kloek, A.T.; Leib, S.L.; Mourvillier, B.; Ostergaard, C.; Pagliano, P.; et al. ESCMID guideline: Diagnosis and treatment of acute bacterial meningitis. Clin. Microbiol. Infect. 2016, 3, S37–S62. [Google Scholar] [CrossRef] [PubMed]
- Klapa, S.; Grefer, J.; Sobottka, I.; Kurowski, V. A 56-Year-Old Woman with Chronic Hepatitis C Liver Disease and Meningitis due to Streptococcus equi subsp. Zooepidemicus. Case Rep. Crit. Care 2021, 2021, 7227054. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.-Y.; Yang, F.-C.; Lee, J.-T.; Wang, C.-W. Streptococcus anginosus, tooth extraction and brain abscess. Qjm Int. J. Med. 2013, 107, 671–672. [Google Scholar] [CrossRef]
- Maritsa, S.-H.; Mouhib, N.; Tariq, C. 720: A little Streptococcus anginosus goes a long way: A strange case of meningitis. Crit. Care Med. 2019, 47, 340. [Google Scholar]
- Castillo, Y.; Delgadillo, N.A.; Neuta, Y.; Hernández, A.; Acevedo, T.; Cárdenas, E.; Montaño, A.; Lafaurie, G.I.; Castillo, D.M. Antibiotic Susceptibility and Resistance Genes in Oral Clinical Isolates of Prevotella intermedia, Prevotella nigrescens, and Prevotella melaninogenica. Antibiotics 2022, 11, 888. [Google Scholar] [CrossRef]
- Al Majid, F.; Aldrees, A.; Barry, M.; Binkhamis, K.; Allam, A.; Almohaya, A. Streptococcus anginosus group infections: Management and outcome at a tertiary care hospital. J. Infect. Public Health 2020, 13, 1749–1754. [Google Scholar] [CrossRef]
- Olender, A.; Bogut, A.; Bańska, A. The role of opportunistic “Corynebacterium” spp. in human infections. Eur. J. Clin. Exp. Med. 2019, 7, 157–161. [Google Scholar] [CrossRef]
- Zhang, M.J.; Cao, X.J.; Fan, J.; Yin, Z.G.; Yu, K. Corynebacterium striatum meningitis combined with suspected brain and lung abscesses: A case report and review. BMC Infect. Dis. 2020, 20, 389. [Google Scholar] [CrossRef]
- Dragomirescu, C.C.; Lixandru, B.E.; Coldea, I.L.; Corneli, O.N.; Pana, M.; Palade, A.M.; Cristea, V.C.; Suciu, I.; Suciu, G.; Manolescu, L.S.C.; et al. Antimicrobial Susceptibility Testing for Corynebacterium Species Isolated from Clinical Samples in Romania. Antibiotics 2020, 9, 31. [Google Scholar] [CrossRef]
- Park, Y.; Choi, J.Y.; Yong, D.; Lee, K.; Kim, J.M. Clinical features and prognostic factors of anaerobic infections: A 7-year ret-rospective study. Korean J. Intern. Med. 2009, 24, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Finegold, S. Host factors predisposing to anaerobic infections. FEMS Immunol. Med. Microbiol. 1993, 6, 159–163. [Google Scholar] [CrossRef]
- Siegler, D.; Faiers, M.C.; Willis, A.T. Bacteroides meningitis complicating chronic mastoiditis. Postgrad. Med. J. 1982, 58, 560–561. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hawkey, P.M.; Jewes, L.A. How common is meningitis caused by anaerobic bacteria? J. Clin. Microbiol. 1985, 22, 325. [Google Scholar] [CrossRef]
- Lien, C.-Y.; Huang, C.-R.; Tsai, W.-C.; Hsu, C.-W.; Tsai, N.-W.; Chang, C.-C.; Lu, C.-H.; Chien, C.-C.; Chang, W.-N. Epidemiologic trend of adult bacterial meningitis in southern Taiwan (2006–2015). J. Clin. Neurosci. 2017, 42, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Shah, H.N.; Collins, D.M. Prevotella, a New Genus to Include Bacteroides Melaninogenicus and Related Species Formerly Classified in the Genus Bacteroides. Int. J. Syst. Bacteriol. 1990, 40, 205–208. [Google Scholar] [CrossRef]
- Bancescu, G.; Didilescu, A.; Bancescu, A.; Bari, M. Antibiotic susceptibility of 33 Prevotella strains isolated from Romanian patients with abscesses in head and neck spaces. Anaerobe 2015, 35 Pt A, 41–44. [Google Scholar] [CrossRef]
- Brook, I. Prevotella intermedia meningitis associated with cerebrospinal fluid leakage in an adolescent. Pediatr. Infect. Dis. J. 2003, 22, 751–753. [Google Scholar] [CrossRef]
- Könönen, E.; Fteita, D.; Gursoy, U.K.; Gursoy, M. Prevotella species as oral residents and infectious agents with potential impact on systemic conditions. J. Oral Microbiol. 2022, 14, 2079814. [Google Scholar] [CrossRef] [PubMed]
- Kalay, G.; Dalgic, N.; Bozan, T.; Toprak, N.U.; Bayraktar, B.; Soyletir, G. Polymicrobial anaerobic meningitis caused by Bacteroides fragilis, Bacteroides thetaiotaomicron, Fusobacterium necrophorum and Slackia exigua in a patient with mastoiditis following otitis media. Anaerobe 2019, 56, 95–97. [Google Scholar] [CrossRef]
- Pittman, M.E.; Thomas, B.S.; Wallace, M.A.; Weber, C.J.; Burnham, C.-A.D. Routine Testing for Anaerobic Bacteria in Cerebrospinal Fluid Cultures Improves Recovery of Clinically Significant Pathogens. J. Clin. Microbiol. 2014, 52, 1824–1829. [Google Scholar] [CrossRef]
- Garcia, M.; Hirata, M.; Hossain, D.N.; Kunz, A. Prevotella melaninogenica Meningitis and Abscess: Normal Flora in an Abnormal Location. Pediatrics 2018, 142, 602. [Google Scholar] [CrossRef]
- Mittal, M.K.; Zimmerman, R.A. Meningitis and Epidural Abscess Related to Pansinusitis. Pediatr. Emerg. Care 2009, 25, 267–268. [Google Scholar] [CrossRef]
- Luca, C.; Mihalache, D.; Luca, V.; Turcu, T. The clinical picture, treatment and prognosis of meningitis due to anaerobic and nonfermentative bacteria. Rev. Med. Chir. Soc. Med. Nat. Iasi 1999, 103, 158–160. [Google Scholar] [PubMed]
- Miftode, E.; Vâţă, A.; Leca, D.; Hurmuzache, M.; Dorneanu, O.; Manciuc, C.; Luca, V.; Dorobăţ, C. Community acquired acute bacterial meningitis—A 10 years review. Rev. Med. Chir. Soc. Med. Nat. Iasi 2009, 113, 402–409. [Google Scholar] [PubMed]
- Mo, S.; Wei, L.; Chen, H.; Li, R.; Li, S.; Luo, G. A chinese case of prevotella intermedia and streptococcus constellatus intracranial mixed infection. Metab. Brain Dis. 2018, 33, 161–166. [Google Scholar] [CrossRef]
- Llitjos, J.-F.; Mongardon, N.; Loubinoux, J.; Sonneville, R.; Charpentier, J.; Pène, F.; Mira, J.-P. Polymicrobial anaerobic meningitis. Med. Mal. Infect. 2016, 46, 230–232. [Google Scholar] [CrossRef]
- Ganeshalingham, A.; Buckley, D.; Shaw, I.; Freeman, J.T.; Wilson, F.; Best, E. Bacteroides fragilis concealed in an infant with Escherichia coli meningitis. J. Paediatr. Child. Health 2014, 50, 78–80. [Google Scholar] [CrossRef]
- Luo, L.; Wang, C.; Shen, N.; Zhao, R.; Tao, Y.; Mo, X.; Cao, Q. Polymicrobial anaerobic bacterial meningitis secondary to dermal sinus: A case report. Transl. Pediatr. 2021, 10, 3118–3123. [Google Scholar] [CrossRef] [PubMed]
- Bergeron, E.; Roux, A.; Demers, J.; Vanier, L.E.; Moore, L. A 40-Year-Old Woman with Cauda Equina Syndrome Caused by Rectothecal Fistula Arising from an Anterior Sacral Meningocele. Neurosurgery 2010, 67, E1464–E1467. [Google Scholar] [CrossRef] [PubMed]
- Guerin, J.; Leibinger, F.; Raskine, L.; Ekherian, J. Polymicrobial meningitis revealing an anterior sacral meningocele in a 23-year-old woman. J. Infect. 2000, 40, 195–197. [Google Scholar] [CrossRef] [PubMed]
- Jeltema, H.-R.; Broens, P.M.A.; Brouwer, O.F.; Groen, R.J.M. Severe bacterial meningitis due to an enterothecal fistula in a 6-year-old child with Currarino syndrome: Evaluation of surgical strategy with review of the literature. Child’s Nerv. Syst. 2019, 35, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Chun, C.; Sacks, B.; Jao, J. Polymicrobial feculent meningitis. Clin. Infect. Dis. 1995, 21, 693–694. [Google Scholar] [CrossRef] [PubMed]
- García-Lechuz, J.M.; Hernangómez, S.; San Juan, R.; Bouza, E. Feculent meningitis: Polymicrobial meningitis in colorectal surgery. Diagn. Microbiol. Infect. Dis. 2000, 38, 169–170. [Google Scholar] [CrossRef]
- Walsh, T.J.; Weinstein, R.A.; Malinoff, H.; Breyer, M.D.; Berelowitz, B.A. Meningorectal fistula as a cause of polymicrobial anaerobic meningitis. Am. J. Clin. Pathol. 1982, 78, 127–130. [Google Scholar] [CrossRef]
- Thyss, J.; Chabert, J.M.; Bocquet, J.P.; Gazaix, M.; Korn, M.; Carles, D.; Etesse, H. Méningite post-opératoire plurimicrobienne à germes aérobies et anaérobies traitée par l’ornidazole. Nouv. Press. Med. 1980, 9, 381. [Google Scholar]
- Schartz, D.A.; Polacco, M.A.; Holmgren, E.P.; McCool, R.R. A Rare Case of Odontogenic Chronic Suppurative Otitis Media. Cureus 2019, 11, e4284. [Google Scholar] [CrossRef]
- Niemelä, S.; Lempinen, L.; Löyttyniemi, E.; Oksi, J.; Jero, J. Bacterial meningitis in adults: A retrospective study among 148 patients in an 8-year period in a university hospital, Finland. BMC Infect. Dis. 2023, 23, 45. [Google Scholar] [CrossRef]
- Cheng, H.; Xu, L.; Yang, F.; Jia, L.; Zhao, D.; Li, H.; Liu, W.; Li, Y.; Liu, X.; Geng, X.; et al. Case report: Meningitis and intracranial aneurysm caused by mixed infection of oral microflora dominated by anaerobes. Front. Neurol. 2022, 13, 889838. [Google Scholar] [CrossRef]
- Anderson, A.C.; von Ohle, C.; Frese, C.; Boutin, S.; Bridson, C.; Schoilew, K.; Peikert, S.A.; Hellwig, E.; Pelz, K.; Wittmer, A.; et al. The oral microbiota is a reservoir for antimicrobial resistance: Resistome and phenotypic resistance characteristics of oral biofilm in health, caries, and periodontitis. Ann. Clin. Microbiol. Antimicrob. 2023, 22, 37. [Google Scholar] [CrossRef] [PubMed]
- Barie, P.S.; Narayan, M.; Jose, V.M.A.; Shapiro, M.J. Antibiotic Use in the Intensive Care Unit: The Old and the New. In Current Therapy of Trauma and Surgical Critical Care; Elsevier: Amsterdam, The Netherlands, 2023; pp. 803–814.e1. [Google Scholar]
- Rubinstein, E.; Keynan, Y. Vancomycin Revisited—60 Years Later. Front. Public Health 2014, 2, 217. [Google Scholar] [CrossRef] [PubMed]
- Tunkel, A.R.; Hasbun, R.; Bhimraj, A.; Byers, K.; Kaplan, S.L.; Scheld, W.M.; van de Beek, D.; Bleck, T.P.; Garton, H.J.L.; Zunt, J.R. 2017 Infectious Diseases Society of America’s Clinical Practice Guidelines for Healthcare-Associated Ventriculitis and Meningitis. Clin. Infect. Dis. 2017, 64, e34–e65. [Google Scholar] [CrossRef] [PubMed]
| Sample | Bacteria | Susceptibility | |
|---|---|---|---|
| Sensible | Resistant | ||
| CSF | Streptococcus anginosus group | PEN, CRO, CTX, MXF, TEC, VA | - |
| Corynebacterium spp. | PEN, CLI, RIF, VA, LIN | - | |
| Prevotella spp. | AMX, AMC, TIC, TPZ, IPM, CLI, MXF, RIF | PEN, MTR | |
| Ear drainage | Proteus mirabilis | AMP, AMC, AMS, SXT, CTX, CAZ, GEN | - |
| Enterococcus faecalis | AMP i.v | - | |
| Author | Gender/Age | Comorbidities | Microorganisms | Treatment | Evolution |
|---|---|---|---|---|---|
| Li et al., 2022 [1] | F/16 years | Sinusitis | CSF: Porphyromonas gingivalis, Prevotella enoeca, Campylobacter rectus, Fusobacterium uncleatum, Actinomyces israelii | Ceftriaxone/ Vancomycin/ Metronidazole | Favorable |
| Kalay et al., 2019 [32] | M/16 years | Mastoiditis | CSF: Bacteroides fragilis, Bacteroides thetaiotaomicron, Fusobacterium necrophorum, Slackia exigua | Metronidazole/ Meropenem | Favorable |
| Mo et al., 2018 [38] | M/48 years | Cerebral infarction Possible sinusitis | CSF: Prevotella intermedia and Streptococcus constellatus | Ceftriaxone | Unknown |
| Mittal et al., 2009 [35] | F/11 years | Pansinusitis Epidural abscess | CSF: negative culture Sinus fluid cultures: Staphylococcus aureus, alpha hemolytic streptococci, Eikenella spp.; Prevotella intermedia, Fusobacterium spp, Peptostreptococcus anaerobius. | Cefotaxime + vancomycin/ ceftriaxone + metroniddazole + surgery | Favorable |
| Llitjos et al., 2017 [39] | F/69 years | None relevant | CSF: Peptostreptococcus micros, Fusobacterium necrophorum, Porphyromonas gingivalis, Campylobacter rectus | High-dose amoxicillin/ metronidazole | Death on day 47 |
| Ganeshalingham et al., 2014 [40] | M/8-week | None | CSF: E. coli, Bacteroides fragilis | Ceftriaxone/ Amoxicillin | Death |
| Luo et al., 2021 [41] | M/9-month | Lumbar dermal sinus | CSF: Finegoldia magna, Campylobacter ureolyticus, Bacteroides fragilis, Porphyromonas bennonis | Vancomycin/ ceftriaxone/ meropenem/ metronidazole | Favorable |
| Bergeron et al., 1980 [42] | F /40 years | Anterior sacral meningocele | CSF: Escherichia coli, group F streptococci, Bacteroides fragilis, Peptostreptococcus anaerobius, Candida glabrata | Ceftazidime/ metronidazole + surgery | Favorable |
| Guerin et al., 2000 [43] | F/23 years | Anterior sacral meningocele | CSF: Enterococcus faecalis, Streptococcus constelatus, Prevotella bivia | Vancomycin/ metronidazole/ cefotaxime/ piperacillin/tazobactam | |
| Jeltema et al., 2019 [44] | F/6 years | Currarino syndrome | CSF: Streptococcus anginosus (milleri), Bacteroides fragilis. | Broad-spectrum antibiotics + surgery | |
| Chun et al., 1995 [45] | M/56 years | Colon cancer | Non—perfringens Clostridium spp., Peptostreptococcus spp., Veillonela spp. | Penicillin G/ ceftriaxone/ metronidazole | Favorable |
| García-Lechuz et al, 2000 [46] | M/68 years | Rectal cancer | Bacteroides fragilis, MRSA, Morganella morgagnii | Vancomycin/ meropenem | |
| Walsh et al., 1982 [47] | F/49 years | Rectal cancer | Bacteroides fragilis, Bacteroides thetaiotaomicron, Bacteroides melaninogenicus, Clostridium ramosum, C. clostridiforme, Peptostreptococcus anaerobius | Ampicillin/ penicillin/ chloramphenicole/ metronidazole | Death after 5 months |
| Thyss et al., 1980 [48] | F/67 years | Not known | Streptococcus mitior, Bacteroides fragilis, Eubacterium lentum | Ornidazole | Favorable |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vâţă, A.; Irimie-Băluţă, E.; Roşu, F.M.; Onofrei, I.M.; Loghin, I.I.; Perţea, M.; Avădanei, A.N.; Miron, M.; Rădulescu, L.; Eşanu, I.; et al. Polymicrobial Bacterial Meningitis in a Patient with Chronic Suppurative Otitis Media: Case Report and Literature Review. Medicina 2023, 59, 1428. https://doi.org/10.3390/medicina59081428
Vâţă A, Irimie-Băluţă E, Roşu FM, Onofrei IM, Loghin II, Perţea M, Avădanei AN, Miron M, Rădulescu L, Eşanu I, et al. Polymicrobial Bacterial Meningitis in a Patient with Chronic Suppurative Otitis Media: Case Report and Literature Review. Medicina. 2023; 59(8):1428. https://doi.org/10.3390/medicina59081428
Chicago/Turabian StyleVâţă, Andrei, Erika Irimie-Băluţă, Florin Manuel Roşu, Ioana Maria Onofrei, Isabela Ioana Loghin, Mihaela Perţea, Andrei Nicolae Avădanei, Mihnea Miron, Luminiţa Rădulescu, Irina Eşanu, and et al. 2023. "Polymicrobial Bacterial Meningitis in a Patient with Chronic Suppurative Otitis Media: Case Report and Literature Review" Medicina 59, no. 8: 1428. https://doi.org/10.3390/medicina59081428
APA StyleVâţă, A., Irimie-Băluţă, E., Roşu, F. M., Onofrei, I. M., Loghin, I. I., Perţea, M., Avădanei, A. N., Miron, M., Rădulescu, L., Eşanu, I., & Luca, C. M. (2023). Polymicrobial Bacterial Meningitis in a Patient with Chronic Suppurative Otitis Media: Case Report and Literature Review. Medicina, 59(8), 1428. https://doi.org/10.3390/medicina59081428







