Subsequent Domino Osteoporotic Vertebral Fractures Adversely Affect Short-Term Health-Related Quality of Life: A Prospective Multicenter Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Conservative Treatment
2.3. Patient-Reported Outcome Measures (PROMs)
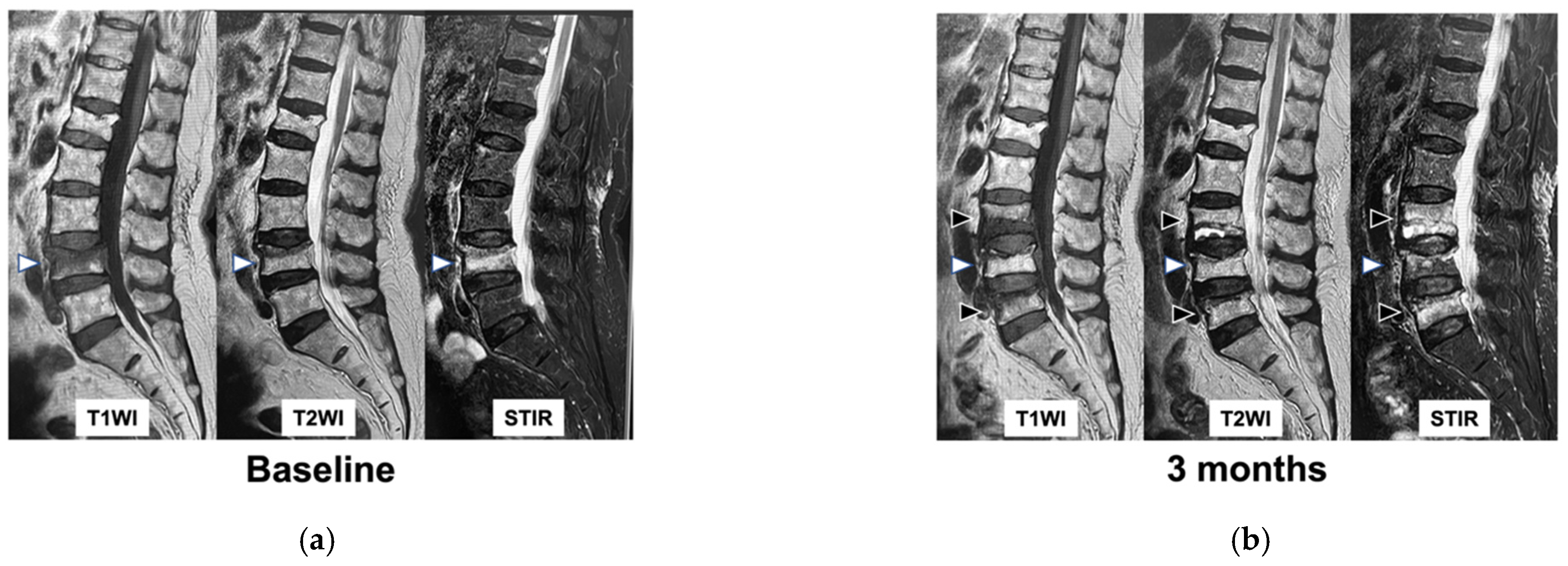
2.4. Imaging Assessment
2.5. Data Analysis
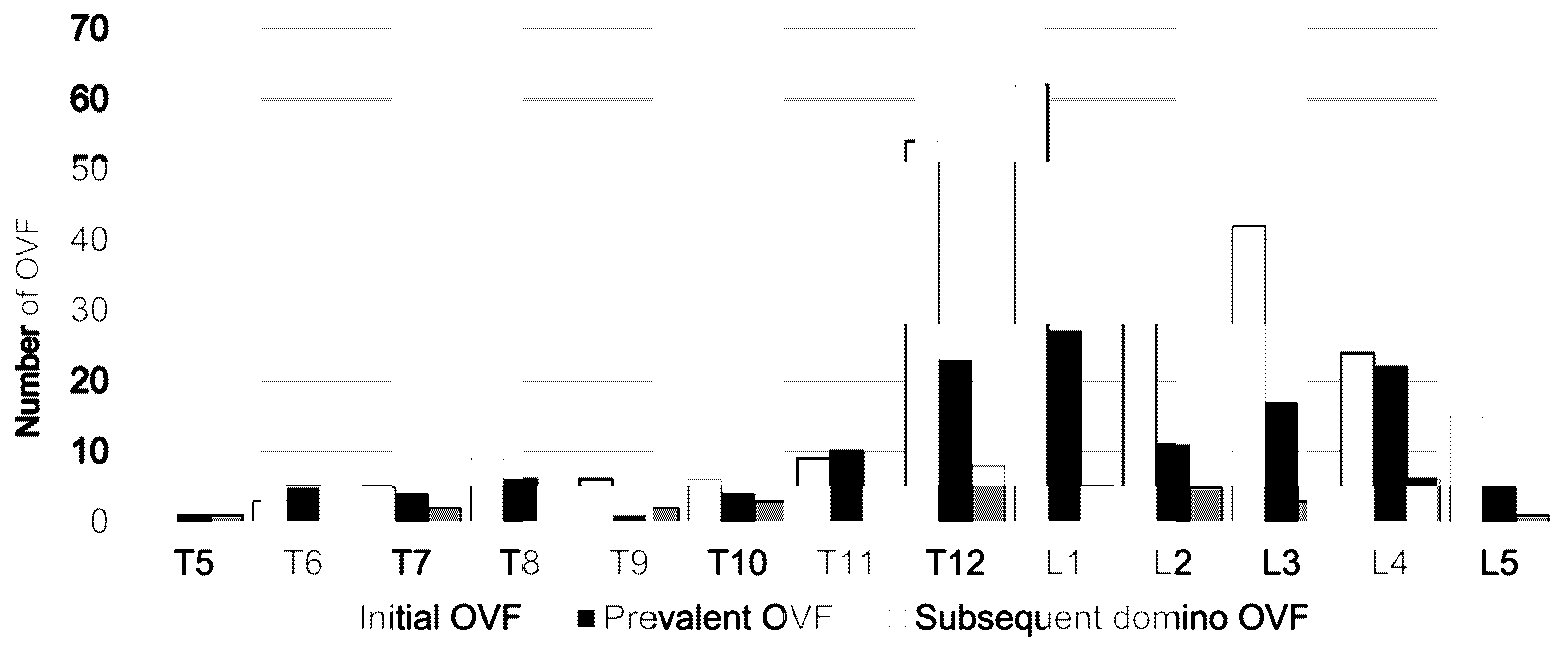
3. Results
3.1. Patient Characteristics
3.2. Comparison of Characteristics and Treatment between the Non-Domino OVF and Domino OVF Groups
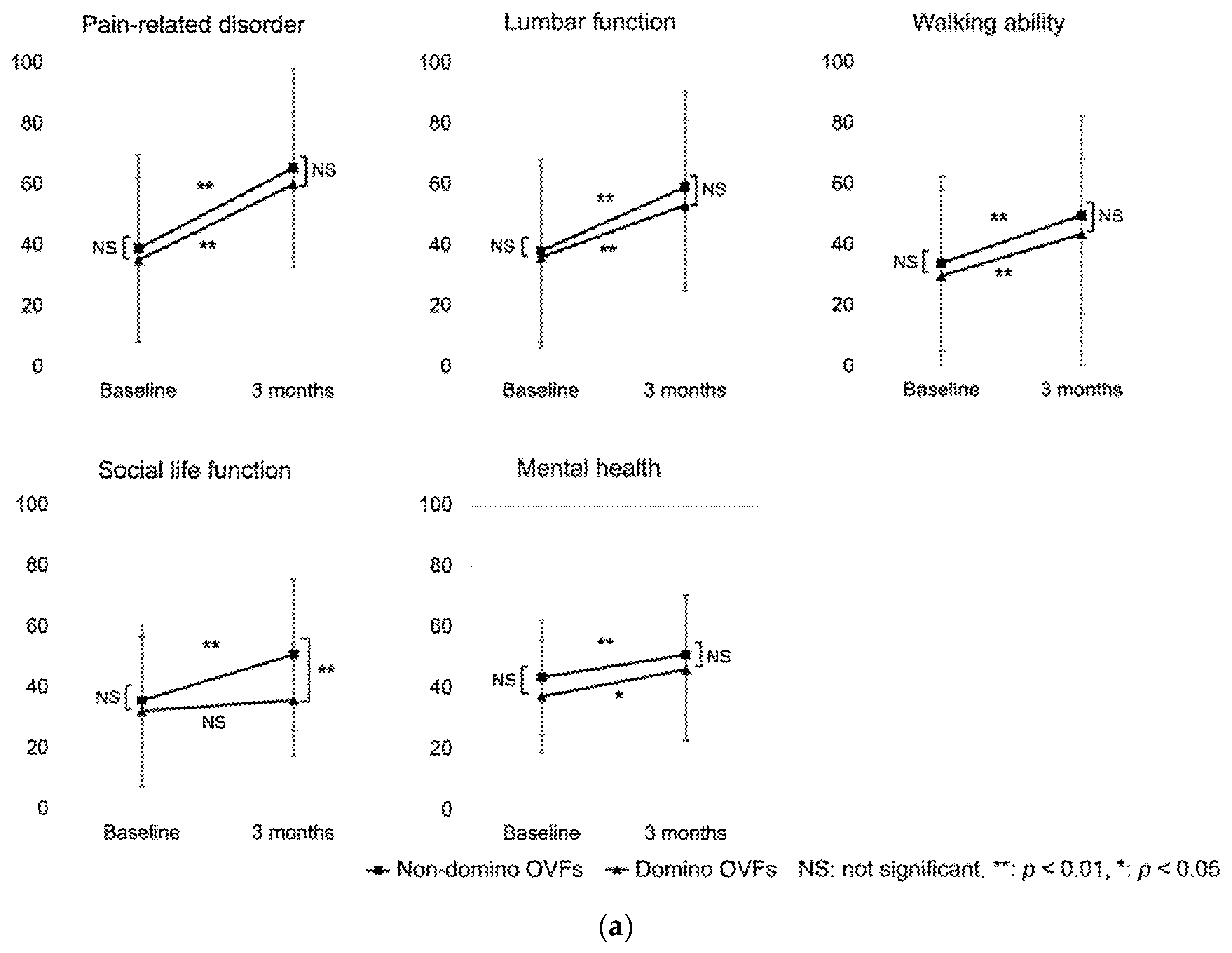
3.3. Comparison of PROMs between the Non-Domino OVF and Domino OVF Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yoshimura, N.; Muraki, S.; Oka, H.; Mabuchi, A.; Kinoshita, H.; Yosihda, M.; Kawaguchi, H.; Nakamura, K.; Akune, T. Epidemiology of lumbar osteoporosis and osteoarthritis and their causal relationship--is osteoarthritis a predictor for osteoporosis or vice versa?: The Miyama study. Osteoporos. Int. 2009, 20, 999–1008. [Google Scholar] [CrossRef]
- Fujiwara, S.; Buchanan-Hughes, A.; Ng, A.; Page, J.; Adachi, K.; Li, H. Real-world evaluation of osteoporotic fractures using the Japan Medical Data Vision database. Osteoporos. Int. 2022, 33, 2205–2216. [Google Scholar] [CrossRef]
- Inose, H.; Kato, T.; Ichimura, S.; Nakamura, H.; Hoshino, M.; Togawa, D.; Hirano, T.; Tokuhashi, Y.; Ohba, T.; Haro, H.; et al. Risk factors for subsequent vertebral fracture after acute osteoporotic vertebral fractures. Eur. Spine J. 2021, 30, 2698–2707. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, A.; Zhang, J.; Chen, L.; Wenkert, D.; Daigle, S.G.; Grauer, A.; Curtis, J.R. Risk of subsequent fracture after prior fracture among older women. Osteoporos. Int. 2019, 30, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Wong, P.Y.; Liu, C.; Wong, H.W.; Chung, Y.L.; Chow, S.K.H.; Law, S.W.; Cheung, W.H. The imminent risk of a fracture-existing worldwide data: A systematic review and meta-analysis. Osteoporos Int. 2022, 33, 2453–2466. [Google Scholar] [CrossRef] [PubMed]
- van Geel, T.A.; Huntjens, K.M.; van den Bergh, J.P.; Dinant, G.J.; Geusens, P.P. Timing of subsequent fractures after an initial fracture. Curr. Osteoporos. Rep. 2010, 8, 118–122. [Google Scholar] [CrossRef]
- Söreskog, E.; Ström, O.; Spångéus, A.; Åkesson, K.E.; Borgström, F.; Banefelt, J.; Toth, E.; Libanati, C.; Charokopou, M. Risk of major osteoporotic fracture after first, second and third fracture in Swedish women aged 50 years and older. Bone 2020, 134, 115286. [Google Scholar] [CrossRef]
- Yamauchi, K.; Adachi, A.; Kameyama, M.; Murakami, M.; Sato, Y.; Kato, C.; Kato, T. A risk factor associated with subsequent new vertebral compression fracture after conservative therapy for patients with vertebral compression fracture: A retrospective observational study. Arch. Osteoporos. 2020, 15, 9. [Google Scholar] [CrossRef]
- Yamaura, T.; Maruo, K.; Arizumi, F.; Kishima, K.; Yoshie, N.; Kusukawa, T.; Tachibana, T. Adjacent vertebral Hounsfield unit value of acute osteoporotic vertebral fracture is a risk factor for concomitant domino osteoporotic vertebral fractures. J. Orthop. Sci. 2022; in press. [Google Scholar]
- Lenski, M.; Büser, N.; Scherer, M. Concomitant and previous osteoporotic vertebral fractures. Acta Orthop. 2017, 88, 192–197. [Google Scholar] [CrossRef]
- Ahmadi, S.A.; Takahashi, S.; Hoshino, M.; Takayama, K.; Sasaoka, R.; Tsujio, T.; Yasuda, H.; Kanematsu, F.; Kono, H.; Toyoda, H.; et al. Association between MRI findings and back pain after osteoporotic vertebral fractures: A multicenter prospective cohort study. Spine J. 2019, 19, 1186–1193. [Google Scholar] [CrossRef]
- Takahashi, S.; Hoshino, M.; Takayama, K.; Iseki, K.; Sasaoka, R.; Tsujio, T.; Yasuda, H.; Sasaki, T.; Kanematsu, F.; Kono, H.; et al. Time course of osteoporotic vertebral fractures by magnetic resonance imaging using a simple classification: A multicenter prospective cohort study. Osteoporos. Int. 2017, 28, 473–482. [Google Scholar] [CrossRef]
- Genant, H.K.; Wu, C.Y.; van Kuijk, C.; Nevitt, M.C. Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 1993, 8, 1137–1148. [Google Scholar] [CrossRef]
- Lindsay, R.; Silverman, S.L.; Cooper, C.; Hanley, D.A.; Barton, I.; Broy, S.B.; Licata, A.; Benhamou, L.; Geusens, P.; Flowers, K.; et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001, 285, 320–323. [Google Scholar] [CrossRef]
- Kim, S.H.; Choi, H.S.; Rhee, Y.; Kim, K.J.; Lim, S.K. Prevalent vertebral fractures predict subsequent radiographic vertebral fractures in postmenopausal Korean women receiving antiresorptive agent. Osteoporos. Int. 2011, 22, 781–787. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.J.; Koo, H.W.; Yoon, S.W.; Sohn, M.J. Usefulness of trabecular CT attenuation measurement of lumbar spine in predicting osteoporotic compression fracture: Is the L4 trabecular region of interest most relevant? Spine (Phila Pa 1976) 2021, 46, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Shevroja, E.; Mo Costabella, F.; Gonzalez Rodriguez, E.; Lamy, O.; Hans, D. The fracture predictive ability of lumbar spine BMD and TBS as calculated based on different combinations of the lumbar spine vertebrae. Arch. Osteoporos. 2022, 17, 83. [Google Scholar] [CrossRef]
- Nardi, A.; Tarantino, U.; Ventura, L.; Armotti, P.; Resmini, G.; Cozzi, L.; Tonini, G.; Ramazzina, E.; Rossini, M. Domino Effect: Mechanic factors role. Clin. Cases Miner. Bone Metab. 2011, 8, 38–42. [Google Scholar]
- Nardi, A.; Ventura, L.; Rossini, M.; Ramazzina, E. The importance of mechanics in the pathogenesis of fragility fractures of the femur and vertebrae. Clin. Cases Miner. Bone Metab. 2010, 7, 130–134. [Google Scholar] [PubMed]
- Okamoto, Y.; Murakami, H.; Demura, S.; Kato, S.; Yoshioka, K.; Hayashi, H.; Sakamoto, J.; Kawahara, N.; Tsuchiya, H. The effect of kyphotic deformity because of vertebral fracture: A finite element analysis of a 10° and 20° wedge-shaped vertebral fracture model. Spine J. 2015, 15, 713–720. [Google Scholar] [CrossRef]
- Piazzolla, A.; Solarino, G.; Lamartina, C.; De Giorgi, S.; Bizzoca, D.; Berjano, P.; Garofalo, N.; Setti, S.; Dicuonzo, F.; Moretti, B. Vertebral bone marrow edema (VBME) in conservatively treated acute vertebral compression fractures (VCFs): Evolution and clinical correlations. Spine (Phila Pa 1976) 2015, 40, E842–E848. [Google Scholar] [CrossRef]
- Inose, H.; Kato, T.; Ichimura, S.; Nakamura, H.; Hoshino, M.; Takahashi, S.; Togawa, D.; Hirano, T.; Tokuhashi, Y.; Ohba, T.; et al. Factors contributing to residual low back pain after osteoporotic vertebral fractures. J. Clin. Med. 2022, 11, 1566. [Google Scholar] [CrossRef]
- Hoshino, M.; Nakamura, H.; Terai, H.; Tsujio, T.; Nabeta, M.; Namikawa, T.; Matsumura, A.; Suzuki, A.; Takayama, K.; Takaoka, K. Factors affecting neurological deficits and intractable back pain in patients with insufficient bone union following osteoporotic vertebral fracture. Eur. Spine J. 2009, 18, 1279–1286. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Man, G.C.W.; Kwok, A.K.L.; Law, S.W.; Chu, W.W.C.; Cheung, W.H.; Qiu, Y.; Cheng, J.C.Y. Global sagittal alignment in elderly patients with osteoporosis and its relationship with severity of vertebral fracture and quality of life. Arch. Osteoporos. 2018, 13, 95. [Google Scholar] [CrossRef] [PubMed]
- LeBoff, M.S.; Greenspan, S.L.; Insogna, K.L.; Lewiecki, E.M.; Saag, K.G.; Singer, A.J.; Siris, E.S. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos. Int. 2022, 33, 2049–2102. [Google Scholar] [CrossRef] [PubMed]
- Bouxsein, M.L.; Eastell, R.; Lui, L.Y.; Wu, L.A.; de Papp, A.E.; Grauer, A.; Marin, F.; Cauley, J.A.; Bauer, D.C.; FNIH Bone Quality Project; et al. Change in Bone Density and Reduction in Fracture Risk: A Meta-Regression of Published Trials. J. Bone Miner. Res. 2019, 34, 632–642. [Google Scholar] [CrossRef]


| Variables | Total n = 227 |
|---|---|
| Age (years) | 80.1 ± 7.3 |
| Sex (female, n, (%)) | 177 (78) |
| Weight (kg) | 52.4 ± 9.5 |
| Height (cm) | 153.1 ± 9.5 |
| BMI (kg/m2) | 22.4 ± 3.6 |
| Number of prevalent OVFs (n, (%)) | |
| 0 | 125 (55) |
| 1 | 70 (31) |
| 2 | 32 (14) |
| Number of initial AOVFs (n, (%)) | |
| 1 | 187 (82.4) |
| 2 | 33 (14.5) |
| 3 | 5 (2.2) |
| 4 | 2 (0.8) |
| HU values (L4) | 56.4 ± 33.8 |
| Lumbar YAM (%) | 77.3 ± 15.9 |
| Femoral YAM (%) | 70.2 ± 14.1 |
| TRACP5b (mU/dL) | 469.3 ± 218.4 |
| P1NP (μg/L) | 76 ± 76.1 |
| Characteristics | Non-domino OVFs n = 196 | Domino OVFs n = 31 | p Value |
|---|---|---|---|
| Age (years) | 79.7 ± 7.5 | 82.1 ± 1.3 | 0.1 |
| Sex (men/women) | 41/155 | 9/22 | 0.31 |
| Body weight (kg) | 52.5 ± 9.7 | 51.9 ± 8.7 | 0.75 |
| Height (cm) | 152.8 ± 8 | 155.2 ± 9.7 | 0.16 |
| Body mass index (kg/m2) | 22.5 ± 3.7 | 21.5 ± 2.5 | 0.22 |
| Number of prevalent OVFs (n, %) | 0.01 * | ||
| none | 113 (57.7) | 12 (38.7) | |
| 1 | 60 (30.6) | 10 (32.2) | |
| 2 | 23 (11.7) | 9 (29) | |
| Multiple AOVFs | 32 (16) | 8 (26) | 0.22 |
| HU values (L4) | 57.8 ± 33.7 | 47.9 ± 34.4 | 0.2 |
| Lumbar BMD (YAM value, %) | 77.7 ± 16.3 | 74.6 ± 12.7 | 0.41 |
| Total hip BMD (YAM value, %) | 70.6 ± 14.6 | 67.8 ± 10.3 | 0.34 |
| TRACP5b (mU/dL) | 458.7 ± 209.8 | 540.2 ± 262.7 | 0.09 |
| P1NP (μg/L) | 76.1 ± 73.4 | 75.7 ± 93.8 | 0.47 |
| Variables | Non-domino OVFs n = 196 | Domino OVFs n = 31 | p Value |
|---|---|---|---|
| Type of brace (n, %) | 0.1 | ||
| hard | 89 (45.4) | 17 (54.8) | |
| soft | 97 (49.5) | 13 (41.9) | |
| none | 7 (3.6) | 1 (3.2) | |
| Hospitalization (yes (n, %)) | 86 (43.9) | 13 (41.9) | 0.84 |
| Anti-osteoporosis medications (n, %) | |||
| Bisphosphonate | 57 (29.1) | 5 (16.1) | 0.54 |
| SERMs | 6 (3.1) | 0 (0) | |
| Denosumab | 11 (5.6) | 4 (12.9) | |
| Teriparatide | 71 (36) | 12 (38.7) | |
| Romosozumab | 22 (11.2) | 7 (22.6) | |
| None | 29 (14.8) | 3 (9.7) | |
| Measures | Non-domino OVFs n = 173 | Domino OVFs n = 22 | p Value |
|---|---|---|---|
| JOABPEQ | |||
| Pain-related disorder | |||
| At baseline | 38 ± 30.6 | 36 ± 32.5 | 0.74 |
| 3 months | 65.4 ± 32.1 | 59.9 ± 37.3 | 0.65 |
| Lumbar function | |||
| At baseline | 33.9 ± 30.5 | 29.7 ± 27.8 | 0.51 |
| 3 months | 59.1 ± 31.3 | 53.1 ± 33.9 | 0.35 |
| Walking ability | |||
| At baseline | 30.7 ± 29.4 | 25.4 ± 23.7 | 0.52 |
| 3 months | 49.6 ± 32 | 43.4 ± 36.4 | 0.31 |
| Social life function | |||
| At baseline | 35.6 ± 24.4 | 32.1 ± 26.9 | 0.37 |
| 3 months | 50.7 ± 24.7 | 35.7 ± 22.3 | <0.01 * |
| Mental health | |||
| At baseline | 43.4 ± 18.3 | 37.1 ± 20.9 | 0.12 |
| 3 months | 50.8 ± 19.1 | 46 ± 23.7 | 0.37 |
| VAS low back pain | |||
| At baseline | 66.1 ± 25.6 | 68 ± 24.5 | 0.8 |
| 3 months | 31.7 ± 25.1 | 43.7 ± 28.7 | 0.04 * |
| ODI | |||
| At baseline | 50.9 ± 22.7 | 54.5 ± 20.6 | 0.58 |
| 3 months | 31.7 ± 20.6 | 44 ± 24.4 | <0.01 * |
| ODI > 40% [n, (%)] | |||
| At baseline | 130 (69.1) | 19 (73.1) | 0.68 |
| 3 months | 53 (30.3) | 15 (60) | <0.01 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kusukawa, T.; Maruo, K.; Toi, M.; Yamaura, T.; Hatano, M.; Nagao, K.; Oishi, H.; Horinouchi, Y.; Arizumi, F.; Kishima, K.; et al. Subsequent Domino Osteoporotic Vertebral Fractures Adversely Affect Short-Term Health-Related Quality of Life: A Prospective Multicenter Study. Medicina 2023, 59, 590. https://doi.org/10.3390/medicina59030590
Kusukawa T, Maruo K, Toi M, Yamaura T, Hatano M, Nagao K, Oishi H, Horinouchi Y, Arizumi F, Kishima K, et al. Subsequent Domino Osteoporotic Vertebral Fractures Adversely Affect Short-Term Health-Related Quality of Life: A Prospective Multicenter Study. Medicina. 2023; 59(3):590. https://doi.org/10.3390/medicina59030590
Chicago/Turabian StyleKusukawa, Tomoyuki, Keishi Maruo, Masakazu Toi, Tetsuto Yamaura, Masaru Hatano, Kazuma Nagao, Hayato Oishi, Yutaka Horinouchi, Fumihiro Arizumi, Kazuya Kishima, and et al. 2023. "Subsequent Domino Osteoporotic Vertebral Fractures Adversely Affect Short-Term Health-Related Quality of Life: A Prospective Multicenter Study" Medicina 59, no. 3: 590. https://doi.org/10.3390/medicina59030590
APA StyleKusukawa, T., Maruo, K., Toi, M., Yamaura, T., Hatano, M., Nagao, K., Oishi, H., Horinouchi, Y., Arizumi, F., Kishima, K., Yoshie, N., & Tachibana, T. (2023). Subsequent Domino Osteoporotic Vertebral Fractures Adversely Affect Short-Term Health-Related Quality of Life: A Prospective Multicenter Study. Medicina, 59(3), 590. https://doi.org/10.3390/medicina59030590






