Tongue Base Ectopic Thyroid Tissue—Is It a Rare Encounter?
Abstract
1. Introduction
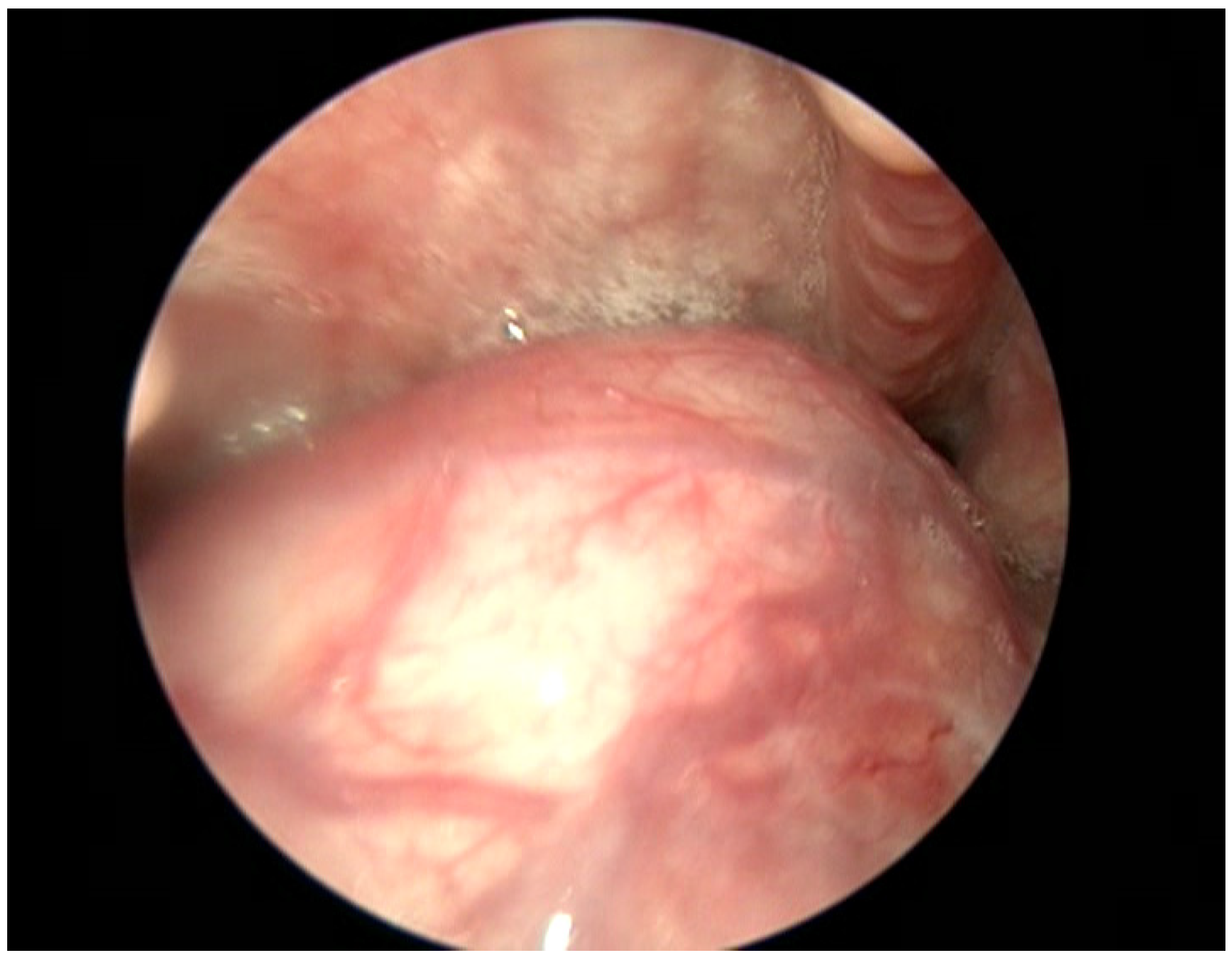
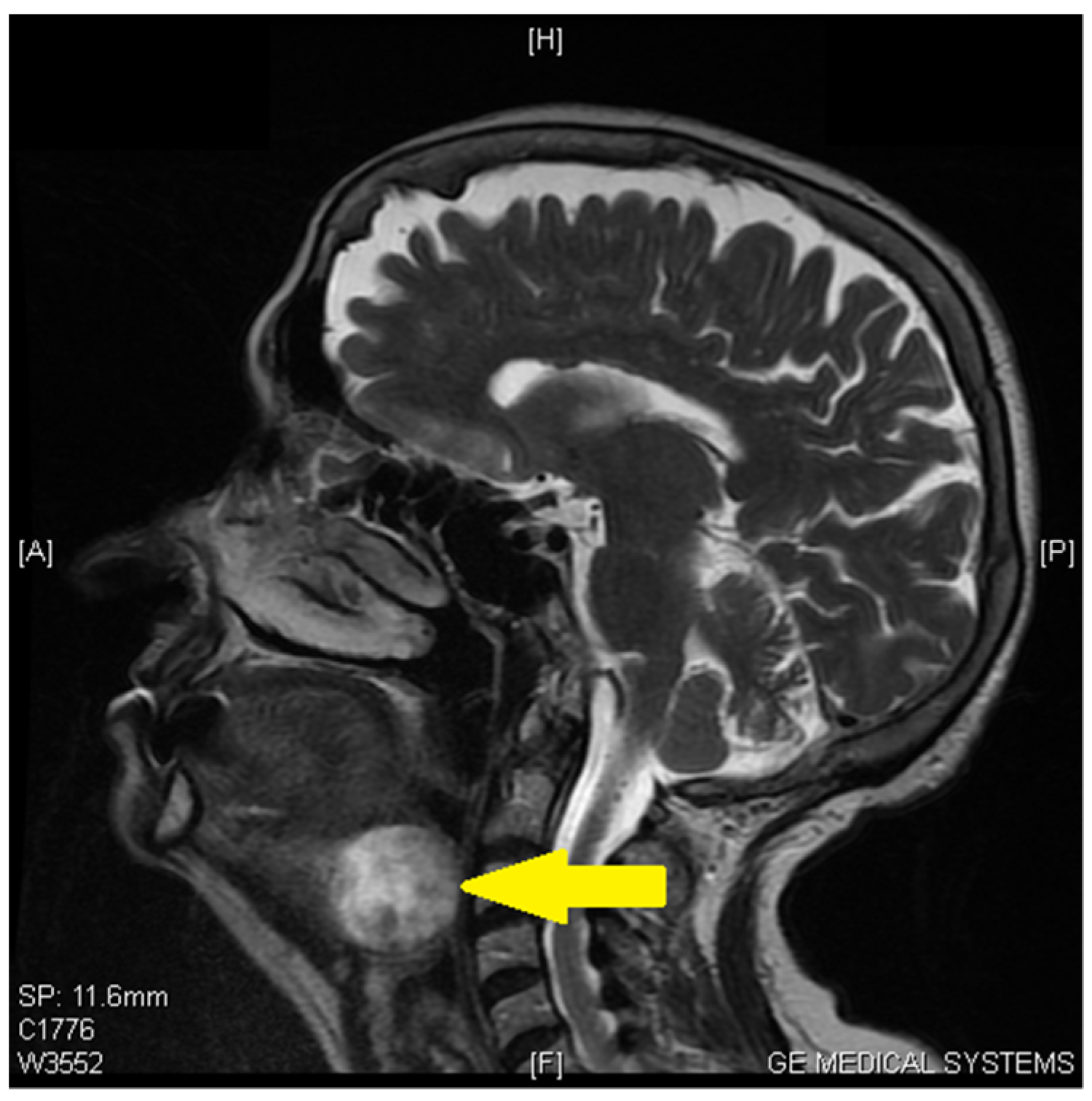
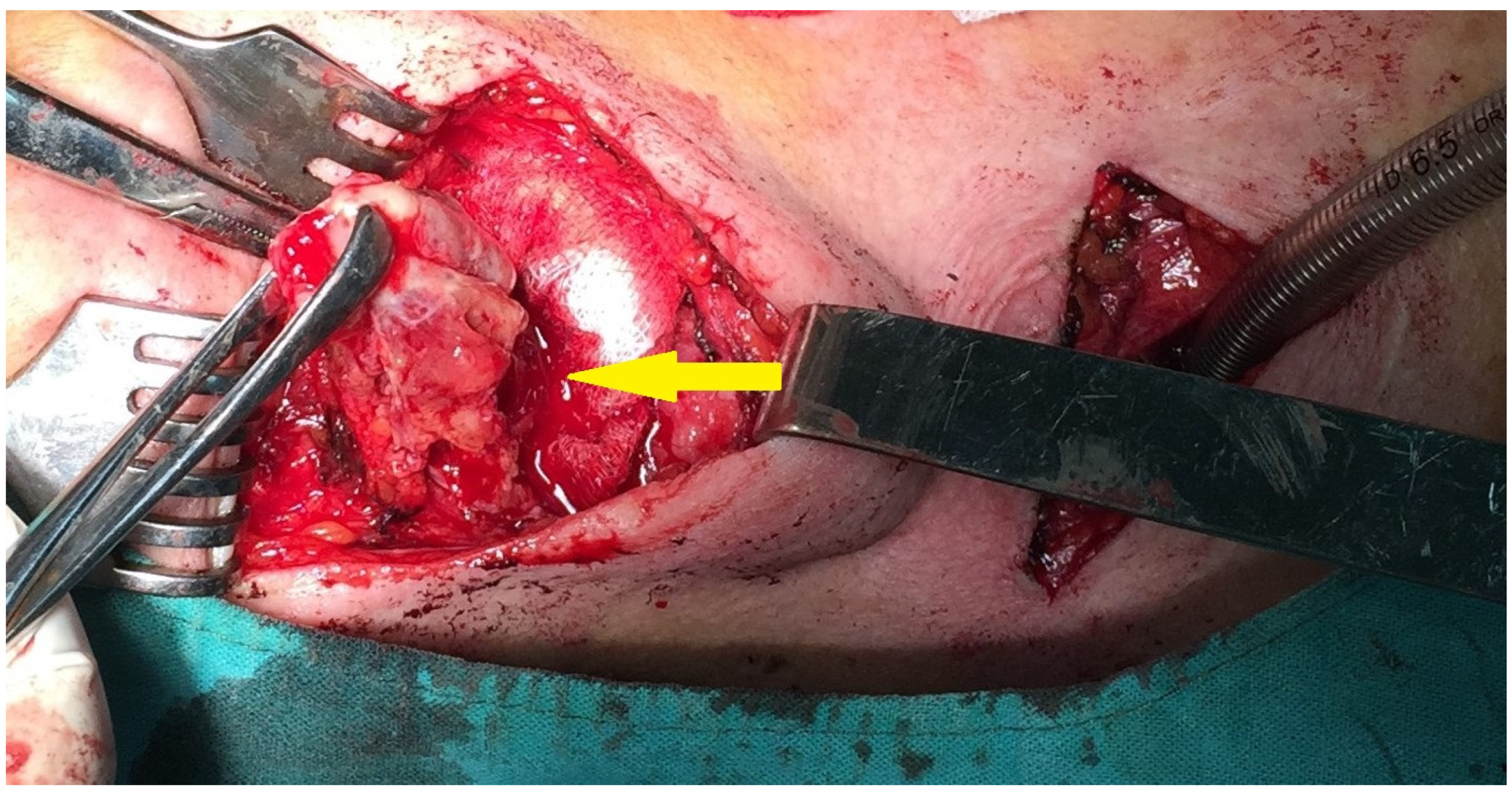
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Babazade, F.; Mortazavi, H.; Jalalian, H.; Shahvali, E. Thyroid tissue as a submandibular mass: A case report. J. Oral Sci. 2009, 51, 655–657. [Google Scholar] [CrossRef] [PubMed]
- Di Benedetto, V. Ectopic thyroid gland in the submandibular region simulating a thyroglossal duct cyst: A case report. J. Pediatr. Surg. 1997, 32, 1745–1746. [Google Scholar] [CrossRef] [PubMed]
- Noussios, G.; Anagnostis, P.; Goulis, D.G.; Lappas, D.; Natsis, K. Ectopic thyroid tissue: Anatomical, clinical, and surgical implications of a rare entity. Eur. J. Endocrinol. 2011, 165, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Toso, A.; Colombani, F.; Averono, G.; Aluffi, P.; Pia, F. Lingual thyroid causing dysphagia and dyspnoea. Case reports and review of the literature. ACTA Otorhinolaryngol. 2009, 29, 213–217. [Google Scholar]
- Adelchi, C.; Mara, P.; Melissa, L.; De Stefano, A.; Cesare, M. Ectopic thyroid tissue in the head and neck: A case series. BMC Res. Notes 2014, 7, 790. [Google Scholar] [CrossRef]
- Saito, M.; Banno, H.; Ito, Y.; Ido, M.; Goto, M.; Ando, T.; Kousaka, J.; Mouri, Y.; Fujii, K.; Imai, T.; et al. Case report: Surgical management of symptomatic pretracheal thyroid gland in a patient with dual ectopic thyroid. Thyroid. Res. 2022, 15, 23. [Google Scholar] [CrossRef]
- Choudhury, B.K.; Saikia, U.K.; Sarma, D.; Saikia, M.; Choudhury, S.D.; Barua, S.; Dewri, S. Dual ectopic thyroid with normally located thyroid: A case report. J. Thyroid. Res. 2011, 2011, 159703. [Google Scholar] [CrossRef]
- Eli, S.U.; Marnane, C.; Peter, R.; Winter, S. Ectopic, submandibular thyroid causing hyperthyroidism. J. Laryngol. Otol. 2011, 125, 1091–1093. [Google Scholar] [CrossRef]
- Mace, A.T.M.; Mclaughlin, I.; Gibson, I.W.; Clark, L.J. Benign ectopic submandibular thyroid with a normotopic multinodular goitre. J. Laryngol. Otol. 2003, 117, 739–740. [Google Scholar] [CrossRef]
- Alderson, D.J.; Lannigan, F.J. Lingual thyroid presenting after previous thyroglossal cyst excision. J. Laryngol. Otol. 1994, 108, 341–343. [Google Scholar] [CrossRef]
- Alanazi, S.M.; Limaiem, F. Ectopic Thyroid. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar] [PubMed]
- DeFelice, M.; Lauro, R. Thyroid development and its disorders: Genetics and molecular mechanisms. Endocr. Rev. 2004, 25, 722–746. [Google Scholar] [CrossRef]
- Gallo, A.; Leonetti, F.; Torri, E.; Manciocco, V.; Simonelli, M.; De Vincentiis, M. Ectopic lingual thyroid as unusual cause of severe dysphagia. Dysphagia 2001, 16, 220–223. [Google Scholar] [CrossRef]
- Cassol, C.A.; Noria, D.; Asa, S. Ectopic thyroid tissue within the gall bladder: Case report and brief review of the literature. Endocr. Pathol. 2010, 21, 263–265. [Google Scholar] [CrossRef]
- Shuno, Y.; Kobayashi, T.; Morita, K.; Shimizu, S.; Nishio, Y.; Ito, A.; Kobayashi, K.; Kawahara, M.; Teruya, M. Ectopic thyroid in the adrenal gland presenting as cystic lesion. Surgery 2006, 139, 580–582. [Google Scholar] [CrossRef]
- Nettore, I.C.; Cacace, V.; De Fusco, C.; Colao, A.; Macchia, P.E. The molecular causes of thyroid dysgenesis: A systematic review. J. Endocrinol. Investig. 2013, 36, 654–664. [Google Scholar]
- Abu-Khudir, R.; Paquette, J.; Lefort, A.; Libert, F.; Chanoine, J.P.; Vassart, G.; Deladoëy, J. Transcriptome, methylome and genomic variations analysis of ectopic thyroid glands. PLoS ONE 2010, 5, e13420. [Google Scholar] [CrossRef]
- Kumar, R.; Sharma, S.; Marwah, A.; Moorthy, D.; Dhanwal, D.; Malhotra, A. Ectopic goiter masquerading as submandibular gland swelling: A case report and review of the literature. Clin. Nucl. Med. 2001, 26, 306–309. [Google Scholar] [CrossRef]
- Kousta, E.; Konstantinidis, K.; Michalakis, C.; Vorias, M.; Sambalis, G.; Georgiou, M.; Theodoropoulos, G.E. Ectopic thyroid tissue in the lower neck with a coexisting normally located multinodular goiter and brief literature review. Hormones 2005, 4, 231–234. [Google Scholar] [CrossRef]
- Bersaneti, J.A.; Silva, R.; Ramos, P.; Matsushita, M.; Souto, L. Ectopic thyroid presenting as a submandibular mass. Head Neck Pathol. 2011, 5, 63–66. [Google Scholar] [CrossRef]
- Sood, A.; Sood, V.; Sharma, D.R.; Seam, R.K.; Kumar, R. Thyroid scintigraphy in detecting dual ectopic thyroid: A review. Eur. J. Nucl. Med. 2008, 35, 843–846. [Google Scholar] [CrossRef]
- Jha, P.S.; Rote-Kaginalkar, V.; Titare, P.; Jadhav, M.B. Hemiagenesisofthyroidwithdualthyroidectopia:Ararecasereport. Indian J. Radiol. Imaging 2018, 28, 4–17. [Google Scholar]
- Ma, A.; Liu, H. Ectopicthyroidofthepancreas:Acasereportandliteraturereview. Medicine 2017, 96, e8707. [Google Scholar] [CrossRef] [PubMed]
- Massine, R.E.; Durning, S.J.; Koroscil, T.M. Lingual thyroid carcinoma: A case report and review of the literature. Thyroid 2001, 11, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Eyüboğlu, E.; Kapan, M.; Ipek, T.; Ersan, Y.; Oz, F. Ectopic thyroid in the abdomen: Report of a case. Surg. Today 1999, 29, 472–474. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, N.; Bley, T.; Altehoefer, C.; Högerle, S.; Langer, M. Ectopic thyroid gland in the porta hepatis and lingua. Thyroid 2003, 13, 503–507. [Google Scholar] [CrossRef]
- Takahashi, T.; Ishikura, H.; Kato, H.; Tanabe, T.; Yoshiki, T. Ectopic thyroid follicles in the submucosa of the duodenum. Virchows Arch. A Pathol. Anat. Histopathol. 1991, 418, 547–550. [Google Scholar] [CrossRef]
- Wagner, H.; Auw-Hädrich, C.; Werner, M.; Reinhard, T. Ectopic thyroid tissue in the iris: A case report. BMC Ophthalmol. 2021, 21, 314. [Google Scholar] [CrossRef]
- Kondo, T.; Katoh, R.; Omata, K.; Oyama, T.; Yagawa, A.; Kawaoi, A. Incidentally detected liver metastasis of well-differentiated follicular carcinoma of the thyroid, mimicking ectopic thyroid. Pathol. Int. 2000, 50, 509–513. [Google Scholar] [CrossRef]
- Campora, M.; Antonelli, C.T.; Mastracci, L.; Pigozzi, S.; Grillo, F. A Never Ending Journey: Ectopic Thyroid. Int. J. Surg. Pathol. 2017, 25, 241–242. [Google Scholar] [CrossRef]
- Romero-Rojas, A.; Bella-Cueto, M.R.; Meza-Cabrera, I.A.; Cabezuelo-Hernández, A.; García-Rojo, D.; Vargas-Uricoechea, H.; Cameselle-Teijeiro, J. Ectopic thyroid tissue in the adrenal gland: A report of two cases with pathogenetic implications. Thyroid 2013, 23, 1644–1650. [Google Scholar] [CrossRef]
- Sarău, C.A.; Poenaru, M.; Balica, N.C.; Baderca, F. Rare sinonasal lesions. Rom. J. Morphol. Embryol. 2017, 58, 1541–1547. [Google Scholar]
- Hazarika, P.; Siddiqui, S.A.; Pujary, K.; Shah, P.; Nayak, D.R.; Balakrishnan, R. Dual ectopic thyroid: A report of two cases. J. Laryngol. Otol. 1998, 112, 393–395. [Google Scholar] [CrossRef]
- Kamparoudi, P.; Paliouras, D.; Gogakos, A.S.; Rallis, T.; Schizas, N.C.; Lazopoulos, A.; Chatzinikolaou, F.; Sarafis, P.; Serchan, P.; Katsikogiannis, N.; et al. Percutaneous tracheostomy—Beware of the thyroidea-ima artery. Ann. Transl. Med. 2016, 4, 449. [Google Scholar] [CrossRef]
- Gwilym, S.; Cooney, A. Acute fatal haemorrhage during percutaneous dilatational tracheostomy. BJA Br. J. Anaesth. 2004, 92, 298. [Google Scholar] [CrossRef]
- Yurasakpong, L.; Nantasenamat, C.; Janta, S.; Eiamratchanee, P.; Coey, J.; Chaiyamoon, A.; Kruepunga, N.; Senarai, T.; Langer, M.F.; Meemon, K.; et al. The decreasing prevalence of the thyroid ima artery: A systematic review and machine learning assisted meta-analysis. Ann. Anat. 2022, 239, 151803. [Google Scholar] [CrossRef]
- Prasad, K.C.; Bhat, V. Surgical management of lingual thyroid: A report of four cases. J. Oral Maxillofac. Surg. 2000, 58, 223–227. [Google Scholar] [CrossRef]
- Wu, Z.X.; Zheng, L.W.; Dong, Y.J.; Li, Z.B.; Zhang, W.F.; Zhao, Y.F. Modified approach for lingual thyroid transposition: Report of two cases. Thyroid 2008, 18, 465–468. [Google Scholar] [CrossRef]
- Guerra, G.; Cinelli, M.; Mesolella, M.; Tafuri, D.; Rocca, A.; Amato, B.; Rengo, S.; Testa, D. Morphological, diagnostic and surgical features of ectopic thyroid gland: A review of literature. Int. J. Surg. 2014, 12, S3–S11. [Google Scholar] [CrossRef]
- Elechi, H.A. Hypothyroidism following sistrunk procedure: Thyroglossal duct cyst or ectopic thyroid? Afr. J. Paediatr. Surg. 2021, 18, 231–234. [Google Scholar] [CrossRef]
- Lim, L.X.; Kwok, G.T.; Wong, E.; Morgan, G.J. Dual thyroid ectopia with submental thyroid excision using Sistrunk procedure: A case report. Int. J. Surg. Case Rep. 2021, 82, 105909. [Google Scholar] [CrossRef]
- Kim, C.H.; Byeon, H.K.; Shin, Y.S.; Koh, Y.W.; Choi, E.C. Robot-assisted Sistrunk operation via a retroauricular approach for thyroglossal duct cyst. Head Neck 2014, 36, 456–458. [Google Scholar] [CrossRef] [PubMed]
- Poon, H.; Li, C.; Gao, W.; Ren, H.; Lim, C.M. Evolution of robotic systems for transoral head and neck surgery. Oral Oncol. 2018, 87, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Atiyeh, B.S.; Abdelnour, A.; Haddad, F.F.; Ahmad, H. Lingual thyroid: Tongue-splitting incision for transoral excision. J. Laryngol. Otol. 1995, 109, 520–524. [Google Scholar] [CrossRef] [PubMed]
- Vairaktaris, E.; Semergidis, T.; Christopoulou, P.; Papadogeorgakis, N.; Martis, C. Lingual thyroid: A new surgical approach—A case report. J. Craniomaxillofac. Surg. 1994, 22, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Prisman, E.; Patsias, A.; Genden, E.M. Transoral robotic excision of ectopic lingual thyroid: Case series and literature review. Head Neck 2015, 37, E88–E91. [Google Scholar] [CrossRef]
- Vincent, A.; Jategaonkar, A.; Kadakia, S.; Ducic, Y. TORS excision of lingual thyroid carcinoma: Technique and systematic review. Am. J. Otolaryngol. 2019, 40, 435–439. [Google Scholar] [CrossRef]
- Huang, H.; Lin, Y.H. Lingual thyroid with severe hypothyroidism: A case report. Medicine 2021, 100, e27612. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Constantin, B.N.; Marina, T.C.; Eugen, S.H.; Ileana, E.; Adrian, G. Tongue Base Ectopic Thyroid Tissue—Is It a Rare Encounter? Medicina 2023, 59, 313. https://doi.org/10.3390/medicina59020313
Constantin BN, Marina TC, Eugen SH, Ileana E, Adrian G. Tongue Base Ectopic Thyroid Tissue—Is It a Rare Encounter? Medicina. 2023; 59(2):313. https://doi.org/10.3390/medicina59020313
Chicago/Turabian StyleConstantin, Balica Nicolae, Trandafir Cornelia Marina, Stefanescu Horatiu Eugen, Enatescu Ileana, and Gluhovschi Adrian. 2023. "Tongue Base Ectopic Thyroid Tissue—Is It a Rare Encounter?" Medicina 59, no. 2: 313. https://doi.org/10.3390/medicina59020313
APA StyleConstantin, B. N., Marina, T. C., Eugen, S. H., Ileana, E., & Adrian, G. (2023). Tongue Base Ectopic Thyroid Tissue—Is It a Rare Encounter? Medicina, 59(2), 313. https://doi.org/10.3390/medicina59020313






