Mini-Implants Retaining Removable Partial Dentures in Subjects without Posterior Teeth: A 5-Year Prospective Study Comparing the Maxilla and the Mandible
Abstract
1. Introduction
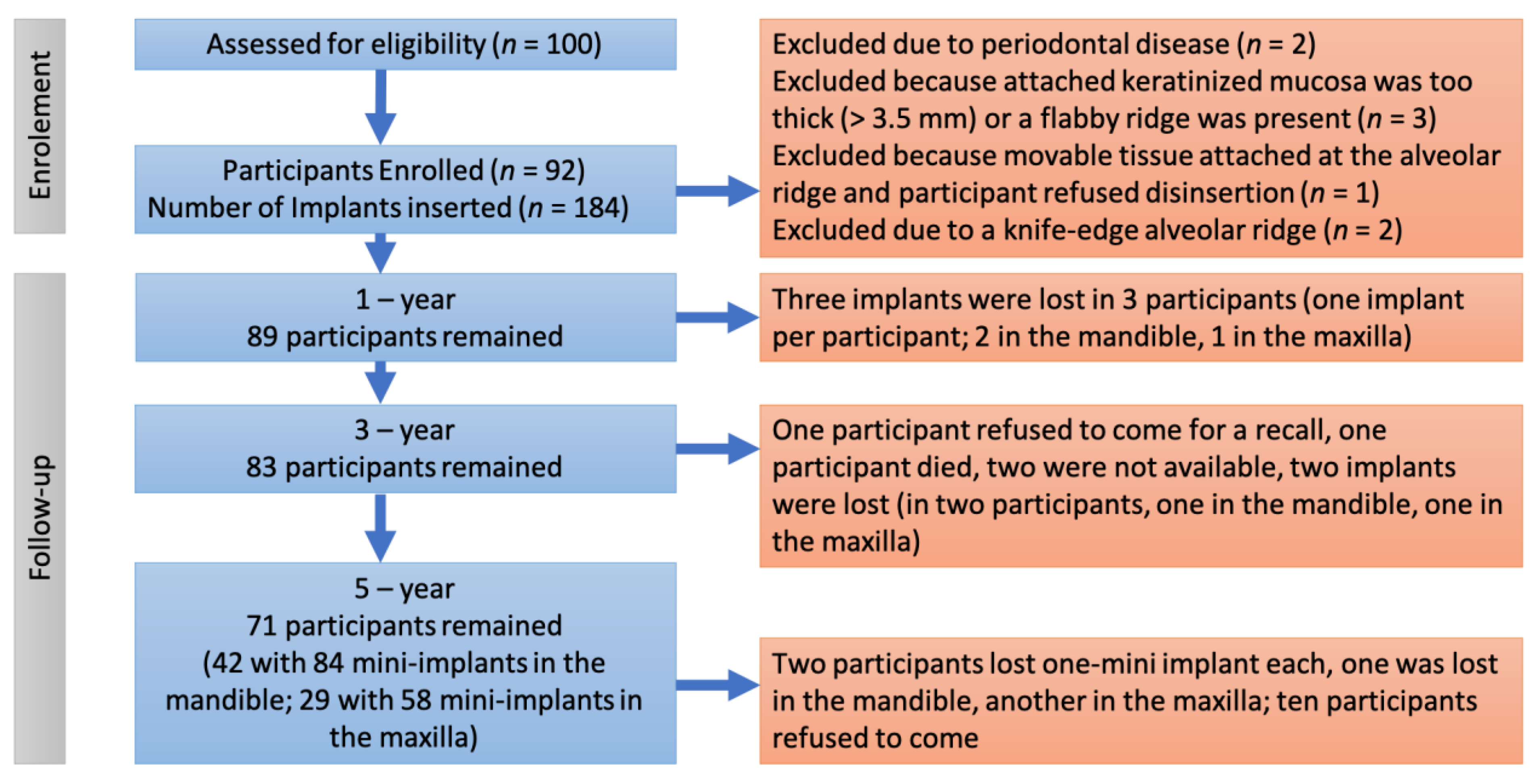
2. Materials and Methods
2.1. Study Design
2.2. Sample Size
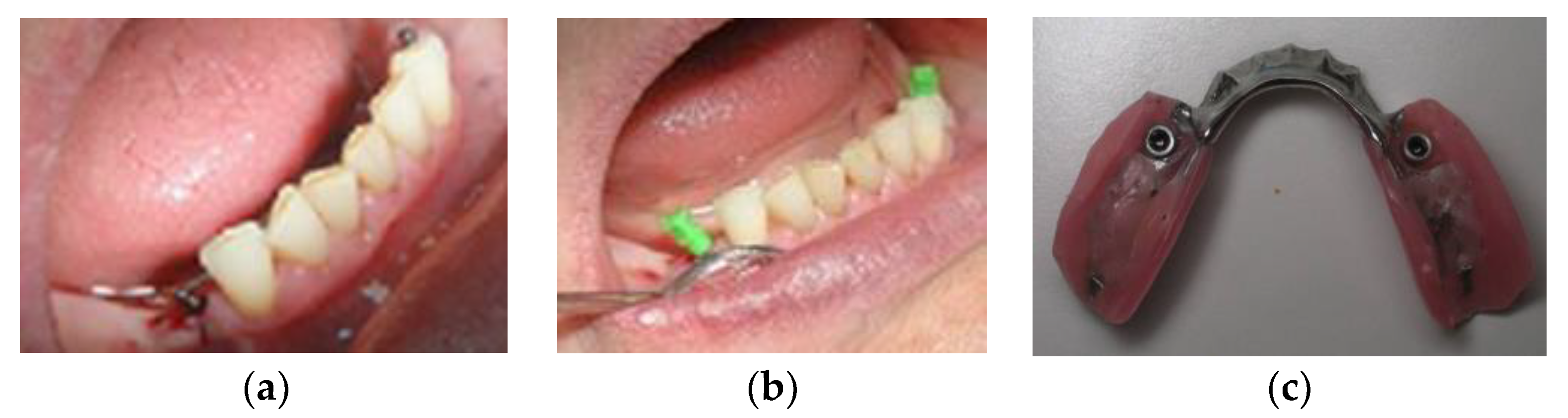
2.3. Surgical Protocol
2.4. Prosthodontic Protocol
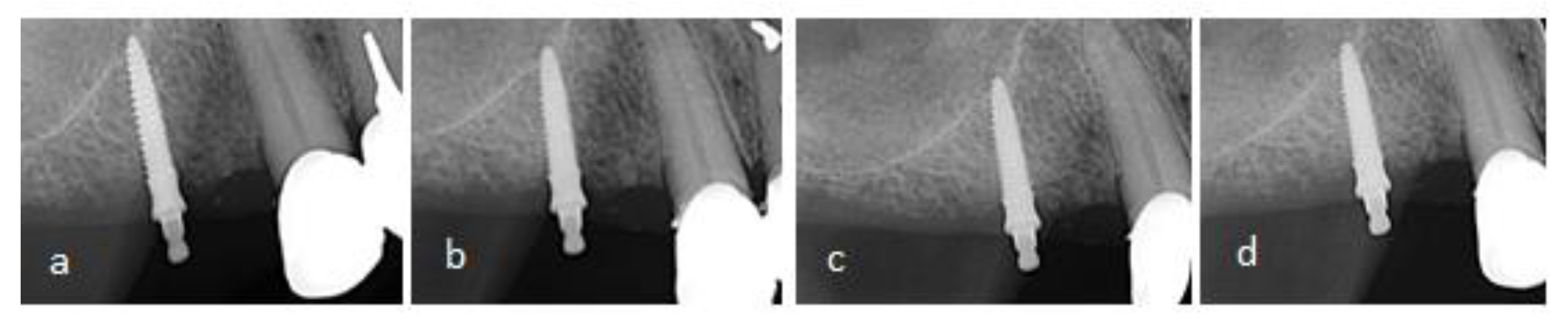
2.5. Clinical and Radiographic Evaluation
2.6. Prosthodontic Maintenance
2.7. Statistical Analysis
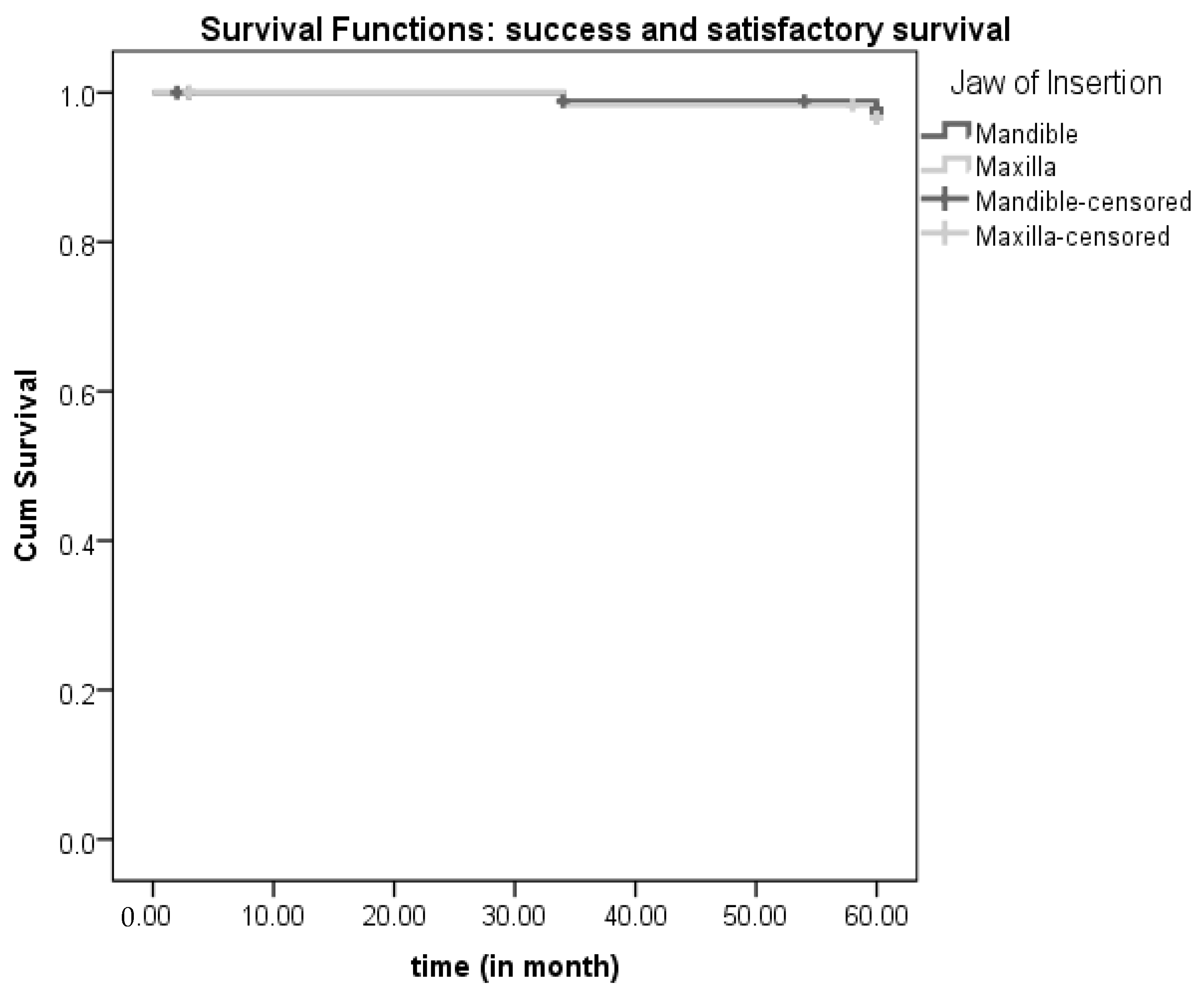
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peršić, S.; Kranjčić, J.; Pavičić, D.K.; Mikić, V.L.; Čelebić, A. Treatment Outcomes Based on Patients’ Self-Reported Measures after Receiving New Clasp or Precision Attachment-Retained Removable Partial Dentures. J. Prosthodont. 2017, 26, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.; Speksnijder, C.M.; Raghoebar, G.M.; Kerdijk, W.; Meijer, H.J.A.; Cune, M.S. Implant-Supported Mandibular Removable Partial Dentures: Functional, Clinical and Radiographical Parameters in Relation to Implant Position. Clin. Implant Dent. Relat. Res. 2017, 19, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Putra Wigianto, A.Y.; Goto, T.; Iwawaki, Y.; Ishida, Y.; Watanabe, M.; Ichikawa, T. Treatment Outcomes of Implant-Assisted Removable Partial Denture with Distal Extension Based on the Kennedy Classification and Attachment Type: A Systematic Review. Int. J. Implant Dent. 2021, 7, 111. [Google Scholar] [CrossRef]
- Mijiritsky, E. Implants in Conjunction with Removable Partial Dentures: A Literature Review. Implant Dent. 2007, 16, 146–154. [Google Scholar] [CrossRef]
- Kim, J.J. Revisiting the Removable Partial Denture. Dent. Clin. N. Am. 2019, 63, 263–278. [Google Scholar] [CrossRef]
- Peršić, S.; Čelebić, A. Influence of Different Prosthodontic Rehabilitation Options on Oral Health-Related Quality of Life, Orofacial Esthetics and Chewing Function Based on Patient-Reported Outcomes. Qual. Life Res. 2015, 24, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Petricevic, N.; Celebic, A.; Rener-Sitar, K. A 3-Year Longitudinal Study of Quality-of-Life Outcomes of Elderly Patients with Implant- and Tooth-Supported Fixed Partial Dentures in Posterior Dental Regions. Gerodontology 2012, 29, e956–e963. [Google Scholar] [CrossRef] [PubMed]
- Mousa, M.A.; Abdullah, J.Y.; Jamayet, N.B.; El-Anwar, M.I.; Ganji, K.K.; Alam, M.K.; Husein, A. Biomechanics in Removable Partial Dentures: A Literature Review of FEA-Based Studies. BioMed Res. Int. 2021, 2021, 5699962. [Google Scholar] [CrossRef]
- Shahmiri, R.A.; Atieh, M.A. Mandibular Kennedy Class I Implant-Tooth-Borne Removable Partial Denture: A Systematic Review. J. Oral Rehabil. 2010, 37, 225–234. [Google Scholar] [CrossRef]
- Zancopé, K.; Abrão, G.M.; Karam, F.K.; Neves, F.D. Placement of a Distal Implant to Convert a Mandibular Removable Kennedy Class I to an Implant-Supported Partial Removable Class III Dental Prosthesis: A Systematic Review. J. Prosthet. Dent. 2015, 113, 528–533.e3. [Google Scholar] [CrossRef]
- Molinero-Mourelle, P.; Bischof, F.; Yilmaz, B.; Schimmel, M.; Abou-Ayash, S. Clinical Performance of Tooth Implant-Supported Removable Partial Dentures: A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2022, 26, 6003–6014. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Lee, J.-Y.; Shin, S.-W.; Kim, H.-J. Effect of Conversion to Implant-Assisted Removable Partial Denture in Patients with Mandibular Kennedy Classification Ⅰ: A Systematic Review and Meta-Analysis. Clin. Oral Implants Res. 2020, 31, 360–373. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.; Heo, S.-J.; Koak, J.-Y.; Kim, S.-K. Clinical Outcomes of Implant-Assisted Removable Partial Dentures According to Implant Strategic Position. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2022; in press. [Google Scholar] [CrossRef]
- Jensen, C.; Raghoebar, G.M.; Kerdijk, W.; Meijer, H.J.A.; Cune, M.S. Implant-Supported Mandibular Removable Partial Dentures; Patient-Based Outcome Measures in Relation to Implant Position. J. Dent. 2016, 55, 92–98. [Google Scholar] [CrossRef]
- Jung, R.E.; Al-Nawas, B.; Araujo, M.; Avila-Ortiz, G.; Barter, S.; Brodala, N.; Chappuis, V.; Chen, B.; De Souza, A.; Almeida, R.F.; et al. Group 1 ITI Consensus Report: The Influence of Implant Length and Design and Medications on Clinical and Patient-Reported Outcomes. Clin. Oral Implants Res. 2018, 29 (Suppl. S16), 69–77. [Google Scholar] [CrossRef] [PubMed]
- Elsyad, M.A.; Gebreel, A.A.; Fouad, M.M.; Elshoukouki, A.H. The Clinical and Radiographic Outcome of Immediately Loaded Mini Implants Supporting a Mandibular Overdenture. A 3-Year Prospective Study. J. Oral Rehabil. 2011, 38, 827–834. [Google Scholar] [CrossRef]
- Elsyad, M.A. Patient Satisfaction and Prosthetic Aspects with Mini-Implants Retained Mandibular Overdentures. A 5-Year Prospective Study. Clin. Oral Implants Res. 2016, 27, 926–933. [Google Scholar] [CrossRef]
- Chatrattanarak, W.; Aunmeungtong, W.; Khongkhunthian, P. Comparative Clinical Study of Conventional Dental Implant and Mini Dental Implant-Retained Mandibular Overdenture: A 5- to 8-Year Prospective Clinical Outcomes in a Previous Randomized Clinical Trial. Clin. Implant Dent. Relat. Res. 2022, 24, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Topić, J.; Poljak-Guberina, R.; Persic-Kirsic, S.; Kovacic, I.; Petricevic, N.; Popovac, A.; Čelebić, A. Adaptation to New Dentures and 5 Years of Clinical Use: A Comparison between Complete Denture and Mini-Implant Mandibular Overdenture Patients Based on Oral Health-Related Quality of Life (OHRQoL) and Orofacial Esthetics. Acta Stomatol. Croat. 2022, 56, 132–142. [Google Scholar] [CrossRef]
- Kovačić, I.; Peršić, S.; Kranjčić, J.; Čelebić, A. A Cohort Study on Short Mini-Implants for Mandibular Overdentures Compared to Those of Standard Length. Clin. Oral Implants Res. 2020, 31, 121–132. [Google Scholar] [CrossRef]
- Borges, G.A.; Codello, D.J.; Del Rio Silva, L.; Dini, C.; Barão, V.A.R.; Mesquita, M.F. Factors and Clinical Outcomes for Standard and Mini-Implants Retaining Mandibular Overdentures: A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Enkling, N.; Moazzin, R.; Geers, G.; Kokoschka, S.; Abou-Ayash, S.; Schimmel, M. Clinical Outcomes and Bone-Level Alterations around One-Piece Mini Dental Implants Retaining Mandibular Overdentures: 5-Year Follow-up of a Prospective Cohort Study. Clin. Oral Implants Res. 2020, 31, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Peršić, S.; Ćelić, R.; Vojvodić, D.; Petričević, N.; Kranjčić, J.; Zlatarić, D.K.; Čelebić, A. Oral Health-Related Quality of Life in Different Types of Mandibular Implant Overdentures in Function Longer Than 3 Years. Int. J. Prosthodont. 2016, 29, 28–30. [Google Scholar] [CrossRef] [PubMed]
- Ćorić, A.; Kovačić, I.; Kiršić, S.P.; Čelebić, A. Are Mini Dental Implants Suitable for Support of Crowns or Small Bridges in the Mandibular Incisor Region? A 5-Year Longitudinal Study. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2022, 80, 1811–1826. [Google Scholar] [CrossRef] [PubMed]
- Van Doorne, L.; De Kock, L.; De Moor, A.; Shtino, R.; Bronkhorst, E.; Meijer, G.; De Bruyn, H. Flaplessly Placed 2.4-Mm Mini-Implants for Maxillary Overdentures: A Prospective Multicentre Clinical Cohort Study. Int. J. Oral Maxillofac. Surg. 2020, 49, 384–391. [Google Scholar] [CrossRef]
- ELsyad, M.A.; Ghoneem, N.E.; El-Sharkawy, H. Marginal Bone Loss around Unsplinted Mini-Implants Supporting Maxillary Overdentures: A Preliminary Comparative Study between Partial and Full Palatal Coverage. Quintessence Int. 2013, 44, 45–52. [Google Scholar] [CrossRef]
- Rungsiyakull, P.; Kujarearntaworn, K.; Khongkhunthian, P.; Swain, M.; Rungsiyakull, C. Effect of the Location of Dental Mini-Implants on Strain Distribution under Mandibular Kennedy Class I Implant-Retained Removable Partial Dentures. Int. J. Dent. 2021, 2021, 6688521. [Google Scholar] [CrossRef]
- Jia-Mahasap, W.; Rungsiyakull, C.; Bumrungsiri, W.; Sirisereephap, N.; Rungsiyakull, P. Effect of Number and Location on Stress Distribution of Mini Dental Implant-Assisted Mandibular Kennedy Class I Removable Partial Denture: Three-Dimensional Finite Element Analysis. Int. J. Dent. 2022, 2022, 4825177. [Google Scholar] [CrossRef] [PubMed]
- Pisani, M.X.; Presotto, A.G.C.; Mesquita, M.F.; Barão, V.A.R.; Kemmoku, D.T.; Del Bel Cury, A.A. Biomechanical Behavior of 2-Implant– and Single-Implant–Retained Mandibular Overdentures with Conventional or Mini Implants. J. Prosthet. Dent. 2018, 120, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Al Jaghsi, A.; Mundt, T. Upgrading Removable Denture Design by Using Strategic Implants: A Case Report. Ann. Anat. Anat. Anz. 2023, 245, 152002. [Google Scholar] [CrossRef] [PubMed]
- Disha, V.; Čelebić, A.; Rener-Sitar, K.; Kovačić, I.; Filipović Zore, I.; Peršić, S. Mini Dental Implant-Retained Removable Partial Dentures: Treatment Effect Size and 6-Months Follow-Up. Acta Stomatol. Croat. 2018, 52, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Mundt, T.; Schwahn, C.; Heinemann, F.; Schimmel, M.; Lucas, C.; Al Jaghsi, A. Stabilizing Removable Partial Dentures by Immediate or Delayed Loading of Mini-Implants: Chewing Efficiency in a Randomized Controlled Clinical Trial. Int. J. Oral Maxillofac. Implants 2020, 35, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Threeburuth, W.; Aunmeungtong, W.; Khongkhunthian, P. Comparison of Immediate-Load Mini Dental Implants and Conventional-Size Dental Implants to Retain Mandibular Kennedy Class I Removable Partial Dentures: A Randomized Clinical Trial. Clin. Implant Dent. Relat. Res. 2018, 20, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Lemos, C.A.A.; Nunes, R.G.; Santiago-Júnior, J.F.; Marcela de Luna Gomes, J.; Oliveira Limirio, J.P.J.; Rosa, C.D.D.R.D.; Verri, F.R.; Pellizzer, E.P. Are Implant-Supported Removable Partial Dentures a Suitable Treatment for Partially Edentulous Patients? A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2021; in press. [Google Scholar] [CrossRef]
- Al Jaghsi, A.; Heinemann, F.; Biffar, R.; Mundt, T. Immediate versus Delayed Loading of Strategic Mini-Implants under Existing Removable Partial Dentures: Patient Satisfaction in a Multi-Center Randomized Clinical Trial. Clin. Oral Investig. 2021, 25, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Mundt, T.; Heinemann, F.; Müller, J.; Schwahn, C.; Al Jaghsi, A. Survival and Stability of Strategic Mini-Implants with Immediate or Delayed Loading under Removable Partial Dentures: A 3-Year Randomized Controlled Clinical Trial. Clin. Oral Investig. 2022, 1–13. [Google Scholar] [CrossRef]
- Palmer, R.; Palmer, P.; Howe, L. Complications and Maintenance. Br. Dent. J. 1999, 187, 653–658. [Google Scholar] [CrossRef]
- Müller, F.; Schimmel, M. Revised Success Criteria: A Vision to Meet Frailty and Dependency in Implant Patients. Int. J. Oral Maxillofac. Implants 2016, 31, 15. [Google Scholar]
- Hwang, D.; Wang, H.-L. Medical Contraindications to Implant Therapy: Part I: Absolute Contraindications. Implant Dent. 2006, 15, 353–360. [Google Scholar] [CrossRef]
- González-Valls, G.; Roca-Millan, E.; Céspedes-Sánchez, J.M.; González-Navarro, B.; Torrejon-Moya, A.; López-López, J. Narrow Diameter Dental Implants as an Alternative Treatment for Atrophic Alveolar Ridges: Systematic review and meta-analysis. Materials 2021, 14, 3234. [Google Scholar] [CrossRef]
- Marcello-Machado, R.M.; Faot, F.; Schuster, A.J.; Nascimento, G.G.; Del Bel Cury, A.A. Mini-Implants and Narrow Diameter Implants as Mandibular Overdenture Retainers: A Systematic Review and Meta-Analysis of Clinical and Radiographic Outcomes. J. Oral Rehabil. 2018, 45, 161–183. [Google Scholar] [CrossRef] [PubMed]
- Zygogiannis, K.; Wismeijer, D.; Parsa, A. A Pilot Study on Mandibular Overdentures Retained by Mini Dental Implants: Marginal Bone Level Changes and Patient-Based Ratings of Clinical Outcome. Int. J. Oral Maxillofac. Implants 2016, 31, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Mundt, T.; Schwahn, C.; Biffar, R.; Heinemann, F. Changes in Bone Levels Around Mini-Implants in Edentulous Arches. Int. J. Oral Maxillofac. Implants 2015, 30, 1149–1155. [Google Scholar] [CrossRef] [PubMed]
- Yoo, R.H.; Chuang, S.-K.; Erakat, M.S.; Weed, M.; Dodson, T.B. Changes in Crestal Bone Levels for Immediately Loaded Implants. Int. J. Oral Maxillofac. Implants 2006, 21, 253–261. [Google Scholar] [PubMed]
- Mombelli, A.; van Oosten, M.A.; Schurch, E.; Land, N.P. The Microbiota Associated with Successful or Failing Osseointegrated Titanium Implants. Oral Microbiol. Immunol. 1987, 2, 145–151. [Google Scholar] [CrossRef]
- Misch, C.E.; Perel, M.L.; Wang, H.-L.; Sammartino, G.; Galindo-Moreno, P.; Trisi, P.; Steigmann, M.; Rebaudi, A.; Palti, A.; Pikos, M.A.; et al. Implant Success, Survival, and Failure: The International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008, 17, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Morton, D.; Gallucci, G.; Lin, W.-S.; Pjetursson, B.; Polido, W.; Roehling, S.; Sailer, I.; Aghaloo, T.; Albera, H.; Bohner, L.; et al. Group 2 ITI Consensus Report: Prosthodontics and Implant Dentistry. Clin. Oral Implants Res. 2018, 29 (Suppl. S16), 215–223. [Google Scholar] [CrossRef]
- Kovačić, I.; Peršić, S.; Disha, V.; Rener-Sitar, K.; Čelebić, A. Short-Term Postoperative Pain and Swelling Associated with Mini and Standard-Size Implants in the Same Patients. Int. J. Prosthodont. 2018, 31, 117–119. [Google Scholar] [CrossRef]
- Kahn, A.; Masri, D.; Shalev, T.; Meir, H.; Sebaoun, A.; Chaushu, L. Patients’ Perception of Recovery after Dental Implant Placement. Medicina 2021, 57, 1111. [Google Scholar] [CrossRef]
- Bassi, F.; Schierano, G.; Lorenzetti, M.; Preti, G. Oral Conditions and Aptitude to Receive Implants in Patients with Removable Partial Denture: A Cross-Sectional Study: Part II Aptitude. J. Oral Rehabil. 1996, 23, 175–178. [Google Scholar] [CrossRef] [PubMed]
- Della Vecchia, M.P.; Leles, C.R.; Cunha, T.R.; Ribeiro, A.B.; Sorgini, D.B.; Muglia, V.A.; Reis, A.C.; Albuquerque, R.F.; de Souza, R.F. Mini-Implants for Mandibular Overdentures: Cost-Effectiveness Analysis alongside a Randomized Trial. JDR Clin. Transl. Res. 2018, 3, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, D.; Mascolo, A. The Mini Dental Implant in Fixed and Removable Prosthetics: A Review. J. Oral Implantol. 2011, 37 Spec No, 123–132. [Google Scholar] [CrossRef]
- Sato, M.; Suzuki, Y.; Kurihara, D.; Shimpo, H.; Ohkubo, C. Effect of Implant Support on Mandibular Distal Extension Removable Partial Dentures: Relationship between Denture Supporting Area and Stress Distribution. J. Prosthodont. Res. 2013, 57, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Oh, W.; Oh, T.-J.; Park, J. Impact of Implant Support on Mandibular Free-End Base Removable Partial Denture: Theoretical Study. Clin. Oral Implants Res. 2016, 27, e87-90. [Google Scholar] [CrossRef] [PubMed]
- Cunha, L.D.A.P.; Pellizzer, E.P.; Verri, F.R.; Pereira, J.A. Evaluation of the Influence of Location of Osseointegrated Implants Associated with Mandibular Removable Partial Dentures. Implant Dent. 2008, 17, 278–287. [Google Scholar] [CrossRef]
- Jensen, C.; Ross, J.; Feenstra, T.L.; Raghoebar, G.M.; Speksnijder, C.; Meijer, H.J.A.; Cune, M.S. Cost-Effectiveness of Implant-Supported Mandibular Removable Partial Dentures. Clin. Oral Implants Res. 2017, 28, 594–601. [Google Scholar] [CrossRef]
- ELsyad, M.A.; Omran, A.O.; Fouad, M.M. Strains Around Abutment Teeth with Different Attachments Used for Implant-Assisted Distal Extension Partial Overdentures: An In Vitro Study. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2017, 26, 42–47. [Google Scholar] [CrossRef]
- Elsyad, M.A.; Setta, F.A.; Khirallah, A.S. Strains around Distally Inclined Implants Retaining Mandibular Overdentures with Locator Attachments: An in Vitro Study. J. Adv. Prosthodont. 2016, 8, 116–124. [Google Scholar] [CrossRef]
- Ying, Z.; Gonda, T.; Maeda, Y. Influence of Attachment Height and Shape on Lateral Force Transmission in Implant Overdenture Treatment. Int. J. Prosthodont. 2017, 30, 586–591. [Google Scholar] [CrossRef]
- Jofré, J.; Hamada, T.; Nishimura, M.; Klattenhoff, C. The Effect of Maximum Bite Force on Marginal Bone Loss of Mini-Implants Supporting a Mandibular Overdenture: A Randomized Controlled Trial. Clin. Oral Implants Res. 2010, 21, 243–249. [Google Scholar] [CrossRef]
- Lemos, C.A.A.; Verri, F.R.; de Batista, V.E.S.; Júnior, J.F.S.; Mello, C.C.; Pellizzer, E.P. Complete Overdentures Retained by Mini Implants: A Systematic Review. J. Dent. 2017, 57, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Temizel, S.; Heinemann, F.; Dirk, C.; Bourauel, C.; Hasan, I. Clinical and Radiological Investigations of Mandibular Overdentures Supported by Conventional or Mini-Dental Implants: A 2-Year Prospective Follow-up Study. J. Prosthet. Dent. 2017, 117, 239–246.e2. [Google Scholar] [CrossRef] [PubMed]
- Schiegnitz, E.; Al-Nawas, B. Narrow-Diameter Implants: A Systematic Review and Meta-Analysis. Clin. Oral Implants Res. 2018, 29 (Suppl. S16), 21–40. [Google Scholar] [CrossRef]
- Jawad, S.; Clarke, P.T. Survival of Mini Dental Implants Used to Retain Mandibular Complete Overdentures: Systematic Review. Int. J. Oral Maxillofac. Implants 2019, 34, 343–356. [Google Scholar] [CrossRef]
- Vi, S.; Pham, D.; Du, Y.Y.M.; Arora, H.; Tadakamadla, S.K. Mini-Implant-Retained Overdentures for the Rehabilitation of Completely Edentulous Maxillae: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public. Health 2021, 18, 4377. [Google Scholar] [CrossRef] [PubMed]
- Enkling, N.; Haueter, M.; Worni, A.; Müller, F.; Leles, C.R.; Schimmel, M. A Prospective Cohort Study on Survival and Success of One-Piece Mini-Implants with Associated Changes in Oral Function: Five-Year Outcomes. Clin. Oral Implants Res. 2019, 30, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Tawil, G.; Younan, R.; Azar, P.; Sleilati, G. Conventional and Advanced Implant Treatment in the Type II Diabetic Patient: Surgical Protocol and Long-Term Clinical Results. Int. J. Oral Maxillofac. Implants 2008, 23, 744–752. [Google Scholar]
- De la Rosa, M.; Rodríguez, A.; Sierra, K.; Mendoza, G.; Chambrone, L. Predictors of Peri-Implant Bone Loss during Long-Term Maintenance of Patients Treated with 10-Mm Implants and Single Crown Restorations. Int. J. Oral Maxillofac. Implants 2013, 28, 798–802. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T. Implant Failures and Age at the Time of Surgery: A Retrospective Study on Implant Treatments in 4585 Edentulous Jaws. Clin. Implant Dent. Relat. Res. 2019, 21, 514–520. [Google Scholar] [CrossRef] [PubMed]
- González-Gil, D.; Dib-Zaitum, I.; Flores-Fraile, J.; López-Marcos, J. Importance of Osseoperception and Tactile Sensibility during Masticatory Function in Different Prosthetic Rehabilitations: A Review. Medicina 2022, 58, 92. [Google Scholar] [CrossRef]
- Lee, I.-K.; Choi, H.-S.; Jeong, S.-H.; Lee, J.-T. The Effect of Three Surgical Therapies to Increase Keratinized Mucosa Surrounding Dental Implants with Peri-Implantitis: A Pilot Study. Medicina 2021, 57, 1093. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosio, F.; Caggiano, M.; Schiavo, L.; Savarese, G.; Carpinelli, L.; Amato, A.; Iandolo, A. Chronic Stress and Depression in Periodontitis and Peri-Implantitis: A Narrative Review on Neurobiological, Neurobehavioral and Immune-Microbiome Interplays and Clinical Management Implications. Dent. J. 2022, 10, 49. [Google Scholar] [CrossRef] [PubMed]
| Variable | All Participants | Mandible | Maxilla | p-Value |
|---|---|---|---|---|
| Sample size (n) | 71 (100%) | 42 (59.2%) | 29 (40.8%) | |
| Gender, female | 57 (80.3) | 33 (57.9%) | 24 (42.1%) | 0.770 N.S. |
| Age, years | 67.55 ± 7.93 | 66.38 ± 8.61 | 69.24 ± 6.61 | 0.140 N.S. |
| Age group | 0.131 NS | |||
| <60 years | 12 (16.9%) | 10 (83.3%) | 2 (16.7%) | |
| 61–70 years | 34 (47.9%) | 17 (50.0%) | 17 (50.0%) | |
| >70 years | 25 (35.2%) | 15 (60.0%) | 10 (40.0%) | |
| Antagonistic jaw | 0.061 N.S. | |||
| Complete denture | 26 (36.6%) | 15 (57.7%) | 11 (42.3%) | |
| RPD | 31 (43.7%) | 15 (48.4%) | 16 (51.6%) | |
| Natural teeth/FPD | 14 (19.7) | 12 (85.7%) | 2 (14.3%) | |
| Number of mini dental implant at baseline | 142 | 84 | 58 | |
| Number of mini dental implants lost to follow-up | 5 | 3 | 2 |
| MBL Change | N | x | SD | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| All participants | 1 year | 71 | −0.22 | 0.36 | 0.13–0.30 | |
| 3 years | 71 | −0.38 | 0.56 | 0.25–0.52 | ||
| 5 years | 71 | −0.51 | 0.66 | 0.35–0.67 | ||
| Jaw of Insertion | Mandible | 1 year | 42 | −0.22 | 0.32 | 0.10–0.33 |
| 3 years | 42 | −0.37 | 0.48 | 0.19–0.54 | ||
| 5 years | 42 | −0.50 | 0.56 | 0.29–0.70 | ||
| Maxilla | 1 year | 29 | −0.22 | 0.41 | 0.08–0.35 | |
| 3 years | 29 | −0.40 | 0.67 | 0.19–0.61 | ||
| 5 years | 29 | −0.52 | 0.78 | 0.28–0.77 | ||
| Gender | Female | 1 year | 57 | −0.24 | 0.37 | 0.13–0.36 |
| 3 years | 57 | −0.42 | 0.59 | 0.19–0.54 | ||
| 5 years | 57 | −0.54 | 0.67 | 0.27–0.68 | ||
| Male | 1 year | 14 | −0.22 | 0.26 | 0.03–0.41 | |
| 3 years | 14 | −0.32 | 0.41 | 0.06–0.65 | ||
| 5 years | 14 | −0.51 | 0.57 | 0.17–0.86 | ||
| Antagonistic jaw status | Complete denture | 1 year | 26 | −0.16 | 0.26 | 0.06–0.26 |
| 3 years | 26 | −0.25 | 0.34 | 0.11–0.38 | ||
| 5 years | 26 | −0.39 | 0.47 | 0.20–0.58 | ||
| Removable partial denture | 1 year | 31 | −0.24 | 0.40 | 0.09–0.38 | |
| 3 years | 31 | −0.51 | 0.70 | 0.25–0.77 | ||
| 5 years | 31 | −0.64 | 0.80 | 0.34–0.93 | ||
| Natural teeth or Fixed partial denture | 1 year | 14 | −0.28 | 0.43 | 0.03–0.52 | |
| 3 years | 14 | −0.35 | 0.53 | 0.04–0.65 | ||
| 5 years | 14 | −0.44 | 0.59 | 0.09–0.78 |
| Successful Implants | 95% Confidence Interval (Time in Month) | |||||
|---|---|---|---|---|---|---|
| Group | Number of implants (baseline) | Number of Events | n | Rate (%) | Lower bound | Upper bound |
| Mandible | 106 | 6 (6.7%) | 83 | 93.3 | 55.94 | 60.17 |
| Failure | Success or satisfactory survival | |||||
| Maxilla | 78 | 4 (6.6%) | 57 | 93.4 | 56.34 | 60.90 |
| Failure or compromised survival | Success or satisfactory survival | |||||
| Overall | 184 | 10 (6.7%) | 140 | 93.3 | 56.80 | 59.76 |
| Failure or compromised survival | Success or satisfactory survival | |||||
| P L A Q U E I N D E X | Modified Plaque Index: 1-year follow-up | Degree | Frequency (n) | Percent (%) |
| 0 | 21 | 29.6 | ||
| 1 | 30 | 42.3 | ||
| 2 | 20 | 28.2 | ||
| Modified Plaque Index: 3-year follow-up | 0 | 20 | 28.2 | |
| 1 | 31 | 43.7 | ||
| 2 | 15 | 21.1 | ||
| 3 | 5 | 7.0 | ||
| Modified Plaque Index: 5-year follow-up | 0 | 16 | 22.5 | |
| 1 | 33 | 46.5 | ||
| 2 | 17 | 23.9 | ||
| 3 | 4 | 5.6 | ||
| B L E E D I N G I N D E X | Modified Bleeding Index: 1-year follow-up | Degree | Frequency (n) | Percent (%) |
| 0 | 27 | 38.0 | ||
| 1 | 35 | 49.3 | ||
| 2 | 9 | 12.7 | ||
| Modified Bleeding Index: 3-year follow-up | 0 | 19 | 26.8 | |
| 1 | 35 | 49.3 | ||
| 2 | 17 | 23.9 | ||
| Modified Bleeding Index: 5-year follow-up * | 0 | 16 | 22.5 | |
| 1 | 36 | 50.7 | ||
| 2 | 18 | 25.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Celebic, A.; Kovacic, I.; Petricevic, N.; Puljic, D.; Popovac, A.; Kirsic, S.P. Mini-Implants Retaining Removable Partial Dentures in Subjects without Posterior Teeth: A 5-Year Prospective Study Comparing the Maxilla and the Mandible. Medicina 2023, 59, 237. https://doi.org/10.3390/medicina59020237
Celebic A, Kovacic I, Petricevic N, Puljic D, Popovac A, Kirsic SP. Mini-Implants Retaining Removable Partial Dentures in Subjects without Posterior Teeth: A 5-Year Prospective Study Comparing the Maxilla and the Mandible. Medicina. 2023; 59(2):237. https://doi.org/10.3390/medicina59020237
Chicago/Turabian StyleCelebic, Asja, Ines Kovacic, Nikola Petricevic, Dario Puljic, Aleksandra Popovac, and Sanja Persic Kirsic. 2023. "Mini-Implants Retaining Removable Partial Dentures in Subjects without Posterior Teeth: A 5-Year Prospective Study Comparing the Maxilla and the Mandible" Medicina 59, no. 2: 237. https://doi.org/10.3390/medicina59020237
APA StyleCelebic, A., Kovacic, I., Petricevic, N., Puljic, D., Popovac, A., & Kirsic, S. P. (2023). Mini-Implants Retaining Removable Partial Dentures in Subjects without Posterior Teeth: A 5-Year Prospective Study Comparing the Maxilla and the Mandible. Medicina, 59(2), 237. https://doi.org/10.3390/medicina59020237







