Clostridioides difficile Infections among Pediatric Patients Hospitalized at an Oncology Department of a Tertiary Hospital in Poland
Abstract
1. Introduction
- Grade 1—2.0 × 109/L to 1.5 × 109/L
- Grade 2—1.5 × 109/L to 1.0 × 109/L
- Grade 3—1.0 × 109/L to 0.5 × 109/L
- Grade 4—<0.5 × 109/L
2. Materials and Methods
2.1. General Data
2.2. Laboratory Diagnostics
2.3. Definition of CDI
2.4. Statistical Methods
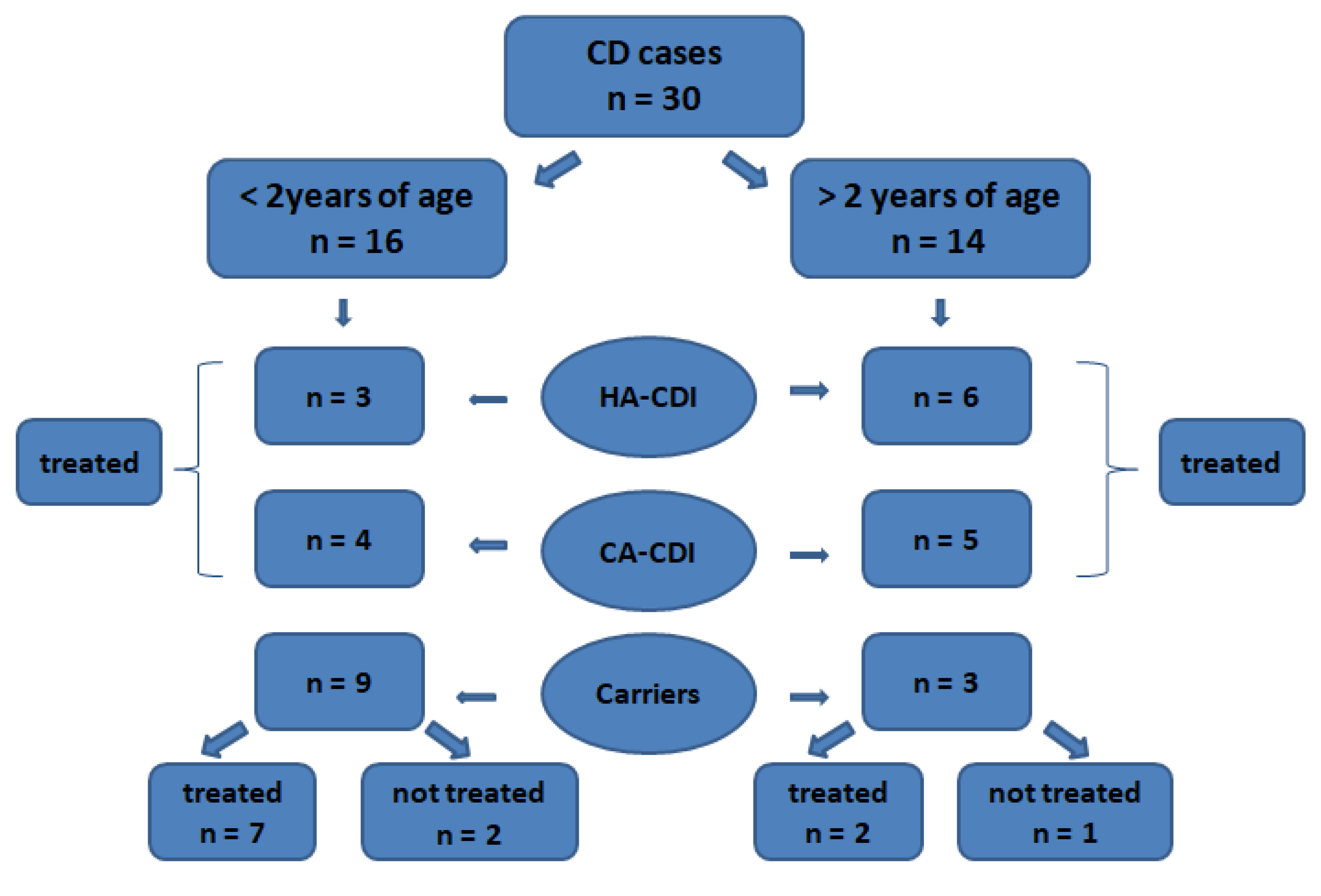
2.5. Study Populations
3. Results
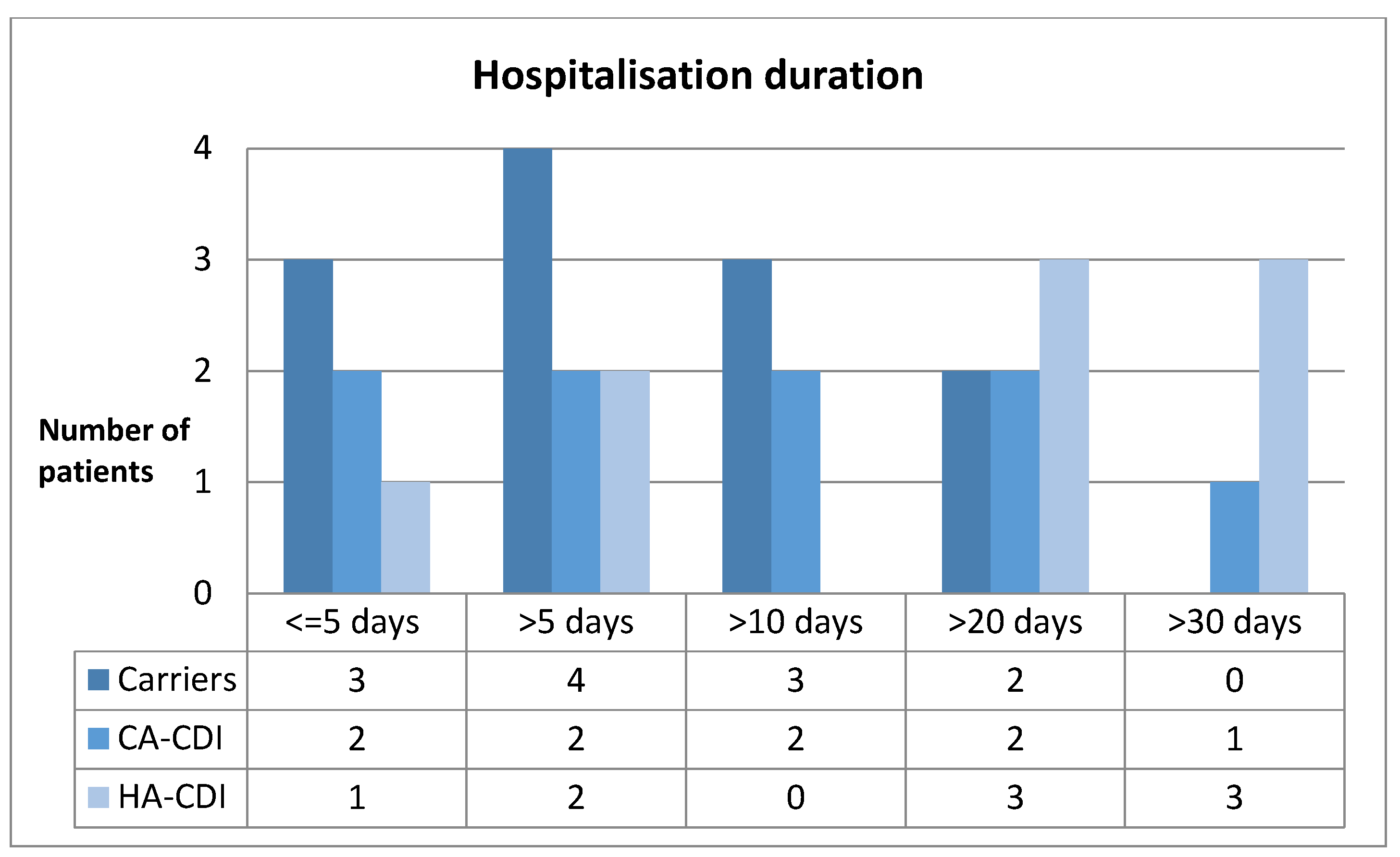
3.1. Hospitalizations
3.2. Antibiotic Therapy
3.3. Treatment of CDI
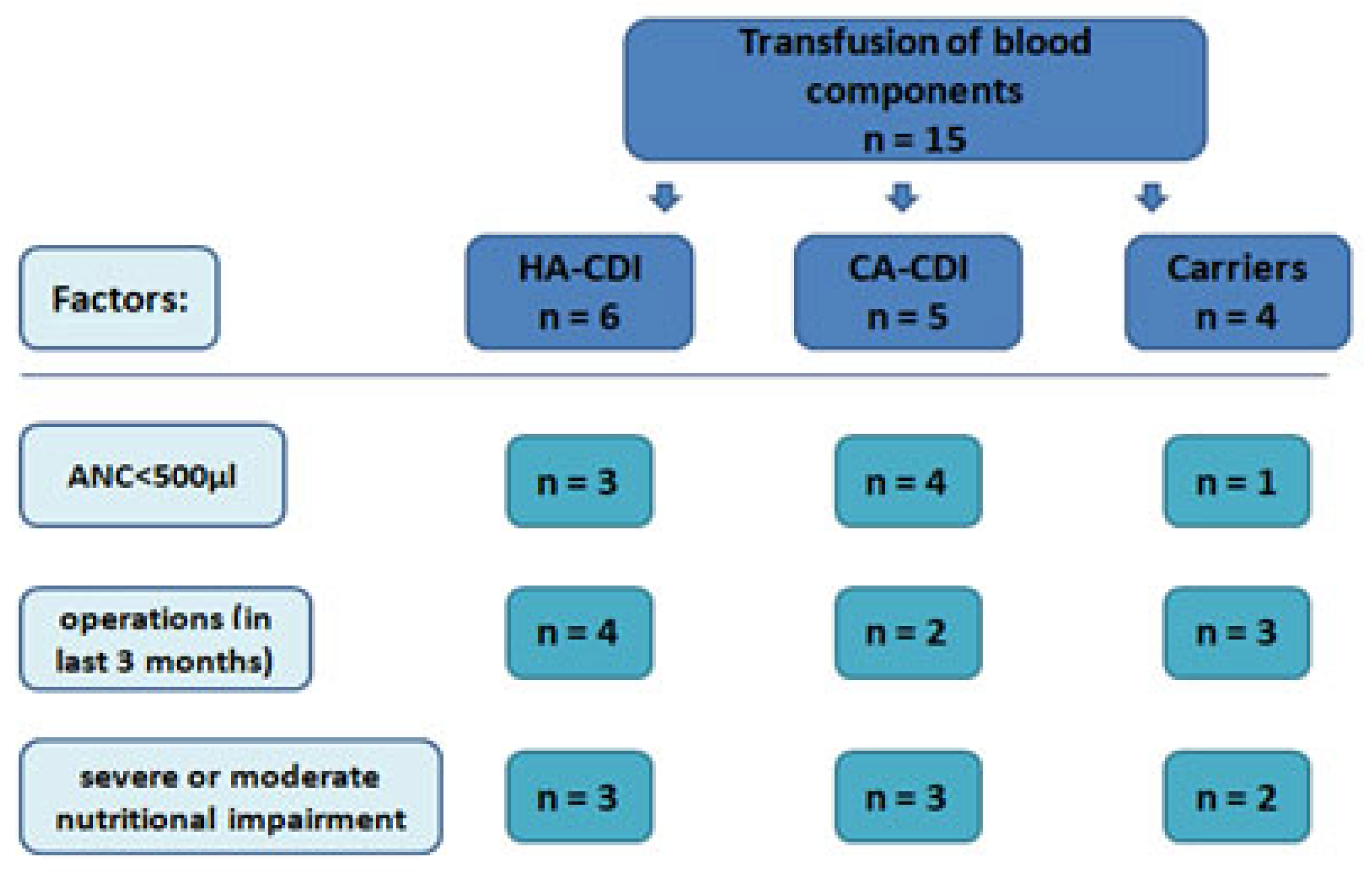
3.4. Hematological and Biochemical Parameters
3.5. Nutrition Indicators
3.6. Invasive Procedures
3.7. Hospital-Acquired Infection Charts
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sierocka, A.; Kiersnowska, Z.; Lemiech-Mirowska, E.; Marczak, M. Costs Associated with the Treatment of Clostridioides difficile Infections. Int. J. Environ. Res. Public Health 2021, 18, 7647. [Google Scholar] [CrossRef]
- Cózar-Llistó, A.; Ramos-Martinez, A.; Cobo, J. Clostridium difficile Infection in Special High-Risk Populations. Infect. Dis. Ther. 2016, 5, 253–269. [Google Scholar] [CrossRef]
- Schwenk, H.T.; Pollock, N.R.; Vaughan-Malloy, A.M. Pediatric Clostridioides difficile Infection: Diagnosis and Diagnostic Stewardship. J. Pediatr. Infect. Dis. Soc. 2021, 10 (Suppl. S3), S16–S21. [Google Scholar] [CrossRef]
- Elgarten, C.W.; Aplenc, R. Pediatric acute myeloid leukemia: Updates on biology, risk stratification, and therapy. Curr. Opin. Pediatr. 2020, 32, 57–66. [Google Scholar] [CrossRef]
- Steliarova-Foucher, E.; Colombet, M.; Ries, L.A.G.; Moreno, F.; Dolya, A.; Bray, F.; Hesseling, P.; Shin, H.Y.; Stiller, C.A.; Bouzbid, S.; et al. International incidence of childhood cancer, 2001–2010: A population-based registry study. Lancet Oncol. 2017, 18, 719–731. [Google Scholar] [CrossRef] [PubMed]
- Steinmeier, T.; Schulze Schleithoff, S.; Timmermann, B. Evolving Radiotherapy Techniques in Paediatric Oncology. Clin. Oncol. 2019, 31, 142–150. [Google Scholar] [CrossRef]
- Sohail, H.; Ahmed, S.A.; Usman, P.; Khalid, F.; Haque, A.U.; Abbas, Q. Red blood cell transfusion in critically-ill children and its association with outcome. J. Pak. Med. Assoc. 2021, 71, 1967–1971. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Song, K.-H.; Bae, J.Y.; Yoon, D.; Hwang, J.-H.; Choe, P.G.; Park, W.B.; Bang, J.H.; Kim, E.S.; Park, S.W.; et al. Risk factors for poor outcome in community-onset Clostridium difficile infection. Antimicrob. Resist. Infect. Control. 2018, 7, 75. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, K.A.; Le, D.Q.; Bui, Y.T.; Advani, S.D.; Renzulli, J., 2nd; Kenney, P.A.; Leapman, M.S. Incidence, risk factors, and outcome of Clostridioides difficile infection following urological surgeries. World J. Urol. 2021, 39, 2995–3003. [Google Scholar] [CrossRef]
- Baluch, A.; Shewayish, S. Neutropenic Fever. In Infections in Neutropenic Cancer Patients; Velez, A.P., Lamarche, J., Greene, J.N., Eds.; Springer: Berlin/Heidelberg, Germany, 2019; pp. 105–117. [Google Scholar] [CrossRef]
- Anderson, K.; Bradford, N.; Edwards, R.; Nicholson, J.; Lockwood, L.; Clark, J.E. Improving management of fever in neutropenic children with cancer across multiple sites. Eur. J. Cancer Care 2021, 30, e13413. [Google Scholar] [CrossRef]
- Lehrnbecher, T.; Robinson, P.; Fisher, B.; Alexander, S.; Ammann, R.A.; Beauchemin, M.; Carlesse, F.; Groll, A.H.; Haeusler, G.; Santolaya, M.; et al. Guideline for the Management of Fever and Neutropenia in Children with Cancer and Hematopoietic Stem-Cell Transplantation Recipients: 2017 Update. J. Clin. Oncol. 2017, 35, 2082–2094. [Google Scholar] [CrossRef] [PubMed]
- Storz, E.; Gschwend, J.E.; Retz, M. Chemotherapie-induzierte Nausea und Emesis: Aktuelle Empfehlungen zur Prophylaxe [Chemotherapy-induced nausea and vomiting: Current recommendations for prophylaxis]. Urol. A 2018, 57, 532–542. [Google Scholar] [CrossRef] [PubMed]
- Trimpe, K.; Shaw, M.R.; Wilson, M.; Haberman, M.R. Review of the Effectiveness of Enteral Feeding in Pediatric Oncology Patients. J. Pediatr. Oncol. Nurs. 2017, 34, 439–445. [Google Scholar] [CrossRef]
- McGrath, K.H.; Evans, V.; Yap, J. Indications and Patterns of Use for Parenteral Nutrition in Pediatric Oncology. J. Parenter. Enter. Nutr. 2020, 44, 632–638. [Google Scholar] [CrossRef]
- Kiersnowska, Z.; Lemiech-Mirowska, E.; Michałkiewicz, M.; Marczak, M. Hand hygiene as the basic method of reducing Clostridium difficile infections (CDI) in a hospital environment. Ann. Agric. Environ. Med. 2021, 28, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Song, J.H.; Kim, Y.S. Recurrent Clostridium difficile Infection: Risk Factors, Treatment, and Prevention. Gut Liver 2019, 13, 16–24. [Google Scholar] [CrossRef]
- Kiersnowska, Z.; Lemiech-Mirowska, E.; Ginter-Kramarczyk, D.; Kruszelnicka, I.; Michałkiewicz, M.; Marczak, M. Problems of Clostridium difficile infection (CDI) in Polish healthcare units. Ann. Agric. Environ. Med. 2021, 28, 224–230. [Google Scholar] [CrossRef]
- O’Keefe, S.J. Tube feeding, the microbiota, and Clostridium difficile infection. World J. Gastroenterol. 2010, 16, 139–142. [Google Scholar] [CrossRef]
- Kiersnowska, Z.M.; Lemiech-Mirowska, E.; Semczuk, K.; Michałkiewicz, M.; Sierocka, A.; Marczak, M. Level of Knowledge of Medical Staff on the Basis of the Survey in Terms of Risk Management, Associated with Clostridioides difficile Infections. Int. J. Environ. Res. Public Health 2021, 18, 7060. [Google Scholar] [CrossRef]
- McDonald, L.C.; Gerding, D.N.; Johnson, S.; Bakken, J.S.; Carroll, K.C.; Coffin, S.E.; Dubberke, E.R.; Garey, K.W.; Gould, C.V.; Kelly, C.; et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin. Infect. Dis. 2018, 66, e1–e48. [Google Scholar] [CrossRef]
- Nicholson, M.R.; Thomsen, I.P.; Slaughter, J.C.; Creech, C.B.; Edwards, K.M. Novel Risk Factors for Recurrent Clostridium difficile Infection in Children. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 18–22. [Google Scholar] [CrossRef]
- Krutova, M.; Kinross, P.; Barbut, F.; Hajdu, A.; Wilcox, M.H.; Kuijper, E.J.; Survey Contributors. How to: Surveillance of Clostridium difficile infections. Clin. Microbiol. Infect. 2018, 24, 469–475. [Google Scholar] [CrossRef]
- Balsells, E.; Filipescu, T.; Kyaw, M.H.; Wiuff, C.; Campbell, H.; Nair, H. Infection prevention and control of Clostridium difficile: A global review of guidelines, strategies, and recommendations. J. Glob. Health 2016, 6, 020410. [Google Scholar] [CrossRef] [PubMed]
- Duleba, K.; Pawlowska, M.; Wietlicka-Piszcz, M. Clostridium difficile infection in children hospitalized due to diarrhea. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 201–209. [Google Scholar] [CrossRef]
- Gnocchi, M.; Gagliardi, M.; Gismondi, P.; Gaiani, F.; D’Angelis, G.L.; Esposito, S. Updated Management Guidelines for Clostridioides difficile in Paediatrics. Pathogens 2020, 9, 291. [Google Scholar] [CrossRef] [PubMed]
- Cowan, A.N.; Kutty, G. Clostridium difficile Colitis in a Patient with Abdominal Distention, Pain, and Severe Constipation. Fed. Pract. 2018, 35, 44–46. [Google Scholar]
- Crews, J.D.; Koo, H.L.; Jiang, Z.D.; Starke, J.R.; DuPont, H.L. A hospital-based study of the clinical characteristics of Clostridium difficile infection in children. Pediatr. Infect. Dis. J. 2014, 33, 924–928. [Google Scholar] [CrossRef]
- Tai, E.; Richardson, L.C.; Townsend, J.; Howard, E.; Mcdonald, L.C. Clostridium difficile infection among children with cancer. Pediatr. Infect. Dis. J. 2011, 30, 610–612. [Google Scholar] [CrossRef]
- Boyle, N.M.; Magaret, A.; Stednick, Z.; Morrison, A.; Butler-Wu, S.; Zerr, D.; Rogers, K.; Podczervinski, S.; Cheng, A.; Wald, A.; et al. Evaluating risk factors for Clostridium difficile infection in adult and pediatric hematopoietic cell transplant recipients. Antimicrob. Resist. Infect. Control. 2015, 4, 41. [Google Scholar] [CrossRef]
- Rzayev, T.; YükselMayda, P.; Erkan, T.; Kocazeybek, B.; Kutlu, T. Clostridium difficile Colonization before and after Hospitalization in Children. Turk. Arch. Pediatr. 2021, 56, 585–590. [Google Scholar] [CrossRef] [PubMed]
- Kiersnowska, Z.M.; Lemiech-Mirowska, E.; Michałkiewicz, M.; Sierocka, A.; Marczak, M. Detection and Analysis of Clostridioides difficile Spores in a Hospital Environment. Int. J. Environ. Res. Public Health 2022, 19, 15670. [Google Scholar] [CrossRef] [PubMed]
- Lemiech-Mirowska, E.; Michałkiewicz, M.; Sierocka, A.; Gaszyńska, E.; Marczak, M. The Hospital Environment as a Potential Source for Clostridioides difficile Transmission Based on Spore Detection Surveys Conducted at Paediatric Oncology and Gastroenterology Units. Int. J. Environ. Res. Public Health 2023, 20, 1590. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.A.; Khanafer, N.; Daneman, N.; Fisman, D.N. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob. Agents Chemother. 2013, 57, 2326–2332. [Google Scholar] [CrossRef]
- Bartlett, J.G. Clostridium difficile: Old and New observations. J. Clin. Gastroenterol. 2007, 41, S24–S29. [Google Scholar] [CrossRef]
- Abughanimeh, O.; Qasrawi, A.; Kaddourah, O.; Al Momani, L.; Abu Ghanimeh, M. Clostridium difficile infection in oncology patients: Epidemiology, pathophysiology, risk factors, diagnosis, and treatment. Hosp. Pract. 2018, 46, 266–277. [Google Scholar] [CrossRef]
- Babrowski, T.; Holbrook, C.; Moss, J.; Gottlieb, L.; Valuckaite, V.; Zaborin, A.; Poroyko, V.; Liu, D.C.; Zaborina, O.; Alverdy, J.C. Pseudomonas aeruginosa virulence expression is directly activated by morphine and is capable of causing lethal gut-derived sepsis in mice during chronic morphine administration. Ann. Surg. 2012, 255, 386–393. [Google Scholar] [CrossRef]
| Original Diagnosis | Number of Patients | Patients with CDI | Patients Colonized by CD |
|---|---|---|---|
| Neuroblastoma type 4 | 4 | 2 | 2 |
| Malignant neoplasms of the brain and CNS | 8 | 3 | 5 |
| Malignant neoplasms of the eye | 3 | 1 | 2 |
| Malignant neoplasms of the liver | 4 | 3 | 1 |
| Lymphoma | 2 | 2 | - |
| Malignant neoplasm of the kidney | 2 | 1 | 1 |
| Non-malignant neoplasm of brain and other parts of CNS | 1 | 1 | - |
| Neurofibromatosis type 1 | 1 | 1 | - |
| Malignant neoplasm of connective tissue | 1 | 1 | - |
| Malignant neoplasm of the ovary | 1 | 1 | - |
| Rhabdomyosarcoma, RMS | 2 | 1 | 1 |
| Malignant neoplasm of soft tissue | 1 | 1 | - |
| Antibiotic Group | Administered Antibiotic | Number of Patients Subjected to Treatment | Classification of CDI Risk |
|---|---|---|---|
| 3rd generation cephalosporins | Ceftriaxone | 8 | High risk |
| Cefotaxime | 5 | ||
| Ceftazidime | 2 | ||
| Beta-lactam antibiotics with an inhibitor | Amoxicillin with clavulanic acid | 12 | High risk |
| Aminoglycosides | Amikacin | 5 | Low risk |
| Lincosamides | Clindamycin | 3 | High risk |
| Fluoroquinolones | Ciprofloxacin | 3 | High risk |
| Sulfonamides | Trimethoprim/Sulfamethoxazole | 3 | Low risk |
| Macrolides | Clarithromycin | 2 | Medium risk |
| Carbapenems | Imipenem | 1 | Medium risk |
| Meropenem | 1 | ||
| Glycopeptides | Teicoplanin | 1 | Low risk |
| Factor | Total | Patients with Confirmed CDI | Patients Colonised with CD | p | ||||
|---|---|---|---|---|---|---|---|---|
| n | [%] | n | [%] | n | [%] | |||
| Gastrointestinal tract symptoms up to 48 h since admission | No | 13 | 43.33 | 9 | 50.00 | 4 | 33.32 | 0.3669 (1) |
| Yes | 17 | 56.67 | 9 | 50.00 | 8 | 66.68 | ||
| Feeding | Normal | 5 | 16.7 | 1 | 5.56 | 4 | 33.32 | - |
| Broviac catheter | 7 | 23.3 | 5 | 27.8 | 2 | 16.66 | ||
| Intestinal probe | 17 | 56.7 | 11 | 61.10 | 6 | 50.00 | ||
| Gastrostomy | 1 | 3.3 | 1 | 5.56 | 0 | 0.00 | ||
| Cole index% | M ± SD Me (min.–max.) | 92.9 ± 13.3 94.6 (62.4–123.7) | 92.4 ± 14.3 90.9 (73.2–123.7) | 93.4 ± 12.2 95.5 (62.4–105.7) | 0.6114 (2) | |||
| Assessment of nutritional state | Overweight | 2 | 6.7 | 2 | 11.11 | 0 | 0 | - |
| Correct nutrition state | 16 | 53.3 | 7 | 38.89 | 9 | 75.00 | ||
| Mild impairment of nutrition state | 4 | 13.3 | 3 | 16.67 | 1 | 8.33 | ||
| Moderate impairment of nutrition state | 5 | 16.7 | 4 | 22.22 | 1 | 8.33 | ||
| Severe malnutrition | 3 | 10.0 | 2 | 11.11 | 1 | 8.33 | ||
| Hospital-Acquired Infections Charts | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Patients | |||||||||
| Age | 2 | 7 | 3 | 9 | 1 | 12 | 2 | 5 | 3 |
| Sex: male (M), female (F) | M | F | M | M | F | M | M | M | F |
| Antibiotic therapy | + | + | + | + | + | + | + | + | + |
| Chemotherapy | + | + | + | + | + | + | + | − | + |
| Immunosuppression | + | − | − | + | − | + | − | + | − |
| Advanced stage of disease | + | + | + | + | + | + | + | + | + |
| Organ transplant | − | − | − | − | − | + | − | − | − |
| Central venous access device | − | + | + | + | − | − | + | − | + |
| Extended hospitalisation | + | + | + | + | + | + | + | + | + |
| Another stay | + | + | + | + | + | + | + | + | + |
| Admitted from home | + | − | + | + | + | + | + | − | + |
| Admitted from another unit | − | + | − | − | − | − | − | + | − |
| Clinical course of infection: mild (Mi), moderate (Mo) | Mi | Mi | Mi | Mi | Mi | Mo | Mo | Mi | Mi |
| Treatment: metronidazole (MTZ), vancomycin (VA), rifaximin (R) | MTZ | MTZ | MTZ | MTZ | R | VA | MTZ/ VA | MTZ | MTZ |
| Diarrhoea | + | + | + | + | + | + | −/+ | + | + |
| Vomiting | − | − | + | − | + | + | + | + | − |
| Fever | − | − | − | + | − | + | + | + | − |
| Implemented procedures: isolation (I), cohortation (CO) | I | I | I | CO | I | I | I | I | I |
| Disinfecting the unit | |||||||||
| Type of infection: endogenous (EN)/exogenous(EX) | EN | EN | EX | EN | EN | EN | EN | EN | EN |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lemiech-Mirowska, E.; Gaszyńska, E.; Sierocka, A.; Kiersnowska, Z.; Marczak, M. Clostridioides difficile Infections among Pediatric Patients Hospitalized at an Oncology Department of a Tertiary Hospital in Poland. Medicina 2023, 59, 1363. https://doi.org/10.3390/medicina59081363
Lemiech-Mirowska E, Gaszyńska E, Sierocka A, Kiersnowska Z, Marczak M. Clostridioides difficile Infections among Pediatric Patients Hospitalized at an Oncology Department of a Tertiary Hospital in Poland. Medicina. 2023; 59(8):1363. https://doi.org/10.3390/medicina59081363
Chicago/Turabian StyleLemiech-Mirowska, Ewelina, Ewelina Gaszyńska, Aleksandra Sierocka, Zofia Kiersnowska, and Michał Marczak. 2023. "Clostridioides difficile Infections among Pediatric Patients Hospitalized at an Oncology Department of a Tertiary Hospital in Poland" Medicina 59, no. 8: 1363. https://doi.org/10.3390/medicina59081363
APA StyleLemiech-Mirowska, E., Gaszyńska, E., Sierocka, A., Kiersnowska, Z., & Marczak, M. (2023). Clostridioides difficile Infections among Pediatric Patients Hospitalized at an Oncology Department of a Tertiary Hospital in Poland. Medicina, 59(8), 1363. https://doi.org/10.3390/medicina59081363







