Topical Fibrin Sealant (Tisseel@) Does Not Provide a Synergic Blood-Conservation Effect with Tranexamic Acid in Total Knee Arthroplasty—A Prospective Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Intervention Protocol
2.4. Outcomes
2.5. Randomization and Blinding
2.6. Minimum Sample Size
2.7. Statistical Analysis
3. Results
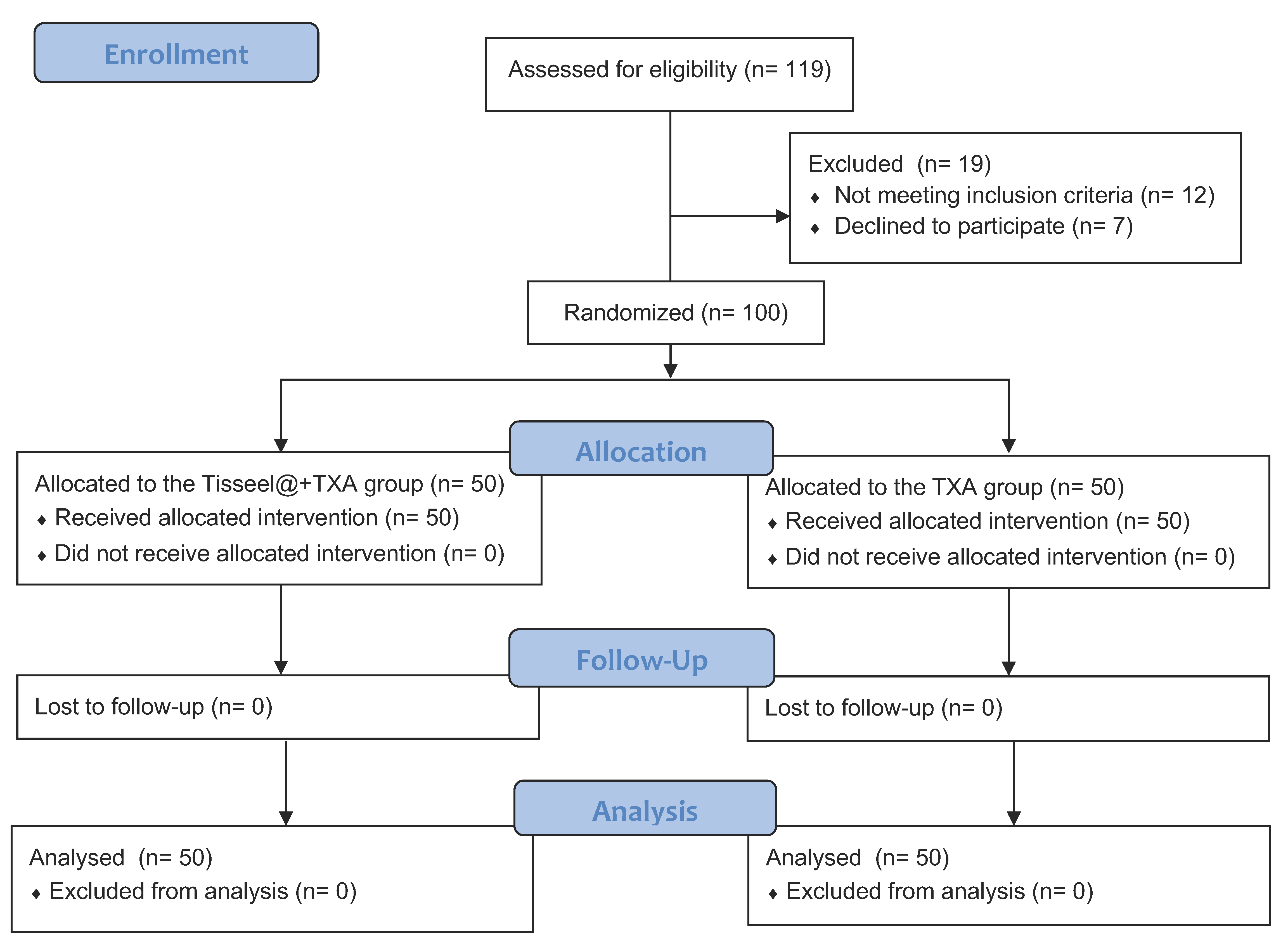
3.1. Participants’ Flow
3.2. Baseline Data
3.3. Primary and Secondary Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br. J. Anaesth. 1997, 78, 606–617. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.L.; Wainwright, T.W.; Foster, J.D.; Smith, J.R.; Middleton, R.G.; Francis, N.K. A systematic review of patient reported outcomes and patient experience in enhanced recovery after orthopaedic surgery. Ann. R. Coll. Surg. Engl. 2014, 96, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Soffin, E.M.; YaDeau, J.T. Enhanced recovery after surgery for primary hip and knee arthroplasty: A review of the evidence. Br. J. Anaesth. 2016, 117, iii62–iii72. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Qian, W.; Jiang, C.; Ye, C.; Chen, X. Enhanced recovery after surgery for hip and knee arthroplasty: A systematic review and meta-analysis. Postgrad. Med. J. 2017, 93, 736–742. [Google Scholar] [CrossRef]
- Kim, K.I. Blood Management in Total Knee Arthroplasty: Updates and Debates. Knee Surg. Relat. Res. 2016, 28, 177–178. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, G.C.; Hawes, T.; Cushner, F.D.; Scott, W.N. Current trends in blood conservation in total knee arthroplasty. Clin. Orthop. Relat. Res. 2005, 440, 170–174. [Google Scholar] [CrossRef]
- Alshryda, S.; Sukeik, M.; Sarda, P.; Blenkinsopp, J.; Haddad, F.S.; Mason, J.M. A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Jt. J. 2014, 96, 1005–1015. [Google Scholar] [CrossRef]
- Aguilera, X.; Martínez-Zapata, M.J.; Hinarejos, P.; Jordán, M.; Leal, J.; González, J.C.; Monllau, J.C.; Celaya, F.; Rodríguez-Arias, A.; Fernández, J.A.; et al. Topical and intravenous tranexamic acid reduce blood loss compared to routine hemostasis in total knee arthroplasty: A multicenter, randomized, controlled trial. Arch. Orthop. Trauma Surg. 2015, 135, 1017–1025. [Google Scholar] [CrossRef]
- Wu, Q.; Zhang, H.A.; Liu, S.L.; Meng, T.; Zhou, X.; Wang, P. Is tranexamic acid clinically effective and safe to prevent blood loss in total knee arthroplasty? A meta-analysis of 34 randomized controlled trials. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 525–541. [Google Scholar] [CrossRef]
- Chang, C.H.; Chang, Y.; Chen, D.W.; Ueng, S.W.; Lee, M.S. Topical tranexamic acid reduces blood loss and transfusion rates associated with primary total hip arthroplasty. Clin. Orthop. Relat. Res. 2014, 472, 1552–1557. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Barrena, E.; Ortega-Andreu, M.; Padilla-Eguiluz, N.G.; Pérez-Chrzanowska, H.; Figueredo-Zalve, R. Topical intra-articular compared with intravenous tranexamic acid to reduce blood loss in primary total knee replacement: A double-blind, randomized, controlled, noninferiority clinical trial. J. Bone Jt. Surg. 2014, 96, 1937–1944. [Google Scholar] [CrossRef] [PubMed]
- Budde, S.; Noll, Y.; Zieglschmid, V.; Schroeder, C.; Koch, A.; Windhagen, H. Determination of the efficacy of EVICEL™ on blood loss in orthopaedic surgery after total knee replacement: Study protocol for a randomised controlled trial. Trials 2015, 16, 299. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Cao, J.G.; Wang, L.; Ma, X.L. Effect of fibrin sealant on blood loss following total knee arthroplasty: A systematic review and meta-analysis. Int. J. Surg. 2014, 12, 95–102. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yang, T.Q.; Geng, X.L.; Ding, M.C.; Yang, M.X.; Zhang, Q. The efficacy of fibrin sealant in knee surgery: A meta-analysis. Orthop. Traumatol. Surg. Res. 2015, 101, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Shan, L.; Zeng, H.; Sun, M.; Hua, Y.; Cai, Z. Is fibrin sealant effective and safe in total knee arthroplasty? A meta-analysis of randomized trials. J. Orthop. Surg. Res. 2014, 9, 36. [Google Scholar] [CrossRef]
- Molloy, D.O.; Archbold, H.A.; Ogonda, L.; McConway, J.; Wilson, R.K.; Beverland, D.E. Comparison of topical fibrin spray and tranexamic acid on blood loss after total knee replacement: A prospective, randomised controlled trial. J. Bone Jt. Surg. Br. 2007, 89, 306–309. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef]
- Haas, S.B.; Cook, S.; Beksac, B. Minimally invasive total knee replacement through a mini midvastus approach: A comparative study. Clin. Orthop. Relat. Res. 2004, 428, 68–73. [Google Scholar] [CrossRef]
- Nadler, S.B.; Hidalgo, J.H.; Bloch, T. Prediction of blood volume in normal human adults. Surgery 1962, 51, 224–232. [Google Scholar]
- Gross, J.B. Estimating allowable blood loss: Corrected for dilution. Anesthesiology 1983, 58, 277–280. [Google Scholar] [CrossRef]
- Price, D.D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef]
- Vince, K.; Chivas, D.; Droll, K.P. Wound complications after total knee arthroplasty. J. Arthroplast. 2007, 22, 39–44. [Google Scholar] [CrossRef]
- Roos, E.M.; Roos, H.P.; Lohmander, L.S.; Ekdahl, C.; Beynnon, B.D. Knee Injury and Osteoarthritis Outcome Score (KOOS)—Development of a self-administered outcome measure. J. Orthop. Sports Phys. Ther. 1998, 28, 88–96. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Gao, F.; Ma, J.; Sun, W.; Guo, W.; Li, Z.; Wang, W. Topical fibrin sealant versus intravenous tranexamic acid for reducing blood loss following total knee arthroplasty: A systematic review and meta-analysis. Int. J. Surg. 2016, 32, 31–37. [Google Scholar] [CrossRef]
- Courtney, P.M.; Boniello, A.J.; Berger, R.A. Complications Following Outpatient Total Joint Arthroplasty: An Analysis of a National Database. J. Arthroplast. 2017, 32, 1426–1430. [Google Scholar] [CrossRef] [PubMed]
- Pennestrì, F.; Maffulli, N.; Sirtori, P.; Perazzo, P.; Negrini, F.; Banfi, G.; Peretti, G.M. Blood management in fast-track orthopedic surgery: An evidence-based narrative review. J. Orthop. Surg. Res. 2019, 14, 263. [Google Scholar] [CrossRef] [PubMed]
- Hardy, J.F.; Desroches, J. Natural and synthetic antifibrinolytics in cardiac surgery. Can. J. Anaesth. 1992, 39, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Chen, J.; Chen, F.; Que, W. The effect of tranexamic acid on blood loss and use of blood products in total knee arthroplasty: A meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1742–1752. [Google Scholar] [CrossRef] [PubMed]
- Abrishami, A.; Chung, F.; Wong, J. Topical application of antifibrinolytic drugs for on-pump cardiac surgery: A systematic review and meta-analysis. Can. J. Anaesth. 2009, 56, 202–212. [Google Scholar] [CrossRef] [PubMed]
- Ker, K.; Edwards, P.; Perel, P.; Shakur, H.; Roberts, I. Effect of tranexamic acid on surgical bleeding: Systematic review and cumulative meta-analysis. BMJ 2012, 344, e3054. [Google Scholar] [CrossRef]
- Ho, K.M.; Ismail, H. Use of intravenous tranexamic acid to reduce allogeneic blood transfusion in total hip and knee arthroplasty: A meta-analysis. Anaesth. Intensive Care 2003, 31, 529–537. [Google Scholar] [CrossRef]
- Shemshaki, H.; Nourian, S.M.; Nourian, N.; Dehghani, M.; Mokhtari, M.; Mazoochian, F. One step closer to sparing total blood loss and transfusion rate in total knee arthroplasty: A meta-analysis of different methods of tranexamic acid administration. Arch. Orthop. Trauma Surg. 2015, 135, 573–588. [Google Scholar] [CrossRef] [PubMed]
- Cronkite, E.P.; Lozner, E.L.; Deaver, J.M. Use of thrombin and fibrinogen in skin grafting: Preliminary report. J. Am. Med. Assoc. 1944, 124, 976–978. [Google Scholar] [CrossRef]
- Gasser, G.; Mossig, H.; Fischer, M.; Eidler, R.; Kläring, W.; Lurf, H. Modification of suprapubic prostatectomy using a biological gluing technic. Wien. Klin. Wochenschr. 1983, 95, 399–403. [Google Scholar] [PubMed]
- Wurtz, A.; Chambon, J.P.; Sobecki, L.; Batrouni, R.; Huart, J.J.; Burnouf, T. Use of a biological glue in partial pulmonary excision surgery. Results of a controlled trial in 50 patients. Ann. Chir. 1991, 45, 719–723. [Google Scholar] [PubMed]
- Milne, A.A.; Murphy, W.G.; Reading, S.J.; Ruckley, C.V. Fibrin sealant reduces suture line bleeding during carotid endarterectomy: A randomised trial. Eur. J. Vasc. Endovasc. Surg. 1995, 10, 91–94. [Google Scholar] [CrossRef]
- Akizuki, S.; Yasukawa, Y.; Takizawa, T. A new method of hemostasis for cementless total knee arthroplasty. Bull. Hosp. Jt. Dis. 1997, 56, 222–224. [Google Scholar]
- Levy, O.; Martinowitz, U.; Oran, A.; Tauber, C.; Horoszowski, H. The use of fibrin tissue adhesive to reduce blood loss and the need for blood transfusion after total knee arthroplasty. A prospective, randomized, multicenter study. J. Bone Jt. Surg. 1999, 81, 1580–1588. [Google Scholar] [CrossRef]
- Benoni, G.; Fredin, H. Fibrinolytic inhibition with tranexamic acid reduces blood loss and blood transfusion after knee arthroplasty: A prospective, randomised, double-blind study of 86 patients. J. Bone Jt. Surg. Br. 1996, 78, 434–440. [Google Scholar] [CrossRef]
- Hiippala, S.; Strid, L.; Wennerstrand, M.; Arvela, V.; Mäntylä, S.; Ylinen, J.; Niemelä, H. Tranexamic acid (Cyklokapron) reduces perioperative blood loss associated with total knee arthroplasty. Br. J. Anaesth. 1995, 74, 534–537. [Google Scholar] [CrossRef]
| TXA (n = 50) | Tisseel@ + TXA (n = 50) | p-Value | |
|---|---|---|---|
| Age (years) | 68.48 (49~80) | 71.42 (56~80) | 0.3 |
| Gender (female: male) | 41:9 | 30:20 | 0.027 |
| Body mass index (kg/m2) | 28.75 | 27.22 | 0.224 |
| Preoperative Hb (g/dL) | 13.78 ± 1.2 (12.0~17.1) | 13.67 ± 1.0 (12.2~16.4) | 0.254 |
| Preoperative Hct (%) | 41.67 | 41.18 | 0.191 |
| Preoperative INR | 1.4 | 1.3 | |
| Platelet count (1000/µL) | 158 | 147 | |
| American Society of Anesthesiologists (ASA) grade | 2.8 | 2.7 |
| TXA (n = 50) | Tisseel@ + TXA (n = 50) | p-Value | |
|---|---|---|---|
| Blood transfusion (no./total no) | 0/50 | 0/50 | 1 |
| Hb level change on post-OP day 1 | 1.46 ± 0.82 (−0.2~3.4) | 1.57 ± 0.83 (0.2~3.2) | 0.892 |
| Hct level change on post-OP day 1 | 4.92 ± 2.22 (0.9~10.1) | 4.92 ± 2.33 (0.6~9.6) | 0.498 |
| Estimated total blood loss (L) | 0.455 ± 0.2522 (0.083~1.213) | 0.463 ± 0.2422 (0.057~1.074) | 0.9 |
| Drainage volume (L) | 0.155 ± 0.099 (0~0.46) | 0.148 ± 0.099 (0~0.42) | 0.862 |
| Intra-operative blood loss (L) | 0.118 ± 0.051 (0.05~0.3) | 0.111 ± 0.040 (0.05~0.2) | 0.285 |
| Calculated blood loss (L) | 0.268 ± 0.108 (0.1~0.56) | 0.259 ± 0.1 (0.55~0.52) | 0.341 |
| VAS post-OP day 1 | 2.3 (0~6) | 2.6 (0~8) | |
| VAS post-OP day 2 | 2.1 (0~6) | 2.3 (1~6) | |
| Length of hospital stay (days) | 4.6 | 4.3 | |
| Range-of-motion (ROM) arc at discharge day | 116.8° | 114.9° | |
| KOOS score (post-OP 2 weeks) | 76.8 | 74.5 | |
| KOOS score (post-OP 6 weeks) | 86.5 | 86.9 |
| TXA (n = 50) | Tisseel@ + TXA (n = 50) | |
|---|---|---|
| Wound length in extension (cm) | 8.6 | 9.1 |
| Circumferential length change of knee (cm) (post-OP day 2) | 2.8 ± 0.9 | 3.1 ± 0.6 |
| Extensive ecchymosis status (post-OP 2 weeks) | 2 | 1 |
| Subcutaneous hematoma (post-OP 2 weeks) | 2 | 3 |
| Wound dehiscence (post-OP 2 weeks) | 1 | 0 |
| Deep-vein thrombosis (post-OP 2 weeks) | 0 | 1 (suspected) |
| Wound infection (post-OP 6 weeks) | 0 | 0 |
| Deep periprosthetic joint infection (post-OP 6 weeks) | 0 | 0 |
| Reoperation due to any reasons (post-OP 2 years) | 0 | 0 |
| Readmission for general complications (post-OP 2 years) | 0 | 0 |
| Cohen’s d | |
|---|---|
| Estimated total blood loss | 0.032382 |
| Calculated blood loss | 0.094433 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, C.-H.; Chang, C.-H.; Chang, Y.-H.; Shih, H.-N.; Hu, C.-C. Topical Fibrin Sealant (Tisseel@) Does Not Provide a Synergic Blood-Conservation Effect with Tranexamic Acid in Total Knee Arthroplasty—A Prospective Randomized Controlled Trial. Medicina 2023, 59, 2078. https://doi.org/10.3390/medicina59122078
Liu C-H, Chang C-H, Chang Y-H, Shih H-N, Hu C-C. Topical Fibrin Sealant (Tisseel@) Does Not Provide a Synergic Blood-Conservation Effect with Tranexamic Acid in Total Knee Arthroplasty—A Prospective Randomized Controlled Trial. Medicina. 2023; 59(12):2078. https://doi.org/10.3390/medicina59122078
Chicago/Turabian StyleLiu, Chia-Hung, Chih-Hsiang Chang, Yu-Han Chang, Hsin-Nung Shih, and Chih-Chien Hu. 2023. "Topical Fibrin Sealant (Tisseel@) Does Not Provide a Synergic Blood-Conservation Effect with Tranexamic Acid in Total Knee Arthroplasty—A Prospective Randomized Controlled Trial" Medicina 59, no. 12: 2078. https://doi.org/10.3390/medicina59122078
APA StyleLiu, C.-H., Chang, C.-H., Chang, Y.-H., Shih, H.-N., & Hu, C.-C. (2023). Topical Fibrin Sealant (Tisseel@) Does Not Provide a Synergic Blood-Conservation Effect with Tranexamic Acid in Total Knee Arthroplasty—A Prospective Randomized Controlled Trial. Medicina, 59(12), 2078. https://doi.org/10.3390/medicina59122078









