Association between Patients’ Self-Judgement, Coagulated Menstrual Blood, and Menorrhagia: Results from a Questionnaire Survey and Blood Test Analysis
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Name | |
| Date of birth | Year month date |
| Patient’s number |
- Do you believe that you have an excessive menstrual flow? □ Yes □ No
- Is your menstrual cycle regular?cycles regular? □ Regular □ Irregular
- How many days is your total menstrual period? How many days do you have heavy bleeding during your period?
- -
- Total menstrual period days
- -
- Heavy bleeding days during menstruation days
- How many total sanitary pads (or tampons) do you use during your menstrual period?
- -
- Total
- How many sanitary pads (or tampons) do you use per day on heavy menstrual days?
- -
- Use of sanitary pads (or tampons) on heavy days
- Will your clothes get wet if you don’t use large sanitary napkins, such as overnight sanitary napkins, or multiple sanitary pads in layers during the night? □ Yes □ No
- Do you pass blood clots that are larger than one inch in diameter during your menstrual period? □ Yes □ No
- Have you ever taken an iron supplement or received an iron supplement injection within the last few months due to anemia? □ Yes □ No
- Are you using contraceptives, intrauterine devices (such as Mirena), and implantable contraceptives (such as Implanon) due to excessive menstrual flow? □ Yes □ No
- Are you taking anticoagulants (warfarin, herapin, etc.) or antiplatelet/antithrombotic drugs (Aspirin, plavix or any other antiplatelet /antithrombotic drugs)? □ Yes □ No
- Do you have a coagulopathy disorder or bleeding disorder (thrombocytopenia, leukemia, etc.)? □ Yes □ No
References
- Apgar, B.S.; Kaufman, A.H.; George-Nwogu, U.; Kittendorf, A.L. Treatment of menorrhagia. Am. Fam. Physician 2007, 75, 1813–1819. [Google Scholar]
- Oehler, M.K.; Rees, M.C. Menorrhagia: An update. Acta Obstet. Gynecol. Scand. 2003, 82, 405–422. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J. Menometrorrhagia during the premenopause: An overview. Gynecol. Endocrinol. 2011, 27 (Suppl. S1), 1114–1119. [Google Scholar] [CrossRef] [PubMed]
- Berek, J.S.; Berek, D.L. Berek & Novak’s Gynecology, 16th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2020. [Google Scholar]
- Hallberg, L.; Högdahl, A.-M.; Nilsson, L.; Rybo, G. Menstrual blood loss—A population study. Variation at different ages and attempts to define normality. Acta Obstet. Gynecol. Scand. 1966, 45, 320–351. [Google Scholar]
- Warner, P.E.; Critchley, H.O.; Lumsden, M.A.; Campbell-Brown, M.; Douglas, A.; Murray, G.D. Menorrhagia II: Is the 80-mL blood loss criterion useful in management of complaint of menorrhagia? Am. J. Obstet. Gynecol. 2004, 190, 1224–1229. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.H.; Coffey, W.; Borger, J. Menorrhagia. In StatPearls; Treasure Island: Zephyrhills, FL, USA, 2023. [Google Scholar]
- Fraser, I.S.; Warner, P.; Marantos, P.A. Estimating menstrual blood loss in women with normal and excessive menstrual fluid volume. Obstet. Gynecol. 2001, 98 Pt 1, 806–814. [Google Scholar] [CrossRef]
- van Eijkeren, M.A.; Scholten, P.C.; Christiaens, G.C.; Alsbach, G.P.; Haspels, A.A. The alkaline hematin method for measuring menstrual blood loss—A modification and its clinical use in menorrhagia. Eur. J. Obstet. Gynecol. Reprod. Biol. 1986, 22, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Magnay, J.L.; Schönicke, G.; Nevatte, T.M.; O’Brien, S.; Junge, W. Validation of a rapid alkaline hematin technique to measure menstrual blood loss on feminine towels containing superabsorbent polymers. Fertil. Steril. 2011, 96, 394–398. [Google Scholar] [CrossRef]
- Magnay, J.L.; Nevatte, T.M.; Dhingra, V.; O’Brien, S. Menstrual blood loss measurement: Validation of the alkaline hematin technique for feminine hygiene products containing superabsorbent polymers. Fertil. Steril. 2010, 94, 2742–2746. [Google Scholar] [CrossRef]
- Haberland, C.; Filonenko, A.; Seitz, C.; Börner, M.; Gerlinger, C.; Doll, H.; Wessiepe, D. Validation of a menstrual pictogram and a daily bleeding diary for assessment of uterine fibroid treatment efficacy in clinical studies. J. Patient Rep. Outcomes 2020, 4, 97. [Google Scholar] [CrossRef]
- Ko, J.K.Y.; Lao, T.T.; Cheung, V.Y.T. Pictorial Blood Loss Assessment Chart for evaluating heavy menstrual bleeding in Asian women. Hong Kong Med. J. 2021, 27, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Magnay, J.L.; O’Brien, S.; Gerlinger, C.; Seitz, C. A systematic review of methods to measure menstrual blood loss. BMC Womens Health 2018, 18, 142. [Google Scholar] [CrossRef] [PubMed]
- Magnay, J.L.; Nevatte, T.M.; O’Brien, S.; Gerlinger, C.; Seitz, C. Validation of a new menstrual pictogram (superabsorbent polymer-c version) for use with ultraslim towels that contain superabsorbent polymers. Fertil. Steril. 2014, 101, 515–522. [Google Scholar] [CrossRef]
- Magnay, J.L.; O’brien, S.; Gerlinger, C.; Seitz, C. Pictorial methods to assess heavy menstrual bleeding in research and clinical practice: A systematic literature review. BMC Womens Health 2020, 20, 24. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, U.; Schumacher, J.; Mellinger, U.; Gerlinger, C.; Wienke, A.; Endrikat, J. Estimation of menstrual blood loss volume based on menstrual diary and laboratory data. BMC Womens Health 2012, 12, 24. [Google Scholar] [CrossRef] [PubMed]
- Fraser, I.S.; Zeun, S.; Parke, S.; Wilke, B.; Junge, W.; Serrani, M. Improving the objective quality of large-scale clinical trials for women with heavy menstrual bleeding: Experience from 2 multi-center, randomized trials. Reprod. Sci. 2013, 20, 745–754. [Google Scholar] [CrossRef]
- Matteson, K.A. Menstrual questionnaires for clinical and research use. Best. Pract. Res. Clin. Obstet. Gynaecol. 2017, 40, 44–54. [Google Scholar] [CrossRef]
- Liberty, A.; Samuelson Bannow, B.; Matteson, K.; Edelman, A.; Colwill, A. Menstrual Technology Innovations and the Implications for Heavy Menstrual Bleeding. Obstet. Gynecol 2023, 141, 666–673. [Google Scholar] [CrossRef]
- Toxqui, L.; Pérez-Granados, A.M.; Blanco-Rojo, R.; Wright, I.; Vaquero, M.P. A simple and feasible questionnaire to estimate menstrual blood loss: Relationship with hematological and gynecological parameters in young women. BMC Womens Health 2014, 14, 71. [Google Scholar] [CrossRef]
- Perelló, J.; Pujol, P.; Pérez, M.; Artés, M.; Calaf, J. Heavy Menstrual Bleeding-Visual Analog Scale, an Easy-to-Use Tool for Excessive Menstrual Blood Loss That Interferes with Quality-of-Life Screening in Clinical Practice. Womens Health Rep. 2022, 3, 483–490. [Google Scholar] [CrossRef]
- Ruta, D.A.; Garratt, A.M.; Chadha, Y.C.; Flett, G.M.; Hall, M.H.; Russell, I.T. Assessment of patients with menorrhagia: How valid is a structured clinical history as a measure of health status? Qual. Life Res. 1995, 4, 33–40. [Google Scholar] [CrossRef]
- Dutton, B.; Kai, J. Women’s experiences of heavy menstrual bleeding and medical treatment: A qualitative study in primary care. Br. J. Gen. Pract. 2023, 73, e294–e301. [Google Scholar] [CrossRef] [PubMed]
- Lancastle, D.; Kallner, H.K.; Hale, G.; Wood, B.; Ashcroft, L.; Driscoll, H. Development of a brief menstrual quality of life measure for women with heavy menstrual bleeding. BMC Womens Health 2023, 23, 105. [Google Scholar] [CrossRef] [PubMed]
- Taylor, H.S.; Pal, L.; Sell, E. Speroff’s Clinical Gynecologic Endocrinology and Infertility, 9th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2020. [Google Scholar]
- Jameson, J.L.; Kasper, D.L.; Longo, D.L.; Fauci, A.S.; Hauser, S.L.; Loscalzo, J. (Eds.) Harrison’s Principles of Internal Medicine, 20th ed.; Principles of Internal Medicine; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- Mansour, D.; Hofmann, A.; Gemzell-Danielsson, K. A Review of Clinical Guidelines on the Management of Iron Deficiency and Iron-Deficiency Anemia in Women with Heavy Menstrual Bleeding. Adv. Ther. 2021, 38, 201–225. [Google Scholar] [CrossRef] [PubMed]
- Munro, M.G.; Mast, A.E.; Powers, J.M.; Kouides, P.A.; O’brien, S.H.; Richards, T.; Lavin, M.; Levy, B.S. The relationship between heavy menstrual bleeding, iron deficiency, and iron deficiency anemia. Am. J. Obstet. Gynecol. 2023. [CrossRef]
- Cooke, A.G.; McCavit, T.L.; Buchanan, G.R.; Powers, J.M. Iron Deficiency Anemia in Adolescents Who Present with Heavy Menstrual Bleeding. J. Pediatr. Adolesc. Gynecol. 2017, 30, 247–250. [Google Scholar] [CrossRef]
- Kawabata, H.; Tamura, T.; Tamai, S.; Fujibayashi, A.; Sugimura, M. Intravenous ferric derisomaltose versus saccharated ferric oxide for iron deficiency anemia associ-ated with menorrhagia: A randomized, open-label, active-controlled, noninferiority study. Int. J. Hematol. 2022, 116, 647–658. [Google Scholar] [CrossRef]
- Warner, P.E.; Critchley, H.O.; Lumsden, M.A.; Campbell-Brown, M.; Douglas, A.; Murray, G.D. Menorrhagia I: Measured blood loss, clinical features, and outcome in women with heavy periods: A survey with follow-up data. Am. J. Obstet. Gynecol. 2004, 190, 1216–1223. [Google Scholar] [CrossRef]
- Donoso, M.B.; Serra, R.; Rice, G.E.; Gana, M.T.; Rojas, C.; Khoury, M.; Arraztoa, J.A.; Monteiro, L.J.; Acuña, S.; Illanes, S.E. Normality Ranges of Menstrual Fluid Volume During Reproductive Life Using Direct Quantification of Menses with Vaginal Cups. Gynecol. Obstet. Invest. 2019, 84, 390–395. [Google Scholar] [CrossRef]
- Gudmundsdottir, B.R.; Hjaltalin, E.F.; Bragadottir, G.; Hauksson, A.; Geirsson, R.T.; Onundarson, P.T. Quantification of menstrual flow by weighing protective pads in women with normal, decreased or increased menstruation. Acta Obstet. Gynecol. Scand. 2009, 88, 275–279. [Google Scholar] [CrossRef]
- Shaw, S.T.; Aaronson, D.E., Jr.; Moyer, D.L. Quantitation of menstrual blood loss--further evaluation of the alkaline hematin method. Contraception 1972, 5, 497–513. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.S.; Alsina, J.C.; Vannuccini, S.; Koga, K.; Silva-Filho, A.L.; Yang, X.; Estrade, J.-P.; Catherino, W. Clinical perspectives on the menstrual pictogram for the assessment of heavy menstrual bleeding. Hum. Reprod. Open. 2022, 2022, hoac048. [Google Scholar] [CrossRef]
- Zakherah, M.S.; Sayed, G.H.; El-Nashar, S.A.; Shaaban, M.M. Pictorial blood loss assessment chart in the evaluation of heavy menstrual bleeding: Diagnostic accuracy compared to alkaline hematin. Gynecol. Obstet. Invest. 2011, 71, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Quinn, S.D.; Higham, J. Outcome measures for heavy menstrual bleeding. Womens Health 2016, 12, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Beller, F.K. Observations on the clotting of menstrual blood and clot formation. Am. J. Obstet. Gynecol. 1971, 111, 535–546. [Google Scholar] [CrossRef] [PubMed]
| 1. Self-judgement: do you believe that you have an excessive menstrual flow? |
| 2. Lasting days: - Does your menses last for more than 7 days? - Total number of days in a single menstrual period 3. Total pad counts per single menstrual period: - Do you use more than 20 pads during a single menstrual period? - Total pad counts in a single menstrual period 4. Number of sanitary products changed per day: - Do you need to change pads or tampons more frequently than every 3 h? - Number of pads on the day with the heaviest menstrual flow 5. Leakaging of menstrual blood: do you experience frequent episodes of accidental soiling of your clothing or bedsheet? 6. Presence of coagulated menstrual blood: do you pass blood clots that are larger than one inch in diameter? |
| Women with Gynecological Diseases | Number |
|---|---|
| Myoma | 63 |
| Myoma with benign ovarian cyst | 11 |
| Adenomyosis | 9 |
| Adenomyosis with benign ovarian cyst | 6 |
| Myoma with Adenomyosis | 14 |
| EM pathology (EM polyp, EM hyperplasia, etc.) | 15 |
| Benign ovarian cyst | 47 |
| CIN~CIS | 37 |
| TOA | 2 |
| Others | 7 |
| Women without known gynecological diseases | 90 |
| Total | 301 |
| No. (%) Or Mean ± SD | Odds Ratio (95% CI) | p-Value | |
|---|---|---|---|
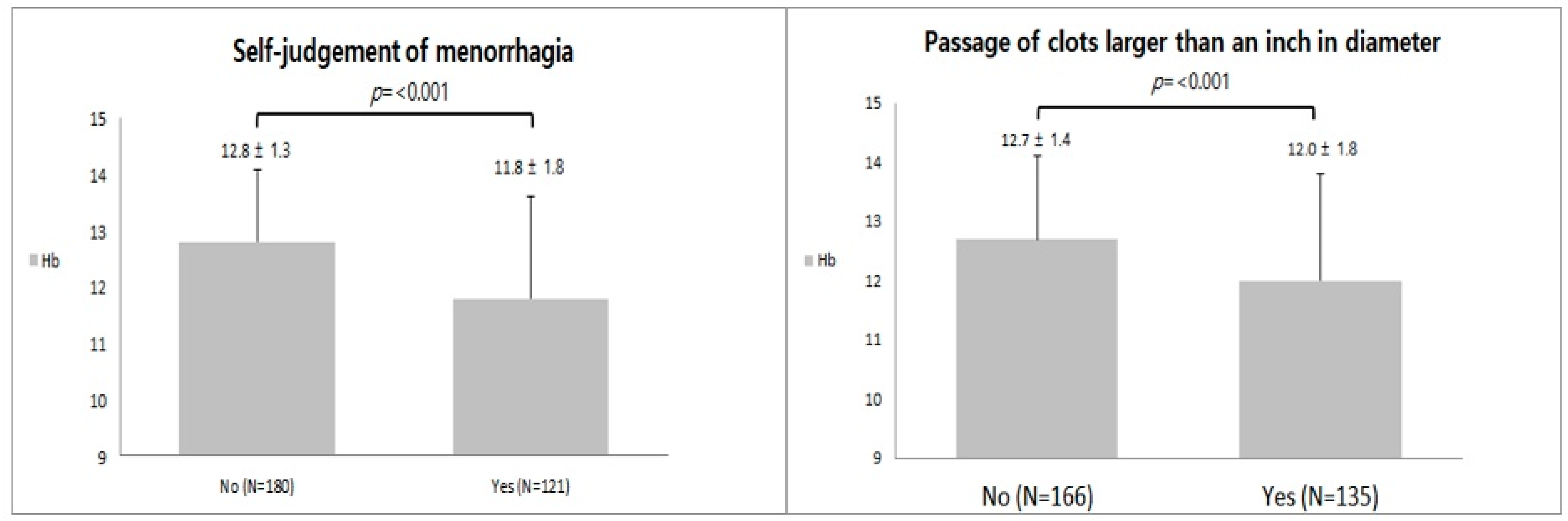
| -Self-judgement of menorrhagia | 121 (40.2%) | 3.818 (2.133–6.835) | <0.001 * |
| -Total number of days in a single menstrual period (days, mean ± SD) | 6.0 ± 3.4 | 1.069 (0.994–1.150) | 0.074 |
| -Menses lasting longer than 7 days | 26 (8.6%) | 3.072 (1.334–7.071) | 0.008 * |
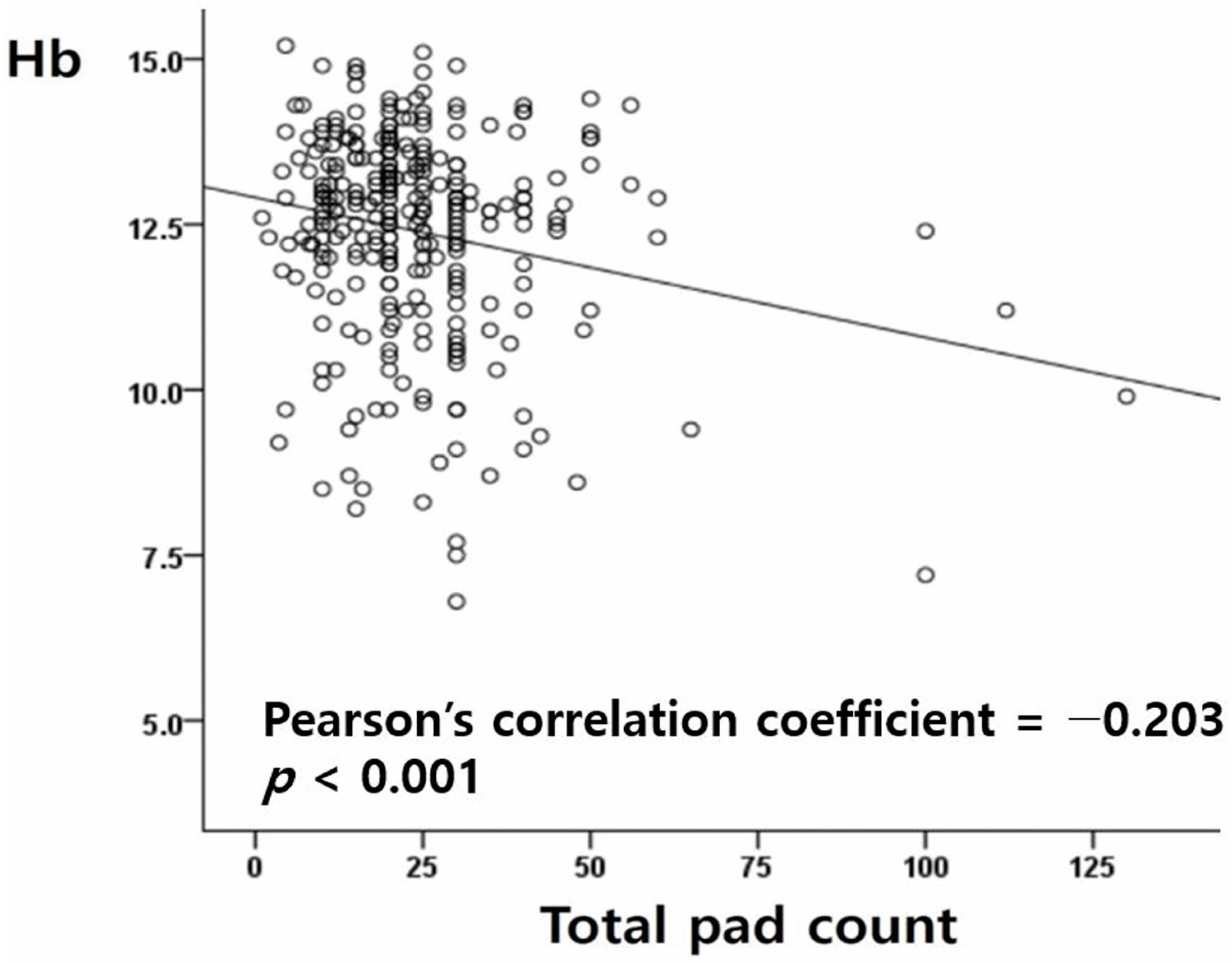
| -Total pad counts in a single menstrual period (counts, mean ± SD) | 24.1 ± 15.3 | 1.033 (1.014–1.052) | 0.001 * |
| -Use of 20 or more pads per menstrual cycle | 198 (63.8%) | 1.740 (0.932–3.249) | 0.082 |
| -Number of pads on the day with the heaviest menstrual flow (counts, mean ± SD) | 6.2 ± 3.6 (296/301) | 1.086 (1.011–1.167) | 0.023 * |
| -Changing of pads more often than every 3 h | 63 (21.1%) (298/301) | 2.616 (1.408–4.861) | 0.002 * |
| -Accidental leakage of menses on bed sheets | 164 (54.5%) | 2.349 (1.297–4.252) | 0.005 * |
| -Passage of clots larger than one inch in diameter | 135 (44.9%) | 3.205 (1.778–5.745) | <0.001 * |
| Odds Ratio | 95% CI | p-Value | |
|---|---|---|---|
| Self-judgement of menorrhagia | 2.217 | 1.057–4.647 | 0.035 |
| Menses lasting longer than 7 days | 1.638 | 0.625–4.288 | 0.315 |
| Total pad counts in a single menstrual period | 1.011 | 0.989–1.034 | 0.316 |
| Changing of pads more often than every 3 h | 1.262 | 0.588–2.706 | 0.550 |
| Leakaging of menstrual blood | 1.011 | 0.484–2.113 | 0.976 |
| Presence of coagulated menstrual blood | 1.886 | 0.977–3.642 | 0.059 |
| Odds Ratio | 95% CI | p-Value | |
|---|---|---|---|
| Menses lasting longer than 7 days | 1.867 | 0.721–4.837 | 0.199 |
| Total pad counts in a single menstrual period | 1.014 | 0.992–1.036 | 0.226 |
| Changing of pads more often than every 3 h | 1.422 | 0.669–3.022 | 0.359 |
| Leakaging of menstrual blood | 1.413 | 0.737–2.712 | 0.298 |
| Presence of coagulated menstrual blood | 2.113 | 1.111–4.019 | 0.023 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.J.; Ahn, J.E.; Ryu, J.M.; Jeong, Y.Y.; Choi, Y.S. Association between Patients’ Self-Judgement, Coagulated Menstrual Blood, and Menorrhagia: Results from a Questionnaire Survey and Blood Test Analysis. Medicina 2023, 59, 874. https://doi.org/10.3390/medicina59050874
Lee EJ, Ahn JE, Ryu JM, Jeong YY, Choi YS. Association between Patients’ Self-Judgement, Coagulated Menstrual Blood, and Menorrhagia: Results from a Questionnaire Survey and Blood Test Analysis. Medicina. 2023; 59(5):874. https://doi.org/10.3390/medicina59050874
Chicago/Turabian StyleLee, Eun Ji, Ji Eun Ahn, Jung Min Ryu, Yoon Young Jeong, and Youn Seok Choi. 2023. "Association between Patients’ Self-Judgement, Coagulated Menstrual Blood, and Menorrhagia: Results from a Questionnaire Survey and Blood Test Analysis" Medicina 59, no. 5: 874. https://doi.org/10.3390/medicina59050874
APA StyleLee, E. J., Ahn, J. E., Ryu, J. M., Jeong, Y. Y., & Choi, Y. S. (2023). Association between Patients’ Self-Judgement, Coagulated Menstrual Blood, and Menorrhagia: Results from a Questionnaire Survey and Blood Test Analysis. Medicina, 59(5), 874. https://doi.org/10.3390/medicina59050874







