Epstein–Barr Virus-Positive Cutaneous and Systemic Plasmacytosis with TAFRO Syndrome-like Symptoms Successfully Treated with Rituximab
Abstract
1. Introduction
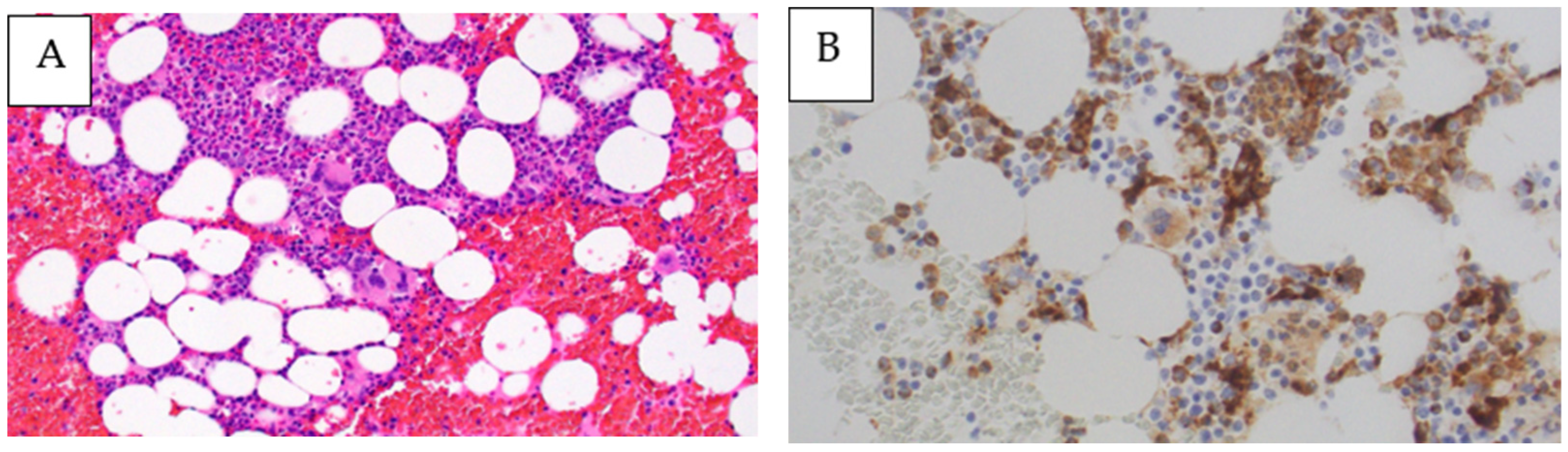
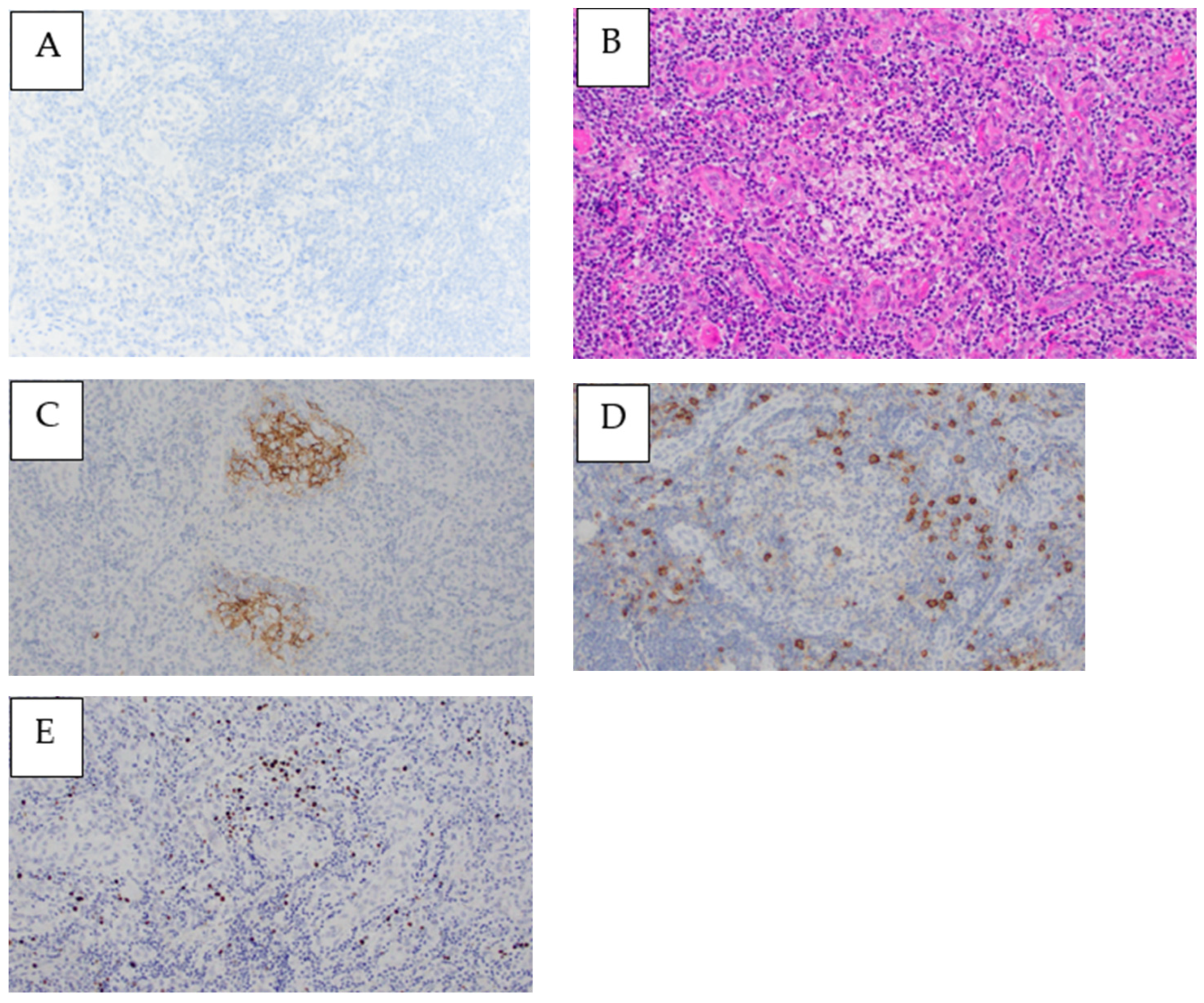
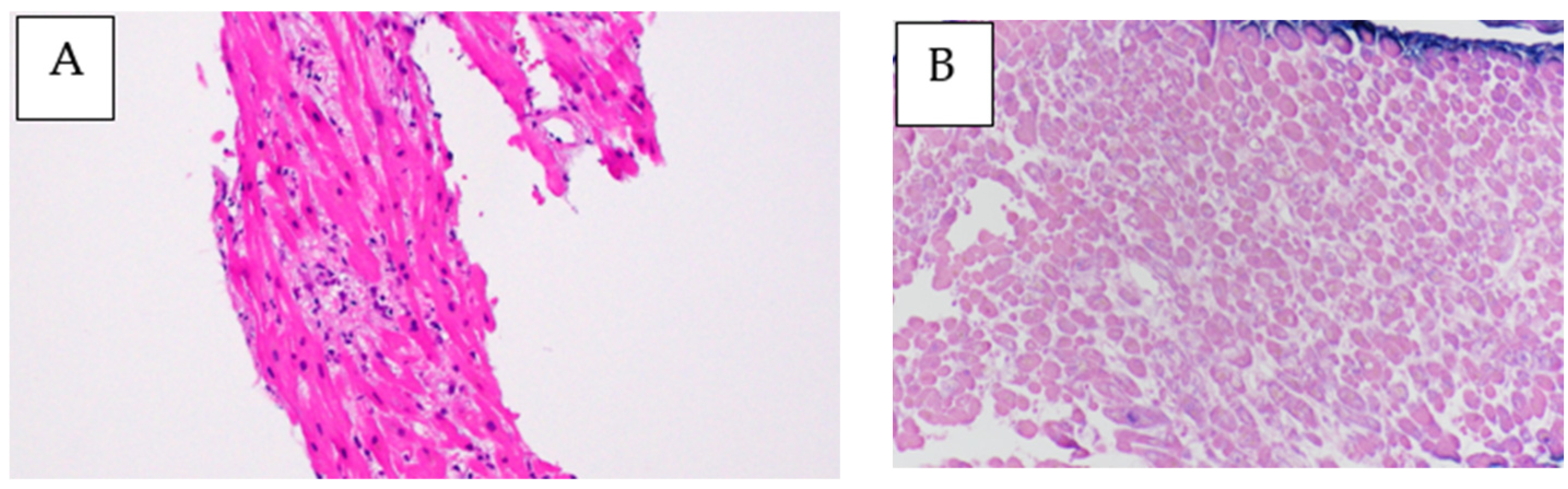
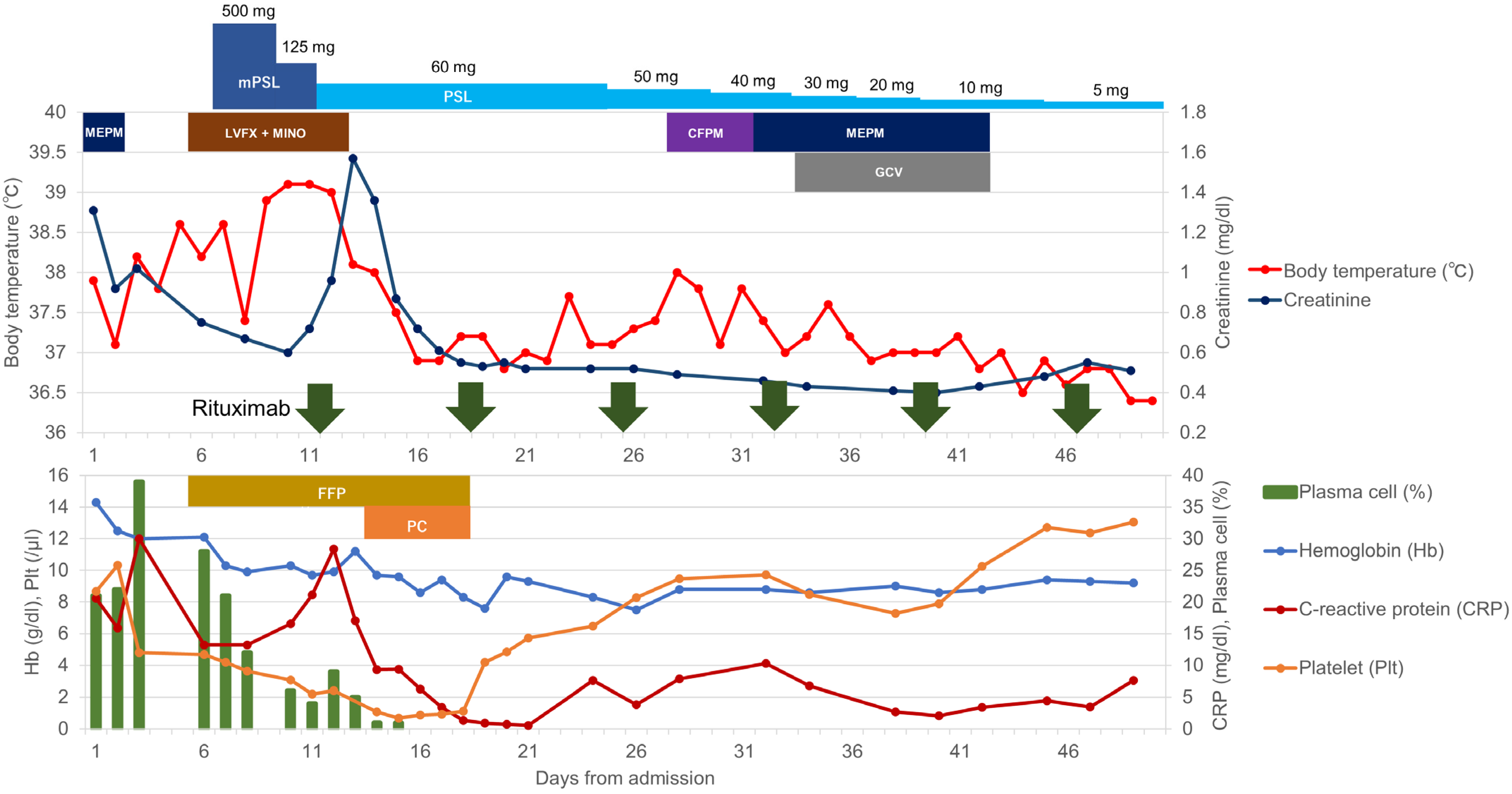
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aita, T.; Hamaguchi, S.; Shimotani, Y.; Nakamoto, Y. Idiopathic multicentric Castleman disease preceded by cutaneous plasmacytosis successfully treated by tocilizumab. BMJ Case Rep. 2020, 13, e236283. [Google Scholar] [CrossRef]
- Drissi, M.; Dunlap, R.; Clayton, L.; Raess, P.W.; Mengden Koon, S.; White, K. Cutaneous plasmacytosis and idiopathic multicentric Castleman disease: A spectrum of disease? Am. J. Dermatopathol. 2022, 44, 294–296. [Google Scholar] [CrossRef] [PubMed]
- Takai, K.; Nikkuni, K.; Shibuya, H.; Hashidate, H. Thrombocytopenia with mild bone marrow fibrosis accompanied by fever, pleural effusion, ascites, and hepatosplenomegaly. Rinsho Ketsueki 2010, 51, 320–325. [Google Scholar] [PubMed]
- Kurose, N.; Futatsuya, C.; Mizutani, K.-I.; Kumagai, M.; Shioya, A.; Guo, X.; Aikawa, A.; Nakada, S.; Fujimoto, S.; Kawabata, H.; et al. The clinicopathological comparison among nodal cases of idiopathic multicentric Castleman disease with and without TAFRO syndrome. Hum. Pathol. 2018, 77, 130–138. [Google Scholar] [CrossRef]
- Fajgenbaum, D.C.; van Rhee, F.; Nabel, C.S. HHV-8-negative, idiopathic multicentric Castleman disease: Novel insights into biology, pathogenesis, and therapy. Blood 2014, 123, 2924–2933. [Google Scholar] [CrossRef]
- Iwaki, N.; Fajgenbaum, D.C.; Nabel, C.S.; Gion, Y.; Kondo, E.; Kawano, M.; Masunari, T.; Yoshida, I.; Moro, H.; Nikkuni, K.; et al. Clinicopathologic analysis of TAFRO syndrome demonstrates a distinct subtype of HHV-8-negative multicentric Castleman disease. Am. J. Hematol. 2016, 91, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, S.; Sakai, T.; Kawabata, H.; Kurose, N.; Yamada, S.; Takai, K.; Aoki, S.; Kuroda, J.; Ide, M.; Setoguchi, K.; et al. Is TAFRO syndrome a subtype of idiopathic multicentric Castleman disease? Am. J. Hematol. 2019, 94, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Masaki, Y.; Arita, K.; Sakai, T.; Takai, K.; Aoki, S.; Kawabata, H. Castleman disease and TAFRO syndrome. Ann. Hematol. 2022, 101, 485–490. [Google Scholar] [CrossRef]
- Masaki, Y.; Kawabata, H.; Takai, K.; Kojima, M.; Tsukamoto, N.; Ishigaki, Y.; Kurose, N.; Ide, M.; Murakami, J.; Nara, K.; et al. Proposed diagnostic criteria, disease severity classification and treatment strategy for TAFRO syndrome, 2015 version. Int. J. Hematol. 2016, 103, 686–692. [Google Scholar] [CrossRef]
- Masaki, Y.; Japanese TAFRO Syndrome Research Team; Kawabata, H.; Takai, K.; Tsukamoto, N.; Fujimoto, S.; Ishigaki, Y.; Kurose, N.; Miura, K.; Nakamura, S.; et al. 2019 Updated diagnostic criteria and disease severity classification for TAFRO syndrome. Int. J. Hematol. 2020, 111, 155–158. [Google Scholar] [CrossRef]
- Fujimoto, S.; Kawabata, H.; Sakai, T.; Yanagisawa, H.; Nishikori, M.; Nara, K.; Ohara, S.; Tsukamoto, N.; Kurose, N.; Yamada, S.; et al. Optimal treatments for TAFRO syndrome: A retrospective surveillance study in Japan. Int. J. Hematol. 2021, 113, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Liu, H.C.; Hung, T.T.; Liu, T.P. Possible roles of Epstein-Barr virus in Castleman disease. J. Cardiothorac. Surg. 2009, 4, 31. [Google Scholar] [CrossRef] [PubMed]
- Kurose, N.; Mizutani, K.-I.; Kumagai, M.; Shioya, A.; Guo, X.; Nakada, S.; Fujimoto, S.; Kawabata, H.; Masaki, Y.; Takai, K.; et al. An extranodal histopathological analysis of idiopathic multicentric Castleman disease with and without TAFRO syndrome. Pathol. Res. Pract. 2019, 215, 410–413. [Google Scholar] [CrossRef]
- Hiramatsu, S.; Ohmura, K.; Tsuji, H.; Kawabata, H.; Kitano, T.; Sogabe, A.; Hashimoto, M.; Murakami, K.; Imura, Y.; Yukawa, N.; et al. Successful treatment by rituximab in a patient with TAFRO syndrome with cardiomyopathy. Jpn. J. Clin. Immunol. 2016, 39, 64–71. [Google Scholar] [CrossRef]
- Shirai, T.; Onishi, A.; Waki, D.; Saegusa, J.; Morinobu, A. Successful treatment with tacrolimus in TAFRO syndrome: Two case reports and literature review. Medicine 2018, 97, e11045. [Google Scholar] [CrossRef]
- Yasuda, S.; Tanaka, K.; Ichikawa, A.; Watanabe, K.; Uchida, E.; Yamamoto, M.; Yamamoto, K.; Mizuchi, D.; Miura, O.; Fukuda, T. Aggressive TAFRO syndrome with reversible cardiomyopathy successfully treated with combination chemotherapy. Int. J. Hematol. 2016, 104, 512–518. [Google Scholar] [CrossRef]
- Dumic, I.; Radovanovic, M.; Igandan, O.; Savic, I.; Nordstrom, C.W.; Jevtic, D.; Subramanian, A.; Ramanan, P. A Fatal Case of Kaposi Sarcoma Immune Reconstitution Syndrome (KS-IRIS) Complicated by Kaposi Sarcoma Inflammatory Cytokine Syndrome (KICS) or Multicentric Castleman Disease (MCD): A Case Report and Review. Am. J. Case Rep. 2020, 21, e926433. [Google Scholar] [CrossRef] [PubMed]
- Micali, C.; Russotto, Y.; Facciolà, A.; Marino, A.; Celesia, B.M.; Pistarà, E.; Caci, G.; Nunnari, G.; Pellicanò, G.F.; Rullo, E.V. Pulmonary Kaposi Sarcoma without Respiratory Symptoms and Skin Lesions in an HIV-Naïve Patient: A Case Report and Literature Review. Infect. Dis. Rep. 2022, 14, 228–242. [Google Scholar] [CrossRef] [PubMed]
- Van Rhee, F.; Voorhees, P.; Dispenzieri, A.; Fosså, A.; Srkalovic, G.; Ide, M.; Munshi, N.; Schey, S.; Streetly, M.; Pierson, S.; et al. International, evidence-based consensus treatment guidelines for idiopathic multicentric Castleman disease. Blood 2018, 132, 2115–2124. [Google Scholar] [CrossRef] [PubMed]
- Kanda, J.; Kawabata, H.; Yamaji, Y.; Ichinohe, T.; Ishikawa, T.; Tamura, T.; Furukawa, Y.; Kimura, T.; Kita, T.; Uchiyama, T. Reversible cardiomyopathy associated with Multicentric Castleman disease: Successful treatment with tocilizumab, an anti-interleukin 6 receptor antibody. Int. J. Hematol. 2007, 85, 207–211. [Google Scholar] [CrossRef]
- Yamamoto, S.; Nakatani, S.; Kijima, K.; Kohno, K.; Morita, S.; Koito, H.; Yutaka, H.; Miyasaka, Y.; Nakamura, S.; Iwasaka, T.; et al. Multicentric Castleman’s disease with reversible left ventricular diffuse hypokinesis. Nihon Naika Gakkai Zasshi J. Jpn. Soc. Intern. Med. 2001, 90, 123–126. [Google Scholar] [CrossRef] [PubMed]


| <Complete Blood Count> | <Others> | ||||
| White blood cell | 13,300 | μ/L | IgG | 2558 | mg/dL |
| Neutrophil | 34 | % | IgA | 334 | mg/dL |
| Lymphocyte | 13 | % | IgM | 1630 | mg/dL |
| Monocyte | 2 | % | IgD | 0.7 | mg/dL |
| Eosinophil | 22 | % | IgE | 1490 | IU/mL |
| Myelocyte | 1 | % | IgG4 | 54.8 | mg/dL |
| Plasma cell | 28 | % | κ free light chain | 207 | mg/dL |
| Hemoglobin | 12.1 | g/dL | λ free light chain | 211 | mg/dL |
| Red blood cell | 473 | ×104/μ/L | Soluble interleukin-2 receptor | 6120 | U/mL |
| Hematocrit | 40.2 | % | Interleukin-6 | 13.2 | pg/mL |
| Mean corpuscular volume | 85 | fl | VEGF (plasma) | 28 | pg/mL |
| Platelet | 11.7 | ×109/L | Proteinase 3-ANCA | <1.0 | U/mL |
| Myeloperoxidase-ANCA | <1.0 | U/mL | |||
| <Coagulation> | Antinuclear antibody | <40 | |||
| PT | 50 | % | Anti-ds DNA antibodies IgG | <10 | |
| APTT | 37.6 | sec | Anti-SS A | 1.6 | U/mL |
| PT–INR | 1.63 | Anti-SS B | 5.2 | U/mL | |
| Fibrinogen | 101 | mg/dL | Rheumatoid factor | 5.1 | IU/mL |
| D-dimer | 1.73 | μg/mL | HIV antigen/antibody | (−) | |
| FDP | 6.8 | μg/mL | Hepatitis B surface antigen | (−) | |
| Antithrombin III | 64 | % | Hepatitis B surface antibody | (+) | |
| Hepatitis B virus DNA | (−) | ||||
| <Blood Chemistry> | Hepatitis C virus antibody | (−) | |||
| Total protein | 6.5 | g/dL | T-SPOT. TB | (−) | |
| Albumin | 1.7 | g/dL | EB-VCA-IgG | 20 | |
| Aspartate aminotransferase | 18 | U/L | EB-VCA-IgM | <10 | |
| Alanine aminotransferase | 19 | U/L | EB-EADR IgG | <10 | |
| Alkaline phosphatase | 90 | U/L | EB-EADR IgM | <10 | |
| γ-Glutamyltranspeptidase | 40 | U/L | EBNA | 10 | |
| Lactate dehydrogenase | 388 | U/L | Epstein–Barr virus DNA | 4.69 | Log IU/mL |
| Total bilirubin | 0.77 | mg/dL | Cytomegalovirus DNA | (−) | |
| Blood urea nitrogen | 19.1 | mg/dL | Human herpesvirus-8 DNA | (−) | |
| Uric acid | 8.0 | mg/dL | ACE | 10.0 | U/L |
| Creatinine | 0.75 | mg/dL | ADAMTS13 activity | 60 | % |
| Sodium | 138 | mEq/L | |||
| Potassium | 3.5 | mEq/L | <Dipstick urinalysis> | ||
| Chloride | 105 | mEq/L | pH | 5.0 | |
| Phosphate | 3.7 | mg/dL | Specific gravity | 1.023 | |
| Magnesium | 2.0 | mg/dL | Blood | (++) | |
| Creatinine phosphokinase | 26 | U/L | Protein | (++) | |
| C-reactive protein | 5.29 | mg/dL | <Urine microscopy> | ||
| Haptoglobin | 143 | mg/dL | White blood cell | 5–9 | /HPF |
| Red blood cell | 30–49 | /HPF | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kakiuchi, S.; Akiyama, H.; Harima, I.; Takagi, I.; Rikitake, J.; Kozuki, Y.; Inaba, M.; Fujiwara, H.; Kurose, N.; Yamada, S.; et al. Epstein–Barr Virus-Positive Cutaneous and Systemic Plasmacytosis with TAFRO Syndrome-like Symptoms Successfully Treated with Rituximab. Medicina 2023, 59, 216. https://doi.org/10.3390/medicina59020216
Kakiuchi S, Akiyama H, Harima I, Takagi I, Rikitake J, Kozuki Y, Inaba M, Fujiwara H, Kurose N, Yamada S, et al. Epstein–Barr Virus-Positive Cutaneous and Systemic Plasmacytosis with TAFRO Syndrome-like Symptoms Successfully Treated with Rituximab. Medicina. 2023; 59(2):216. https://doi.org/10.3390/medicina59020216
Chicago/Turabian StyleKakiuchi, Seiji, Hiroaki Akiyama, Isamu Harima, Ikumi Takagi, Junpei Rikitake, Yoko Kozuki, Mayumi Inaba, Hiroshi Fujiwara, Nozomu Kurose, Sohsuke Yamada, and et al. 2023. "Epstein–Barr Virus-Positive Cutaneous and Systemic Plasmacytosis with TAFRO Syndrome-like Symptoms Successfully Treated with Rituximab" Medicina 59, no. 2: 216. https://doi.org/10.3390/medicina59020216
APA StyleKakiuchi, S., Akiyama, H., Harima, I., Takagi, I., Rikitake, J., Kozuki, Y., Inaba, M., Fujiwara, H., Kurose, N., Yamada, S., & Masaki, Y. (2023). Epstein–Barr Virus-Positive Cutaneous and Systemic Plasmacytosis with TAFRO Syndrome-like Symptoms Successfully Treated with Rituximab. Medicina, 59(2), 216. https://doi.org/10.3390/medicina59020216






