Acupuncture for Treating Attention Deficit Hyperactivity Disorder in Children: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Registration
2.2. Study Selection
2.2.1. Types of Studies
2.2.2. Types of Participants
2.2.3. Types of Interventions and Controls
2.2.4. Types of Outcome Measures
2.3. Data Sources and Searches
2.3.1. Databases and Other Searches
2.3.2. Search Strategy
2.4. Data Collection, Extraction, and Quality Assessment
2.4.1. Data Extraction
2.4.2. Quality Assessment
2.5. Data Analysis
3. Results
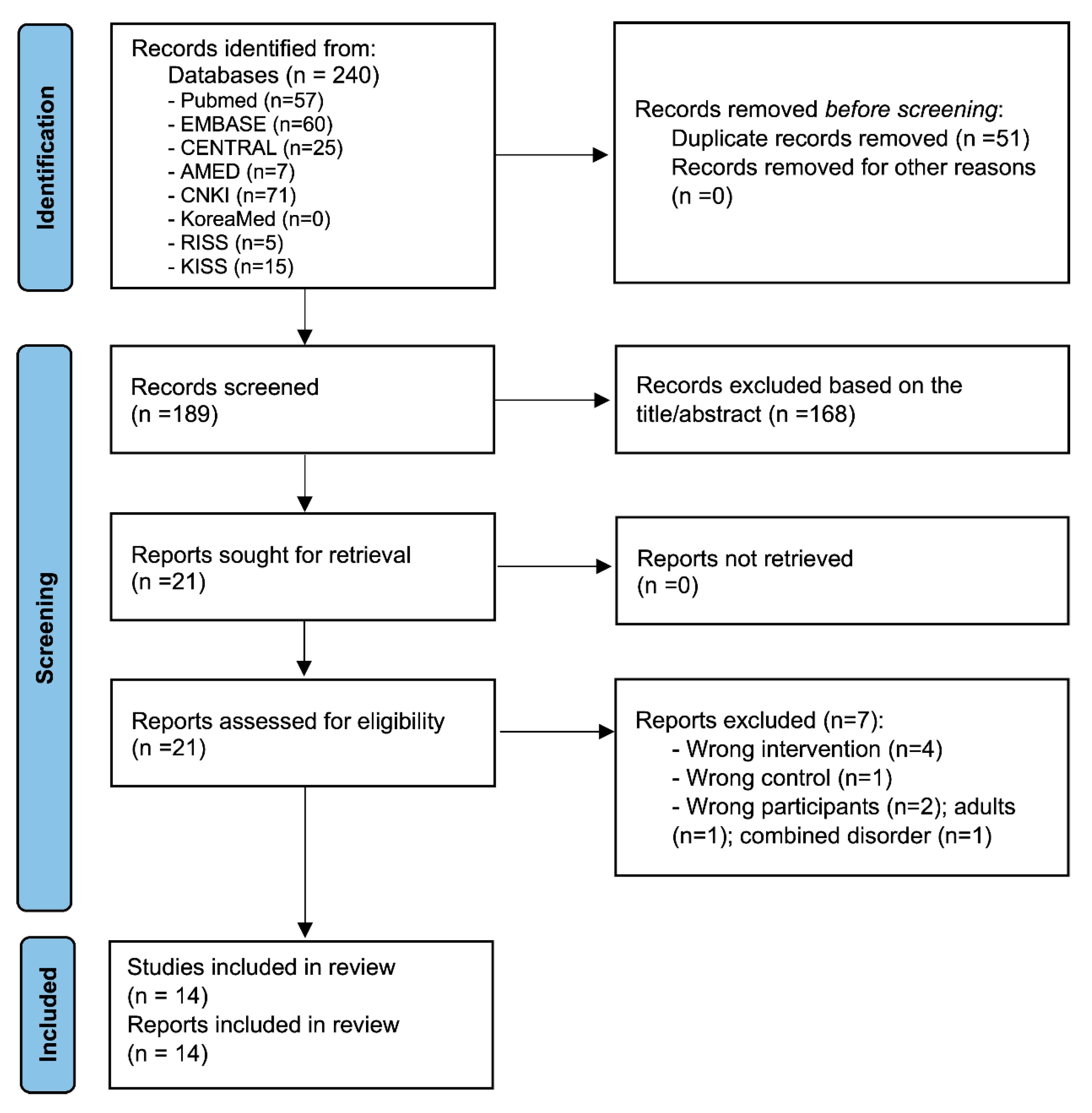
3.1. Study Selection
3.2. Study Characteristics
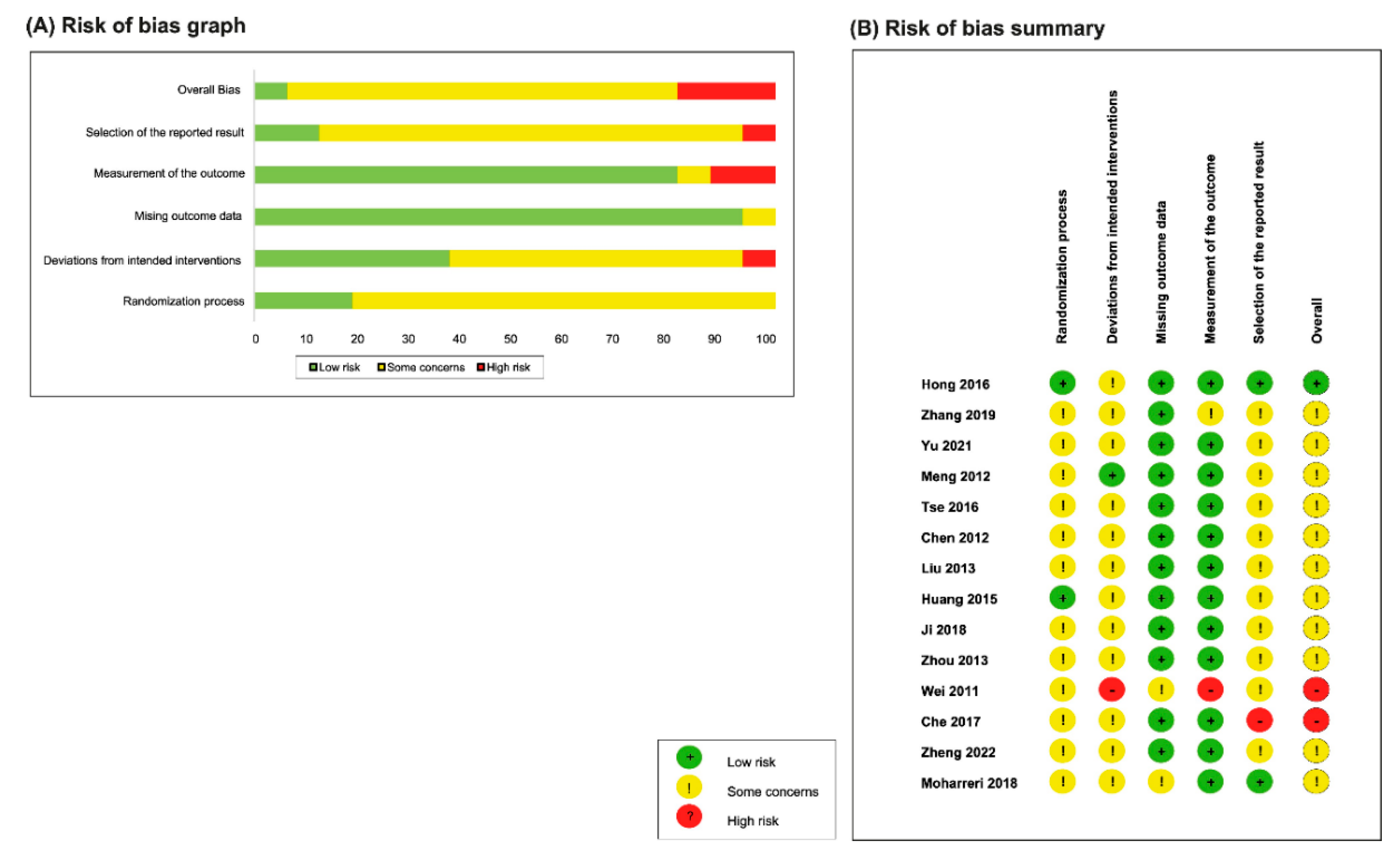
3.3. Risk-of-Bias Assessment
3.4. Effects of Interventions
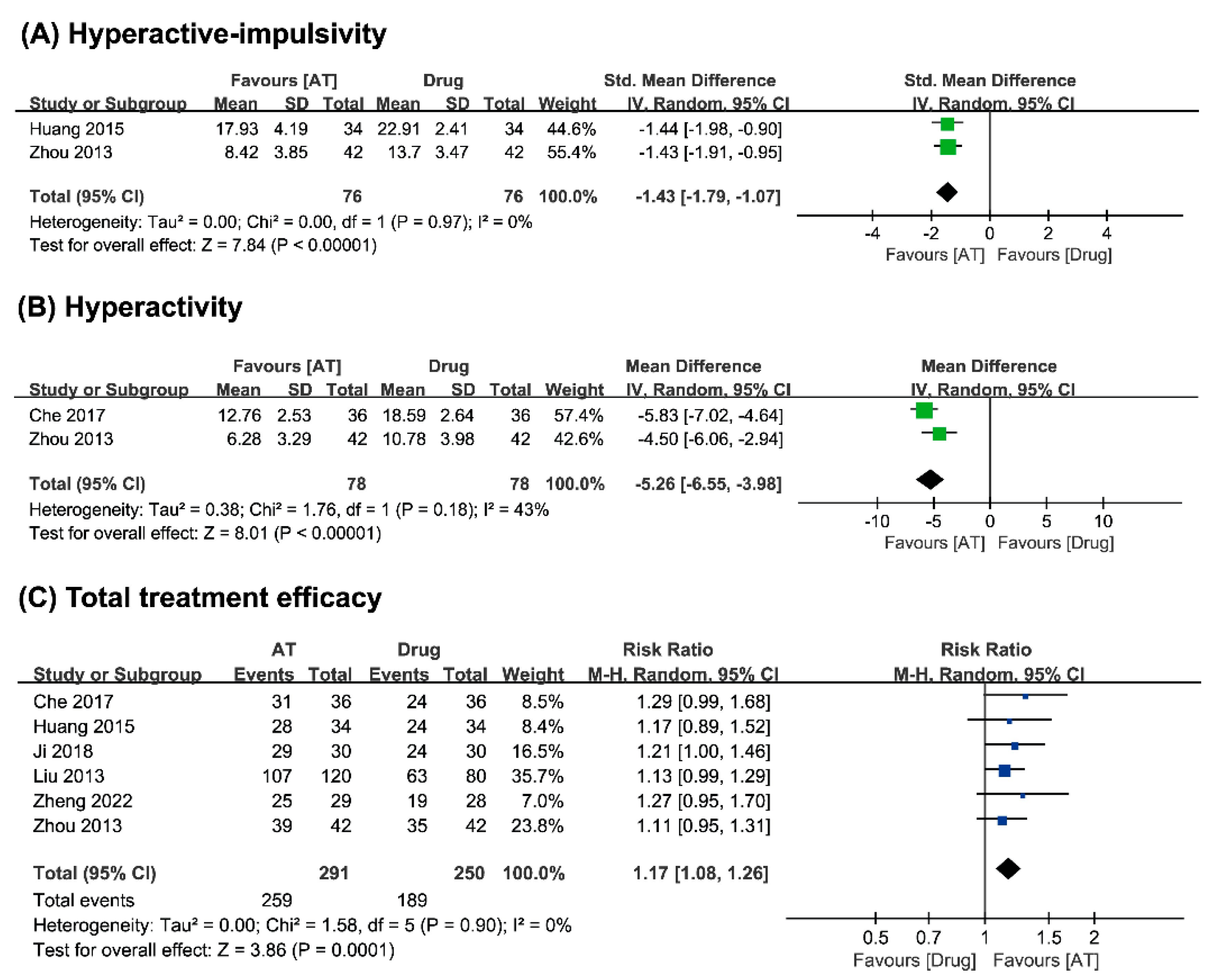
3.4.1. Acupuncture vs. Conventional Medicine
Inattention
Hyperactivity–Impulsivity
Hyperactivity
Conduct Problems
Learning Problems
Total Treatment Efficacy
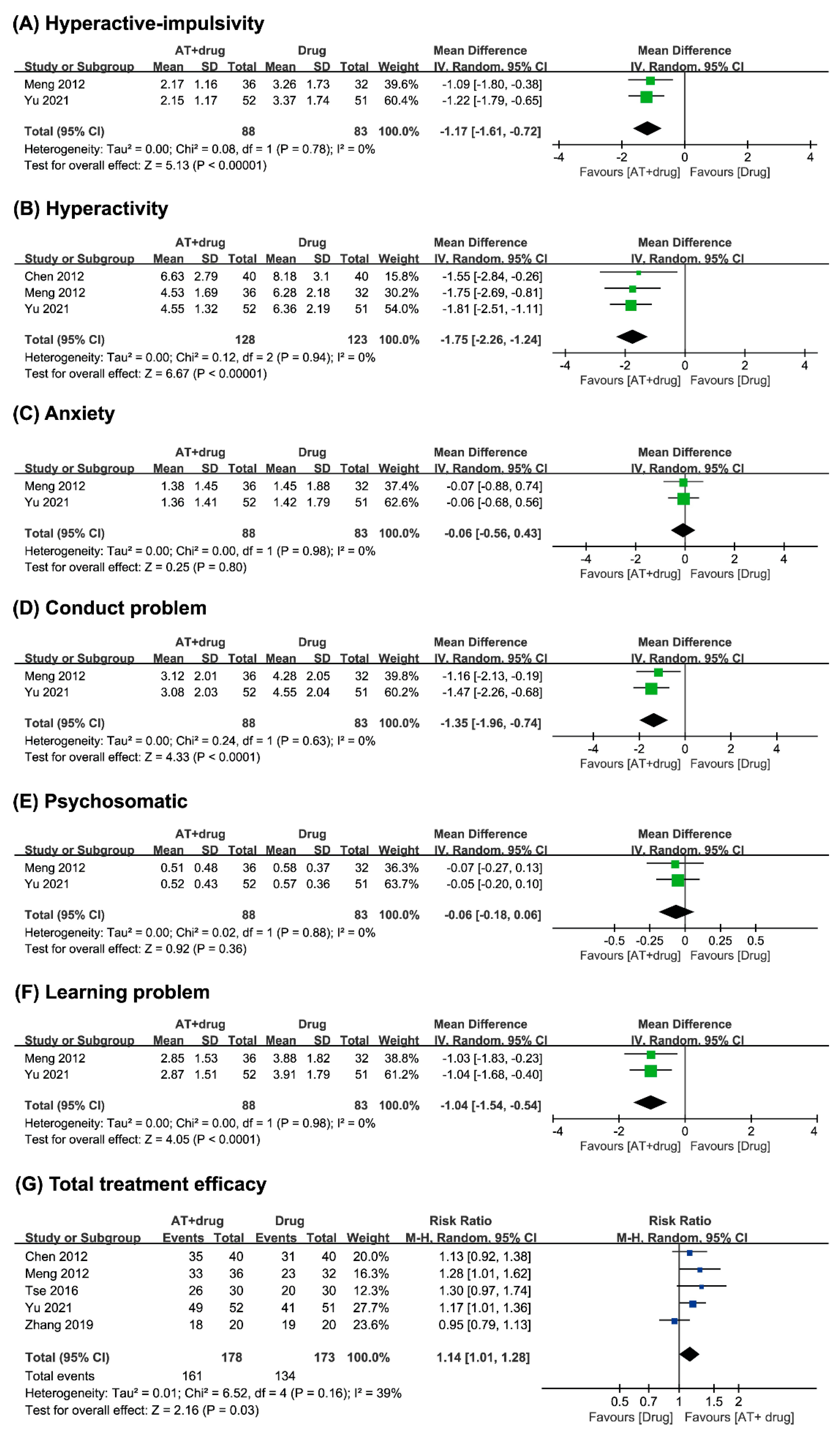
3.4.2. Acupuncture Plus Conventional Medicine vs. Conventional Medicine
Hyperactivity–Impulsivity
Hyperactivity
Anxiety
Conduct Problems
Psychosomatic
Learning Problems
Total Treatment Efficacy
3.4.3. Acupuncture Plus Conventional Medicine vs. Sham Acupuncture Plus Conventional Medicine
Inattention
Hyperactivity–Impulsivity
3.4.4. Adverse Events (AEs)
4. Discussion
4.1. Summary of Main Results
4.2. Overall Completeness and Applicability of Evidence
4.3. Agreements and Disagreements with Other Reviews
4.4. Limitations
4.5. Implications for Practice and Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Magnus, W.; Nazir, S.; Anilkumar, A.C.; Shaban, K. Attention Deficit Hyperactivity Disorder; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Scandurra, V.; Emberti Gialloreti, L.; Barbanera, F.; Scordo, M.R.; Pierini, A.; Canitano, R. Neurodevelopmental Disorders and Adaptive Functions: A Study of Children with Autism Spectrum Disorders (ASD) and/or Attention Deficit and Hyperactivity Disorder (ADHD). Front. Psychiatry 2019, 10, 673. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Treatment of ADHD. Available online: https://www.cdc.gov/ncbddd/adhd/treatment.html (accessed on 5 December 2022).
- Wolraich, M. Attention Deficit Hyperactivity Disorder in Children. BMJ Best Practice. Available online: https://bestpractice.bmj.com/topics/en-gb/142 (accessed on 16 February 2023).
- Zhang, H.J.; Dong, X.L.; Zhang, Y.F.; Fang, Y.F.; Zhang, H.Y. Effect of combination of acupuncture and psychological intervention on attention, response inhibition and cerebral blood flow in children with attention deficit hyperactivity disorder. Zhongguo Zhen Jiu 2021, 41, 400–404. [Google Scholar] [CrossRef]
- Lystad, G.O.; Johannessen, B. Acupuncture and Methylphenidate Drugs in Adults with Attention Deficit Hyperactivity Disorder: A Pilot Study of Self-Reported Symptoms. Complement. Med. Res. 2018, 25, 198–200. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Hao, Z.; Zhang, L.L.; Guo, Q. Efficacy and safety of acupuncture in children: An overview of systematic reviews. Pediatr. Res. 2015, 78, 112–119. [Google Scholar] [CrossRef]
- Chen, Y.C.; Wu, L.K.; Lee, M.S.; Kung, Y.L. The Efficacy of Acupuncture Treatment for Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Complement. Med. Res. 2021, 28, 357–367. [Google Scholar] [CrossRef]
- Lee, M.S.; Choi, T.Y.; Kim, J.I.; Kim, L.; Ernst, E. Acupuncture for treating attention deficit hyperactivity disorder: A systematic review and meta-analysis. Chin. J. Integr. Med. 2011, 17, 257–260. [Google Scholar] [CrossRef]
- Li, S.; Yu, B.; Zhou, D.; He, C.; Kang, L.; Wang, X.; Jiang, S.; Chen, X. Acupuncture for Attention Deficit Hyperactivity Disorder (ADHD) in children and adolescents. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Lansdown, G.; Vaghri, Z. Article 1: Definition of a Child. In Monitoring State Compliance with the UN Convention on the Rights of the Child: An Analysis of Attributes; Vaghri, Z., Zermatten, J., Lansdown, G., Ruggiero, R., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 407–412. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Meng, X.; Zhang, Q. Therapeutic observation on combining acupuncture with Western medication for attention deficit hyperactivity disorder of childhood. Shanghai J. Acupunct. Moxibustion (Shanghai Zhanjiu Zazhi) 2012, 31, 732–733. [Google Scholar]
- Chen, Y.; Zhu, D.; Yang, L. Observation on the efficacy and safety of behavior therapy combined with acupuncture and moxibustion focus on children with ADHD. J. Jianghan Univ. (Jianghan Daxue Xuebao Ziran Kexue Ban) 2012, 40, 93–96. [Google Scholar]
- Tse, W.M. Clinical Study on Treating Attention Deficit Hyperkinetic Disorder with Fang’s Scalp Acupuncture. Ph.D. Thesis, Guangzhou University of Chinese Medicine, Guangzhou, China, 2016. [Google Scholar]
- Yu, C. Clinical observation on acupuncture combined with Western medicine in the treatment of attention deficit hyperactivity disorder in children. Chin. Med. Mod. Distance Educ. China (Zhongguo Zhongyiyao Xiandai Yuancheng Jiaoyu) 2021, 19, 135–137. [Google Scholar] [CrossRef]
- Zhang, P.; Zhan, L.; Wu, Z.; Huang, Y. Observation on treating pediatric ADHD by acupuncture. Clin. J. Chin. Med. (Zhongguo Linchuang Yanjiu) 2019, 11, 35–37. [Google Scholar] [CrossRef]
- Liu, J. Clinical observation on the treatment of attention deficit hyperactivity disorder with Xingnao Kaiqiao acupuncture. Tianjin J. Trad. Chin. Med. (Tianjin Zhonyiyao) 2013, 30, 54–56. [Google Scholar] [CrossRef]
- Huang, L. The Clinical Research on Treating Attention Deficit Hyperactivity Disorder by Tiaorentongdu Acupuncture Therapy. Master’s Thesis, Guangzhou University of Chinese Medicine, Guangzhou, China, 2015. [Google Scholar]
- Ji, X.; He, J.; Zhao, W.; Kou, Z.; Zhou, X. Acupuncture in treating 30 case of children ADHD. Clin. J. Chin. Med. (Zhongguo Linchuang Yanjiu) 2018, 10, 125–127. [Google Scholar] [CrossRef]
- Zhou, X. Observation of curative effect of body acupuncture on children’s attention deficit hyperactivity disorder. Chin. Foreign Med. Res. (Zhongwai Yixue Yanjiu) 2013, 11, 33–34. [Google Scholar] [CrossRef]
- Wei, H. Analysis of clinical treatment of children with ADHD. China Med. Pharm. (Zhongguo Yiyao Kexue) 2011, 1, 157. [Google Scholar]
- Che, J. The 36 cases of children with ADHD caused by yin deficiency and yang hyperactivity treated using acupuncture with calming and eliminating wind technique. World Latest Med. Info. (Shijie Zuixin Yixue Xinxi Wenzhai) 2017, 17, 135–136. [Google Scholar] [CrossRef]
- Zheng, S.; Lian, J.; Wang, Q.; Cui, X.; Ren, R.; Zeng, D. Effect of Tong Yuan acupuncture on electroencephalogram in children with attention deficit disorder with hyperactivity. Shanghai J. Acupunct. Moxibustion (Shanghai Zhanjiu Zazhi) 2022, 41, 392–395. [Google Scholar] [CrossRef]
- Moharreri, F.; Khorsand Vakilzadeh, A.; Soltanifar, A.; Abdollahian, E.; Eslami, S.; Nahidi, M. Efficacy of adding acupuncture to Methylphenidate in children and adolescents with attention deficit hyperactivity disorder: A randomized clinical trial. Eur. J. Integr. Med. 2018, 22, 62–68. [Google Scholar] [CrossRef]
- Hong, S.-S.; Cho, S.-H. Treating attention deficit hyperactivity disorder with acupuncture: A randomized controlled trial. Eur. J. Integr. Med. 2016, 8, 150–157. [Google Scholar] [CrossRef]
| Study ID | Sample Size Gender (M/F) | Age Disease Course (I/C, yr.) | Intervention Group (Regimen, n) | Control Group (Regimen, n) | Acupuncture Points (Main Points) | Outcome Measures/ Rating Scale Used | Results (MD/RR [95%CI], p-Value) |
|---|---|---|---|---|---|---|---|
| Meng 2012 [14] | 68 52/16 | 9/9 5.2/5.3 | (A) AT (3 times per week for 12 weeks, n = 36), plus B | (B) CM (methylphenidate hydrochloride ER tablets, once a day, n = 32) | DU20, DU24, GB13(bil), EM1, PC6, HT7, SP6, KI3, LV3 | (1) PSQ score (2) Treatment efficacy | (1) Anxiety: MD −0.07 [−0.88, 0.74], NS; conduct problems: MD −1.16 [−2.13, −0.19], p = 0.02; hyperactivity: MD −1.75 [−2.69, −0.81], p = 0.0002; hyperactivity–impulsivity: MD −1.09 [−1.80, −0.38], p = 0.003; learning problems: MD −1.09 [−1.80, −0.38], p = 0.003; psychosomatic: MD −0.07 [−0.27, 0.13], NS (2) RR 1.28 [1.01, 1.62], p = 0.05 |
| Chen 2012 [15] | 120 86/34 | 8.6/8.8 2.1/2.3 | (A) AT (2–3 times a week for 12 weeks, n = 40), plus B | (B) CM (methylphenidate hydrochloride ER tablets, once a day, n = 40) (C) Behavioral therapy, plus B (n = 40) | EM2, DU23, DU20, PC6, LI4, DU26, ST36, KI3, SP6, LV3 | (1) PSQ score (2) Treatment efficacy | (1) A vs. B: hyperactivity: MD −5.83 [−7.02, −4.64], p < 0.00001 (2) A vs. B: RR 1.13 [0.92, 1.38], NS |
| Tse 2016 [16] | 60 35/25 | 8.4/9.5 2.5/2.0 | (A) AT (5 times per week for 24 weeks, n = 30), plus B | (B) CM (methylphenidate hydrochloride ER tablets, twice a day, n = 30) | Fang’s scalp acupuncture: Bregma, Lambda, Fuxiang tou, Fuzang shangjiao, Siwei, Jiyi, Yunping | (1) PSQ score (2) SNAP-IV score (3) CRT score (4) Treatment efficacy | (1) Inappropriate reporting (2) MD −3.37 [−5.92, −0.82], p = 0.010 (3) MD 7.85 [5.43, 10.27], p < 0.00001 (4) RR 1.30 [0.97, 1.74], NS |
| Yu 2021 [17] | 103 92/11 | 9.5/9.5 3.2/4.3 | (A) AT (3 times per week for 4 weeks, n = 52), plus B | (B) CM (venlafaxine, once daily, n = 51) | DU20, DU24, GB13(bil), EM1, PC6, HT7, SP6, KI3, LV3 | (1) PSQ score (2) Treatment efficacy | (1) Anxiety: MD −0.06 [−0.68, 0.56], NS; conduct problems: MD −1.47 [−2.26, −0.68], p = 0.0002; hyperactivity: MD −1.81 [−2.51, −1.11], p < 0.00001; hyperactivity–impulsivity: MD −1.22 [−1.79, −0.65], p < 0.0001; learning problems: MD −1.04 [−1.68, −0.40], p = 0.001; psychosomatic: MD −0.05 [−0.20, 0.10], NS (2) RR 1.17 [1.01, 1.36], p = 0.04 |
| Zhang 2019 [18] | 40 27/13 | 8.5 n.r. | (A) AT (1 or 2 times per week for 30 therapies, n = 20), plus B | (B) CM (methylphenidate hydrochloride ER tablets, once daily, n = 20) | EM1, DU24, GB13(bil), EM2, GB14 (bil) | (1) Treatment efficacy (2) Behavioral score * (3) Hyperactivity index * | (1) RR 0.95 [0.79,1.13], NS (2) MD 9.11 [7.19, 11.03], p < 0.00001 (3) MD 2.25 [0.81, 3.69], p = 0.002 |
| Liu 2013 [19] | 200 131/69 | 6–14 n.r. | AT (3 times per week for 12 weeks, n = 120) | CM (methylphenidate hydrochloride ER tablets, twice a day, n = 80) | PC6, DU26, SP6, Du20, EM2, DU23, HT7, PC7 | (1) Treatment efficacy (2) Symptom disappearance rate | (1) RR 1.13 [0.99, 1.29], NS (2) Inappropriate reporting, NS |
| Huang 2015 [20] | 68 35/33 | 6–13 0.5–<1 | AT (3 times per week for 8 weeks, n = 34) | CM (methylphenidate hydrochloride ER tablets, once a day, n = 34) | DU14, DU1, CV15 | (1) SNAP-IV score (2) CRT score (3) Treatment efficacy | (1) Total: MD −8.61 [−10.59, −6.63], p < 0.00001; hyperactivity–impulsivity: MD −4.98 [−6.60, −3.36], p < 0.00001; inattention: MD −5.16 [−6.94, −3.38], p < 0.00001; others: MD −2.25 [−4.38, −0.12], p = 0.04 (2) MD −0.70 [−4.72, 3.32], NS (3) RR 1.17 [0.89, 1.52], NS |
| Ji 2018 [21] | 60 36/24 | 7.6/8.4 0.2–4 | AT (10 times, n = 30) | CM (methylphenidate hydrochloride ER tablets, twice per day, n = 30) | DU20, DU17, EM1, DU24, EM2, ST36 | Treatment efficacy | RR 1.21 [1.00, 1.46], p = 0.05 |
| Zhou 2013 [22] | 84 64/20 | 8.9/8.8 1.9/1.8 | AT (3 times per week for 12 weeks, n = 42) | CM (methylphenidate hydrochloride ER tablets, twice a day, n = 42) | PC6, DU24, SP6, HT7, PC7 | (1) PSQ score (2) Treatment efficacy | (1) Conduct problems: MD 8.25 [4.76, 11.74], p < 0.00001; hyperactivity: MD −4.50 [−6.06, −2.94], p < 0.00001; hyperactivity–impulsivity: MD −5.28 [−6.85, −3.71], p < 0.00001; learning problems: MD 9.70 [5.44, 13.96], p < 0.00001 (2) RR 1.11 [0.95, 1.31], NS |
| Wei 2011 [23] | 70 38/32 | 10.8 n.r. | AT (3 times per week for 4 weeks, n = 35) | CM (methylphenidate hydrochloride ER tablets, twice a day, n = 35) | DU14, CV8 | (1) Rating score * (2) Treatment efficacy | (1) Inappropriate reporting, p < 0.05 (2) Inappropriate reporting, NS |
| Che 2017 [24] | 72 11/7 * | 9.2/7.6 0.8–3.2 | AT (once daily for 4 weeks, n = 36) | CM (Methylphenidate hydrochloride ER tablets, n.r., n = 36) | LV3, KI3, SP6, GB34, LI4, Dacha, HT7, GB-20, EM5, EM2, EM1 | (1) PSQ score (2) Treatment efficacy | (1) Hyperactivity: MD −1.55 [−2.84, −0.26], p = 0.02 (2) RR 1.29 [0.99, 1.68], NS |
| Zheng 2022 [25] | 57 40/17 | 11/11 3.0/3.1 | EA (5 times per week for 12 weeks, n = 30) | Methylphenidate hydrochloride ER tablets, once a day (n = 30) | DU26, EM2, DU20, DU14, BL15 (bil), BL17 (bil), BL18 (bil), BL20 (bil), BL23 (bil), ST25 (bil), CV6, CV4, ST29 (bil) | Treatment efficacy | RR 1.27 [0.95, 1.70], NS |
| Moharreri 2018 [26] | 90 57/7 | 10.4/10.9 n.r. | AT (3 times per week for 4 weeks, n = 51), plus CM ✝ | Sham acupuncture (3 times per week for 4 weeks, n = 39), plus CM ✝ | BL18, BL20, BL23, KI3, LV3, SP6, LI4, CV17, CV12, DU24, DU20, EM2 | (1) ADHD-RS score (2) Visual CPT score | (1) Total: MD −1.06 [−6.28, 4.16], NS; hyperactivity–impulsivity: MD 0.88 [−1.94, 3.70], NS; inattention: MD −1.95 [−4.90, 1.00], NS (2) Correct hit: MD 3.24 [−3.05, 9.53], NS; omission error: MD −4.30 [−7.68, −0.92], p = 0.01; commission error: MD 1.06 [−3.65, 5.77], NS; reaction time: MD −24.06 [−88.96, 40.84], NS |
| Hong 2016 [27] | 93 78/15 | 10.9/11.1 n.r. | AT (twice per week for 6 weeks, n = 46) | Waitlist (n = 47) | DU20, EM1, LI4 (bil), LI11 (bil), SP6 (bil), LV3 (bil) | (1) ADHD-RS score ‡ (2) PSQ score ‡ (3) IOWA-RS score ‡ (4) CGI-S score ‡ (5) FAIR score ‡ (6) CBCL score ‡ (7) CNT score ‡ (8) CPT ‡ (9) CCPT ‡ | (1) Total: NS; Hyperactivity–impulsivity: NS; inattention: NS (2–3) NS (4) p = 0.012 (5) P: NS; Q: p = 0.022; C: NS (6) Total: NS; ADHD subscale: NS; external subscale: NS (7) Digit span test: forward: NS, backward: p = 0.027; visual span test: forward: NS, backward: p = 0.03; verbal learning test: p = 0.007 (8) Auditory—correct hit: NS; omission error: NS; commission error: NS; reaction time: p = 0.011; visual—correct hit: NS; omission error: NS; commission error: NS; reaction time: p = 0.004 (9) Auditory: Correct hit: NS, Omission error: NS, Commission error 1: NS, Commission error 2: NS, Reaction time: NS; Visual: Correct hit: NS, Omission error: NS, Commission error 1: NS, Commission error 2: NS, Reaction time: NS |
| Study ID | AEs |
|---|---|
| Meng 2012 [14] | n.r. |
| Chen 2012 [15] | Loss of appetite (AT, 2; CM, 7), headache (AT,1; CM, 1), insomnia (AT, 1; CM, 5), abdominal pain (CM, 2) |
| Tse 2016 [16] | n.r. |
| Yu 2021 [17] | n.r. |
| Zhang 2019 [18] | Vomiting, hallucinations, agitation, hyperreflexia, muscle twitches, convulsions, euphoria, tremor, confusion, delirium, sweating, flushing, headache, high fever, tachycardia, palpitations, hypertension, mydriasis, arrhythmia, dry mouth, etc. (AT/CM: n = 5/6) n.r. in details |
| Liu 2013 [19] | Nausea, dry mouth, constipation, loss of appetite, etc. (n = 15) Not differentiated according to intervention |
| Huang 2015 [20] | n.r. |
| Ji 2018 [21] | n.r. |
| Zhou 2013 [22] | n.r. |
| Wei 2011 [23] | n.r. |
| Che 2017 [24] | n.r. |
| Zheng 2022 [25] | Loss of appetite (CM, 6), insomnia (CM, 4), headache (CM, 3), abdominal pain (CM, 1), muscle twitches (CM, 1) |
| Moharreri 2018 [26] | None |
| Hong 2016 [27] | Mild headaches (AT, 3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ang, L.; Kim, J.T.; Kim, K.; Lee, H.W.; Choi, J.-Y.; Kim, E.; Lee, M.S. Acupuncture for Treating Attention Deficit Hyperactivity Disorder in Children: A Systematic Review and Meta-Analysis. Medicina 2023, 59, 392. https://doi.org/10.3390/medicina59020392
Ang L, Kim JT, Kim K, Lee HW, Choi J-Y, Kim E, Lee MS. Acupuncture for Treating Attention Deficit Hyperactivity Disorder in Children: A Systematic Review and Meta-Analysis. Medicina. 2023; 59(2):392. https://doi.org/10.3390/medicina59020392
Chicago/Turabian StyleAng, Lin, Jung Tae Kim, Kibong Kim, Hye Won Lee, Jun-Yong Choi, Eunseop Kim, and Myeong Soo Lee. 2023. "Acupuncture for Treating Attention Deficit Hyperactivity Disorder in Children: A Systematic Review and Meta-Analysis" Medicina 59, no. 2: 392. https://doi.org/10.3390/medicina59020392
APA StyleAng, L., Kim, J. T., Kim, K., Lee, H. W., Choi, J.-Y., Kim, E., & Lee, M. S. (2023). Acupuncture for Treating Attention Deficit Hyperactivity Disorder in Children: A Systematic Review and Meta-Analysis. Medicina, 59(2), 392. https://doi.org/10.3390/medicina59020392








