The Role of Hyperbaric Oxygen Therapy in the Treatment of Surgical Site Infections: A Narrative Review
Abstract
1. Introduction
2. HBOT Procedure
3. Clinical Application of HBOT
4. Methods
5. Results and Discussion
5.1. Application of HBOT in Surgical Site Infections
5.1.1. Application of HBOT in Sternal Wound Infection Infections
5.1.2. Application of HBOT in SSIs following Neuromodulation or Neuro-Muscular Surgery
5.1.3. Application of HBOT in SSIs following the Urogenital Surgery
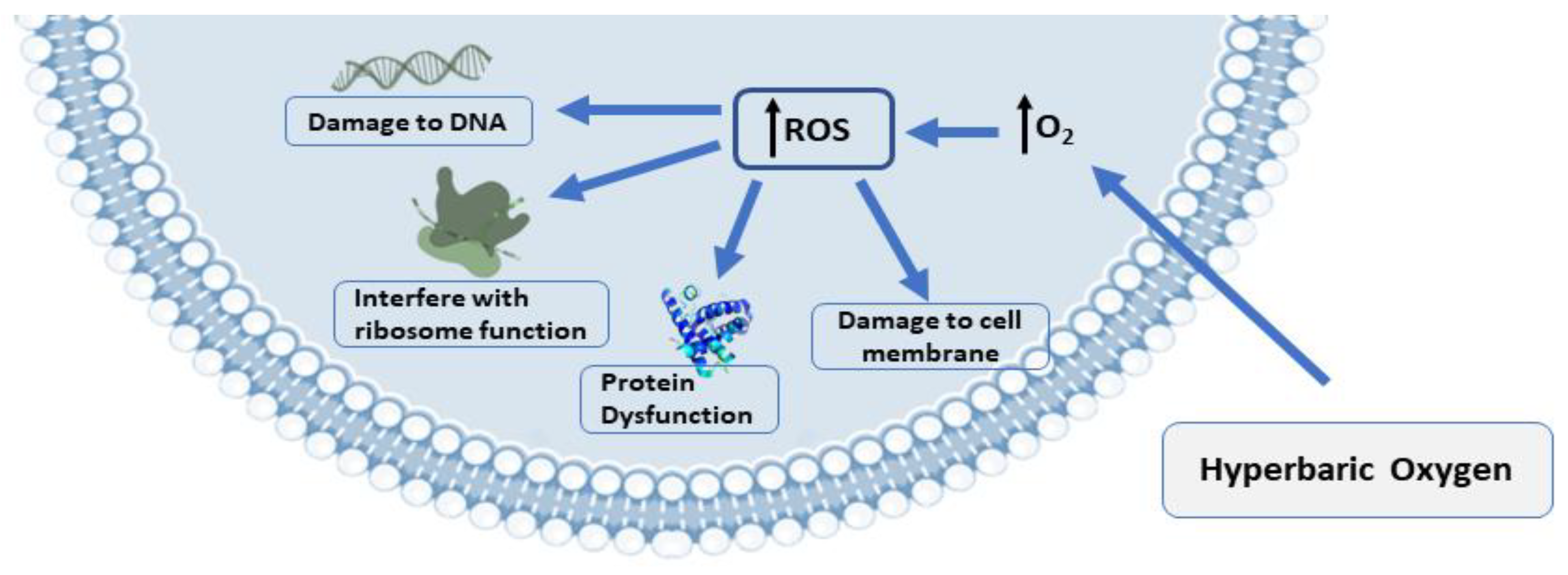
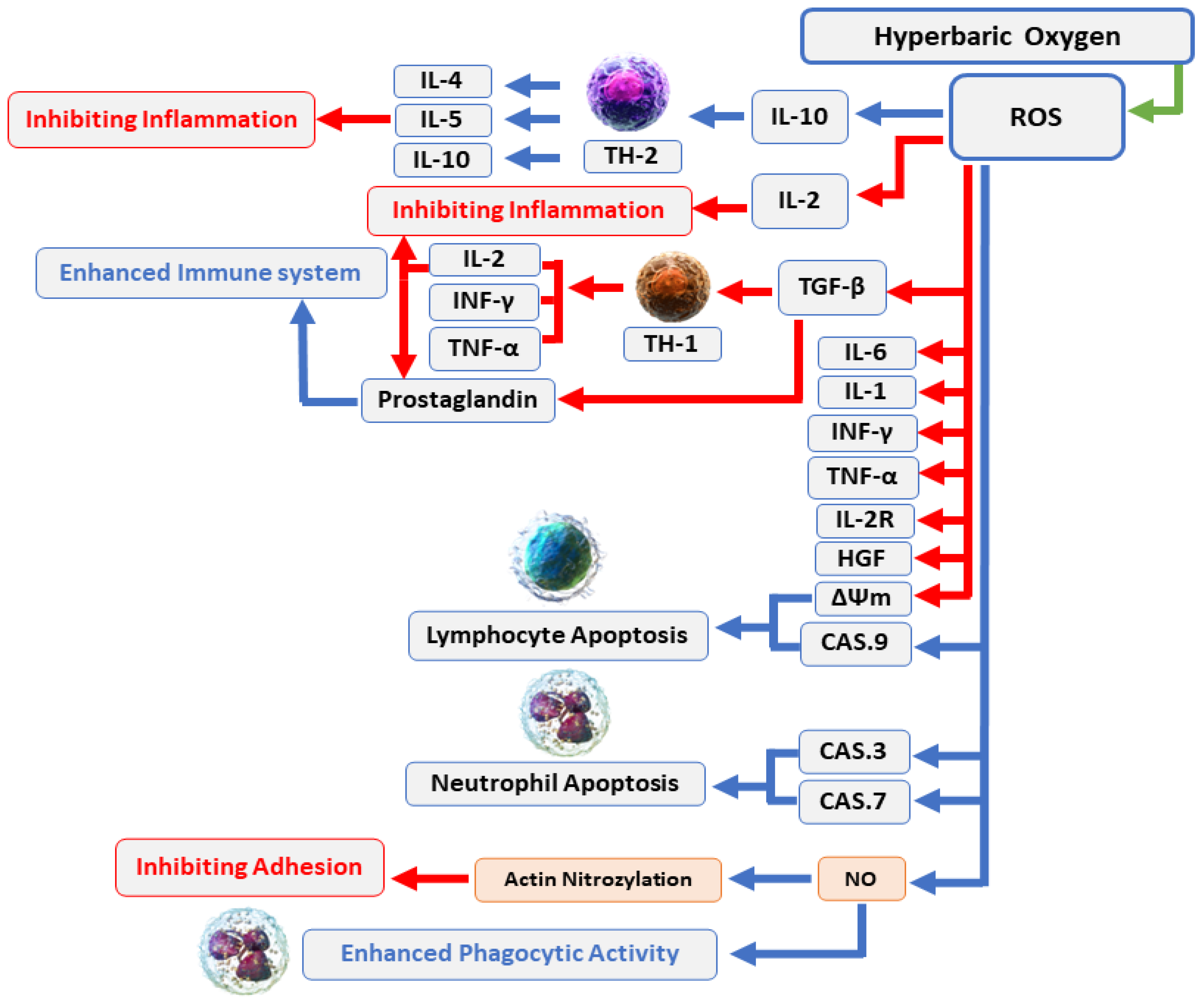
5.2. The Mechanisms of Action of Hyperbaric Oxygen Therapy (HBOT)
5.3. The Complications and Side Effects of HBOT
6. Limitations
7. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leaper, D.J.; Van Goor, H.; Reilly, J.; Petrosillo, N.; Geiss, H.K.; Torres, A.J.; Berger, A. Surgical site infection—A European perspective of incidence and economic burden. Int. Wound J. 2004, 1, 247–273. [Google Scholar] [CrossRef] [PubMed]
- Leaper, D. Surgical-site infection. J. Br. Surg. 2010, 97, 1601–1602. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Guidelines for the Prevention of Surgical Site Infection; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization. Report on the Burden of Endemic Health Care-Associated Infection Worldwide; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Allegranzi, B.; Bischoff, P.; de Jonge, S.; Kubilay, N.Z.; Zayed, B.; Gomes, S.M.; Abbas, M.; Atema, J.J.; Gans, S.; van Rijen, M. New WHO recommendations on preoperative measures for surgical site infection prevention: An evidence-based global perspective. Lancet Infect. Dis. 2016, 16, e276–e287. [Google Scholar] [CrossRef]
- Ban, K.A.; Minei, J.P.; Laronga, C.; Harbrecht, B.G.; Jensen, E.H.; Fry, D.E.; Itani, K.M.; Dellinger, P.E.; Ko, C.Y.; Duane, T.M. American College of Surgeons and Surgical Infection Society: Surgical site infection guidelines, 2016 update. J. Am. Coll. Surg. 2017, 224, 59–74. [Google Scholar] [CrossRef]
- Cheadle, W.G. Risk factors for surgical site infection. Surg. Infect. 2006, 7, s7–s11. [Google Scholar] [CrossRef] [PubMed]
- Florschutz, A.V.; Fagan, R.P.; Matar, W.Y.; Sawyer, R.G.; Berrios-Torres, S.I. Surgical site infection risk factors and risk stratification. J. Am. Acad. Orthop. Surg. 2015, 23, S8. [Google Scholar] [CrossRef]
- Malone, D.L.; Genuit, T.; Tracy, J.K.; Gannon, C.; Napolitano, L.M. Surgical site infections: Reanalysis of risk factors. J. Surg. Res. 2002, 103, 89–95. [Google Scholar] [CrossRef]
- Allegranzi, B.; Zayed, B.; Bischoff, P.; Kubilay, N.Z.; de Jonge, S.; de Vries, F.; Gomes, S.M.; Gans, S.; Wallert, E.D.; Wu, X. Surgical site infections 2. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: An evidence-based global perspective. Lancet Infect. Dis. 2016, 16, e288–e303. [Google Scholar] [CrossRef]
- Chauveaux, D. Preventing surgical-site infections: Measures other than antibiotics. Orthop. Traumatol. Surg. Res. 2015, 101, S77–S83. [Google Scholar] [CrossRef]
- Marano, L.; Carbone, L.; Poto, G.E.; Calomino, N.; Neri, A.; Piagnerelli, R.; Fontani, A.; Verre, L.; Savelli, V.; Roviello, F. Antimicrobial prophylaxis reduces the rate of surgical site infection in upper gastrointestinal surgery: A systematic review. Antibiotics 2022, 11, 230. [Google Scholar] [CrossRef]
- Najjar, P.A.; Smink, D.S. Prophylactic antibiotics and prevention of surgical site infections. Surg. Clin. 2015, 95, 269–283. [Google Scholar] [CrossRef]
- Arias, C.A.; Murray, B.E. Antibiotic-resistant bugs in the 21st century—A clinical super-challenge. N. Engl. J. Med. 2009, 360, 439–443. [Google Scholar] [CrossRef]
- Munita, J.M.; Arias, C.A. Mechanisms of antibiotic resistance. Microbiol. Spectr. 2016, 4, 481–511. [Google Scholar] [CrossRef]
- Fehr, J.; Hatz, C.; Soka, I.; Kibatala, P.; Urassa, H.; Battegay, M.; Jeffrey, Z.; Smith, T.; Mshinda, H.; Frei, R. Antimicrobial prophylaxis to prevent surgical site infections in a rural sub-Saharan hospital. Clin. Microbiol. Infect. 2006, 12, 1224–1227. [Google Scholar] [CrossRef]
- Teillant, A.; Gandra, S.; Barter, D.; Morgan, D.J.; Laxminarayan, R. Potential burden of antibiotic resistance on surgery and cancer chemotherapy antibiotic prophylaxis in the USA: A literature review and modelling study. Lancet Infect. Dis. 2015, 15, 1429–1437. [Google Scholar] [CrossRef]
- Memar, M.Y.; Yekani, M.; Alizadeh, N.; Baghi, H.B. Hyperbaric oxygen therapy: Antimicrobial mechanisms and clinical application for infections. Biomed. Pharmacother. 2019, 109, 440–447. [Google Scholar] [CrossRef] [PubMed]
- de Smet, G.H.; Kroese, L.F.; Menon, A.G.; Jeekel, J.; van Pelt, A.W.; Kleinrensink, G.J.; Lange, J.F. Oxygen therapies and their effects on wound healing. Wound Repair Regen. 2017, 25, 591–608. [Google Scholar] [CrossRef]
- Greif, R.; Akça, O.; Horn, E.-P.; Kurz, A.; Sessler, D.I. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N. Engl. J. Med. 2000, 342, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Stizzo, M.; Manfredi, C.; Spirito, L.; Sciorio, C.; Romero Otero, J.; Martinez Salamanca, J.I.; Crocetto, F.; Verze, P.; Imbimbo, C.; Fusco, F. Hyperbaric oxygen therapy as adjuvant treatment for surgical site infections after male-to-female gender affirmation surgery: A 10-year experience. Andrology 2022, 10, 1310–1316. [Google Scholar] [CrossRef]
- Tibbles, P.M.; Edelsberg, J.S. Hyperbaric-oxygen therapy. N. Engl. J. Med. 1996, 334, 1642–1648. [Google Scholar] [CrossRef] [PubMed]
- Leach, R.; Rees, P.; Wilmshurst, P. Hyperbaric oxygen therapy. BMJ 1998, 317, 1140–1143. [Google Scholar] [CrossRef]
- Grim, P.S.; Gottlieb, L.J.; Boddie, A.; Batson, E. Hyperbaric oxygen therapy. JAMA 1990, 263, 2216–2220. [Google Scholar] [CrossRef] [PubMed]
- Velure, G.K.; Müller, B.; Hauken, M.A. Symptom burden and health-related quality of life six months after hyperbaric oxygen therapy in cancer survivors with pelvic radiation injuries. Support. Care Cancer 2022, 30, 5703–5711. [Google Scholar] [CrossRef] [PubMed]
- Oscarsson, N.; Müller, B.; Rosén, A.; Lodding, P.; Mölne, J.; Giglio, D.; Hjelle, K.M.; Vaagbø, G.; Hyldegaard, O.; Vangedal, M. Radiation-induced cystitis treated with hyperbaric oxygen therapy (RICH-ART): A randomised, controlled, phase 2–3 trial. Lancet Oncol. 2019, 20, 1602–1614. [Google Scholar] [CrossRef]
- Hachmo, Y.; Hadanny, A.; Hamed, R.A.; Daniel-Kotovsky, M.; Catalogna, M.; Fishlev, G.; Lang, E.; Polak, N.; Doenyas, K.; Friedman, M. Hyperbaric oxygen therapy increases telomere length and decreases immunosenescence in isolated blood cells: A prospective trial. Aging 2020, 12, 22445. [Google Scholar] [CrossRef]
- Oley, M.H.; Oley, M.C.; Durry, M.F.; Adam, R.N.; Gunawan, D.F.; Faruk, M. Fostering a faster post-operative wound healing process with hyperbaric oxygen therapy in a rare case of squamous odontogenic tumor. Int. J. Surg. Case Rep. 2022, 90, 106718. [Google Scholar] [CrossRef] [PubMed]
- Kranke, P.; Bennett, M.H.; Martyn-St James, M.; Schnabel, A.; Debus, S.E.; Weibel, S. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P.; Møller, S.; Lerche, C.; Moser, C.; Bjarnsholt, T.; Ciofu, O.; Faurholt-Jepsen, D.; Høiby, N.; Kolpen, M. Improving antibiotic treatment of bacterial biofilm by hyperbaric oxygen therapy: Not just hot air. Biofilm 2019, 1, 100008. [Google Scholar] [CrossRef]
- Oley, M.H.; Oley, M.C.; Wewengkang, L.A.W.; Kepel, B.J.; Langi, F.L.F.G.; Setiadi, T.; Aling, D.M.R.; Gunawan, D.F.; Tulong, M.T.; Faruk, M. Bactericidal effect of hyperbaric oxygen therapy in burn injuries. Ann. Med. Surg. 2022, 74, 103314. [Google Scholar] [CrossRef]
- Shah, J. Hyperbaric oxygen therapy. J. Am. Coll. Certif. Wound Spec. 2010, 2, 9–13. [Google Scholar] [CrossRef]
- Moen, I.; Stuhr, L.E. Hyperbaric oxygen therapy and cancer—A review. Target. Oncol. 2012, 7, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Kirby, J.P.; Snyder, J.; Schuerer, D.J.; Peters, J.S.; Bochicchio, G.V. Essentials of hyperbaric oxygen therapy: 2019 review. Mo. Med. 2019, 116, 176. [Google Scholar] [PubMed]
- Frykberg, R.G. Topical wound oxygen therapy in the treatment of chronic diabetic foot ulcers. Medicina 2021, 57, 917. [Google Scholar] [CrossRef] [PubMed]
- Feldmeier, J.; Hopf, H.; Warriner III, R.; Fife, C.; Gesell, L.; Bennett, M. UHMS position statement: Topical oxygen for chronic wounds. Undersea Hyperb. Med. 2005, 32, 157–168. [Google Scholar]
- Oguz, H.; Sobaci, G. The use of hyperbaric oxygen therapy in ophthalmology. Surv. Ophthalmol. 2008, 53, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Mogami, H.; Hayakawa, T.; Kanai, N.; Kuroda, R.; Yamada, R.; Ikeda, T.; Katsurada, K.; Sugimoto, T. Clinical application of hyperbaric oxygenation in the treatment of acute cerebral damage. J. Neurosurg. 1969, 31, 636–643. [Google Scholar] [CrossRef]
- Edwards, M.L. Hyperbaric oxygen therapy. Part 2: Application in disease. J. Vet. Emerg. Crit. Care 2010, 20, 289–297. [Google Scholar] [CrossRef]
- Lin, L.J.; Chen, T.X.; Wald, K.J.; Tooley, A.A.; Lisman, R.D.; Chiu, E.S. Hyperbaric oxygen therapy in ophthalmic practice: An expert opinion. Expert Rev. Ophthalmol. 2020, 15, 119–126. [Google Scholar] [CrossRef]
- Helms, A.K.; Whelan, H.T.; Torbey, M.T. Hyperbaric oxygen therapy of cerebral ischemia. Cerebrovasc. Dis. 2005, 20, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Matchett, G.A.; Martin, R.D.; Zhang, J.H. Hyperbaric oxygen therapy and cerebral ischemia: Neuroprotective mechanisms. Neurol. Res. 2009, 31, 114–121. [Google Scholar] [CrossRef]
- McDonagh, M.S.; Morgan, D.; Carson, S.; Russman, B.S. Systematic review of hyperbaric oxygen therapy for cerebral palsy: The state of the evidence. Dev. Med. Child Neurol. 2007, 49, 942–947. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.-Y.; Yang, Y.-R.; Chang, H.-C. The SDF1-CXCR4 axis is involved in the hyperbaric oxygen therapy-mediated neuronal cells migration in transient brain ischemic rats. Int. J. Mol. Sci. 2022, 23, 1780. [Google Scholar] [CrossRef]
- Thiankhaw, K.; Chattipakorn, N.; Chattipakorn, S.C. The effects of hyperbaric oxygen therapy on the brain with middle cerebral artery occlusion. J. Cell. Physiol. 2021, 236, 1677–1694. [Google Scholar] [CrossRef] [PubMed]
- Cevolani, D.; Di Donato, F.; Santarella, L.; Bertossi, S.; Cellerini, M. Functional MRI (fMRI) evaluation of hyperbaric oxygen therapy (HBOT) efficacy in chronic cerebral stroke: A small retrospective consecutive case series. Int. J. Environ. Res. Public Health 2021, 18, 190. [Google Scholar] [CrossRef] [PubMed]
- Borab, Z.; Mirmanesh, M.D.; Gantz, M.; Cusano, A.; Pu, L.L. Systematic review of hyperbaric oxygen therapy for the treatment of radiation-induced skin necrosis. J. Plast. Reconstr. Aesthetic Surg. 2017, 70, 529–538. [Google Scholar] [CrossRef]
- Lalieu, R.C.; Brouwer, R.J.; Ubbink, D.T.; Hoencamp, R.; Bol Raap, R.; van Hulst, R.A. Hyperbaric oxygen therapy for nonischemic diabetic ulcers: A systematic review. Wound Repair Regen. 2020, 28, 266–275. [Google Scholar] [CrossRef]
- Brouwer, R.J.; Lalieu, R.C.; Hoencamp, R.; van Hulst, R.A.; Ubbink, D.T. A systematic review and meta-analysis of hyperbaric oxygen therapy for diabetic foot ulcers with arterial insufficiency. J. Vasc. Surg. 2020, 71, 682–692.e681. [Google Scholar] [CrossRef] [PubMed]
- Löndahl, M.; Boulton, A.J. Hyperbaric oxygen therapy in diabetic foot ulceration: Useless or useful? A battle. Diabetes/Metab. Res. Rev. 2020, 36, e3233. [Google Scholar] [CrossRef]
- Lerche, C.J.; Schwartz, F.; Pries-Heje, M.M.; Fosbøl, E.L.; Iversen, K.; Jensen, P.Ø.; Høiby, N.; Hyldegaard, O.; Bundgaard, H.; Moser, C. Potential advances of adjunctive hyperbaric oxygen therapy in infective endocarditis. Front. Cell. Infect. Microbiol. 2022, 12, 15. [Google Scholar] [CrossRef]
- Hajhosseini, B.; Kuehlmann, B.A.; Bonham, C.A.; Kamperman, K.J.; Gurtner, G.C. Hyperbaric oxygen therapy: Descriptive review of the technology and current application in chronic wounds. Plast. Reconstr. Surg. Glob. Open 2020, 8, e3136. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Petzold, T.; Feindt, P.R.; Carl, U.M.; Gams, E. Hyperbaric oxygen therapy in deep sternal wound infection after heart transplantation. Chest 1999, 115, 1455–1458. [Google Scholar] [CrossRef] [PubMed]
- Siondalski, P.; Keita, L.; Sićko, Z.; Zelechowski, P.; Jaworski, Ł.; Rogowski, J. Surgical treatment and adjunct hyperbaric therapy to improve healing of wound infection complications after sterno-mediastinitis. Pneumonol. Alergol. Pol. 2003, 71, 12–16. [Google Scholar] [PubMed]
- Barili, F.; Polvani, G.; Topkara, V.K.; Dainese, L.; Cheema, F.H.; Roberto, M.; Naliato, M.; Parolari, A.; Alamanni, F.; Biglioli, P. Role of hyperbaric oxygen therapy in the treatment of postoperative organ/space sternal surgical site infections. World J. Surge. 2007, 31, 1702–1706. [Google Scholar] [CrossRef]
- Sun, I.F.; Lee, S.S.; Chiu, C.C.; Lin, S.D.; Lai, C.S. Hyperbaric oxygen therapy with topical negative pressure: An alternative treatment for the refractory sternal wound infection. J. Card. Surg. 2008, 23, 677–680. [Google Scholar] [CrossRef]
- Larsson, A.; Uusijärvi, J.; Lind, F.; Gustavsson, B.; Saraste, H. Hyperbaric oxygen in the treatment of postoperative infections in paediatric patients with neuromuscular spine deformity. Eur. Spine J. 2011, 20, 2217–2222. [Google Scholar] [CrossRef]
- Yu, W.-K.; Chen, Y.-W.; Shie, H.-G.; Lien, T.-C.; Kao, H.-K.; Wang, J.-H. Hyperbaric oxygen therapy as an adjunctive treatment for sternal infection and osteomyelitis after sternotomy and cardiothoracic surgery. J. Cardiothorac. Surg. 2011, 6, 141. [Google Scholar] [CrossRef]
- Egito, J.G.T.d.; Abboud, C.S.; Oliveira, A.P.V.d.; Máximo, C.A.G.; Montenegro, C.M.; Amato, V.L.; Bammann, R.; Farsky, P.S. Clinical evolution of mediastinitis in patients undergoing adjuvant hyperbaric oxygen therapy after coronary artery bypass surgery. Einstein 2013, 11, 345–349. [Google Scholar]
- Inanmaz, M.E.; Kose, K.C.; Isik, C.; Atmaca, H.; Basar, H. Can hyperbaric oxygen be used to prevent deep infections in neuro-muscular scoliosis surgery? BMC Surg. 2014, 14, 85. [Google Scholar] [CrossRef]
- Litwinowicz, R.; Bryndza, M.; Chrapusta, A.; Kobielska, E.; Kapelak, B.; Grudzień, G. Hyperbaric oxygen therapy as additional treatment in deep sternal wound infections-a single center’s experience. Kardiochir. Torakochir. Pol. 2016, 13, 198–202. [Google Scholar] [CrossRef]
- Bartek, J., Jr.; Skyrman, S.; Nekludov, M.; Mathiesen, T.; Lind, F.; Schechtmann, G. Hyperbaric oxygen therapy as adjuvant treatment for hardware-related infections in neuromodulation. Stereotact. Funct. Neurosurg. 2018, 96, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Copeland, H.; Newcombe, J.; Yamin, F.; Bhajri, K.; Mille, V.A.; Hasaniya, N.; Bailey, L.; Razzouk, A.J. Role of negative pressure wound care and hyperbaric oxygen therapy for sternal wound infections after pediatric cardiac surgery. World J. Pediatr. Congenit. Heart Surg. 2018, 9, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Riddick, M. Sternal wound infections, dehiscence, and sterna osteomyelitis: The role of hyperbaric oxygen therapy. In Hyperbaric Medicine Practice; Best Publishing Company: Flagstaff, AZ, USA, 1999; pp. 617–639. [Google Scholar]
- De Feo, M.; Gregorio, R.; Della Corte, A.; Marra, C.; Amarelli, C.; Renzulli, A.; Utili, R.; Cotrufo, M. Deep sternal wound infection: The role of early debridement surgery. Eur. J. Cardio-Thorac. Surg. 2001, 19, 811–816. [Google Scholar] [CrossRef]
- Kaide, C.G.; Khandelwal, S. Hyperbaric oxygen: Applications in infectious disease. Emerg. Med. Clin. N. Am. 2008, 26, 571–595. [Google Scholar] [CrossRef]
- Vatansever, F.; de Melo, W.C.; Avci, P.; Vecchio, D.; Sadasivam, M.; Gupta, A.; Chandran, R.; Karimi, M.; Parizotto, N.A.; Yin, R. Antimicrobial strategies centered around reactive oxygen species–bactericidal antibiotics, photodynamic therapy, and beyond. FEMS Microbiol. Rev. 2013, 37, 955–989. [Google Scholar] [CrossRef]
- Lam, G.; Fontaine, R.; Ross, F.L.; Chiu, E.S. Hyperbaric oxygen therapy: Exploring the clinical evidence. Adv. Ski. Wound Care 2017, 30, 181–190. [Google Scholar] [CrossRef]
- Memar, M.Y.; Ghotaslou, R.; Samiei, M.; Adibkia, K. Antimicrobial use of reactive oxygen therapy: Current insights. Infect. Drug Resist. 2018, 11, 567. [Google Scholar] [CrossRef]
- Gill, A.Á.; Bell, C.N. Hyperbaric oxygen: Its uses, mechanisms of action and outcomes. QJM 2004, 97, 385–395. [Google Scholar] [CrossRef]
- Ortega, M.A.; Fraile-Martinez, O.; García-Montero, C.; Callejón-Peláez, E.; Sáez, M.A.; Álvarez-Mon, M.A.; García-Honduvilla, N.; Monserrat, J.; Álvarez-Mon, M.; Bujan, J. A general overview on the hyperbaric oxygen therapy: Applications, mechanisms and translational opportunities. Medicina 2021, 57, 864. [Google Scholar] [CrossRef]
- Shinomiya, N. Molecular mechanisms of hyperbaric oxygen therapy. In Hyperbaric Oxygenation Therapy; Springer: Singapore, 2020; pp. 3–20. [Google Scholar]
- Çimşit, M.; Uzun, G.; Yıldız, Ş. Hyperbaric oxygen therapy as an anti-infective agent. Expert Rev. Anti-Infect. Ther. 2009, 7, 1015–1026. [Google Scholar] [CrossRef] [PubMed]
- Mills, C. The role of hyperbaric oxygen therapy in the treatment of sternal wound infection. Eur. J. Cardio-Thorac. Surg. 2006, 30, 153–159. [Google Scholar] [CrossRef]
- Dryden, M.; Cooke, J.; Salib, R.; Holding, R.; Pender, S.L.; Brooks, J. Hot topics in reactive oxygen therapy: Antimicrobial and immunological mechanisms, safety and clinical applications. J. Glob. Antimicrob. Resist. 2017, 8, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.G.; Cooper, M.; Yost, A.; Paff, M.; Ercan, U.K.; Fridman, G.; Friedman, G.; Fridman, A.; Brooks, A.D. Nonthermal dielectric-barrier discharge plasma-induced inactivation involves oxidative DNA damage and membrane lipid peroxidation in Escherichia coli. Antimicrob. Agents Chemother. 2011, 55, 1053–1062. [Google Scholar] [CrossRef] [PubMed]
- Cabiscol Català, E.; Tamarit Sumalla, J.; Ros Salvador, J. Oxidative stress in bacteria and protein damage by reactive oxygen species. Int. Microbiol. 2000, 3, 3–8. [Google Scholar]
- Granowitz, E.; Skulsky, E.; Benson, R.; Wright, J.; Garb, J.; Cohen, E.; Smithline, E.; Brown, R. Exposure to increased pressure or hyperbaric oxygen suppresses interferon-gamma secretion in whole blood cultures of healthy humans. Undersea Hyperb. Med. 2002, 29, 216–225. [Google Scholar]
- Weisz, G.; Lavy, A.; Adir, Y.; Melamed, Y.; Rubin, D.; Eidelman, S.; Pollack, S. Modification of in vivo and in vitro TNF-α, IL-1, and IL-6 secretion by circulating monocytes during hyperbaric oxygen treatment in patients with perianal Crohn’s disease. J. Clin. Immunol. 1997, 17, 154–159. [Google Scholar] [CrossRef]
- Spiegelberg, L.; Swagemakers, S.; Van Ijcken, W.F.; Oole, E.; Wolvius, E.B.; Essers, J.; Braks, J.A. Gene expression analysis reveals inhibition of radiation-induced TGFβ-signaling by hyperbaric oxygen therapy in mouse salivary glands. Mol. Med. 2014, 20, 257–269. [Google Scholar] [CrossRef]
- Weber, S.U.; Koch, A.; Kankeleit, J.; Schewe, J.-C.; Siekmann, U.; Stüber, F.; Hoeft, A.; Schröder, S. Hyperbaric oxygen induces apoptosis via a mitochondrial mechanism. Apoptosis 2009, 14, 97–107. [Google Scholar] [CrossRef]
- Hopf, H.W.; Holm, J. Hyperoxia and infection. Best Pract. Res. Clin. Anaesthesiol. 2008, 22, 553–569. [Google Scholar] [CrossRef]
- Kalns, J.; Lane, J.; Delgado, A.; Scruggs, J.; Ayala, E.; Gutierrez, E.; Warren, D.; Niemeyer, D.; Wolf, E.G.; Bowden, R.A. Hyperbaric oxygen exposure temporarily reduces Mac-1 mediated functions of human neutrophils. Immunol. Lett. 2002, 83, 125–131. [Google Scholar] [CrossRef]
- Buras, J.A.; Stahl, G.L.; Svoboda, K.K.; Reenstra, W.R. Hyperbaric oxygen downregulates ICAM-1 expression induced by hypoxia and hypoglycemia: The role of NOS. Am. J. Physiol.-Cell Physiol. 2000, 278, C292–C302. [Google Scholar] [CrossRef] [PubMed]
- Winterbourn, C.C.; Kettle, A.J.; Hampton, M.B. Reactive oxygen species and neutrophil function. Annu. Rev. Biochem. 2016, 85, 765–792. [Google Scholar] [CrossRef]
- Turhan, V.; Sacar, S.; Uzun, G.; Sacar, M.; Yildiz, S.; Ceran, N.; Gorur, R.; Oncul, O. Hyperbaric oxygen as adjunctive therapy in experimental mediastinitis. J. Surg. Res. 2009, 155, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Jallali, N.; Withey, S.; Butler, P. Hyperbaric oxygen as adjuvant therapy in the management of necrotizing fasciitis. Am. J. Surg. 2005, 189, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Lerche, C.; Christophersen, L.; Kolpen, M.; Nielsen, P.; Trøstrup, H.; Thomsen, K.; Hyldegaard, O.; Bundgaard, H.; Jensen, P.; Høiby, N. Hyperbaric oxygen therapy augments tobramycin efficacy in experimental Staphylococcus aureus endocarditis. Int. J. Antimicrob. Agents 2017, 50, 406–412. [Google Scholar] [CrossRef]
- Mendel, V.; Reichert, B.; Simanowski, H.; Scholz, H.-C. Therapy with hyperbaric oxygen and cefazolin for experimental osteomyelitis due to Staphylococcus aureus in rats. Undersea Hyperb. Med. 1999, 26, 169. [Google Scholar]
- Lima, F.L.; Joazeiro, P.P.; Lancellotti, M.; De Hollanda, L.M.; de Araújo Lima, B.; Linares, E.; Augusto, O.; Brocchi, M.; Giorgio, S. Effects of hyperbaric oxygen on Pseudomonas aeruginosa susceptibility to imipenem and macrophages. Future Microbiol. 2015, 10, 179–189. [Google Scholar] [CrossRef]
- Kolpen, M.; Mousavi, N.; Sams, T.; Bjarnsholt, T.; Ciofu, O.; Moser, C.; Kühl, M.; Høiby, N.; Jensen, P.Ø. Reinforcement of the bactericidal effect of ciprofloxacin on Pseudomonas aeruginosa biofilm by hyperbaric oxygen treatment. Int. J. Antimicrob. Agents 2016, 47, 163–167. [Google Scholar] [CrossRef]
- Plafki, C.; Peters, P.; Almeling, M.; Welslau, W.; Busch, R. Complications and side effects of hyperbaric oxygen therapy. Aviat. Space Environ. Med. 2000, 71, 119–124. [Google Scholar]
- Camporesi, E.M. Side effects of hyperbaric oxygen therapy. Undersea Hyperb. Med. J. Undersea Hyperb. Med. Soc. Inc. 2014, 41, 253–257. [Google Scholar]
- Heyboer III, M.; Sharma, D.; Santiago, W.; McCulloch, N. Hyperbaric oxygen therapy: Side effects defined and quantified. Adv. Wound Care 2017, 6, 210–224. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-Y.; Zhou, Y.-J.; Jia, Y.-Y.; Wang, T.-T.; Meng, D.-H. Adverse effects of hyperbaric oxygen therapy: A systematic review and meta-analysis. Res. Sq. 2023. preprint. [Google Scholar]
- Nasole, E.; Zanon, V.; Marcolin, P.; Bosco, G. Middle ear barotrauma during hyperbaric oxygen therapy; a review of occurrences in 5962 patients. Undersea Hyperb. Med. J. Undersea Hyperb. Med. Soc. Inc. 2019, 46, 101–106. [Google Scholar] [CrossRef]
- Edinguele, W.F.O.P.; Barberon, B.; Poussard, J.; Thomas, E.; Reynier, J.C.; Coulange, M. Middle-ear barotrauma after hyperbaric oxygen therapy: A five-year retrospective analysis on 2610 patients. Undersea Hyperb. Med. J. Undersea Hyperb. Med. Soc. Inc. 2020, 47, 217–228. [Google Scholar]

| Study | Type of Study | Type of Surgery | Type of SSI | Study Population Total; HBOT/Non-HBOT | Pressure (ATA)/Exposure Time (min) | Main Findings and Conclusion |
|---|---|---|---|---|---|---|
| Petzold et al. (1999) [54] | Case report | Cardiac surgery | Sternal SSI | 1 | 2.40/90 | * HBOT resulted in rapid healing and epithelialization of the wound * This was the first reported case of HBOT used for the treatment of deep sternal SSI in a heart transplant recipient. |
| Siondalski et al. (2003) [55] | Retrospective study | Sternotomy | Sternal SSI | 55 | 2.50/90 | * The Sternal SSI was cured in all patients treated with HBOT within an average of 8 weeks * There was no in-hospital death. * The combination of surgical treatment and HBOT could improve clinical outcome in patients with sterno-mediastinis and poststernotomy wound infection after cardiac surgery |
| Barili et al. (2007) [56] | Prospective trial | Cardiac surgery | Sternal SSI | 32; 14/18 | 2–3/90 | * Staphylococcus was the most common pathogen for both groups. * The duration of infection was similar in groups 1 and 2 (31.8 ± 7.6 vs. 29.3 ± 5.7 days, respectively, p = 0.357). * The infection relapse rate was significantly lower in group 1 (0% vs. 33.3%, p = 0.024). * The duration of intravenous antibiotic use (47.8 ± 7.4 vs. 67.6 ± 25.1 days, p = 0.036) and total hospital stay (52.6 ± 9.1 vs. 73.6 ± 24.5 days, p = 0.026) were both significantly shorter in group 1. * HBOT could be a valuable addition to the armamentarium available to physicians treating postoperative organ/space sternal SSI. |
| Sun et al. (2008) [57] | Case report | Cardiac surgery | Sternal SSI | 1 | 2.50/90 | * After nine weeks, the sternal wound was healed and completely epithelialized. * HBOT with Topical Negative Pressure (TNP) dressing is a good alternative method for patients who cannot tolerate or refuse to receive any surgical reconstruction. |
| Larsson et al. (2011) [58] | Retrospective study | neuro-muscular scoliosis surgery | Deep wound infection | 6 | 2.50/3 × 25 | * All infections were resolved and wound healing occurred within an average of 3 months. * Side effects of HBO treatment were minor. * HBOT is a safe and potentially useful adjuvance treatment for early deep postoperative infections in complex situations with spinal implants in high-risk paediatric patients. |
| Yu et al. (2011) [59] | Retrospective study | Cardiac surgery | Sternal SSI | 12; 6/6 | 2.50/90 | * HBOT did not cause any treatment-related complication in patients receiving this additional treatment. * Comparisons of the data between two study groups revealed that the length of stay in ICU (8.7 ± 2.7 days vs. 48.8 ± 10.5 days, p < 0.05), duration of invasive (4 ± 1.5 days vs. 34.8 ± 8.3 days, p < 0.05) and noninvasive (4 ± 1.9 days vs. 22.3 ± 6.2 days, p < 0.05) positive pressure ventilation, and hospital mortality (0 case vs. 3 cases, p < 0.05) were all significantly lower in patients who received additional HBOT, as compared to patients who did not receive HBOT. * In addition to primary treatment with debridement and antibiotic use, HBOT may be used as an adjunctive and safe treatment to improve clinical outcomes in patients with sternal infection and osteomyelitis after sternotomy and cardiothoracic surgery. |
| do Egito et al. (2013) [60] | Retrospective study | Coronary artery bypass surgery | Mediastinitis | 18 | 2.50/90 | * There was only one hospital death, 7 months after the oxygen therapy, which was caused by sepsis and was unrelated to HBOT. * HBOT was well-tolerated. * HBOT used as an adjunctive therapy for treatment of mediastinis patients after CABS resulted in favorable clinical outcomes. |
| Inanmaz et al. (2014) [61] | Retrospective study | neuro-muscular scoliosis surgery | Deep wound infection | 42; 18/24 | 2.40/90 | * The overall incidence of infection in the whole study group was 11.9% (5/42). * The infection rate in the P-HBO and the control group were 5.5% (1/18), and 16.6% (4/24) respectively. * The use of HBO was found to significantly decrease the incidence of postoperative infections in neuromuscular scoliosis patients. * This study indicated that HBOT is a safe and potentially useful supplement which can be used to prevent postoperative deep infections in complex spine deformity in high-risk neuromuscular patients. |
| Litwinowicz et al. (2016) [62] | Retrospective study | Cardiac surgery | Sternal SSI | 10 | 2.50/92 | After 4 weeks of HBOT, seven (70%) patients presented complete wound healing with fibrous scar formation. * One patient qualified for another cycle of HBOT with twenty additional sessions, and after that complete wound healing with fibrous scar formation was observed. * In 2 cases, patients received 5 and 19 of 20 sessions; however, the HBOT course was interrupted because of the patients did not qualify for HBOT. * HBOT, as an additional therapy in DSWI, was successful in 80% of cases, and no complications were observed. |
| Bartek Jr et al. (2018) [63] | Retrospective study | Neuromodulation | Hardware-related infection | 14 | 2.0–2.8/75 | * Twelve out of fourteen events of hardware-related infection were successfully treated without hardware removal (86%). * Two patients treated twice with HBOT on two time-independent occasions could retain their hardware in both cases. * Hardware was removed following HBOT failure in two infection events, with long-term infection control achieved in all patients. * Furthermore, an intrathecal pump malfunction caused by HBOT at 2.8 bars was observed, leading to a change in the manufacturer’s guidelines. * This study indicates a potential benefit of adjuvant HBOT in the treatment of hardware-related infections in neuromodulation, diminishing the need for hardware removal and treatment interruption. |
| Copeland et al. (2018) [64] | Retrospective study | Cardiac surgery | Sternal SSI | 53 | * The time to discharge for patients readmitted with infected sternotomies was 7.71 (+7.339) days (range: 2–39 days). * The mean duration of time for the wounds to heal with the use of Negative Pressure Wound Care Therapy (NPWT) alone was 31.50 (+12.12) days (range: 21–42 days, median: 31.5 days). * The healing time for wounds treated with HBO was a mean of 35 (+9.90) days (range: 28–42 days; median: 35 days). * The duration of HBOT was an average of 16.17 (+8.99) days (range: 5–35 days), and the average number of HBO treatments was 22.6 (+11.06). * The time to heal for patients who had both NPWT and HBO therapy was 42.88 (+24.94) days (range: 21–98 days, median: 42 days). * The results of this study demonstrate that the multimodality therapy of incision and drainage, and NPWT combined with HBOT and appropriate antibiotics, is successful for management of complex deep sternal wound infections in the pediatric population after congenital heart surgery. | |
| Stizzo et al. (2022) [21] | Retrospective study | male-to-female gender affirmation surgery (MtF-GAS) | SSI | 33; 15/18 | 2.2–3.0/90 | * Complete wound healing was obtained in all 15 patients (100%) of the HBOT group and 17 patients (94.4%) in the non-hyperbaric oxygen therapy group (p = 0.35). * Duration of antibiotic therapy, perineal drain time, bladder catheter time, and hospital stay were significantly lower in the HBOT group (p < 0.05). * This study indicated a role for HBOT as an adjuvant treatment for SSIs in patients undergoing MtF GAS. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, D.; Fu, D.; Yan, L.; Xie, L. The Role of Hyperbaric Oxygen Therapy in the Treatment of Surgical Site Infections: A Narrative Review. Medicina 2023, 59, 762. https://doi.org/10.3390/medicina59040762
Zhou D, Fu D, Yan L, Xie L. The Role of Hyperbaric Oxygen Therapy in the Treatment of Surgical Site Infections: A Narrative Review. Medicina. 2023; 59(4):762. https://doi.org/10.3390/medicina59040762
Chicago/Turabian StyleZhou, Dingzi, Daigang Fu, Ling Yan, and Linshen Xie. 2023. "The Role of Hyperbaric Oxygen Therapy in the Treatment of Surgical Site Infections: A Narrative Review" Medicina 59, no. 4: 762. https://doi.org/10.3390/medicina59040762
APA StyleZhou, D., Fu, D., Yan, L., & Xie, L. (2023). The Role of Hyperbaric Oxygen Therapy in the Treatment of Surgical Site Infections: A Narrative Review. Medicina, 59(4), 762. https://doi.org/10.3390/medicina59040762






