Traumatic Brain Injury and Related Antisocial Behavioral Outcomes: A Systematic Review
Abstract
1. Introduction
- How TBI is related to aggression and antisocial behavior;
- The role of biopsychosocial predisposing factors;
- Neuroanatomical correlates of criminal and aggressive behavior;
- The correlation between younger TBI and psychiatric comorbidity.
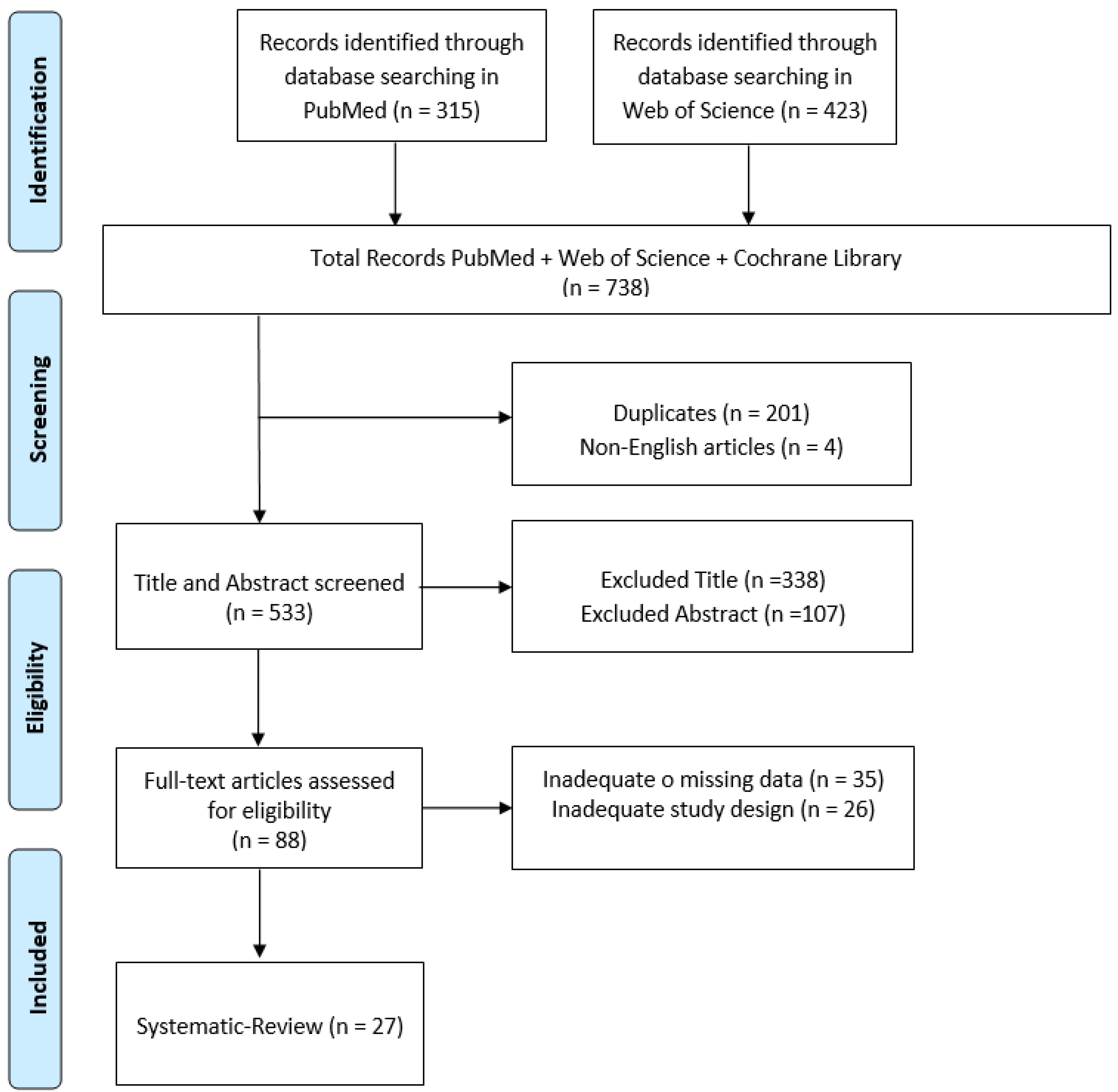
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
3. Results
3.1. TBI, Aggression and Antisocial Behavior
3.2. The Role of Biopsychosocial Predisposing Factors
3.3. Neuroanatomical Correlates of Criminal and Aggressive Behavior
3.4. Correlation between Younger TBI, Psychiatric Comorbidity and Aggression
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schofield, P.W.; Malacova, E.; Preen, D.B.; D’Este, C.; Tate, R.; Reekie, J.; Wand, H.; Butler, T. Does Traumatic Brain Injury Lead to Criminality? A Whole-Population Retrospective Cohort Study Using Linked Data. PLoS ONE 2015, 10, e0132558. [Google Scholar] [CrossRef]
- Linden, M.A.; O’Rourke, C.; Lohan, M. Traumatic brain injury and social competence among young male offenders. Disabil. Rehabil. 2020, 42, 2422–2429. [Google Scholar] [CrossRef] [PubMed]
- Dyer, K.F.; Bell, R.; McCann, J.; Rauch, R. Aggression after traumatic brain injury: Analysing socially desirable responses and the nature of aggressive traits. Brain Inj. 2006, 20, 1163–1173. [Google Scholar] [CrossRef]
- Connolly, E.J.; McCormick, B.F. Mild Traumatic Brain Injury and Psychopathology in Adolescence: Evidence From the Project on Human Development in Chicago Neighborhoods. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2019, 65, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, M.G.; Salas-Wright, C.P.; John, R.; Holzer, K.J.; Qian, Z.; Veeh, C. Traumatic Brain Injury and Psychiatric Co-Morbidity in the United States. Psychiatr. Q. 2019, 90, 151–158. [Google Scholar] [CrossRef]
- Bellesi, G.; Barker, E.D.; Brown, L.; Valmaggia, L. Pediatric traumatic brain injury and antisocial behavior: Are they linked? A systematic review. Brain Inj. 2019, 33, 1272–1292. [Google Scholar] [CrossRef] [PubMed]
- van Goozen, S.H.M.; Langley, K.; Hobson, C.W. Childhood Antisocial Behavior: A Neurodevelopmental Problem. Annu. Rev. Psychol. 2022, 73, 353–377. [Google Scholar] [CrossRef] [PubMed]
- van Reekum, R.; Bolago, I.; Finlayson, M.A.; Garner, S.; Links, P.S. Psychiatric disorders after traumatic brain injury. Brain Inj. 1996, 10, 319–327. [Google Scholar] [CrossRef]
- Rogers, J.M.; Read, C.A. Psychiatric comorbidity following traumatic brain injury. Brain Inj. 2007, 21, 1321–1333. [Google Scholar] [CrossRef] [PubMed]
- Capizzi, A.; Woo, J.; Verduzco-Gutierrez, M. Traumatic Brain Injury: An Overview of Epidemiology, Pathophysiology, and Medical Management. Med. Clin. N. Am. 2020, 104, 213–238. [Google Scholar] [CrossRef]
- McKinlay, A.; Albicini, M. Prevalence of traumatic brain injury and mental health problems among individuals within the criminal justice system. Concussion 2016, 1, CNC25. [Google Scholar] [CrossRef] [PubMed]
- Robinson, C.P. Moderate and Severe Traumatic Brain Injury. Continuum 2021, 27, 1278–1300. [Google Scholar] [CrossRef] [PubMed]
- Hawley, P.H. Strategies of control, aggression, and morality in preschoolers: An evolutionary perspective. J. Exp. Child Psychol. 2003, 85, 213–235. [Google Scholar] [CrossRef] [PubMed]
- Colantonio, A.; Stamenova, V.; Abramowitz, C.; Clarke, D.; Christensen, B. Brain injury in a forensic psychiatry population. Brain Inj. 2007, 21, 1353–1360. [Google Scholar] [CrossRef]
- Baguley, I.J.; Cooper, J.; Felmingham, K. Aggressive behavior following traumatic brain injury: How common is common? J. Head Trauma Rehabil. 2006, 21, 45–56. [Google Scholar] [CrossRef]
- Veeh, C.A.; Renn, T.; Vaughn, M.G.; DeLisi, M. Traumatic brain injury, temperament, and violence in incarcerated youth: A mediation analysis based on Delisi and Vaughn’s theory of temperament and antisocial behavior. Psychol. Crime Law 2018, 24, 1016–1029. [Google Scholar] [CrossRef]
- Williams, W.H.; Cordan, G.; Mewse, A.J.; Tonks, J.; Burgess, C.N. Self-reported traumatic brain injury in male young offenders: A risk factor for re-offending, poor mental health and violence? Neuropsychol. Rehabil. 2010, 20, 801–812. [Google Scholar] [CrossRef]
- Darby, R.R. Neuroimaging abnormalities in neurological patients with criminal behavior. Curr. Neurol. Neurosci. Rep. 2018, 18, 47. [Google Scholar] [CrossRef]
- Glenn, A.L.; Raine, A. Neurocriminology: Implications for the punishment, prediction and prevention of criminal behaviour. Nature reviews. Neuroscience 2014, 15, 54–63. [Google Scholar] [CrossRef]
- Cristofori, I.; Zhong, W.; Mandoske, V.; Chau, A.; Krueger, F.; Strenziok, M.; Grafman, J. Brain Regions Influencing Implicit Violent Attitudes: A Lesion-Mapping Study. J. Neurosci. Off. J. Soc. Neurosci. 2016, 36, 2757–2768. [Google Scholar] [CrossRef]
- Timonen, M.; Miettunen, J.; Hakko, H.; Zitting, P.; Veijola, J.; von Wendt, L.; Räsänen, P. The association of preceding traumatic brain injury with mental disorders, alcoholism and criminality: The Northern Finland 1966 Birth Cohort Study. Psychiatry Res. 2002, 113, 217–226. [Google Scholar] [CrossRef]
- Slaughter, B.; Fann, J.R.; Ehde, D. Traumatic brain injury in a county jail population: Prevalence, neuropsychological functioning and psychiatric disorders. Brain Inj. 2003, 17, 731–741. [Google Scholar] [CrossRef] [PubMed]
- Deb, S.; Aimola, L.; Leeson, V.; Bodani, M.; Li, L.; Weaver, T.; Sharp, D.; Bassett, P.; Crawford, M. Risperidone versus placebo for aggression following traumatic brain injury: A feasibility randomised controlled trial. BMJ Open 2020, 10, e036300. [Google Scholar] [CrossRef]
- Epstein, D.J.; Legarreta, M.; Bueler, E.; King, J.; McGlade, E.; Yurgelun-Todd, D. Orbitofrontal cortical thinning and aggression in mild traumatic brain injury patients. Brain Behav. 2016, 6, e00581. [Google Scholar] [CrossRef]
- Vaughn, M.G.; Salas-Wright, C.P.; DeLisi, M.; Perron, B. Correlates of traumatic brain injury among juvenile offenders: A multi-site study. Crim. Behav. Ment. Health CBMH 2014, 24, 188–203. [Google Scholar] [CrossRef]
- Dailey, N.S.; Smith, R.; Bajaj, S.; Alkozei, A.; Gottschlich, M.K.; Raikes, A.C.; Satterfield, B.C.; Killgore, W.D.S. Elevated Aggression and Reduced White Matter Integrity in Mild Traumatic Brain Injury: A DTI Study. Front. Behav. Neurosci. 2018, 12, 118. [Google Scholar] [CrossRef]
- Elbogen, E.B.; Wolfe, J.R.; Cueva, M.; Sullivan, C.; Johnson, J. Longitudinal Predictors of Criminal Arrest after Traumatic Brain Injury: Results From the Traumatic Brain Injury Model System National Database. J. Head Trauma Rehabil. 2015, 30, E3–E13. [Google Scholar] [CrossRef] [PubMed]
- Gordon, W.A.; Spielman, L.A.; Hahn-Ketter, A.E.; Sy, K.T.L. The Relationship Between Traumatic Brain Injury and Criminality in Juvenile Offenders. J. Head Trauma Rehabil. 2017, 32, 393–403. [Google Scholar] [CrossRef]
- Robert, S. Traumatic brain injury and mood disorders. Ment. Health Clin. 2020, 10, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.L.; Braun, J.M.; Mello, M.; Triche, E.W.; Buka, S.L. The relationship between early childhood head injury and later life criminal behaviour: A longitudinal cohort study. J. Epidemiol. Community Health 2017, 71, 800–805. [Google Scholar] [CrossRef]
- Tateno, A.; Jorge, R.E.; Robinson, R.G. Clinical correlates of aggressive behavior after traumatic brain injury. J. Neuropsychiatry Clin. Neurosci. 2003, 15, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Miles, S.R.; Hammond, F.M.; Neumann, D.; Silva, M.A.; Tang, X.; Kajankova, M.; Dillahunt-Aspillaga, C.; Nakase-Richardson, R. Evolution of Irritability, Anger, and Aggression after Traumatic Brain Injury: Identifying and Predicting Subgroups. J. Neurotrauma 2021, 38, 1827–1833. [Google Scholar] [CrossRef]
- Hammond, F.M.; Zafonte, R.D.; Tang, Q.; Jang, J.H. Carbamazepine for Irritability and Aggression after Traumatic Brain Injury: A Randomized, Placebo-Controlled Study. J. Neurotrauma 2021, 38, 2238–2246. [Google Scholar] [CrossRef] [PubMed]
- Darby, R.R.; Horn, A.; Cushman, F.; Fox, M.D. Lesion network localization of criminal behavior. Proc. Natl. Acad. Sci. USA 2018, 115, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Roy, D.; Vaishnavi, S.; Han, D.; Rao, V. Correlates and Prevalence of Aggression at Six Months and One Year After First-Time Traumatic Brain Injury. J. Neuropsychiatry Clin. Neurosci. 2017, 29, 334–342. [Google Scholar] [CrossRef] [PubMed]
- McCormick, B.F.; Connolly, E.J.; Nelson, D.V. Mild Traumatic Brain Injury as a Predictor of Classes of Youth Internalizing and Externalizing Psychopathology. Child Psychiatry Hum. Dev. 2021, 52, 166–178. [Google Scholar] [CrossRef] [PubMed]
- Ganesalingam, K.; Sanson, A.; Anderson, V.; Yeates, K.O. Self-regulation as a mediator of the effects of childhood traumatic brain injury on social and behavioral functioning. J. Int. Neuropsychol. Soc. JINS 2007, 13, 298–311. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.; Indig, D.; Haysom, L. Traumatic brain injury, mental health, substance use, and offending among incarcerated young people. J. Head Trauma Rehabil. 2014, 29, 239–247. [Google Scholar] [CrossRef]
- Wortzel, H.S.; Arciniegas, D.B. A forensic neuropsychiatric approach to traumatic brain injury, aggression, and suicide. J. Am. Acad. Psychiatry Law 2013, 41, 274–286. [Google Scholar]
- Brower, M.C.; Price, B.H. Neuropsychiatry of frontal lobe dysfunction in violent and criminal behaviour: A critical review. J. Neurol. Neurosurg. Psychiatry 2001, 71, 720–726. [Google Scholar] [CrossRef]
- Palijan, T.Z.; Radeljak, S.; Kovac, M.; Kovacević, D. Relationship between comorbidity and violence risk assessment in forensic psychiatry—the implication of neuroimaging studies. Psychiatr. Danub. 2010, 22, 253–256. [Google Scholar] [PubMed]
- Bufkin, J.L.; Luttrell, V.R. Neuroimaging studies of aggressive and violent behavior: Current findings and implications for criminology and criminal justice. Trauma Violence Abus. 2005, 6, 176–191. [Google Scholar] [CrossRef] [PubMed]
- Williams, W.H.; Chitsabesan, P.; Fazel, S.; McMillan, T.; Hughes, N.; Parsonage, M.; Tonks, J. Traumatic brain injury: A potential cause of violent crime? Lancet Psychiatry 2018, 5, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Tonks, J.; Slater, A.; Frampton, I.; Wall, S.E.; Yates, P.; Williams, W.H. The development of emotion and empathy skills after childhood brain injury. Dev. Med. Child Neurol. 2009, 51, 8–16. [Google Scholar] [CrossRef] [PubMed]
| Study | Aim | Method | Outcome |
|---|---|---|---|
| Baguley et al. (2006) [15] | Evaluate the occurrence and factors influencing aggressive conduct in individuals who have experienced traumatic brain injury (TBI) during three different time points: 6 months, 24 months and 60 months after their discharge from medical care. | Data were collected within a specialized brain injury rehabilitation hospital Service | During each of the follow-up periods, approximately 25% of the participants were identified as displaying aggressive behavior. This group showed connections with depression, concurrent traumatic complaints, being of a younger age at the time of injury and experiencing low life satisfaction. These associations were found to be more relevant than injury-related factors or demographic information. Notably, depression emerged as the most significant factor linked to aggressive behavior. |
| Veeh et al. (2018) [16] | Investigate whether temperament mediates the relationship between TBI and violent behavior within incarcerated youth. | An evaluation was conducted encompassing traumatic brain injury (TBI), temperament, childhood trauma, substance use, mental health conditions and various demographic factors. | The interaction between effortful control and negative emotionality seems to play a crucial role as a mechanism that influences the connection between traumatic brain injury (TBI) and violent behavior. |
| Williams et al. (2010) [17] | Investigate whether self-reported traumatic brain injury (TBI) in male young offenders is a risk factor for reoffending, poor mental health, and violence. | Data were collected through self-reports and interviews with male young offenders who reported a history of traumatic brain injury. | Male young offenders with a history of TBI exhibited an increased risk of reoffending, poor mental health, and violent behavior. |
| Colantonio et al. (2007) [14] | Examine brain injury prevalence in a forensic psychiatry population. | Medical records of forensic psychiatry patients were examined to identify the prevalence of brain injuries. | A significant proportion of the forensic psychiatry patients had evidence of brain injuries. |
| Darby, R.R. (2018) [18] | Investigate neuroimaging abnormalities in neurological patients with criminal behavior. | Neuroimaging data from neurological patients displaying criminal behavior were analyzed to identify any abnormalities. | Neuroimaging analysis revealed abnormalities in neurological patients exhibiting criminal behavior. |
| Glenn & Raine (2014) [19] | Examine the implications of neurocriminology for the punishment, prediction and prevention of criminal behavior. | The implications of neurocriminology for criminal behavior were analyzed, focusing on punishment, prediction and prevention. | The study discussed the potential applications of neurocriminology in dealing with criminal behavior, including its use in punishment, prediction and prevention. |
| Cristofori et al. (2016) [20] | Investigate brain regions influencing implicit violent attitudes using a lesion-mapping study. | A lesion-mapping study was conducted to identify brain regions influencing implicit violent attitudes. | The study identified specific brain regions that played a role in influencing implicit violent attitudes. |
| Timonen et al. (2002) [21] | Assess the association between preceding traumatic brain injury and mental disorders, alcoholism, and criminality using the Northern Finland 1966 Birth Cohort Study. | The Northern Finland 1966 Birth Cohort Study data were analyzed to assess the association between preceding traumatic brain injury and mental disorders, alcoholism and criminality. | Preceding traumatic brain injury was associated with an increased risk of mental disorders, alcoholism and criminal behavior. |
| Slaughter et al. (2003) [22] | Examine the prevalence of traumatic brain injury (TBI) and its association with neuropsychological functioning and psychiatric disorders in a county jail population. | TBI prevalence, neuropsychological functioning and psychiatric disorders were assessed in a county jail population. | TBI was prevalent in the county jail population and associated with neuropsychological impairments and psychiatric disorders. |
| Deb et al. (2020) [23] | Investigate the feasibility of using risperidone as a treatment for aggression following traumatic brain injury. | A randomized controlled trial was conducted to compare risperidone with a placebo for aggression in traumatic brain injury patients. | The feasibility trial suggested that risperidone may be a potential treatment for aggression after traumatic brain injury. |
| Epstein et al. (2016) [24] | Examine orbitofrontal cortical thinning and its relationship with aggression in patients with mild traumatic brain injury. | The study utilized neuroimaging techniques to investigate orbitofrontal cortical thinning in mild traumatic brain injury patients exhibiting aggression. | Patients with mild traumatic brain injury and aggression showed orbitofrontal cortical thinning in neuroimaging scans. |
| Vaughn et al. (2014) [25] | Identify correlates of traumatic brain injury (TBI) in a multi-site study of juvenile offenders. | A multi-site study was conducted to identify the correlates of TBI among juvenile offenders. | The study identified various correlates of traumatic brain injury in juvenile offenders. |
| Dailey et al. (2018) [26] | Investigate elevated aggression and reduced white matter integrity in mild traumatic brain injury patients. | A diffusion tensor imaging (DTI) study was conducted to assess white matter integrity in mild traumatic brain injury patients with elevated aggression. | Mild traumatic brain injury patients with elevated aggression showed reduced white matter integrity in DTI scans. |
| Elbogen et al. (2015) [27] | Examine longitudinal predictors of criminal arrest after traumatic brain injury using the Traumatic Brain Injury Model System National Database. | The study utilized data from the Traumatic Brain Injury Model System National Database to explore longitudinal predictors of criminal arrest after traumatic brain injury. | The study identified longitudinal predictors associated with criminal arrest after traumatic brain injury. |
| Gordon et al. (2017) [28] | Investigate the relationship between traumatic brain injury (TBI) and criminality in juvenile offenders. | The study examined the relationship between TBI and criminal behavior in juvenile offenders. | A relationship between traumatic brain injury (TBI) and criminal behavior was found in juvenile offenders. |
| Robert, S. (2020) [29] | Explore the association between traumatic brain injury (TBI) and mood disorders. | The study investigated the association between TBI and mood disorders. | The study found an association between traumatic brain injury (TBI) and mood disorders. |
| Jackson et al. (2017) [30] | Examine the relationship between early childhood head injury and later life criminal behavior using a longitudinal cohort study. | A longitudinal cohort study was conducted to investigate the relationship between early childhood head injury and later life criminal behavior. | The study revealed a relationship between early childhood head injury and later life criminal behavior. |
| Tateno et al. (2003) [31] | Identify clinical correlates of aggressive behavior after traumatic brain injury. | The study examined clinical correlates of aggressive behavior in patients with traumatic brain injury. | The study identified clinical correlates associated with aggressive behavior after traumatic brain injury. |
| Miles et al. (2021) [32] | Investigate the evolution of irritability, anger and aggression after traumatic brain injury and identify subgroups with predictive factors. | The study analyzed the evolution of irritability, anger and aggression after traumatic brain injury, identifying subgroups with predictive factors. | The study identified subgroups with specific predictive factors for the evolution of irritability, anger and aggression after traumatic brain injury. |
| Hammond et al. (2021) [33] | Assess the efficacy of carbamazepine for treating irritability and aggression after traumatic brain injury in a randomized, placebo-controlled study. | A randomized, placebo-controlled study was conducted to assess the efficacy of carbamazepine for treating irritability and aggression in traumatic brain injury patients. | Carbamazepine showed promise for treating irritability and aggression after traumatic brain injury in the study. |
| Darby et al. (2018) [34] | Investigate lesion network localization of criminal behavior. | The study used lesion network localization techniques to investigate criminal behavior localization in patients with brain lesions. | Lesion network localization revealed specific brain lesion locations associated with criminal behavior. |
| Roy et al. (2017) [35] | Examine the prevalence and correlates of aggression at six months and one year after first-time traumatic brain injury. | The study investigated the prevalence and correlates of aggression at six months and one year after first-time traumatic brain injury. | The study found prevalence rates and correlates of aggression at six months and one year post-traumatic brain injury. |
| McCormick et al. (2021) [36] | Investigate mild traumatic brain injury as a predictor of youth internalizing and externalizing psychopathology using a longitudinal study. | A longitudinal study was conducted to investigate mild traumatic brain injury as a predictor of youth internalizing and externalizing psychopathology. | Mild traumatic brain injury was found to be a predictor of youth internalizing and externalizing psychopathology. |
| Ganesalingam et al. (2007) [37] | Examine self-regulation as a mediator of the effects of childhood traumatic brain injury on social and behavioral functioning. | The study investigated self-regulation as a mediator of the effects of childhood traumatic brain injury on social and behavioral functioning. | Self-regulation mediated the effects of childhood traumatic brain injury on social and behavioral functioning. |
| Moore et al. (2014) [38] | Examine the relationship between traumatic brain injury (TBI), mental health, substance use and criminal offense among incarcerated young people. | The study investigated the relationship between TBI, mental health, substance use and criminal offense in incarcerated young people. Data were collected and analyzed to assess the association between these factors. | Incarcerated young people with TBI were found to have higher rates of mental health issues, substance use, and offending behaviors. |
| Van Reekum et al. (1996) [8] | Explore psychiatric disorders after traumatic brain injury. | The study examined psychiatric disorders following traumatic brain injury. | Psychiatric disorders were found to be prevalent after traumatic brain injury. |
| Vaughn et al. (2019) [5] | Investigate the relationship between traumatic brain injury (TBI) and psychiatric comorbidity in the United States. | Data from the United States were analyzed to study the relationship between TBI and psychiatric comorbidity. | A relationship was observed between traumatic brain injury (TBI) and psychiatric comorbidity in the United States. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maresca, G.; Lo Buono, V.; Anselmo, A.; Cardile, D.; Formica, C.; Latella, D.; Quartarone, A.; Corallo, F. Traumatic Brain Injury and Related Antisocial Behavioral Outcomes: A Systematic Review. Medicina 2023, 59, 1377. https://doi.org/10.3390/medicina59081377
Maresca G, Lo Buono V, Anselmo A, Cardile D, Formica C, Latella D, Quartarone A, Corallo F. Traumatic Brain Injury and Related Antisocial Behavioral Outcomes: A Systematic Review. Medicina. 2023; 59(8):1377. https://doi.org/10.3390/medicina59081377
Chicago/Turabian StyleMaresca, Giuseppa, Viviana Lo Buono, Anna Anselmo, Davide Cardile, Caterina Formica, Desiree Latella, Angelo Quartarone, and Francesco Corallo. 2023. "Traumatic Brain Injury and Related Antisocial Behavioral Outcomes: A Systematic Review" Medicina 59, no. 8: 1377. https://doi.org/10.3390/medicina59081377
APA StyleMaresca, G., Lo Buono, V., Anselmo, A., Cardile, D., Formica, C., Latella, D., Quartarone, A., & Corallo, F. (2023). Traumatic Brain Injury and Related Antisocial Behavioral Outcomes: A Systematic Review. Medicina, 59(8), 1377. https://doi.org/10.3390/medicina59081377







