Assessment of Prescribing Practices and Factors Related to Antibiotic Prescribing in Community Pharmacies
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population and Sample Size
2.3. Data Collection and Analysis
2.4. Ethical Approval
3. Results
3.1. Characteristics of Patients, Pharmacists, and Prescriptions
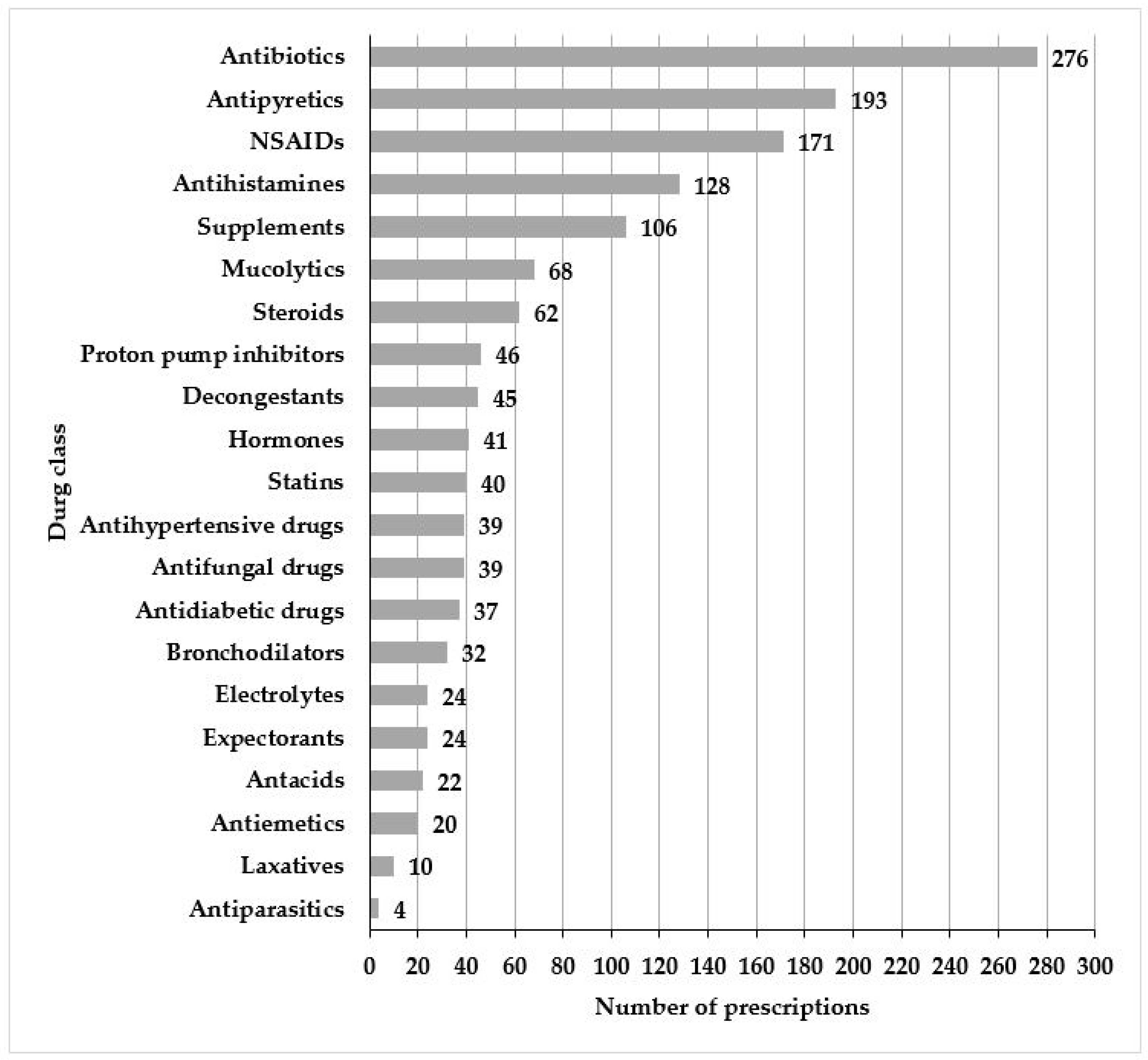
3.2. Prescribing Practices
3.3. WHO Prescribing Indicators
3.4. Antibiotic Prescribing
3.5. Factors Related with Antibiotic Prescribing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Pharmaceutical Federation (FIP). Community Pharmacy Global Report. 2021. Available online: https://www.fip.org/file/5015 (accessed on 1 February 2023).
- World Health Organization. The Legal and Regulatory Framework for Community Pharmacies in the WHO European Region. Available online: https://apps.who.int/iris/bitstream/handle/10665/326394/9789289054249-eng.pdf?sequence=1&isAllowed=y (accessed on 3 February 2023).
- van de Pol, J.M.; van Dijk, L.; Koster, E.S.; de Jong, J.; Bouvy, M.L. How Does the General Public Balance Convenience and Cognitive Pharmaceutical Services in Community Pharmacy Practice. Res. Soc. Adm. Pharm. 2021, 17, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Goode, J.-V.; Owen, J.; Page, A.; Gatewood, S. Community-Based Pharmacy Practice Innovation and the Role of the Community-Based Pharmacist Practitioner in the United States. Pharmacy 2019, 7, 106. [Google Scholar] [CrossRef] [PubMed]
- Pantasri, T. Expanded Roles of Community Pharmacists in COVID-19: A Scoping Literature Review. J. Am. Pharm. Assoc. 2022, 62, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Alden, J.; Crane, K.; Robinson, R.; Rothholz, M.; Watkins, T.; Wu, J.; Wurtz, R. Expansion of Community Pharmacies’ Role in Public Vaccine Delivery to Children: Opportunities and Need. J. Am. Pharm. Assoc. 2022, 62, 1514–1517. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Promoting Rational Use of Medicines: Core Components-WHO Policy Perspectives on Medicine. Available online: http://archives.who.int/tbs/rational/h3011e.pdf (accessed on 1 February 2023).
- World Health Organization. The Rational Use of Drugs: Report of the Conference of Experts, Nairobi, 25–29 November 1985. Available online: https://apps.who.int/iris/handle/10665/37174 (accessed on 3 February 2023).
- Siele, S.M.; Abdu, N.; Ghebrehiwet, M.; Hamed, M.R.; Tesfamariam, E.H. Drug Prescribing and Dispensing Practices in Regional and National Referral Hospitals of Eritrea: Evaluation with WHO/INRUD Core Drug Use Indicators. PLoS ONE 2022, 17, e0272936. [Google Scholar] [CrossRef]
- Ofori-Asenso, R.; Agyeman, A. Irrational Use of Medicines—A Summary of Key Concepts. Pharmacy 2016, 4, 35. [Google Scholar] [CrossRef]
- Krockow, E.M.; Harvey, E.J.; Ashiru-Oredope, D. Addressing Long-Term and Repeat Antibiotic Prescriptions in Primary Care: Considerations for a Behavioural Approach. BMJ Qual. Saf. 2022, 31, 782–786. [Google Scholar] [CrossRef]
- Wu, J.H.C.; Khalid, F.; Langford, B.J.; Beahm, N.P.; McIntyre, M.; Schwartz, K.L.; Garber, G.; Leung, V. Community Pharmacist Prescribing of Antimicrobials: A Systematic Review from an Antimicrobial Stewardship Perspective. Can. Pharm. J. 2021, 154, 179–192. [Google Scholar] [CrossRef]
- Chua, K.-P.; Fischer, M.A.; Linder, J.A. Appropriateness of Outpatient Antibiotic Prescribing among Privately Insured US Patients: ICD-10-CM Based Cross Sectional Study. BMJ 2019, 364, k5092. [Google Scholar] [CrossRef]
- World Health Organization. How to Investigate Drug Use in Health Facilities. Available online: https://apps.who.int/iris/bitstream/handle/10665/60519/WHO_DAP_93.1.pdf (accessed on 3 February 2023).
- Bassoum, O.; Sougou, N.M.; Lèye, M.M.; Dia, O.; Faye, A. Assessment of Prescribing Indicators in the Public and Private Sectors: A Cross-Sectional Study in Twenty Community Pharmacies in an Urban Setting. J. Clin. Med. Ther. 2018, 3, 16. [Google Scholar]
- Jacob, S.; Malviya, R.; Sandhan, S.; Deshpande, P. Evaluation of Prescribing Pattern Based on World Health Organization Indicators in Maharashtra during COVID-19 Pandemic. Indian J. Community Fam. Med. 2022, 8, 121–128. [Google Scholar] [CrossRef]
- Amaha, N.D.; Weldemariam, D.G.; Abdu, N.; Tesfamariam, E.H. Prescribing Practices Using WHO Prescribing Indicators and Factors Associated with Antibiotic Prescribing in Six Community Pharmacies in Asmara, Eritrea: A Cross-Sectional Study. Antimicrob. Resist. Infect. Control 2019, 8, 163. [Google Scholar] [CrossRef] [PubMed]
- Aravamuthan, A.; Arputhavanan, M.; Subramaniam, K.; Udaya Chander, J.S.J. Assessment of Current Prescribing Practices Using World Health Organization Core Drug Use and Complementary Indicators in Selected Rural Community Pharmacies in Southern India. J. Pharm. Policy Pract. 2016, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Chapagain, K.; Pokharel, R.; Paranjape, B.D. Evaluation of Prescription Pattern and Rational Prescribing in Eastern Nepal. J. Nobel Med. Coll. 2016, 5, 32–36. [Google Scholar] [CrossRef]
- Atif, M.; Azeem, M.; Sarwar, M.R.; Shahid, S.; Javaid, S.; Ikram, H.; Baig, U.; Scahill, S. WHO/INRUD Prescribing Indicators and Prescribing Trends of Antibiotics in the Accident and Emergency Department of Bahawal Victoria Hospital, Pakistan. SpringerPlus 2016, 5, 1928. [Google Scholar] [CrossRef]
- Vooss, A.T.; Diefenthaeler Silveira, H. Evaluation of Prescription Indicators Established by the WHO in Getúlio Vargas—RS. Braz. J. Pharm. Sci. 2011, 47, 385–390. [Google Scholar] [CrossRef]
- El Mahalli, A.A. WHO/INRUD Drug Prescribing Indicators at Primary Health Care Centres in Eastern Province, Saudi Arabia. East. Mediterr. Health J. 2012, 18, 1091–1096. [Google Scholar] [CrossRef]
- Aryal, A.; Dahal, A.; Shrestha, R. Study on Drug Use Pattern in Primary Healthcare Centers of Kathmandu Valley. SAGE Open Med. 2020, 8, 2050312120926437. [Google Scholar] [CrossRef]
- Yilma, Z.; Liben, M. Assessment of Drug Prescription Pattern in Mekelle General Hospital, Mekelle, Ethiopia, Using World Health Organization Prescribing Indicators. Biomed Res. Int. 2020, 2020, 3809157. [Google Scholar] [CrossRef]
- Mahmood, A.; Elnour, A.A.; Ali, A.A.A.; Hassan, N.A.G.M.; Shehab, A.; Bhagavathula, A.S. Evaluation of Rational Use of Medicines (RUM) in Four Government Hospitals in UAE. Saudi Pharm. J. 2016, 24, 189–196. [Google Scholar] [CrossRef]
- El-Dahiyat, F.; Salah, D.; Alomari, M.; Elrefae, A.; Jairoun, A.A. Antibiotic Prescribing Patterns for Outpatient Pediatrics at a Private Hospital in Abu Dhabi: A Clinical Audit Study. Antibiotics 2022, 11, 1676. [Google Scholar] [CrossRef]
- Ras Al Khaimah—The Official Portal of the UAE Government. Available online: https://u.ae/en/about-the-uae/the-seven-emirates/ras-al-khaimah (accessed on 28 February 2023).
- World Health Organization. AWaRe Classification. 2021. Available online: https://www.who.int/publications/i/item/2021-aware-classification (accessed on 3 February 2023).
- George, C.; Jacob, D.; Thomas, P.; Ravinandan, A.P.; Srinivasan, R.; Thomas, J. Study of Drug Related Problems in Ambulatory Hemodialysis Patients. J. Pharm. Biol. Sci. 2017, 12, 32–36. [Google Scholar] [CrossRef]
- Walker, L.E.; Mangoni, A.A. Avoiding Harm from Overprescribing: What Are the Challenges and How Do We Overcome Them? Br. J. Clin. Pharmacol. 2021, 87, 6–8. [Google Scholar] [CrossRef]
- Otoom, S.; Culligan, K.; Al-Assoomi, B.; Al-Ansari, T. Analysis of Drug Prescriptions in Primary Health Care Centres in Bahrain. East. Mediterr. Health J. 2010, 16, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Ofori-Asenso, R.; Brhlikova, P.; Pollock, A.M. Prescribing Indicators at Primary Health Care Centers within the WHO African Region: A Systematic Analysis (1995–2015). BMC Public Health 2016, 16, 724. [Google Scholar] [CrossRef] [PubMed]
- Atif, M.; Azeem, M.; Rehan Sarwar, M.; Malik, I.; Ahmad, W.; Hassan, F.; Rehman, A.; Rana, M. Evaluation of Prescription Errors and Prescribing Indicators in the Private Practices in Bahawalpur, Pakistan. J. Chin. Med. Assoc. 2018, 81, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Rabie, D.; Kheder, S.I. Assessment of Prescribing and Dispensing Practices Based on WHO Core Prescribing Indicators in Hospital and Community Pharmacies in Khartoum State—Sudan. J. Med. Inform. Decis. Mak. 2020, 1, 3493. [Google Scholar] [CrossRef]
- Llor, C.; Bjerrum, L. Antimicrobial Resistance: Risk Associated with Antibiotic Overuse and Initiatives to Reduce the Problem. Ther. Adv. Drug Saf. 2014, 5, 229–241. [Google Scholar] [CrossRef]
- World Health Organization. AWaRe Classification Antibiotics. 2019. Available online: https://www.who.int/news/item/01-10-2019-who-releases-the-2019-aware-classification-antibiotics (accessed on 3 February 2023).
- Amponsah, O.K.O.; Buabeng, K.O.; Owusu-Ofori, A.; Ayisi-Boateng, N.K.; Hämeen-Anttila, K.; Enlund, H. Point Prevalence Survey of Antibiotic Consumption across Three Hospitals in Ghana. JAC-Antimicrob. Resist. 2021, 3, 8. [Google Scholar] [CrossRef]
- Chem, E.D.; Anong, D.N.; Akoachere, J.-F.K.T. Prescribing Patterns and Associated Factors of Antibiotic Prescription in Primary Health Care Facilities of Kumbo East and Kumbo West Health Districts, North West Cameroon. PLoS ONE 2018, 13, e0193353. [Google Scholar] [CrossRef]
- Hashmi, H.; Sasoli, N.A.; Sadiq, A.; Raziq, A.; Batool, F.; Raza, S.; Iqbal, Q.; Haider, S.; Umer Jan, S.; Mengal, M.A.; et al. Prescribing Patterns for Upper Respiratory Tract Infections: A Prescription-Review of Primary Care Practice in Quetta, Pakistan and the Implications. Front. Public Health 2021, 9, 787933. [Google Scholar] [CrossRef] [PubMed]
- Saliba-Gustafsson, E.A.; Dunberger Hampton, A.; Zarb, P.; Orsini, N.; Borg, M.A.; Stålsby Lundborg, C. Factors Associated with Antibiotic Prescribing in Patients with Acute Respiratory Tract Complaints in Malta: A 1-Year Repeated Cross-Sectional Surveillance Study. BMJ Open 2019, 9, e032704. [Google Scholar] [CrossRef] [PubMed]
- Sié, A.; Ouattara, M.; Bountogo, M.; Dah, C.; Compaoré, G.; Boudo, V.; Lebas, E.; Brogdon, J.; Nyatigo, F.; Arnold, B.F.; et al. Indication for Antibiotic Prescription Among Children Attending Primary Healthcare Services in Rural Burkina Faso. Clin. Infect. Dis. 2021, 73, 1288–1291. [Google Scholar] [CrossRef] [PubMed]
- Messina, F.; Clavenna, A.; Cartabia, M.; Piovani, D.; Bortolotti, A.; Fortino, I.; Merlino, L.; Bonati, M. Antibiotic Prescription in the Outpatient Paediatric Population Attending Emergency Departments in Lombardy, Italy: A Retrospective Database Review. BMJ Paediatr. Open 2019, 3, e000546. [Google Scholar] [CrossRef]
- Butler, A.M.; Brown, D.S.; Durkin, M.J.; Sahrmann, J.M.; Nickel, K.B.; O’Neil, C.A.; Olsen, M.A.; Hyun, D.Y.; Zetts, R.M.; Newland, J.G. Association of Inappropriate Outpatient Pediatric Antibiotic Prescriptions with Adverse Drug Events and Health Care Expenditures. JAMA Netw. Open 2022, 5, e2214153. [Google Scholar] [CrossRef]
- World Bank. Population Ages 15–64 (% of Total Population)—United Arab Emirates. Available online: https://data.worldbank.org/indicator/SP.POP.1564.TO.ZS?end=2021&locations=AE&start=1960&view=chart (accessed on 28 February 2023).
- World Health Organization. Primary Care. Available online: https://www.who.int/teams/integrated-health-services/clinical-services-and-systems/primary-care (accessed on 5 April 2023).
- Rutschmann, O.T.; Domino, M.E. Antibiotics for Upper Respiratory Tract Infections in Ambulatory Practice in the United States, 1997–1999: Does Physician Specialty Matter? J. Am. Board Fam. Med. 2004, 17, 196–200. [Google Scholar] [CrossRef]
- Poss-Doering, R.; Kronsteiner, D.; Kamradt, M.; Andres, E.; Kaufmann-Kolle, P.; Wensing, M.; Szecsenyi, J.; Wensing, M.; Kamradt, M.; Poß-Doering, R.; et al. Antibiotic Prescribing for Acute, Non-Complicated Infections in Primary Care in Germany: Baseline Assessment in the Cluster Randomized Trial ARena. BMC Infect. Dis. 2021, 21, 877. [Google Scholar] [CrossRef]
| Variable | N (%)/Median (IQR) | 95% CI |
|---|---|---|
| Patient characteristics (N = 630) | ||
| Age (years) | 29 (14–42) | 27–32 |
| Infants: <1 | 13 (2.1) | 1.1–3.3 |
| Children: 1–12 | 135 (21.4) | 18.1–24.8 |
| Adolescents: 13–17 | 33 (5.2) | 3.3–7.0 |
| Adults: 18–64 | 425 (67.5) | 63.8–71.4 |
| Old adults: ≥65 | 24 (3.8) | 2.5–5.4 |
| Gender | ||
| Male | 288 (45.7) | 41.9–49.5 |
| Female | 342 (54.3) | 50.5–58.1 |
| Prescription characteristics (N = 630) | ||
| Prescriber specialty | ||
| General practitioner | 365 (57.9) | 54.1–62.1 |
| Gynecologist | 49 (7.8) | 5.7–10.0 |
| Pediatrician | 35 (5.6) | 3.7–7.3 |
| Cardiologist | 22 (3.5) | 2.2–4.9 |
| Ophthalmologist | 14 (2.2) | 1.1–3.5 |
| Endocrinologist | 3 (0.5) | 0.0–1.1 |
| General surgeon | 10 (1.6) | 0.6–2.5 |
| Dentist | 27 (4.3) | 2.7–6.0 |
| Dermatologist | 25 (4.0) | 2.4–5.4 |
| ENT specialist | 50 (7.9) | 5.9–10.2 |
| Internal medicine specialist | 30 (4.8) | 3.2–6.5 |
| Pharmacist characteristics (N = 21) | ||
| Age (years) | 32 (30–34) | 31.5–36.0 |
| Gender | ||
| Male | 15 (71.4) | 52.4–90.5 |
| Female | 6.0 (28.6) | 9.5–47.6 |
| Education | ||
| BPharm | 13.0 (61.9) | 42.9–81.0 |
| PharmD | 5.0 (23.8) | 4.8–42.9 |
| Master’ degree | 3.0 (14.3) | 0.0–28.6 |
| Work Experience | 5.0 (4.0–7.0) | 4.0–7.0 |
| Position in pharmacy | ||
| Pharmacist In charge | 6.0 (28.6) | 14.3–47.6 |
| Pharmacist | 12.0 (57.1) | 33.3–76.2 |
| Assistant Pharmacist | 3.0 (14.3) | 0.0–28.6 |
| Type of pharmacy | ||
| Independent | 15.0 (71.4) | 52.4–90.5 |
| Chain | 6.0 (28.6) | 9.5–47.6 |
| Number of prescriptions per day | ||
| <100 | 19 (90.5) | 76.2–100 |
| 100–150 | 2.0 (9.5) | 0.0–23.8 |
| Prescribing Indicators | N (%) | 95% CI |
|---|---|---|
| Number of drugs per prescription | ||
| One | 137 (21.7) | 18.4–25.1 |
| Two | 174 (27.6) | 24.0–31.3 |
| Three | 146 (23.2) | 20.0–26.3 |
| Four | 68 (10.8) | 8.6–13.3 |
| Five or more | 105 (16.7) | 13.8–19.5 |
| Number of drugs prescribed by generic name | ||
| None | 261 (41.4) | 37.6–45.4 |
| One | 130 (20.6) | 17.3–23.8 |
| Two | 83 (13.2) | 10.8–15.7 |
| Three | 61 (9.7) | 10.8–15.7 |
| Four | 30 (4.8) | 3.0–6.5 |
| Five or more | 65 (10.3) | 8.3–12.9 |
| Number of drug encounter with antibiotics | ||
| None | 354 (56.2) | 52.4–60.0 |
| One | 236 (37.5) | 33.7–41.4 |
| Two | 39 (6.2) | 4.1–8.3 |
| Three | 1 (0.2) | 0.0–0.5 |
| Number of drug encounter with injection | ||
| None | 627 (99.5) | 98.9–100 |
| One | 3 (0.5) | 0.0–1.1 |
| Number of drugs prescribed from essential drug list | 529 (84) | 80.8–86.7 |
| Prescribing Indicators | Optimal Value | Current Study | Bassoum et al. [2] | Jacob et al. [3] | Amaha et al. [4] | Aravamuthan et al. [5] | Chapagain et al. [6] | Atif et al. [7] | Vooss et al. [8] | Mahalli et al. [9] |
|---|---|---|---|---|---|---|---|---|---|---|
| Average number of drugs per prescription | 1.6–1.8 | 2.88 | 2.5 | 2.89 | 1.76 | 3.7 | 2.14 | 4.5 | 2.03 | 2.4 |
| Percentage of drugs prescribed by generic name | 100% | 58.6 | 7.0 | 0.75 | 83.14 | 8.0 | 45.18 | 23.3 | 72.8 | 61.2 |
| Percentage of prescriptions with an antibiotic prescribed | 20.0–26.8% | 43.8 | 40 | 37.8 | 53 | 58.8 | 40.44 | 39.6 | 21.7 | 32.2 |
| Percentage of encounters with an injection prescribed | 13.4–24.1% | 0.5 | 7 | 2.74 | 7.8 | 24.3 | 3.44 | 19 | 2.4 | 2 |
| Percentage of drugs prescribed from the list of essential drugs | 100% | 83.8 | 32 | 30.08 | 93.39 | 100 | 76.11 | 54.4 | 80.3 | 99.2 |
| AWaRe Classification | ||
|---|---|---|
| Access (%) | Watch (%) | Reserve (%) |
| Amoxicillin/clavulanic-acid (22.4) | Azithromycin (4.4) | - |
| Amoxicillin (3.3) | Cefixime (4.1) | |
| Sulfadiazine (0.2) | Cefuroxime (3.2) | |
| Ciprofloxacin (2.2) | ||
| Fusidic acid (1.4) | ||
| Moxifloxacin (0.8) | ||
| Levofloxacin (0.5) | ||
| Ofloxacin (0.2) | ||
| Ceftriaxone (0.2) | ||
| Variable | Antibiotic Prescribing | Logistic Regression | ||||
|---|---|---|---|---|---|---|
| No | Yes | COR (95%CI) | p-Value * | AOR (95% CI) | p-Value * | |
| Patient age | ||||||
| Infants: <1 | 10 (1.6%) | 3 (0.5%) | 1.5 (0.28–8.03) | 0.630 | 1.01 (0.18–5.60) | 0.987 |
| Children: 1–12 | 52 (8.3%) | 83 (13.2%) | 7.9 (2.5–24.65) | <0.001 | 7.40 (2.32–23.62) | 0.001 |
| Adolescents: 13–17 | 16 (2.5%) | 17 (2.7%) | 5.3 (1.4–18.95) | 0.010 | 5.86 (1.57–21.86) | 0.008 |
| Adults: 18–64 | 256 (40.6%) | 169 (26.8%) | 3.3 (1.1–9.82) | 0.032 | 2.77 (0.90–8.54) | 0.075 |
| Old adults: ≥65 | 20 (3.2%) | 4 (0.6%) | Ref. | Ref. | ||
| Patient gender | ||||||
| Male | 154 (24.4%) | 134 (21.3%) | Ref. | Ref. | ||
| Female | 200 (31.7%) | 142 (22.5%) | 0.82 (0.59–1.12) | 0.207 | 0.95 (0.68–1.34) | 0.786 |
| Prescriber qualification | ||||||
| General practitioner | 185 (29.4%) | 180 (28.6%) | 1.71 (1.23–2.36) | 0.001 | 1.84 (1.30–2.60) | 0.001 |
| Specialist | 169 (26.8%) | 96 (15.2%) | Ref. | Ref. | ||
| Number of drugs per prescription | ||||||
| One | 101 (16%) | 36 (5.7%) | Ref. | Ref. | ||
| Two | 94 (14.9%) | 80 (12.7%) | 2.38 (1.47–3.87) | <0.001 | 2.82 (1.69–4.69) | <0.001 |
| Three | 71 (11.3%) | 75 (11.9%) | 2.96 (1.79–4.88) | <0.001 | 3.21 (1.9–5.43) | <0.001 |
| Four | 35 (5.6%) | 33 (5.2%) | 2.64 (1.43–4.86) | 0.002 | 3.019 (1.59–5.73) | 0.001 |
| Five or more | 53 (8.4%) | 52 (8.3%) | 2.75 (1.6–4.72) | <0.001 | 3.51 (1.98–6.21) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabbani, S.A.; Sridhar, S.B.; Safdar, M.; Rao, P.G.M.; Jaber, A.A.S.; AlAhmad, M.M.; Shaar, K.; Emad, I.; Azim, M.A. Assessment of Prescribing Practices and Factors Related to Antibiotic Prescribing in Community Pharmacies. Medicina 2023, 59, 843. https://doi.org/10.3390/medicina59050843
Rabbani SA, Sridhar SB, Safdar M, Rao PGM, Jaber AAS, AlAhmad MM, Shaar K, Emad I, Azim MA. Assessment of Prescribing Practices and Factors Related to Antibiotic Prescribing in Community Pharmacies. Medicina. 2023; 59(5):843. https://doi.org/10.3390/medicina59050843
Chicago/Turabian StyleRabbani, Syed Arman, Sathvik B. Sridhar, Maryam Safdar, Padma G. M. Rao, Ammar Ali Saleh Jaber, Mohammad M. AlAhmad, Khaled Shaar, Israa Emad, and Muhammad Abdul Azim. 2023. "Assessment of Prescribing Practices and Factors Related to Antibiotic Prescribing in Community Pharmacies" Medicina 59, no. 5: 843. https://doi.org/10.3390/medicina59050843
APA StyleRabbani, S. A., Sridhar, S. B., Safdar, M., Rao, P. G. M., Jaber, A. A. S., AlAhmad, M. M., Shaar, K., Emad, I., & Azim, M. A. (2023). Assessment of Prescribing Practices and Factors Related to Antibiotic Prescribing in Community Pharmacies. Medicina, 59(5), 843. https://doi.org/10.3390/medicina59050843






