Prevalence and Clinical Implications of Incidental Aortic Arch Abnormalities on Contrast-Enhanced Neck MR Angiography: A Single-Center Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Imaging Parameters of Contrast-Enhanced Neck MR Angiography
2.3. Imaging Analyses
2.4. Statistical Analyses
3. Results
3.1. Study Patients
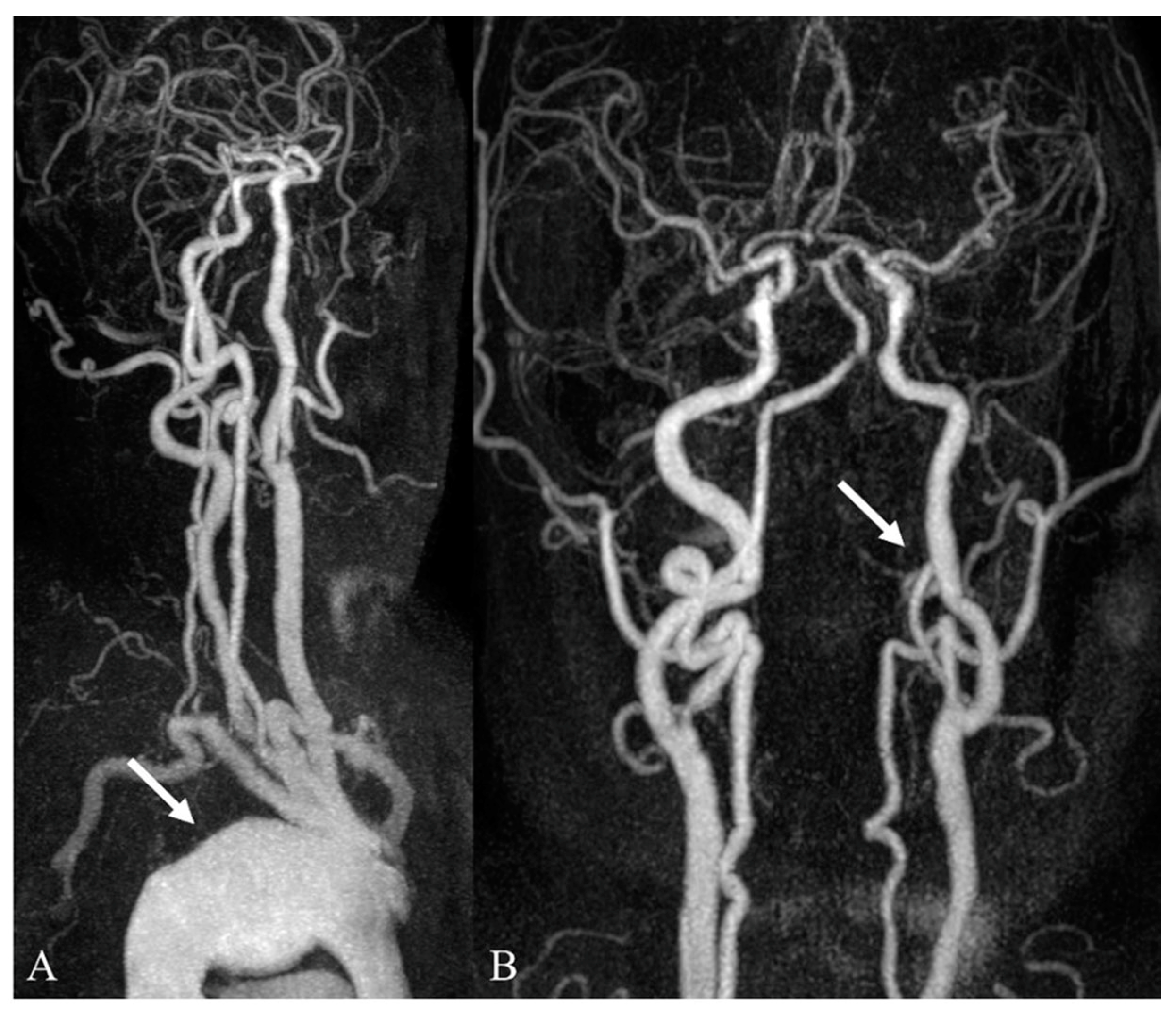
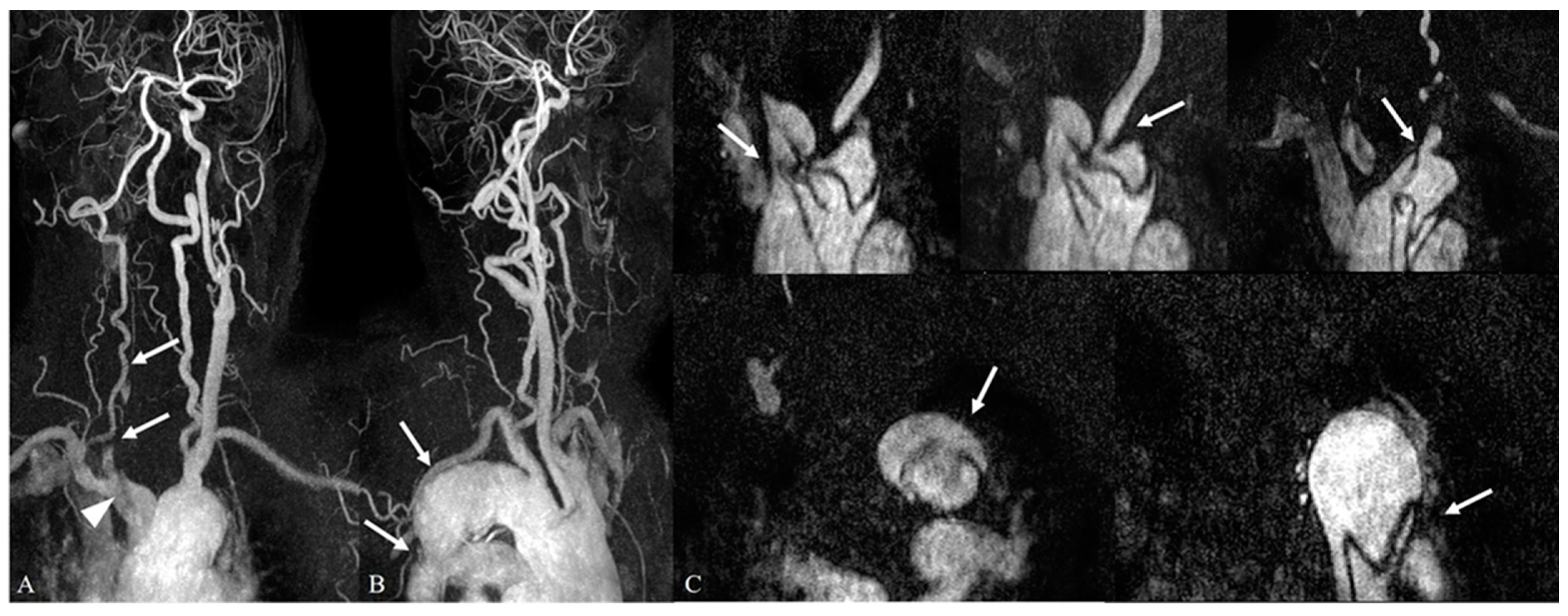
3.2. Incidental Aortic Arch Abnormalities on Contrast-Enhanced Neck MR Angiography
3.3. Intracranial and Extracranial Arterial Abnormalities beyond the Aortic Arch on Contrast-Enhanced Neck MR Angiography
3.4. Comparison between the Aortic Arch Abnormalities and Coexisting Supra-Aortic Arterial Abnormalities According to Clinical Significance
3.5. Comparison of Location-Specific Coexisting Arterial Abnormalities with Aortic Arch Abnormalities According to Clinical Significance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Colletti, P.M. Incidental findings on cardiac imaging. AJR Am. J. Roentgenol. 2008, 191, 882–884. [Google Scholar] [CrossRef] [PubMed]
- Caban, M.; Małecka-Wojciesko, E. Pancreatic incidentaloma. J. Clin. Med. 2022, 11, 4648. [Google Scholar] [CrossRef] [PubMed]
- Lumbreras, B.; Donat, L.; Hernández-Aguado, I. Incidental findings in imaging diagnostic tests: A systematic review. Br. J. Radiol. 2010, 83, 276–289. [Google Scholar] [CrossRef] [PubMed]
- Morris, Z.; Whiteley, W.N.; Longstreth, W.T., Jr.; Weber, F.; Lee, Y.C.; Tsushima, Y.; Alphs, H.; Ladd, S.C.; Warlow, C.; Wardlaw, J.M.; et al. Incidental findings on brain magnetic resonance imaging: Systematic review and meta-analysis. BMJ 2009, 339, b3016. [Google Scholar] [CrossRef] [PubMed]
- Flor, N.; Di Leo, G.; Squarza, S.A.; Tresoldi, S.; Rulli, E.; Cornalba, G.; Sardanelli, F. Malignant incidental extracardiac findings on cardiac CT: Systematic review and meta-analysis. AJR Am. J. Roentgenol. 2013, 201, 555–564. [Google Scholar] [CrossRef]
- Xiong, T.; Richardson, M.; Woodroffe, R.; Halligan, S.; Morton, D.; Lilford, R.J. Incidental lesions found on CT colonography: Their nature and frequency. Br. J. Radiol. 2005, 78, 22–29. [Google Scholar] [CrossRef]
- Desal, H.; Auffray-Calvier, E.; Toulgoat, F.; Guillon, B.; Madoz, A.; de Kersaint-Gilly, A. ARM des vaisseaux cervico-encéphaliques: Technique, principales applications cliniques MR-angiography of the head and neck vessels: Technical considerations and clinical indications. J. Radiol. 2005, 86, 1117–1123. [Google Scholar] [CrossRef]
- Makdissi, J.; Pawar, R.R.; Radon, M.; Holmes, S.B. Incidental findings on MRI of the temporomandibular joint. Dentomaxillofac. Radiol. 2013, 42, 20130175. [Google Scholar] [CrossRef]
- Nam, I.C.; Baek, H.J.; Ryu, K.H.; Moon, J.I.; Cho, E.; An, H.J.; Yoon, S.; Baik, J. Prevalence and clinical implications of incidentally detected parotid lesions as blind spot on brain MRI: A single-center experience. Medicina 2021, 57, 836. [Google Scholar] [CrossRef]
- Boggs, R.A.; Romp, R.L. Persistent fifth aortic arch confirmed by computed tomography angiography. World J. Pediatr. Congenit. Heart Surg. 2015, 6, 670–671. [Google Scholar] [CrossRef]
- Case, D.; Seinfeld, J.; Folzenlogen, Z.; Kumpe, D. Anomalous right vertebral artery originating from the aortic arch distal to the left subclavian artery: A case report and review of the literature. J. Vasc. Interv. Neurol. 2015, 8, 21–24. [Google Scholar]
- Hanneman, K.; Newman, B.; Chan, F. Congenital variants and anomalies of the aortic arch. Radiographics 2017, 37, 32–51. [Google Scholar] [CrossRef]
- Uehara, K.; Matsuda, H.; Matsuo, J.; Inoue, Y.; Omura, A.; Seike, Y.; Sasaki, H.; Kobayashi, J. Acute type A aortic dis-section repair in younger patients. J. Card. Surg. 2018, 33, 184–189. [Google Scholar] [CrossRef]
- Rositzka, M.; Hoffmann, K.T.; Meyer, H.J.; Surov, A. Incidental findings on CT angiography of the head and neck in stroke patients. Evaluation of frequency and detection rate. Clin. Neurol. Neurosurg. 2020, 193, 105783. [Google Scholar] [CrossRef]
- Chen, G.; Xue, Y.; Wei, J.; Duan, Q. The undiagnosed potential clinically significant incidental findings of neck CTA: A large retrospective single-center study. Medicine 2020, 99, e22440. [Google Scholar] [CrossRef]
- Pawlukiewicz, A.J.; Long, D.; Mehta, S. Large vessel occlusion stroke secondary to acute aortic dissection. Cureus 2020, 12, e9278. [Google Scholar] [CrossRef]
- Methodius-Ngwodo, W.C.; Burkett, A.B.; Kochupura, P.V.; Wellons, E.D.; Fuhrman, G.; Rosenthal, D. The role of CT angiography in the diagnosis of blunt traumatic thoracic aortic disruption and unsuspected carotid artery injury. Am. Surg. 2008, 74, 580–585; discussion 585–586. [Google Scholar] [CrossRef]
- Wangaryattawanich, P.; Rutman, A.M.; Petcharunpaisan, S.; Mossa-Basha, M. Incidental findings on brain magnetic resonance imaging (MRI) in adults: A review of imaging spectrum, clinical significance, and management. Br. J. Radiol. 2023, 96, 20220108. [Google Scholar] [CrossRef]
- Rutman, A.M.; Wangaryattawanich, P.; Aksakal, M.; Mossa-Basha, M. Incidental vascular findings on brain magnetic resonance angiography. Br. J. Radiol. 2023, 96, 20220135. [Google Scholar] [CrossRef]
- Suri, M.F.; Qiao, Y.; Ma, X.; Guallar, E.; Zhou, J.; Zhang, Y.; Liu, L.; Chu, H.; Qureshi, A.I.; Alonso, A.; et al. Prevalence of intra-cranial atherosclerotic stenosis using high-resolution magnetic resonance angiography in the general population: The athero-sclerosis risk in communities study. Stroke 2016, 47, 1187–1193. [Google Scholar] [CrossRef]
- Jin, H.; Peng, Q.; Nan, D.; Lv, P.; Liu, R.; Sun, W.; Teng, Y.; Liu, Y.; Fan, C.; Xing, H.; et al. Prevalence and risk factors of intracranial and extracranial artery stenosis in asymptomatic rural residents of 13 villages in China. BMC Neurol. 2017, 17, 136. [Google Scholar] [CrossRef] [PubMed]
- Pourier, V.E.C.; van Laarhoven, C.J.H.C.M.; Vergouwen, M.D.I.; Rinkel, G.J.E.; de Borst, G.J. Prevalence of extracranial carotid artery aneurysms in patients with an intracranial aneurysm. PLoS ONE 2017, 12, e0187479. [Google Scholar] [CrossRef] [PubMed]
- Hakim, A.; Gralla, J.; Rozeik, C.; Mordasini, P.; Leidolt, L.; Piechowiak, E.; Ozdoba, C.; El-Koussy, M. Anomalies and normal variants of the cerebral arterial supply: A comprehensive pictorial review with a proposed workflow for classification and significance. J. Neuroimaging 2018, 28, 14–35. [Google Scholar] [CrossRef] [PubMed]
- Kovač, J.D.; Stanković, A.; Stanković, D.; Kovač, B.; Šaranović, D. Intracranial arterial variations: A comprehensive evaluation using CT angiography. Med. Sci. Monit. 2014, 20, 420–427. [Google Scholar] [CrossRef]
- Kim, Y.S.; Park, H.Y.; Yun, K.H.; Park, H.; Cheong, J.S.; Ha, Y.S. Association of aortic knob calcification with intracranial stenosis in ischemic stroke patients. J. Stroke 2013, 15, 122–125. [Google Scholar] [CrossRef]
- Yamanaka, O.; Sawano, M.; Nakayama, R.; Nemoto, M.; Nakamura, T.; Fujiwara, Y.; Suzuki, S.; Hayashi, Y.; Yamagami, S.; Minamisawa, K.; et al. Clinical significance of coronary calcification. Circ. J. 2002, 66, 473–478. [Google Scholar] [CrossRef]



| Aortic Arch Abnormalities | Number of Patients (%) | Number of Lesions (%) |
|---|---|---|
| Category I (Clinically significant findings) | 29/348 (8.3%) | 29/348 (8.3%) |
| Aortic dissection | 22/348 (6.3%) | |
| Aortic aneurysm | 7/348 (2.0%) | |
| Category II (Minor or no significant findings) | 319/348 (91.7%) | 331/348 (95.1%) |
| Direct aortic arch origin of vertebral artery | 280/348 (80.4%) | |
| Aberrant right subclavian artery | 39/348 (11.2%) | |
| Common trunk | 8/348 (2.3%) | |
| Right-sided aortic arch | 4/348 (1.2%) |
| Arterial Abnormalities | Intracranial Abnormality (250/348, 71.8%) | Extracranial Abnormality (136/348, 39%) |
|---|---|---|
| Category I (Clinically significant findings) | 130/250 (52.0%) | 38/136 (27.9%) |
| Severe stenosis | 37/250 (14.8%) | 23/136 (16.9%) |
| Occlusion | 23/250 (9.2%) | 10/136 (7.4%) |
| Aneurysm | 66/250 (26.4%) | 5/136 (3.7%) |
| Arteriovenous malformation | 4/250 (1.6%) | NA |
| Category II (Minor or no significant findings) | 232/250 (92.8%) | 112/136 (82.4%) |
| Mild to moderate stenosis | 106/250 (42.4%) | 94/136 (69.1%) |
| Penetrating atherosclerotic ulcer | 18/250 (7.2%) | 8/136 (5.9%) |
| Junctional dilatation | 17/250 (6.8%) | 2/136 (1.5%) |
| Congenital anomaly | 75/250 (30%) | 7/136 (5.1%) |
| Stent placement | 16/250 (6.4%) | 1/136 (0.7%) |
| Aortic Arch Abnormalities | p-Value | ||
|---|---|---|---|
| Category I (Clinically Significant Findings) | Category II (Minor or No Significant Findings) | ||
| Coexisting supra-aortic arterial abnormalities | 24/29 (82.7%) | 259/319 (81.2%) | NA |
| Category I (Clinically significant findings) Category II (Minor or no significant findings) | 13/29 (44.8%) | 87/319 (27.3%) | 0.044 |
| 11/29 (37.9%) | 172/319 (53.9%) | ||
| Aortic Arch Abnormalities | p-Value | ||
|---|---|---|---|
| Category I (Clinically Significant Findings) | Category II (Minor or No Significant Findings) | ||
| Intracranial arterial abnormalities | 21/29 (72.4%) | 229/319 (72.0%) | NA |
| Category I (Clinically significant findings) Category II (Minor or no significant findings) | 9/29 (31.0%) | 62/319 (19.4%) | 0.138 |
| 12/29 (41.4%) | 167/319 (52.4%) | ||
| Extracranial arterial abnormalities | 12/29 (41.4%) | 124/319 (38.9%) | NA |
| Category I (Clinically significant findings) Category II (Minor or no significant findings) | 5/29 (17.2%) | 25/319 (7.8%) | 0.136 |
| 7/29 (24.1%) | 99/319 (31.0%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, M.; Choi, D.-S.; Choi, K.-H.; Baek, H.-J.; Cho, E.; Park, J.-M. Prevalence and Clinical Implications of Incidental Aortic Arch Abnormalities on Contrast-Enhanced Neck MR Angiography: A Single-Center Experience. Medicina 2023, 59, 1172. https://doi.org/10.3390/medicina59061172
Hwang M, Choi D-S, Choi K-H, Baek H-J, Cho E, Park J-M. Prevalence and Clinical Implications of Incidental Aortic Arch Abnormalities on Contrast-Enhanced Neck MR Angiography: A Single-Center Experience. Medicina. 2023; 59(6):1172. https://doi.org/10.3390/medicina59061172
Chicago/Turabian StyleHwang, Minhee, Dae-Seob Choi, Kwang-Ho Choi, Hye-Jin Baek, Eun Cho, and Jong-Myung Park. 2023. "Prevalence and Clinical Implications of Incidental Aortic Arch Abnormalities on Contrast-Enhanced Neck MR Angiography: A Single-Center Experience" Medicina 59, no. 6: 1172. https://doi.org/10.3390/medicina59061172
APA StyleHwang, M., Choi, D.-S., Choi, K.-H., Baek, H.-J., Cho, E., & Park, J.-M. (2023). Prevalence and Clinical Implications of Incidental Aortic Arch Abnormalities on Contrast-Enhanced Neck MR Angiography: A Single-Center Experience. Medicina, 59(6), 1172. https://doi.org/10.3390/medicina59061172






