Additional Anterolateral Ligament Reconstruction Helps Patients Improve Dynamic Postural Stability in Revision Anterior Cruciate Ligament Reconstruction
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Surgical Technique
2.2.1. Revision ACLR
2.2.2. ALLR
2.3. Postoperative Rehabilitation
2.4. Outcome Assessment
2.4.1. Subjective Knee Scores
2.4.2. Isokinetic Muscle Strength Test
2.4.3. Single Leg Hop for Distance Test
2.4.4. Y-Balance Test
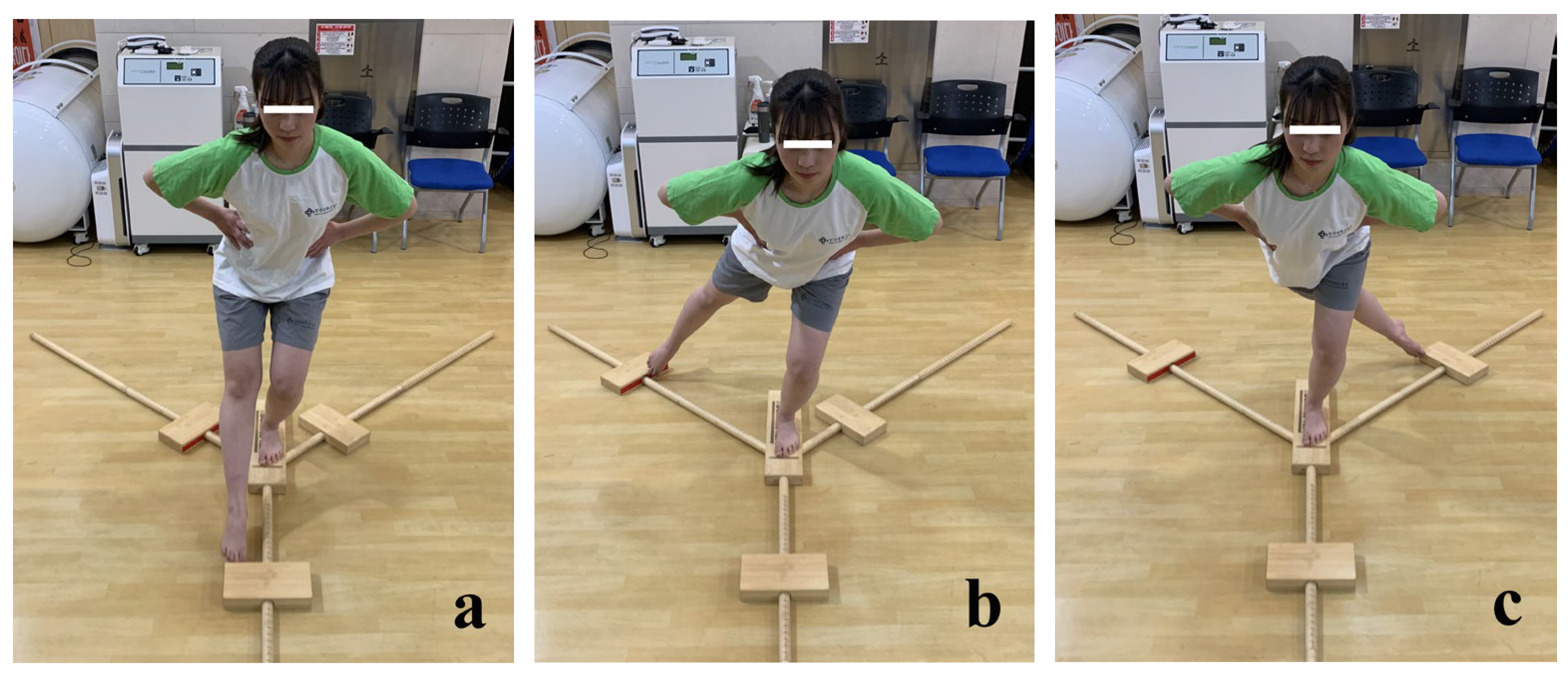
2.5. Statistical Analysis
3. Results
3.1. Subjective Knee Scores
3.2. Isokinetic Muscle Strength Test
3.3. Single Leg Hop for Distance Test
3.4. Y-Balance Test
3.5. Power of the Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Renstrom, P.A. Eight clinical conundrums relating to anterior cruciate ligament (ACL) injury in sport: Recent evidence and a personal reflection. Br. J. Sports Med. 2013, 47, 367–372. [Google Scholar] [CrossRef]
- Grassi, A.; Zicaro, J.P.; Costa-Paz, M.; Samuelsson, K.; Wilson, A.; Zaffagnini, S.; Condello, V.; Committee, E.A. Good mid-term outcomes and low rates of residual rotatory laxity, complications and failures after revision anterior cruciate ligament reconstruction (ACL) and lateral extra-articular tenodesis (LET). Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 418–431. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Saithna, A.; Cavalier, M.; Kajetanek, C.; Temponi, E.F.; Daggett, M.; Helito, C.P.; Thaunat, M. Anterolateral Ligament Reconstruction Is Associated with Significantly Reduced ACL Graft Rupture Rates at a Minimum Follow-up of 2 Years: A Prospective Comparative Study of 502 Patients from the SANTI Study Group. Am. J. Sports Med. 2017, 45, 1547–1557. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Daggett, M.; Fayard, J.M.; Ferretti, A.; Helito, C.P.; Lind, M.; Monaco, E.; de Padua, V.B.C.; Thaunat, M.; Wilson, A.; et al. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament—Deficient knee. J. Orthop. Traumatol. 2017, 18, 91–106. [Google Scholar] [CrossRef]
- Louis, M.L.; D’Ingrado, P.; Ehkirch, F.P.; Bertiaux, S.; Colombet, P.; Sonnery-Cottet, B.; Schlatterer, B.; Pailhe, R.; Panisset, J.C.; Steltzlen, C.; et al. Combined intra- and extra-articular grafting for revision ACL reconstruction: A multicentre study by the French Arthroscopy Society (SFA). Orthop. Traumatol. Surg. Res. 2017, 103, S223–S229. [Google Scholar] [CrossRef]
- Lee, D.W.; Kim, J.G.; Cho, S.I.; Kim, D.H. Clinical Outcomes of Isolated Revision Anterior Cruciate Ligament Reconstruction or in Combination with Anatomic Anterolateral Ligament Reconstruction. Am. J. Sports. Med. 2019, 47, 324–333. [Google Scholar] [CrossRef]
- Yoon, K.H.; Hwang, I.U.; Kim, E.J.; Kwon, Y.B.; Kim, S.G. Anterolateral Ligament Reconstruction Improves Anteroposterior Stability as Well as Rotational Stability in Revision Anterior Cruciate Ligament Reconstruction with High-Grade Pivot Shift. J. Knee. Surg. 2020, 34, 1310–1317. [Google Scholar] [CrossRef]
- Song, G.Y.; Hong, L.; Zhang, H.; Zhang, J.; Li, Y.; Feng, H. Clinical Outcomes of Combined Lateral Extra-articular Tenodesis and Intra-articular Anterior Cruciate Ligament Reconstruction in Addressing High-Grade Pivot-Shift Phenomenon. Arthroscopy 2016, 32, 898–905. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Vieira, T.D.; Ouanezar, H. Anterolateral Ligament of the Knee: Diagnosis, Indications, Technique, Outcomes. Arthroscopy 2019, 35, 302–303. [Google Scholar] [CrossRef] [PubMed]
- Claes, S.; Vereecke, E.; Maes, M.; Victor, J.; Verdonk, P.; Bellemans, J. Anatomy of the anterolateral ligament of the knee. J. Anat. 2013, 223, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.P.; Magnussen, R.A.; Gezmez, F.; Uguen, A.; Jacobi, M.; Weppe, F.; Al-Saati, M.F.; Lustig, S.; Demey, G.; Servien, E.; et al. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg. Sport. Traumatol. Arthrosc. 2012, 20, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, E.T.; Stentz-Olesen, K.; de Raedt, S.; Jorgensen, P.B.; Sorensen, O.G.; Kaptein, B.; Andersen, M.S.; Stilling, M. Influence of the Anterolateral Ligament on Knee Laxity: A Biomechanical Cadaveric Study Measuring Knee Kinematics in 6 Degrees of Freedom Using Dynamic Radiostereometric Analysis. Orthop. J. Sports. Med. 2018, 6, 2325967118789699. [Google Scholar] [CrossRef] [PubMed]
- Parsons, E.M.; Gee, A.O.; Spiekerman, C.; Cavanagh, P.R. The biomechanical function of the anterolateral ligament of the knee. Am. J. Sports. Med. 2015, 43, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, M.T.; Nitri, M.; Williams, B.T.; Moulton, S.G.; Cruz, R.S.; Dornan, G.J.; Goldsmith, M.T.; LaPrade, R.F. An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 1 Secondary Role of the Anterolateral Ligament in the Setting of an Anterior Cruciate Ligament Injury. Am. J. Sports Med. 2016, 44, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Getgood, A. Editorial Commentary: Return to Sport Following Extra-Articular Augmentation of Anterior Cruciate Ligament Reconstruction-Let the LET (Lateral Extra-Articular Tenodesis) Games Commence! Arthroscopy 2021, 37, 388–390. [Google Scholar] [CrossRef]
- Staples, J.R.; Schafer, K.A.; Smith, M.V.; Motley, J.; Halstead, M.; Blackman, A.; Haas, A.; Steger-May, K.; Matava, M.J.; Wright, R.W.; et al. Decreased Postural Control in Patients Undergoing Anterior Cruciate Ligament Reconstruction Compared to Healthy Controls. J. Sport Rehabil. 2019, 29, 1–6. [Google Scholar] [CrossRef]
- Heinert, B.; Willett, K.; Kernozek, T.W. Influence of Anterior Cruciate Ligament Reconstruction on Dynamic Postural Control. Int. J. Sports Phys. Ther. 2018, 13, 432–440. [Google Scholar] [CrossRef]
- Kinzey, S.J.; Armstrong, C.W. The reliability of the star-excursion test in assessing dynamic balance. J. Orthop. Sports Phys. Ther. 1998, 27, 356–360. [Google Scholar] [CrossRef]
- Plisky, P.J.; Gorman, P.P.; Butler, R.J.; Kiesel, K.B.; Underwood, F.B.; Elkins, B. The reliability of an instrumented device for measuring components of the star excursion balance test. N. Am. J. Sports Phys. Ther. 2009, 4, 92–99. [Google Scholar]
- Robinson, R.; Gribble, P. Kinematic predictors of performance on the Star Excursion Balance Test. J. Sport Rehabil. 2008, 17, 347–357. [Google Scholar] [CrossRef]
- Walaszek, R.; Chwala, W.; Walaszek, K.; Burdacki, M.; Blaszczuk, J. Evaluation of the accuracy of the postural stability measurement with the Y-Balance Test based on the levels of the biomechanical parameters. Acta Bioeng. Biomech. 2017, 19, 121–128. [Google Scholar]
- Coughlan, G.F.; Fullam, K.; Delahunt, E.; Gissane, C.; Caulfield, B.M. A comparison between performance on selected directions of the star excursion balance test and the Y balance test. J. Athl. Train. 2012, 47, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Sonnery-Cottet, B.; Lutz, C.; Daggett, M.; Dalmay, F.; Freychet, B.; Niglis, L.; Imbert, P. The Involvement of the Anterolateral Ligament in Rotational Control of the Knee. Am. J. Sports Med. 2016, 44, 1209–1214. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.H.; Lee, Y.S.; Ha, H.C. Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am. J. Sports Med. 2008, 36, 1889–1895. [Google Scholar] [CrossRef] [PubMed]
- Grossman, M.G.; ElAttrache, N.S.; Shields, C.L.; Glousman, R.E. Revision anterior cruciate ligament reconstruction: Three- to nine-year follow-up. Arthroscopy 2005, 21, 418–423. [Google Scholar] [CrossRef]
- Paterno, M.V.; Schmitt, L.C.; Ford, K.R.; Rauh, M.J.; Myer, G.D.; Huang, B.; Hewett, T.E. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am. J. Sports Med. 2010, 38, 1968–1978. [Google Scholar] [CrossRef]
- Gribble, P.A.; Hertel, J.; Plisky, P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: A literature and systematic review. J. Athl. Train. 2012, 47, 339–357. [Google Scholar] [CrossRef]
- Herrington, L.; Hatcher, J.; Hatcher, A.; McNicholas, M. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. Knee 2009, 16, 149–152. [Google Scholar] [CrossRef]
- Head, P.L.; Kasser, R.; Appling, S.; Cappaert, T.; Singhal, K.; Zucker-Levin, A. Anterior cruciate ligament reconstruction and dynamic stability at time of release for return to sport. Phys. Ther. Sport 2019, 38, 80–86. [Google Scholar] [CrossRef]
- Van Lieshout, R.; Reijneveld, E.A.; van den Berg, S.M.; Haerkens, G.M.; Koenders, N.H.; de Leeuw, A.J.; van Oorsouw, R.G.; Paap, D.; Scheffer, E.; Weterings, S.; et al. Reproducibility of the Modified Star Excursion Balance Test Composite and Specific Reach Direction Scores. Int. J. Sports Phys. Ther. 2016, 11, 356–365. [Google Scholar]
- Overmoyer, G.V.; Reiser, R.F., 2nd. Relationships between lower-extremity flexibility, asymmetries, and the Y balance test. J. Strength Cond. Res. 2015, 29, 1240–1247. [Google Scholar] [CrossRef] [PubMed]

| Group A (n = 20) | Group B (n = 19) | p Value | |
|---|---|---|---|
| Gender (Male/Female) | 16/4 | 16/3 | 0.732 a |
| Age * (years) | 25.5 ± 7.87 | 27.3 ± 10.07 | 0.642 b |
| Body Mass Index * (kg/m2) | 26.3 ± 5.2 | 25.5 ± 3.1 | 0.955 b |
| Involved leg (Right/Left) | 8/12 | 10/9 | 0.429 a |
| Group A (n = 20) | Group B (n = 19) | p Value | |
|---|---|---|---|
| Lysholm score * | |||
| Preoperative | 73.1 ± 9.8 | 71.9 ± 13.0 | 0.755 a |
| Postoperative 1 year | 91.4 ± 10.7 | 91.4 ± 10.9 | 0.678 b |
| p value | <0.001 c | 0.004 c | |
| Tegner activity score * | |||
| Preoperative | 6.9 ± 2.6 | 6.8 ± 2.2 | 0.989 b |
| Postoperative 1 year | 6.9 ± 2.0 | 7.6 ± 1.8 | 0.196 b |
| p value | 0.791 c | 0.092 c | |
| IKDC subjective score * | |||
| Preoperative | 65.0 ± 12.9 | 68.3 ± 10.7 | 0.383 a |
| Postoperative 1 year | 88.4 ± 12.7 | 90.5 ± 11.6 | 0.581 b |
| p value | <0.001 c | <0.001 c | |
| Group A (n = 20) | Group B (n = 19) | p Value | |
|---|---|---|---|
| Knee extensor strength deficit compared to the contralateral limb (%, 60°/s Biodex dynamometer) * | |||
| Preoperative | 25.7 ± 23.1 | 27.6 ± 18.3 | 0.779 a |
| Postoperative 1 year | 14.5 ± 15.3 | 11.2 ± 11.8 | 0.463 a |
| p value | 0.008 c | 0.002 c | |
| Knee flexor strength deficit compared to the contralateral limb (%, 60°/s Biodex dynamometer) * | |||
| Preoperative | 18.8 ± 17.1 | 20.4 ± 21.7 | 0.807 a |
| Postoperative 1 year | 0.2 ± 27.4 | 9.0 ± 12.5 | 0.273 b |
| p value | 0.006 c | 0.035 d | |
| Group A (n = 20) | Group B (n = 19) | p Value | |
|---|---|---|---|
| Limb symmetry index (%) * | 88.2 ± 13.5 | 89.9 ± 12.7 | 0.715 a |
| Group A (n = 20) | Group B (n = 19) | p Value | |
|---|---|---|---|
| YBT composite score LSI (%) * | |||
| Preoperative | 90.4 ± 6.7 | 89.3 ± 5.5 | 0.594 a |
| Postoperative 1 year | 97.2 ± 4.0 | 100.3 ± 2.9 | 0.010 a |
| p value | <0.001 c | <0.001 c | |
| YBT anterior reach score LSI (%) * | |||
| Preoperative | 87.3 ± 4.8 | 87.8 ± 13.3 | 0.856 a |
| Postoperative 1 year | 96.0 ± 7.4 | 99.7 ± 6.5 | 0.105 a |
| p value | <0.001 c | 0.001 c | |
| YBT posteromedial reach score LSI (%) * | |||
| Preoperative | 91.1 ± 11.4 | 91.4 ± 6.5 | 0.383 b |
| Postoperative 1 year | 97.6 ± 4.2 | 100.2 ± 4.3 | 0.063 a |
| p value | 0.008 d | 0.001 d | |
| YBT score posterolateral portion LSI (%) * | |||
| Preoperative | 91.9 ± 9.4 | 88.3 ± 6.5 | 0.175 a |
| Postoperative 1 year | 97.7 ± 6.5 | 100.9 ± 4.3 | 0.581 b |
| p value | 0.010 d | <0.001 c | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.K.; Cho, S.-I.; Lee, D.-W.; Yang, S.-J.; Kim, T.-W.; Kim, J.-G. Additional Anterolateral Ligament Reconstruction Helps Patients Improve Dynamic Postural Stability in Revision Anterior Cruciate Ligament Reconstruction. Medicina 2023, 59, 1242. https://doi.org/10.3390/medicina59071242
Lee JK, Cho S-I, Lee D-W, Yang S-J, Kim T-W, Kim J-G. Additional Anterolateral Ligament Reconstruction Helps Patients Improve Dynamic Postural Stability in Revision Anterior Cruciate Ligament Reconstruction. Medicina. 2023; 59(7):1242. https://doi.org/10.3390/medicina59071242
Chicago/Turabian StyleLee, Joon Kyu, Seung-Ik Cho, Dhong-Won Lee, Sang-Jin Yang, Tae-Wook Kim, and Jin-Goo Kim. 2023. "Additional Anterolateral Ligament Reconstruction Helps Patients Improve Dynamic Postural Stability in Revision Anterior Cruciate Ligament Reconstruction" Medicina 59, no. 7: 1242. https://doi.org/10.3390/medicina59071242
APA StyleLee, J. K., Cho, S.-I., Lee, D.-W., Yang, S.-J., Kim, T.-W., & Kim, J.-G. (2023). Additional Anterolateral Ligament Reconstruction Helps Patients Improve Dynamic Postural Stability in Revision Anterior Cruciate Ligament Reconstruction. Medicina, 59(7), 1242. https://doi.org/10.3390/medicina59071242






