Subclavian Artery Pseudoaneurysm Following Bedside Temporary Hemodialysis Catheter Insertion: A Case Report
Abstract
1. Introduction
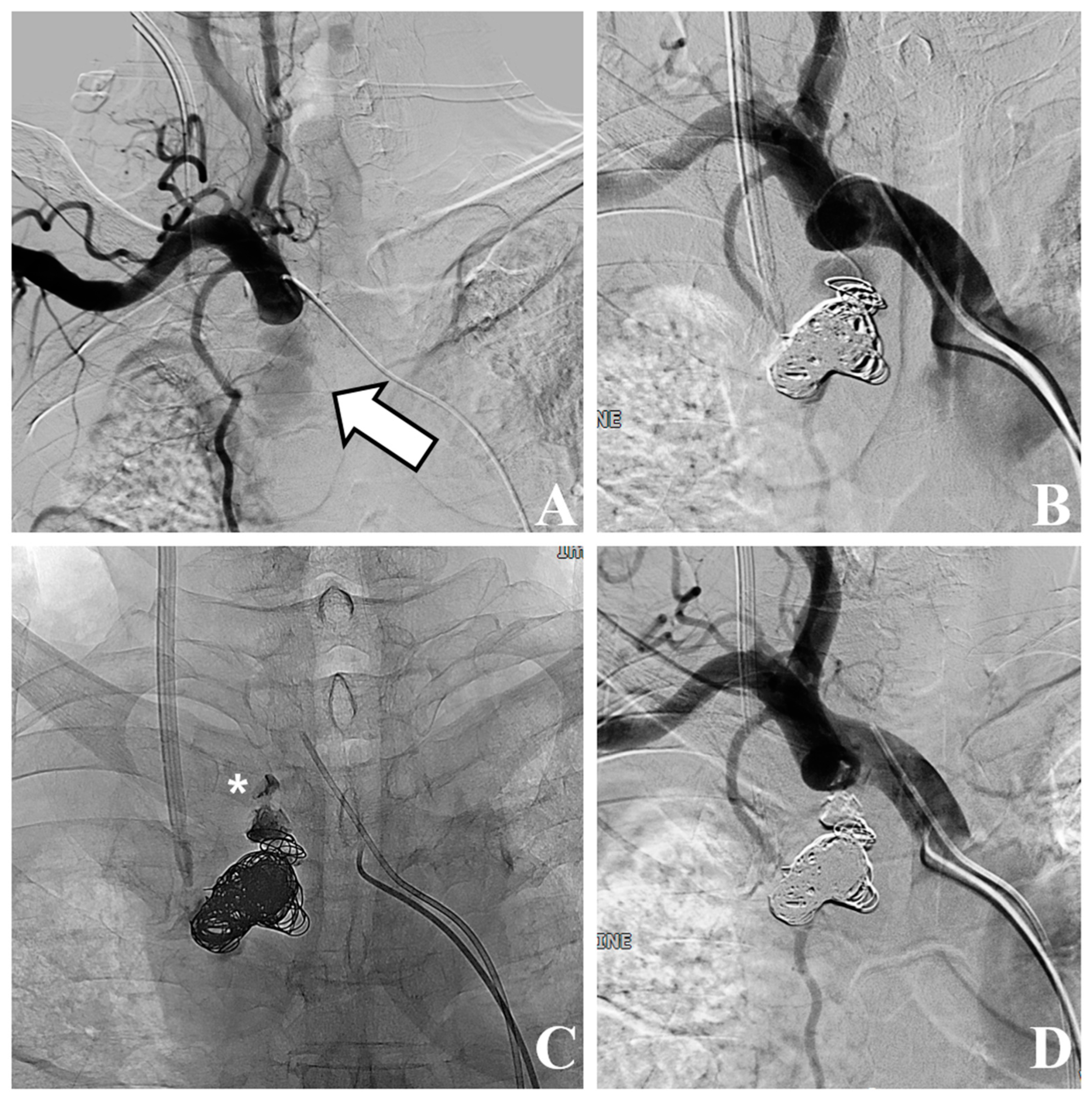
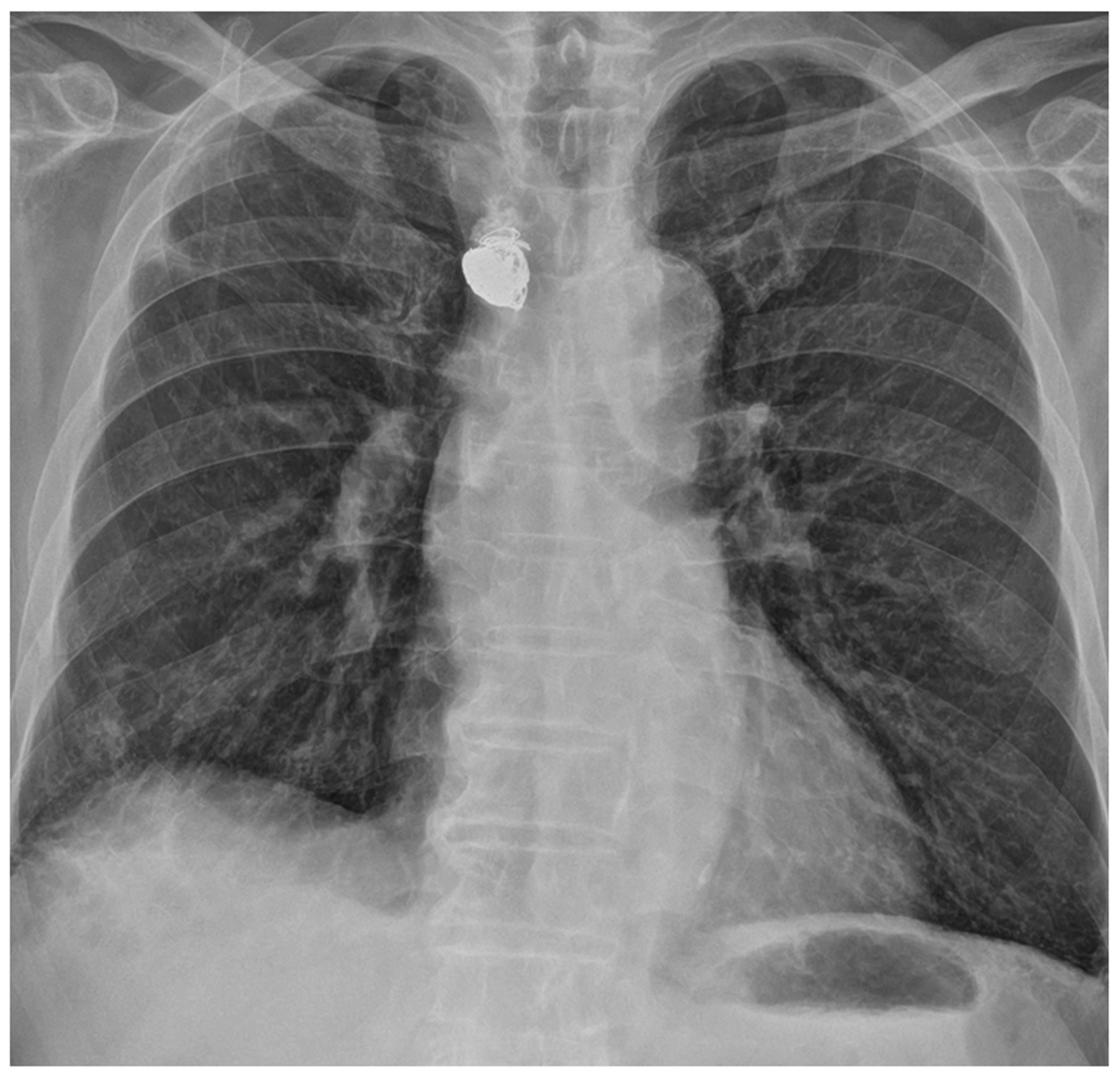
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schummer, W.; Schummer, C.; Tuppatsch, H.; Reinhart, K.; Hüttemann, E. On the use of ultrasound to assist central vein cannulation in Germany: A surgery of 817 departments of anesthesia. Anasthesiol. Intensiv. Notfallmedizin Schmerzther. 2004, 39, 87–93. [Google Scholar] [CrossRef]
- Song, W.G.; Jin, G.Y.; Han, Y.M.; Yu, H.C. Central venous catheterization: Comparison between interventional radiological procedure and blind surgical procedure. J. Korean Soc. Radiol. 2002, 47, 467–472. [Google Scholar] [CrossRef][Green Version]
- Xenos, E.S.; Freeman, M.; Stevens, S.; Cassada, D.; Pacanowski, J.; Goldman, M. Covered stents for injuries of subclavian and axillary arteries. J. Vasc. Surg. 2003, 38, 451–454. [Google Scholar] [CrossRef] [PubMed]
- Boulet, N.; Muller, L.; Rickard, C.M.; Lefrant, J.Y.; Roger, C. How to improve the efficiency and the safety of real-time ultrasound-guided central venous catheterization in 2023: A narrative review. Ann. Intensive Care 2023, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Wisborg, T.; Flaatten, H.; Koller, M.E. Percutaneous placement of permanent central venous catheters: Experience with 200 catheters. Acta Anaesthesiol. Scand. 1991, 35, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Iovino, F.; Pittiruti, M.; Buononato, M.; Lo Schiavo, F. Central venous catheterization: Complications of different placements. Ann. Chir. 2001, 126, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Adrian, M.; Borgquist, O.; Kröger, T.; Linné, E.; Bentzer, P.; Spångfors, M.; Åkeson, J.; Holmström, A.; Linnér, R.; Kander, T. Mechanical complications after central venous catheterisation in the ultrasound-guided era: A prospective multicentre cohort study. Br. J. Anaesth. 2022, 129, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Akkan, K.; Cindil, E.; Kilic, K.; Ilgit, E.; Onal, B.; Erbas, G. Misplaced central venous catheter in the vertebral artery: Endovascular treatment of foreseen hemorrhage during catheter withdrawal. J. Vasc. Access 2014, 15, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Akyuz, M.; Gokalp, O.; Ozcem, B.; Ozcan, S.; Besir, Y.; Gurbuz, A. Surgical management of axillosubclavian vascular injuries. Pak. J. Med. Sci. 2015, 31, 552–555. [Google Scholar] [CrossRef] [PubMed]
- Leonardou, P.; Pappas, P. Urgent endovascular treatment of iatrogenic subclavian artery rupture: Report of three cases. Ulus. Travma Acil Cerrahi Derg. 2012, 18, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Ben Mrad, I.; Ben Fatma, L.; Ben Mrad, M.; Miri, R.; Mleyhi, S.; Mami, I.; Zairi, I.; Denguir, R. Endovascular Management of a Subclavian Arterial Injury During Central Venous Catheter Placement for Hemodialysis. Open Access Emerg. Med. 2021, 13, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Jaldin, R.G.; Bertanha, M.; Sobreira, M.L.; Braz, L.G.; Freitas, C.C.M.; Yoshida, W.B.; Moura, R. Treatment of an iatrogenic subclavian artery pseudoaneurysm near vertebral artery branch: Endovascular approach or open surgery? J. Vasc. Bras. 2013, 12, 237–242. [Google Scholar] [CrossRef][Green Version]
- Mimura, H.; Gobara, H.; Hiraki, T.; Fujiwara, H.; Sarukai, J.; Sugiu, K.; Kanazawa, S. Percutaneous coil embolization using direct puncture technique for a subclavian artery pseudoaneurysm after inadvertent puncture. Cardiovasc. Interv. Radiol. 2009, 32, 371–373. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-W.; Nam, I.-C.; Kim, D.-R.; Kim, J.-J.; Park, S.-E. Subclavian Artery Pseudoaneurysm Following Bedside Temporary Hemodialysis Catheter Insertion: A Case Report. Medicina 2023, 59, 2038. https://doi.org/10.3390/medicina59112038
Kim S-W, Nam I-C, Kim D-R, Kim J-J, Park S-E. Subclavian Artery Pseudoaneurysm Following Bedside Temporary Hemodialysis Catheter Insertion: A Case Report. Medicina. 2023; 59(11):2038. https://doi.org/10.3390/medicina59112038
Chicago/Turabian StyleKim, Sang-Woo, In-Chul Nam, Doo-Ri Kim, Jeong-Jae Kim, and Sung-Eun Park. 2023. "Subclavian Artery Pseudoaneurysm Following Bedside Temporary Hemodialysis Catheter Insertion: A Case Report" Medicina 59, no. 11: 2038. https://doi.org/10.3390/medicina59112038
APA StyleKim, S.-W., Nam, I.-C., Kim, D.-R., Kim, J.-J., & Park, S.-E. (2023). Subclavian Artery Pseudoaneurysm Following Bedside Temporary Hemodialysis Catheter Insertion: A Case Report. Medicina, 59(11), 2038. https://doi.org/10.3390/medicina59112038






