Foreign Body Aspiration in Children—Retrospective Study and Management Novelties
Abstract
1. Introduction
2. Material and Methods
3. Results
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ulas, A.B.; Aydin, Y.; Eroglu, A. Foreign body aspirations in children and adults. Am. J. Surg. 2022, 224, 1168–1173. [Google Scholar] [CrossRef] [PubMed]
- Brkic, F.; Umihanic, S.; Altumbabic, H.; Ramas, A.; Salkic, A.; Umihanic, S.; Mujic, M.; Softic, L.; Zulcic, S. Death as a Consequence of Foreign Body Aspiration in Children. Med. Arch. 2018, 72, 220–223. [Google Scholar] [CrossRef] [PubMed]
- Abd-ElGawad, E.A.; Ibrahim, M.A.; Mubarak, Y.S. Tracheobronchial foreign body aspiration in infants & children: Diagnostic utility of multidetector CT with emphasis on virtual bronchoscopy. Egypt. J. Radiol. Nucl. Med. 2014, 45, 1141–1146. [Google Scholar] [CrossRef]
- Engin, M.M.N.; Erdogan, F.; Kucuk, Ö.; Kaya, M. Foreign body aspiration in an 11-month-old child; the importance of anamnesis and respiratory examination. J. Pediatr. Neonatal Care 2020, 10, 156–157. [Google Scholar] [CrossRef]
- Safari, M.; Hashemi Manesh, M.R. Demographic and clinical findings in children undergoing bronchoscopy for foreign body aspiration. Ochsner J. 2016, 16, 120–124. [Google Scholar]
- Sahadan, D.Z.; Zainudin, N.M.; Kassim, A.; Zahari, Z.; Mahadzir, M.; Che Daud, C.Z.; Mohammad, N. Case serires of foreign body aspiration in Paediatric Institute, Hospital Kuala Lumpur. Med. J. Malays. 2011, 66, 484–486. [Google Scholar]
- Holliday, S.; Gurkowski, M.A. Chapter 188—Foreign body aspiration. In Complications in Anesthesia, 2nd ed.; Elsevier Health Sciences: Philadelphia, PA, USA, 2007; pp. 753–755. [Google Scholar]
- Baram, A.; Sherzad, H.; Saeed, S.; Kakamad, F.H.; Hamawandi, A.M.H. Tracheobronchial Foreign Bodies in Children: The Role of Emergency Rigid Bronchoscopy. Glob. Pediatr. Health 2017, 4, 2333794x17743663. [Google Scholar] [CrossRef]
- Dorofaeff, T.; Plumpton, K. 105—Acute respiratory failure in children. In Oh’s Intensive Care Manual, 2nd ed.; Andrew, D., Bersten, N.S., Eds.; Butterworth-Heinemann: Woburn, MA, USA, 2014; pp. 1085–1095. [Google Scholar]
- Morris, I.R. Anesthesia and Airway Management of Laryngoscopy and Bronchoscopy. In Benumof’s Airway Management; Mosby: London, UK, 2007; pp. 859–888. [Google Scholar] [CrossRef]
- Gatto, A.; Capossela, L.; Ferretti, S.; Orlandi, M.; Pansini, V.; Curatola, A.; Chiaretti, A. Foreign Body Ingestion in Children: Epidemiological, Clinical Features and Outcome in a Third Level Emergency Department. Children 2021, 8, 1182. [Google Scholar] [CrossRef]
- Ikenberry, S.O.; Jue, T.L.; Anderson, M.A.; Appalaneni, V.; Banerjee, S.; Ben-Menachem, T.; Decker, G.A.; Fanelli, R.D.; Fisher, L.R.; Fukami, N.; et al. Management of ingested foreign bodies and food impactions. Gastrointest. Endosc. 2011, 73, 1085–1091. [Google Scholar] [CrossRef]
- Eren, Ş.; Balci, A.E.; Dikici, B.; Doblan, M.; Eren, M.N. Foreign body aspiration in children: Experience of 1160 cases. Ann. Trop. Paediatr. 2003, 23, 31–37. [Google Scholar] [CrossRef]
- Berry, F.; Stemland, C. Foreign body aspiration. In Essence of Anesthesia Practice, 3rd ed.; Elsevier Health Sciences: Philadelphia, PA, USA, 2011; p. 156. [Google Scholar]
- Mohammad, M.; Saleem, M.; Mahseeri, M.; Alabdallat, I.; Alomari, A.; Za’atreh, A.; Qudaisat, I.; Shudifat, A.; Nasri Alzoubi, M. Foreign body aspiration in children: A study of children who lived or died following aspiration. Int. J. Pediatr. Otorhinolaryngol. 2017, 98, 29–31. [Google Scholar] [CrossRef]
- Xu, Y.; Feng, R.L.; Jiang, L.; Ren, H.B.; Li, Q. Correlative factors for the location of tracheobronchial foreign bodies in infants and children. J. Thorac. Dis. 2018, 10, 1037–1042. [Google Scholar] [CrossRef]
- Nasir, Z.M.; Subha, S.T. A Five-Year Review on Pediatric Foreign Body Aspiration. Int. Arch. Otorhinolaryngol. 2021, 25, e193. [Google Scholar] [CrossRef]
- Fidkowski, C.W.; Zheng, H.; Firth, P.G. The anesthetic considerations of tracheobronchial foreign bodies in children: A literature review of 12,979 cases. Anesth. Analg. 2010, 111, 1016–1025. [Google Scholar] [CrossRef]
- Ding, G.; Wu, B.; Vinturache, A.; Cai, C.; Lu, M.; Gu, H. Tracheobronchial foreign body aspiration in children: A retrospective single-center cross-sectional study. Medicine 2020, 99, e20480. [Google Scholar] [CrossRef]
- Field, N.; Cohen, T.; Struelens, M.J.; Palm, D.; Cookson, B.; Glynn, J.R.; Gallo, V.; Ramsay, M.; Sonnenberg, P.; MacCannell, D.; et al. Strengthening the Reporting of Molecular Epidemiology for Infectious Diseases (STROME-ID): An extension of the STROBE statement. Lancet Infect. Dis. 2014, 14, 341–352. [Google Scholar] [CrossRef]
- Dehghani, N.; Ludemann, P. Aspirated foreign bodies in children: BC Children’s Hospital emergency room protocol. BCMJ BC Med. J. 2008, 50, 252–256. [Google Scholar]
- Tang, L.F.; Xu, Y.C.; Wang, Y.S.; Wang, C.F.; Zhu, G.H.; Bao, X.E.; Lu, M.P.; Chen, L.X.; Chen, Z.M. Airway foreign body removal by flexible bronchoscopy: Experience with 1027 children during 2000–2008. World J. Pediatr. 2009, 5, 191–195. [Google Scholar] [CrossRef]
- Gvetadze, P.; Chkhaidze, I.; Baldas, S.; Comoretto, R.; Gregori, D.; Berchialla, P.; Rodriguez, H.; Zaupa, P.; Spitzer, P.; Demetriades, C.; et al. Injuries due to foreign body aspirations in Georgia: A prevention perspective. Int. J. Pediatr. Otorhinolaryngol. 2016, 83, 84–87. [Google Scholar] [CrossRef]
- Tomaske, M.; Gerber, A.C.; Stocker, S.; Weiss, M. Tracheobronchial foreign body aspiration in children-diagnostic value of symptoms and signs. Swiss Med. Wkly. 2006, 136, 533–538. [Google Scholar]
- Kalyanappagol, V.T.; Kulkarni, N.H.; Bidri, L.H. Management of tracheobronchial foreign body aspirations in paediatric age group-a 10 year retrospective analysis. Indian J. Anaesth. 2007, 51, 20–23. [Google Scholar]
- Nyeki, A.R.N.; Miloundja, J.; Dalil, A.B.; Lawson, J.M.M.; Nzenze, S.; Sougou, E.; Nziengui, A.; N’zouba, L. Les corps étrangers laryngo-trachéo-bronchiques: Expérience de l’hôpital d’instruction des armées Omar Bongo Ondimba (HIAOBO) de Libreville. Pan Afr. Med. J. 2015, 20, 298. [Google Scholar] [CrossRef] [PubMed]
- Haller, L.; Barazzone-Argiroffo, C.; Vidal, I.; Corbelli, R.; Anooshiravani-Dumont, M.; Mornand, A. Safely decreasing rigid bronschoscopies for foreign-body aspiration in children: An algorithm for the emergency department. Eur. J. Pediatr. Surg. 2018, 28, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Fasseeh, N.A.; Elagamy, O.A.; Gaafar, A.H.; Reyad, H.M.; Abougabal, M.S.; Heiba, D.A.; Kantar, A. A new scoring system and clinical algorithm for the management of suspected foreign body aspiration in children: A retrospective cohort study. Ital. J. Pediatr. 2021, 47, 194. [Google Scholar] [CrossRef]
- Rance, A.; Mittaine, M.; Michelet, M.; Martin Blondel, A.; Labouret, G. Delayed diagnosis of foreign body aspiration in children. Arch. Pediatr. 2022, 29, 424–428. [Google Scholar] [CrossRef]
- Divarci, E.; Toker, B.; Dokumcu, Z.; Musayev, A.; Ozcan, C.; Erdener, A. The multivariate analysis of indications of rigid bronchoscopy in suspected foreign body aspiration. Int. J. Pediatr. Otorhinolaryngol. 2017, 100, 232–237. [Google Scholar] [CrossRef]
- Buonsenso, D.; Chiaretti, A.; Curatola, A.; Morello, R.; Giacalone, M.; Parri, N. Pediatrician performed point-of-care ultrasound for the detection of ingested foreign bodies: Case series and review of the literature. J. Ultrasound 2021, 24, 107–114. [Google Scholar] [CrossRef]
| Characteristic | Frequency | Percentage |
|---|---|---|
| Total number of patients | 232 | |
| Sex | ||
| Male:Female ratio | 1.77 | |
| Age | ||
| <1 year old | 17 | 7.32% |
| 1–3 years old | 182 | 78.45% |
| 4–16 years old | 33 | 14.22% |
| Place of origin | ||
| Rural area | 162 | 69.82% |
| Urban area | 70 | 30.17% |
| No. of cases based of the nature of the foreign body | ||
| Organic + inorganic bodies | 10 | 4.31% |
| Organic (vegetable) bodies (alone and combined) | 202 | |
| Seeds | 111 | 55% |
| Hazelnut | 47 | 23% |
| Walnut kernel | 26 | 13% |
| Corn kernel | 10 | 5% |
| Beans | 8 | 4% |
| Inorganic bodies | 20 | |
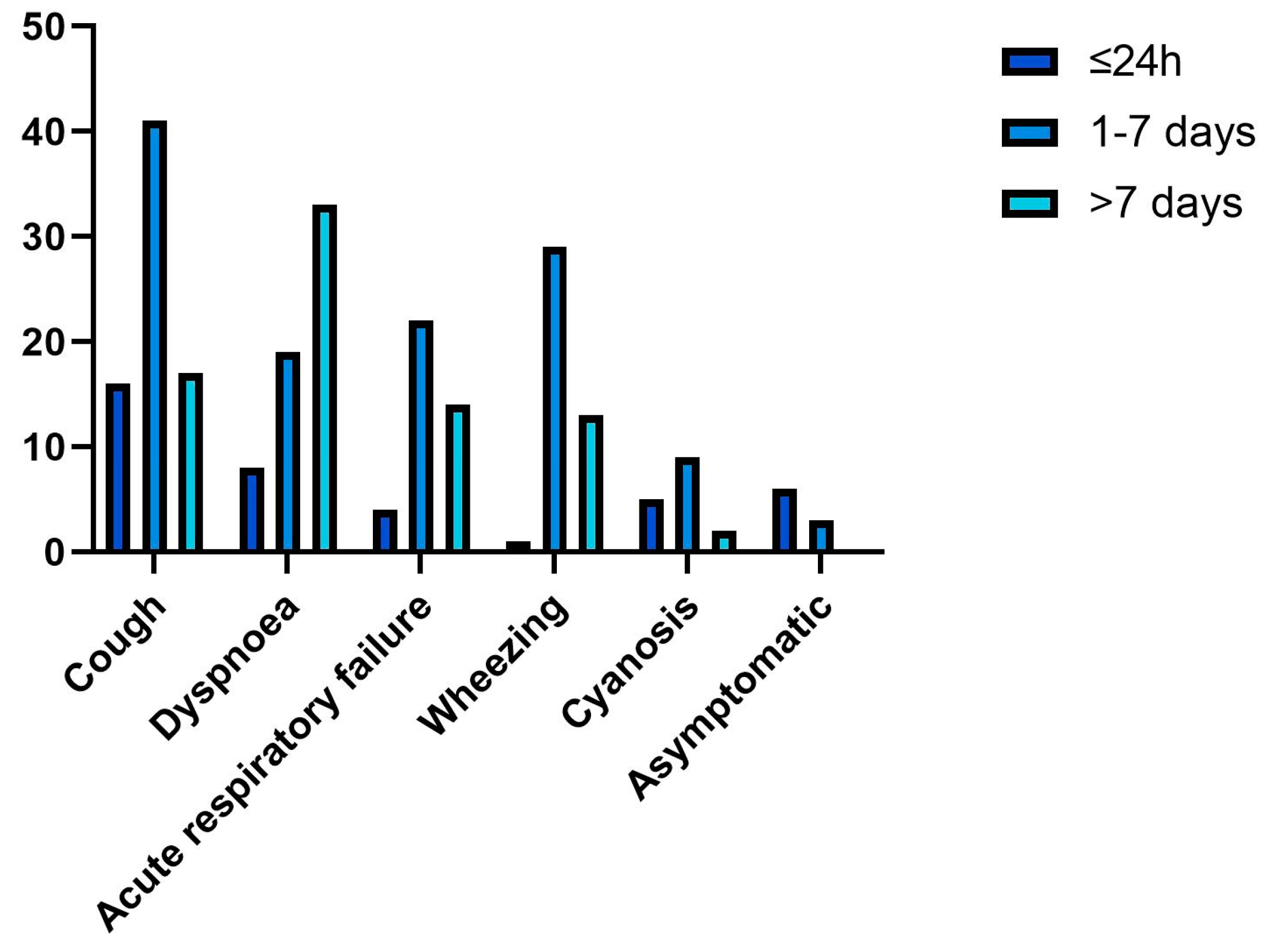
| Time of admission | ||
| Within the first 24 h | 49 | 21% |
| After the first 24 h | 143 | 61.63% |
| After 7 days | 40 | 16.94% |
| Main clinical manifestation | ||
| Sudden onset of cough | 77 | 33.05% |
| Dyspnea | 49 | 21.09% |
| Acute respiratory failure | 44 | 19% |
| Wheezing | 35 | 14.87% |
| Cyanosis | 21 | 9.09% |
| Initial clinical examination | ||
| Decreased lung sounds | 78 | 33.62% |
| Bronchial obstruction and coarse vesicular murmur | 55 | 23.7% |
| Bronchial rales | 116 | 50% |
| Aspiration pneumonia and pulmonary obstruction | 32 | 13.79% |
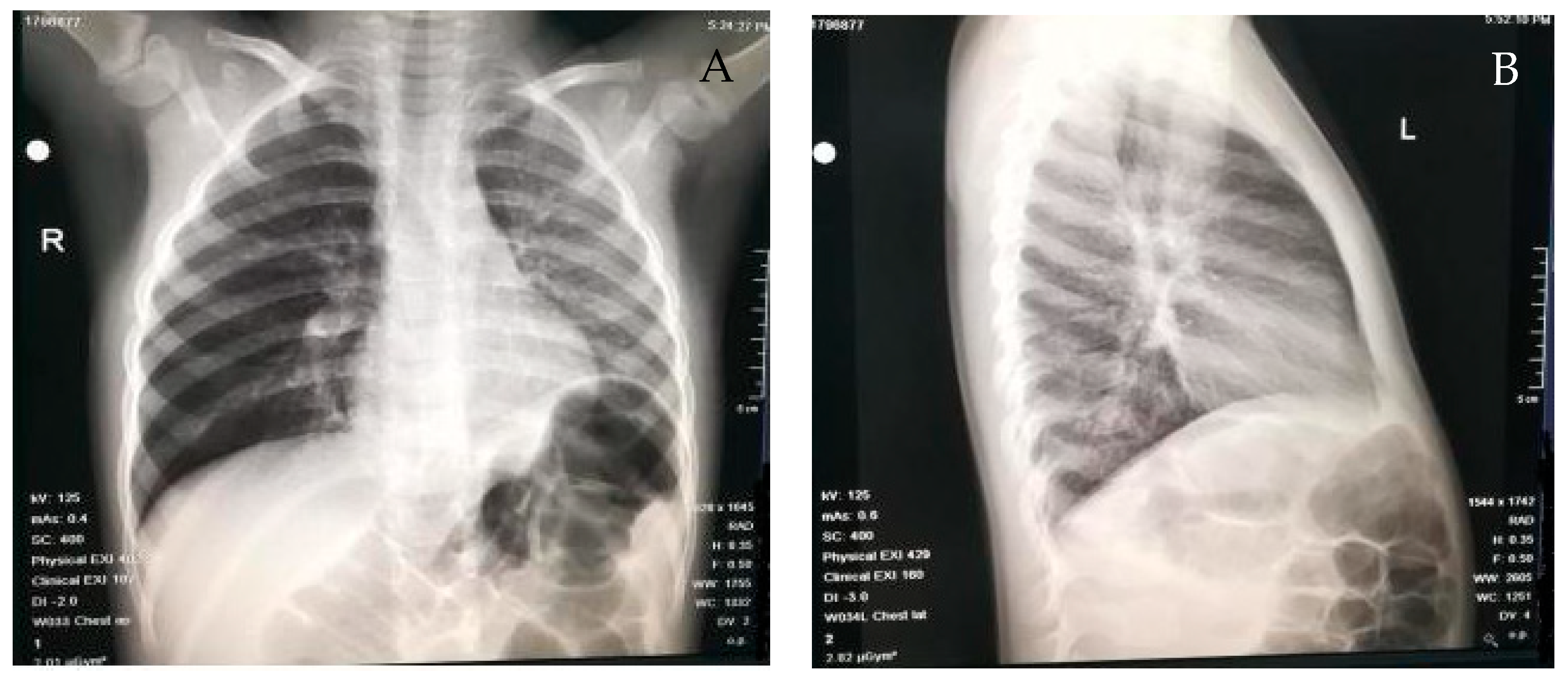
| Chest radiography results | ||
| Pulmonary atelectasis | 62 | 26.85% |
| Pulmonary emphysema | 41 | 17.76% |
| Direct visualization of the foreign body | 8 | 3.44% |
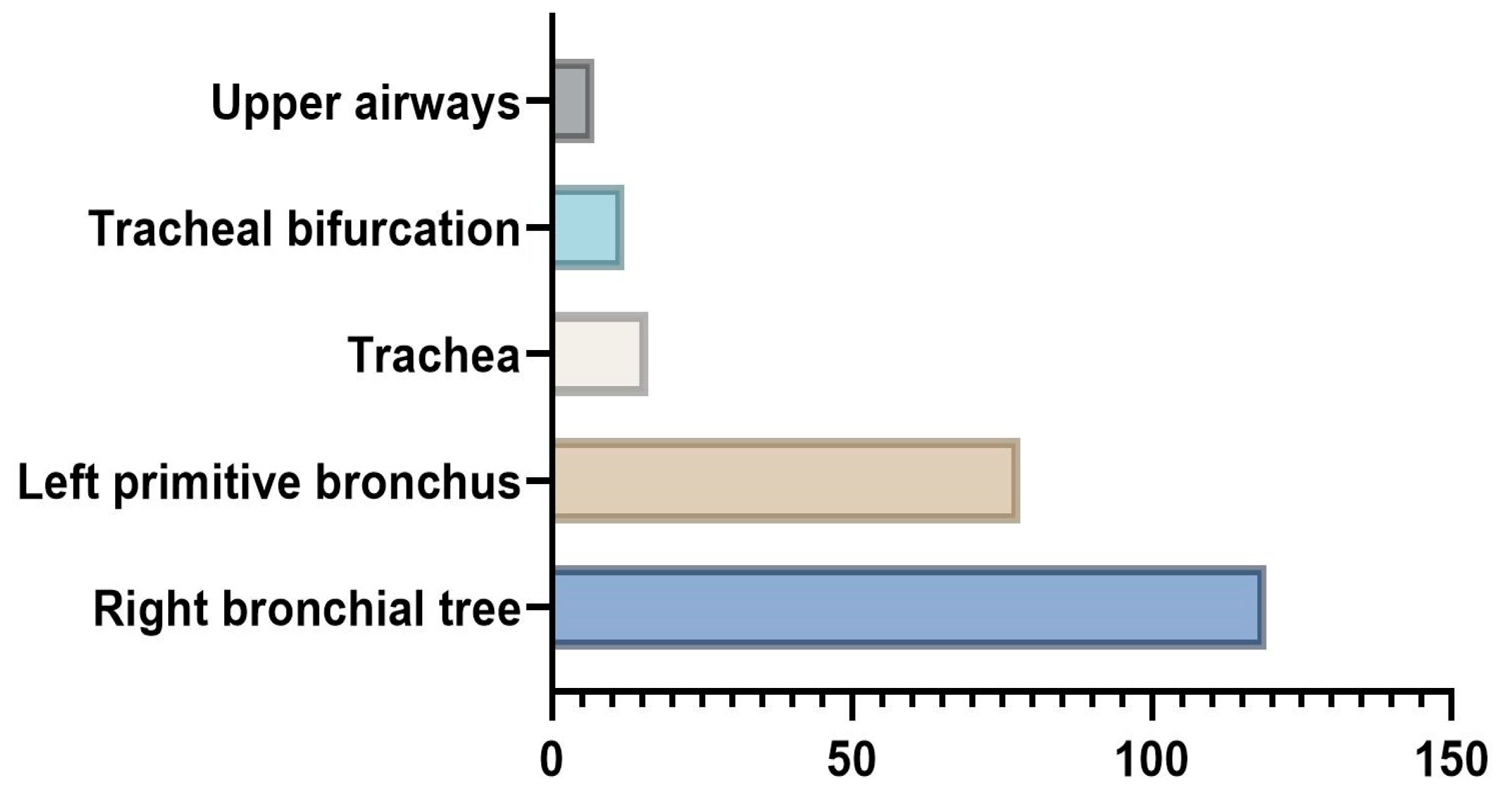
| Location of the foreign body | ||
| Right bronchial tree | 124 | 51.23% |
| Left primitive bronchus | 81 | 33.45% |
| Trachea | 17 | 7.02% |
| Tracheal bifurcation | 13 | 5.37% |
| Upper airways (nostrils and glottis) | 7 | 3% |
| Complications | ||
| Aspiration pneumonia | 123 | 53.01% |
| Acute tracheobronchitis | 13 | 5.6% |
| Laryngitis | 3 | 1.29% |
| Lung abscess | 2 | 0.86% |
| Assisted ventilation | 5 | 2.15% |
| Temporary tracheostomy | 1 | 0.43% |
| Antibiotic therapy | 204 | 88% |
| Period of hospitalization | ||
| <5 days | 107 | 46% |
| >5 days | 125 | 54% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mîndru, D.E.; Păduraru, G.; Rusu, C.D.; Țarcă, E.; Azoicăi, A.N.; Roșu, S.T.; Curpăn, A.-Ș.; Ciomaga Jitaru, I.M.; Pădureț, I.A.; Luca, A.C. Foreign Body Aspiration in Children—Retrospective Study and Management Novelties. Medicina 2023, 59, 1113. https://doi.org/10.3390/medicina59061113
Mîndru DE, Păduraru G, Rusu CD, Țarcă E, Azoicăi AN, Roșu ST, Curpăn A-Ș, Ciomaga Jitaru IM, Pădureț IA, Luca AC. Foreign Body Aspiration in Children—Retrospective Study and Management Novelties. Medicina. 2023; 59(6):1113. https://doi.org/10.3390/medicina59061113
Chicago/Turabian StyleMîndru, Dana Elena, Gabriela Păduraru, Carmen Daniela Rusu, Elena Țarcă, Alice Nicoleta Azoicăi, Solange Tamara Roșu, Alexandrina-Ștefania Curpăn, Irina Mihaela Ciomaga Jitaru, Ioana Alexandra Pădureț, and Alina Costina Luca. 2023. "Foreign Body Aspiration in Children—Retrospective Study and Management Novelties" Medicina 59, no. 6: 1113. https://doi.org/10.3390/medicina59061113
APA StyleMîndru, D. E., Păduraru, G., Rusu, C. D., Țarcă, E., Azoicăi, A. N., Roșu, S. T., Curpăn, A.-Ș., Ciomaga Jitaru, I. M., Pădureț, I. A., & Luca, A. C. (2023). Foreign Body Aspiration in Children—Retrospective Study and Management Novelties. Medicina, 59(6), 1113. https://doi.org/10.3390/medicina59061113







