Ultrasound Prevalence and Clinical Features of Nonalcoholic Fatty Liver Disease in Patients with Inflammatory Bowel Diseases: A Real-Life Cross-Sectional Study
Abstract
:1. Introduction
1.1. Crosstalk between IBD and NAFLD
1.2. Diagnostic Approaches in NAFLD
1.3. Aims
2. Materials and Methods
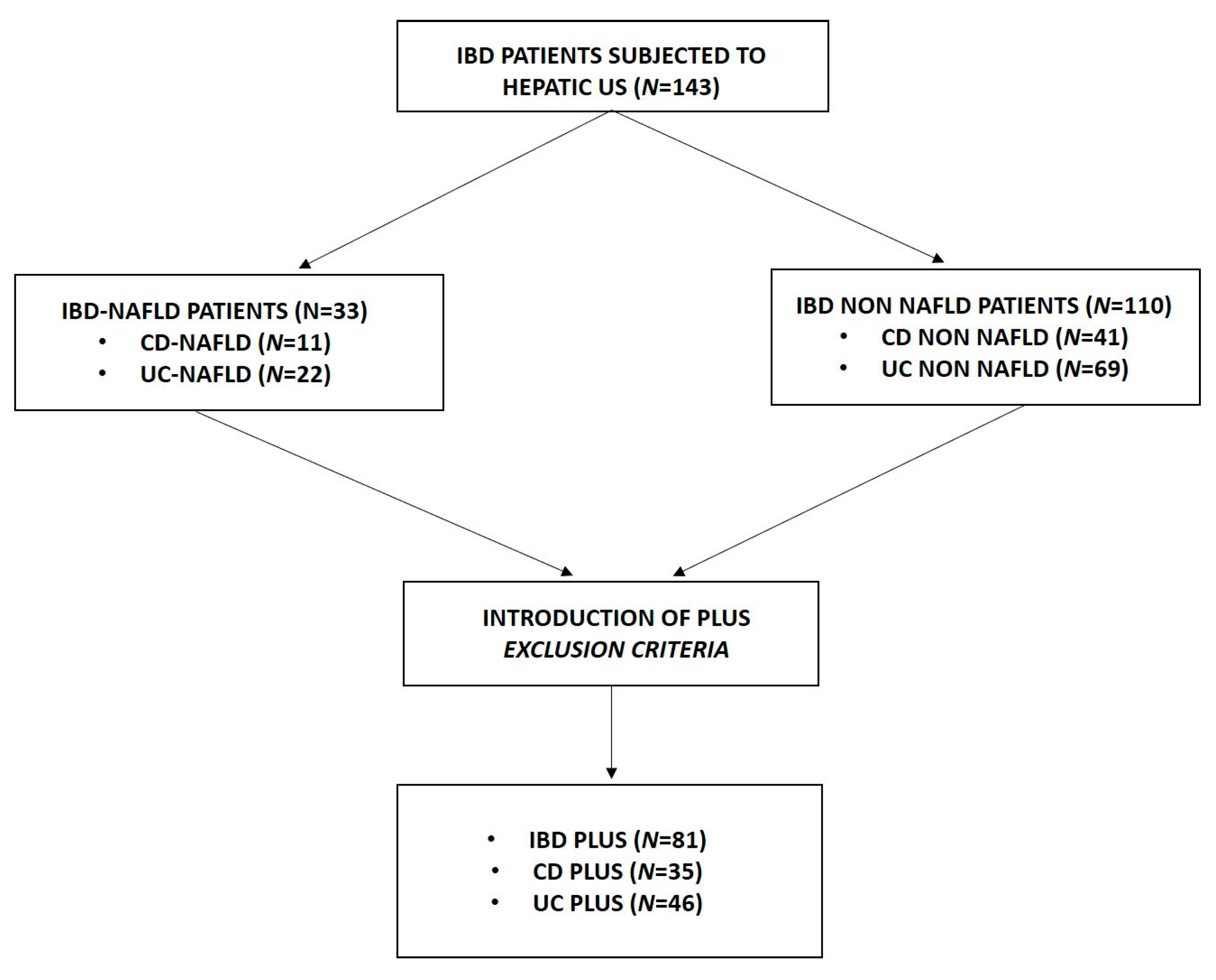
2.1. Patients
2.2. NAFLD Diagnosis
2.3. Study Design
2.4. Statistical Analysis
2.5. Ethics
3. Results
3.1. Characteristics of the Patients Enrolled
3.2. Comparison between IBD Patients
3.3. US Prevalence of NAFLD among IBD Patients
3.4. Comparison between IBD Patients with and without NAFLD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spagnuolo, R.; Larussa, T.; Iannelli, C.; Cosco, C.; Nisticò, E.; Manduci, E.; Bruno, A.; Boccuto, L.; Abenavoli, L.; Luzza, F.; et al. COVID-19 and Inflammatory Bowel Disease: Patient Knowledge and Perceptions in a Single Center Survey. Medicina 2020, 56, 407. [Google Scholar] [CrossRef] [PubMed]
- Malik, T.F.; Aurelio, D.M. Extraintestinal Manifestations of Inflammatory Bowel Disease. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Marotto, D.; Atzeni, F.; Ardizzone, S.; Monteleone, G.; Giorgi, V.; Sarzi-Puttini, P. Extra-intestinal manifestations of inflammatory bowel diseases. Pharmacol. Res. 2020, 161, 105206. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Domínguez, S.J.; García-Mateo, S.; Laredo, V.; Gargallo-Puyuelo, C.J.; Gallego Llera, B.; López de la Cruz, J.; Gomollón, F. Liver Fibrosis in Non-Alcoholic Fatty Liver Disease and Progression to Hepatocellular Carcinoma in Patients with Inflammatory Bowel Disease: A Systematic Review. Cancers 2023, 15, 3367. [Google Scholar] [CrossRef] [PubMed]
- Abenavoli, L.; Giubilei, L.; Procopio, A.C.; Spagnuolo, R.; Luzza, F.; Boccuto, L.; Scarpellini, E. Gut Microbiota in Non-Alcoholic Fatty Liver Disease Patients with Inflammatory Bowel Diseases: A Complex Interplay. Nutrients 2022, 14, 5323. [Google Scholar] [CrossRef]
- Glassner, K.; Malaty, H.M.; Abraham, B.P. Epidemiology and Risk Factors of Nonalcoholic Fatty Liver Disease among Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 998–1003. [Google Scholar] [CrossRef]
- Abenavoli, L.; Scarlata, G.G.M.; Scarpellini, E.; Boccuto, L.; Spagnuolo, R.; Tilocca, B.; Roncada, P.; Luzza, F. Metabolic-Dysfunction-Associated Fatty Liver Disease and Gut Microbiota: From Fatty Liver to Dysmetabolic Syndrome. Medicina 2023, 59, 594. [Google Scholar] [CrossRef]
- Spagnuolo, R.; Montalcini, T.; De Bonis, D.; Ferro, Y.; Cosco, C.; Mazza, E.; Romeo, S.; Doldo, P.; Pujia, A. Weight Gain and Liver Steatosis in Patients with Inflammatory Bowel Diseases. Nutrients 2019, 11, 303. [Google Scholar] [CrossRef]
- Hong, Q.; Shen, J.; Feng, Q.; Zheng, Q.; Qiao, Y. Prevalence and predictors of non-alcoholic liver disease on MRI among patients with Crohn’s disease. BMC Gastroenterol. 2022, 22, 183. [Google Scholar]
- Spagnuolo, R.; Abenavoli, L.; Corea, A.; Larussa, T.; Mancina, R.M.; Cosco, C.; Luzza, F.; Doldo, P. Multifaceted pathogenesis of liver steatosis in inflammatory bowel disease: A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 5818–5825. [Google Scholar]
- Principi, M.; Iannone, A.; Losurdo, G.; Mangia, M.; Shahini, E.; Albano, F.; Rizzi, S.F.; La Fortezza, R.F.; Lovero, R.; Contaldo, A.; et al. Nonalcoholic Fatty Liver Disease in Inflammatory Bowel Disease: Prevalence and Risk Factors. Inflamm. Bowel Dis. 2018, 24, 1589–1596. [Google Scholar] [CrossRef]
- Lin, A.; Roth, H.; Anyane-Yeboa, A.; Rubin, D.T.; Paul, S. Prevalence of Nonalcoholic Fatty Liver Disease in Patients with Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. Inflamm. Bowel Dis. 2021, 27, 947–955. [Google Scholar] [CrossRef] [PubMed]
- Chao, C.Y.; Battat, R.; Al Khoury, A.; Restellini, S.; Sebastiani, G.; Bessissow, T. Co-existence of non-alcoholic fatty liver disease and inflammatory bowel disease: A review article. World J. Gastroenterol. 2016, 22, 7727–7734. [Google Scholar] [CrossRef] [PubMed]
- Larussa, T.; Abenavoli, L.; Fabiano, G.; Mancuso, M.A.; Polimeni, N.; Dumitrascu, D.L.; Luzza, F. Gut microbiota in inflammatory bowel disease: A target for therapy not to be missed. Minerva Gastroenterol. 2021, 67, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Mancina, R.M.; Spagnuolo, R.; Milano, M.; Brogneri, S.; Morrone, A.; Cosco, C.; Lazzaro, V.; Russo, C.; Ferro, Y.; Pingitore, P.; et al. PNPLA3 148M Carriers with Inflammatory Bowel Diseases Have Higher Susceptibility to Hepatic Steatosis and Higher Liver Enzymes. Inflamm. Bowel Dis. 2016, 22, 134–140. [Google Scholar] [CrossRef]
- Bessissow, T.; Le, N.H.; Rollet, K.; Afif, W.; Bitton, A.; Sebastiani, G. Incidence and Predictors of Nonalcoholic Fatty Liver Disease by Serum Biomarkers in Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2016, 22, 1937–1944. [Google Scholar] [CrossRef]
- Kablawi, D.; Aljohani, F.; Palumbo, C.S.; Restellini, S.; Bitton, A.; Wild, G.; Afif, W.; Lakatos, P.L.; Bessissow, T.; Sebastiani, G. Nonalcoholic Fatty Liver Disease Increases Cardiovascular Risk in Inflammatory Bowel Diseases. Crohns Colitis 360 2023, 5, otad004. [Google Scholar] [CrossRef]
- Rodriguez-Duque, J.C.; Calleja, J.L.; Iruzubieta, P.; Hernández-Conde, M.; Rivas-Rivas, C.; Vera, M.I.; Garcia, M.J.; Pascual, M.; Castro, B.; García-Blanco, A.; et al. Increased risk of MAFLD and Liver Fibrosis in Inflammatory Bowel Disease Independent of Classic Metabolic Risk Factors. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2023, 21, 406–414. [Google Scholar] [CrossRef]
- Mancina, R.M.; De Bonis, D.; Pagnotta, R.; Cosco, C.; Cosco, V.; Montalcini, T.; Pujia, A.; Doldo, P.; Spagnuolo, R. Ulcerative Colitis as an Independent Risk Factor for Hepatic Steatosis. Gastroenterol. Nurs. Off. J. Soc. Gastroenterol. Nurses Assoc. 2020, 43, 292–297. [Google Scholar] [CrossRef]
- Nguyen, D.L.; Bechtold, M.L.; Jamal, M.M. National trends and inpatient outcomes of inflammatory bowel disease patients with concomitant chronic liver disease. Scand. J. Gastroenterol. 2014, 49, 1091–1095. [Google Scholar] [CrossRef]
- Hamaguchi, M.; Kojima, T.; Itoh, Y.; Harano, Y.; Fujii, K.; Nakajima, T.; Kato, T.; Takeda, N.; Okuda, J.; Ida, K.; et al. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am. J. Gastroenterol. 2007, 102, 2708–2715. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Diehl, A.M.; Brunt, E.M.; Cusi, K.; Charlton, M.; Sanyal, A.J. The diagnosis and management of non-alcoholic fatty liver disease: Practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 2012, 55, 2005–2023. [Google Scholar] [CrossRef] [PubMed]
- Kobyliak, N.; Abenavoli, L. The role of liver biopsy to assess non-alcoholic fatty liver disease. Rev. Recent. Clin. Trials 2014, 9, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Abenavoli, L.; Beaugrand, M. Transient elastography in non-alcoholic fatty liver disease. Ann. Hepatol. 2012, 11, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.E.; Goh, G.B.; Ngu, J.H.; Tan, H.K.; Tan, C.K. Clinical applications, limitations and future role of transient elastography in the management of liver disease. World J. Gastrointest. Pharmacol. Ther. 2016, 7, 91–106. [Google Scholar] [CrossRef]
- Pouwels, S.; Sakran, N.; Graham, Y.; Leal, A.; Pintar, T.; Yang, W.; Kassir, R.; Singhal, R.; Mahawar, K.; Ramnarain, D. Non-alcoholic fatty liver disease (NAFLD): A review of pathophysiology, clinical management and effects of weight loss. BMC Endocr. Disord. 2022, 22, 63. [Google Scholar] [CrossRef]
- Şendur, H.N.; Cerit, M.N.; Ibrahimkhanli, N.; Şendur, A.B.; Özhan Oktar, S. Interobserver Variability in Ultrasound-Based Liver Fat Quantification. J. Ultrasound Med. 2023, 42, 833–841. [Google Scholar] [CrossRef]
- Zamani, M.; Alizadeh-Tabari, S.; Singh, S.; Loomba, R. Meta-analysis: Prevalence of, and risk factors for, non-alcoholic fatty liver disease in patients with inflammatory bowel disease. Aliment. Pharmacol. Ther. 2022, 55, 894–907. [Google Scholar] [CrossRef]
- Likhitsup, A.; Dundulis, J.; Ansari, S.; Patibandla, S.; Hutton, C.; Kennedy, K.; Helzberg, J.H.; Chhabra, R. High prevalence of non-alcoholic fatty liver disease in patients with inflammatory bowel disease receiving anti-tumor necrosis factor therapy. Ann. Gastroenterol. 2019, 32, 463–468. [Google Scholar] [CrossRef]
- Shintaku, D.; Lopes, M.; de Oliveira, A.C.; Beraldo, R.; Godoi, G.; Castelhano, N.; Pereira, J.; Vulcano, D.; de Oliveira, E.C.; Herrerias, G.; et al. P049 Investigation of Liver Diseases by Ultrasound in Patients with Inflammatory Bowel Disease. Am. J. Gastroenterol. 2021, 116, S12–S13. [Google Scholar] [CrossRef]
- Ferraioli, G.; Soares Monteiro, L.B. Ultrasound-based techniques for the diagnosis of liver steatosis. World J. Gastroenterol. 2019, 25, 6053–6062. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016, 64, 1388–1402. [Google Scholar] [CrossRef] [PubMed]
- Angelico, F.; Pastori, D.; Del Ben, M. Impact of the New Metabolic-Associated Fatty Liver Disease (MAFLD) on NAFLD Patients Classification in Italy. Clin. Gastroenterol. Hepatol. 2021, 19, 2683–2684. [Google Scholar] [CrossRef] [PubMed]
- Sagami, S.; Ueno, Y.; Tanaka, S.; Fujita, A.; Hayashi, R.; Oka, S.; Hyogo, H.; Chayama, K. Significance of non-alcoholic fatty liver disease in Crohn’s disease: A retrospective cohort study. Hepatol. Res. 2017, 47, 872–881. [Google Scholar] [CrossRef] [PubMed]
- Sourianarayanane, A.; Garg, G.; Smith, T.H.; Butt, M.I.; McCullough, A.J.; Shen, B. Risk factors of non-alcoholic fatty liver disease in patients with inflammatory bowel disease. J. Crohn’s Colitis 2013, 7, 279–285. [Google Scholar] [CrossRef]
- Scrivo, B.; Celsa, C.; Busacca, A.; Giuffrida, E.; Pipitone, R.M.; Grimaudo, S.; Calogero, C.; Petta, S.; Cappello, M. P162 Prevalence of NAFLD (nonalcoholic fatty liver disease) and fibrosis in inflammatory bowel disease: The impact of traditional risk factors, intestinal inflammation and genetic phenotype. J. Crohn’s Colitis 2020, 14, 219–220. [Google Scholar] [CrossRef]
- Eslam, M.; Sanyal, A.J.; George, J.; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020, 158, 1999–2014.e1. [Google Scholar] [CrossRef]
- Magrì, S.; Paduano, D.; Chicco, F.; Cingolani, A.; Farris, C.; Delogu, G.; Tumbarello, F.; Lai, M.; Melis, A.; Casula, L.; et al. Nonalcoholic fatty liver disease in patients with inflammatory bowel disease: Beyond the natural history. World J. Gastroenterol. 2019, 25, 5676–5686. [Google Scholar] [CrossRef]
- Hoffmann, P.; Jung, V.; Behnisch, R.; Gauss, A. Prevalence and risk factors of nonalcoholic fatty liver disease in patients with inflammatory bowel diseases: A cross-sectional and longitudinal analysis. World J. Gastroenterol. 2020, 26, 7367–7381. [Google Scholar] [CrossRef]
- Saroli Palumbo, C.; Restellini, S.; Chao, C.Y.; Aruljothy, A.; Lemieux, C.; Wild, G.; Afif, W.; Lakatos, P.L.; Bitton, A.; Cocciolillo, S.; et al. Screening for Nonalcoholic Fatty Liver Disease in Inflammatory Bowel Diseases: A Cohort Study Using Transient Elastography. Inflamm. Bowel Dis. 2019, 25, 124–133. [Google Scholar] [CrossRef]
- Sartini, A.; Gitto, S.; Bianchini, M.; Verga, M.C.; Di Girolamo, M.; Bertani, A.; Del Buono, M.; Schepis, F.; Lei, B.; De Maria, N.; et al. Non-alcoholic fatty liver disease phenotypes in patients with inflammatory bowel disease. Cell Death Dis. 2018, 9, 87. [Google Scholar] [CrossRef]
- Cho, C.W.; You, M.W.; Oh, C.H.; Lee, C.K.; Moon, S.K. Long-term Disease Course of Crohn’s Disease: Changes in Disease Location, Phenotype, Activities, and Predictive Factors. Gut Liver 2022, 16, 57–170. [Google Scholar] [CrossRef] [PubMed]
- Kodali, A.; Okoye, C.; Klein, D.; Mohamoud, I.; Olanisa, O.O.; Parab, P.; Chaudhary, P.; Mukhtar, S.; Moradi, A.; Hamid, P. Crohn’s Disease is a Greater Risk Factor for Nonalcoholic Fatty Liver Disease Compared to Ulcerative Colitis: A Systematic Review. Cureus 2023, 15, e42995. [Google Scholar] [CrossRef] [PubMed]
- Papaefthymiou, A.; Potamianos, S.; Goulas, A.; Doulberis, M.; Kountouras, J.; Polyzos, S.A. Inflammatory Bowel Disease-associated Fatty Liver Disease: The Potential Effect of Biologic Agents. J. Crohn’s Colitis 2022, 16, 852–862. [Google Scholar] [CrossRef]
- Mitrovic, M.; Marković, S.; Kalaba, A.; Zarić, D.; Kralj, D.; Milić, A.; Svorcan, P. The effect of anti-TNF-α and anti-integrin agents on liver steatosis in inflammatory bowel disease patients with non-alcoholic fatty liver disease. J. Crohn’s Colitis 2023, 17, i837. [Google Scholar] [CrossRef]
- Zarghamravanbakhsh, P.; Frenkel, M.; Poretsky, L. Metabolic causes and consequences of nonalcoholic fatty liver disease (NAFLD). Metabol. Open 2021, 12, 100149, Erratum in Metabol. Open 2023, 17, 100231. [Google Scholar] [CrossRef] [PubMed]

| IBD (N = 143) | CD (N = 52) | UC (N = 91) | |
|---|---|---|---|
| Demographic and Anthropometric | |||
| Age (years) | 45 ± 16 | 44 ± 17 | 45 ± 15 |
| Male gender, n (%) | 82 (57) | 31 (60) | 51 (56) |
| Active smoker, n (%) | 4 (3) | 3 (6) | 1 (1) |
| BMI (kg/m2) | 25 ± 4 | 24 ± 4 | 25 ± 5 |
| Waist circumference (cm) | 91 ± 12 | 89 ± 11 | 91 ± 13 |
| Disease characteristic | |||
| Disease duration (years) | 12 ± 9 | 13 ± 9 | 11 ± 10 |
| Age at onset (years) | 33 ± 15 | 34 ± 13 | 32 ± 14 |
| CD (Harvey–Bradshaw index) | - | 7 ± 3 | - |
| UC (full Mayo Score) | - | - | 2 ± 0.7 |
| Relapse/year | 1.3 ± 0.7 | 1.3 ± 0.9 | 1.2 ± 0.7 |
| Active disease, n (%) | 47 (33) | 27 (52) | 20 (22) |
| Extraintestinal manifestations, n (%) | 26 (18) | 13 (25) | 13 (14) |
| NAFLD, n (%) | 33 (23) | 11 (21) | 22 (24) |
| Mild steatosis, n (%) | 24 (17) | 6 (11) | 18 (20) |
| Moderate steatosis, n (%) | 6 (4) | 4 (8) | 2 (2) |
| Severe steatosis, n (%) | 3 (2) | 1 (2) | 2 (2) |
| Surgery, n (%) | 24 (17) | 17 (33) | 7 (8) |
| CD disease location and phenotype, n (%) | |||
| Ileal | - | 21 (41) | - |
| Colonic | - | 8 (15) | - |
| Ileo–colonic | - | 22 (42) | - |
| Upper GI | - | 1 (2) | - |
| Inflammatory | - | 16 (31) | - |
| Fistulizing | - | 15 (29) | - |
| Stenosing | - | 21 (40) | - |
| UC disease location, n (%) | |||
| Proctitis | - | - | 8 (8) |
| Proctosigmoiditis | - | - | 19 (21) |
| Left side | - | - | 16 (17) |
| Pancolitis | - | - | 48 (54) |
| Dysmetabolic comorbidities, n (%) | |||
| T2DM | 11 (8) | 1 (2) | 10 (11) |
| Hypertension | 24 (17) | 8 (15) | 16 (18) |
| Dyslipidemia | 18 (13) | 5 (10) | 13 (14) |
| IBD plus dysmetabolic criteria | 81 (57) | 35 (67) | 46 (50) |
| Laboratory parameters | |||
| ALT (UI/L) | 19 ± 10 | 18 ± 9 | 20 ± 11 |
| AST (UI/L) | 20 ± 9 | 22 ± 9 | 21 ± 10 |
| Total cholesterol (mg/dL) | 168 ± 42 | 167 ± 41 | 168 ± 43 |
| LDL (mg/dL) | 104 ± 35 | 103 ± 34 | 105 ± 35 |
| HDL (mg/dL) | 56 ± 17 | 55 ± 17 | 56 ± 16 |
| Triglycerides (mg/dL) | 99 ± 48 | 99 ± 49 | 100 ± 48 |
| Fasting blood glucose (mg/dL) | 88 ± 20 | 87 ± 19 | 89 ± 21 |
| Fasting insulinemia (mg/dL) | 10 ± 7 | 10 ± 8 | 9 ± 8 |
| HOMA-IR | 2 ± 2 | 2 ± 1 | 2 ± 3 |
| Fecal calprotectin (mcg/gr) | 501 ± 797 | 492 ± 802 | 509 ± 804 |
| Medication, n (%) | |||
| Salicylates, n (%) | 75 (52) | 24 (46) | 51 (56) |
| Azathioprine, n (%) | 47 (33) | 16 (31) | 31 (34) |
| >3 cycles of steroids, n (%) | 34 (24) | 9 (17) | 25 (27) |
| Biological therapy, n (%) | 86 (60) | 33 (63) | 53 (58) |
| Anti-TNF-α, n (%) | 61 (71) | 25 (76) | 36 (68) |
| Vedolizumab, n (%) | 16 (19) | 2 (6) | 14 (26) |
| Ustekinumab, n (%) | 9 (10) | 6 (18) | 3 (6) |
| >1 Biological drug, n (%) | 23 (16) | 4 (8) | 19 (21) |
| Current biological therapy duration (years) | 3 ± 2 | 4 ± 2 | 2 ± 2 |
| Total biological therapy duration (years) | 5 ± 4 | 4 ± 3 | 4 ± 2 |
| IBD–NAFLD (N = 33) | IBD Non-NAFLD (N = 110) | p-Value | |
|---|---|---|---|
| Demographic and Anthropometric | |||
| Age (years) | 53 ± 13 | 43 ± 17 | 0.03 |
| Male gender, n (%) | 24 (73) | 58 (53) | 0.047 |
| Active smoker, n (%) | 0 | 4 (4) | 0.266 |
| BMI (kg/m2) | 27 ± 5 | 24 ± 4 | <0.001 |
| Waist circumference (cm) | 100 ± 11 | 88 ± 11 | <0.001 |
| Disease characteristic | |||
| Disease duration (years) | 15 ± 10 | 11 ± 9 | 0.044 |
| Age at onset (years) | 38 ± 16 | 32 ± 15 | 0.047 |
| CD, n (%) | 11 (33) | 41 (37) | 0.837 |
| UC, n (%) | 22 (66) | 69 (63) | 0.830 |
| CD (Harvey–Bradshaw index) | 5 ± 2 | 7 ± 3 | 0.033 |
| UC (full Mayo Score) | 2 ± 0.6 | 2 ± 0.8 | 0.612 |
| Relapse/year | 1.3 ± 0.7 | 1.3 ± 0.8 | 1.000 |
| Active disease, n (%) | 12 (36) | 35 (32) | 0.675 |
| Extraintestinal manifestations, n (%) | 7 (21) | 19 (17) | 0.612 |
| Surgery, n (%) | 7 (21) | 17 (15) | 0.435 |
| CD disease location and phenotype, n (%) | |||
| Ileal * | 3 (27) | 18 (44) | 0.30 |
| Colonic * | 1 (9) | 7 (17) | 0.51 |
| Ileo–colonic * | 7 (64) | 15 (37) | 0.106 |
| Upper GI * | 0 | 1 (2) | 0.60 |
| Inflammatory * | 1 (9) | 16 (39) | 0.06 |
| Fistulizing * | 3 (27) | 13 (32) | 0.70 |
| Stenosing * | 7 (64) | 12 (29) | 0.035 |
| UC disease location, n (%) | |||
| Proctitis * | 0 | 8 (12) | 0.09 |
| Proctosigmoiditis * | 2 (9) | 17 (25) | 0.11 |
| Left side * | 7 (32) | 9 (13) | 0.044 |
| Pancolitis * | 13 (59) | 35 (50) | 0.42 |
| Dysmetabolic comorbidities, n (%) | |||
| T2DM | 4 (12) | 7 (7) | 0.278 |
| Hypertension | 13 (39) | 11 (10) | <0.001 |
| Dyslipidemia | 5 (15) | 13 (12) | 0.564 |
| IBD plus dysmetabolic criteria | 26 (78) | 36 (33) | <0.001 |
| Laboratory parameter | |||
| ALT (UI/L) | 22 ± 10 | 18 ± 9 | 0.034 |
| AST (UI/L) | 22 ± 10 | 20 ± 9 | 0.187 |
| Total cholesterol (mg/dL) | 168 ± 47 | 167 ± 40 | 0.994 |
| LDL (mg/dL) | 107 ± 38 | 103 ± 33 | 0.591 |
| HDL (mg/dL) | 48 ± 16 | 58 ± 17 | 0.005 |
| Triglycerides (mg/dL) | 123 ± 63 | 93 ± 40 | 0.002 |
| Fasting blood glucose (mg/dL) | 92 ± 25 | 87 ± 18 | 0.156 |
| Fasting insulinemia (mg/dL) | 10 ± 8 | 10 ± 7 | 0.106 |
| HOMA-IR | 3 ± 2 | 2 ± 2 | 0.078 |
| Fecal calprotectin (mcg/gr) | 439 ± 911 | 519 ± 764 | 0.613 |
| Medication, n (%) | |||
| Salicylates, n (%) | 20 (61) | 55 (50) | 0.324 |
| Azathioprine, n (%) | 10 (30) | 37 (33) | 0.834 |
| >3 cycles of steroids, n (%) | 9 (27) | 25 (23) | 0.643 |
| Biological therapy, n (%) | 17 (51) | 69 (63) | 0.311 |
| Anti-TNF-α, n (%) | 15 (88) | 46 (67) | 0.841 |
| Vedolizumab, n (%) | 0 | 16 (23) | 0.023 |
| Ustekinumab, n (%) | 2 (12) | 7 (10) | 1.000 |
| >1 Biological drug, n (%) | 5 (15) | 18 (16) | 1.000 |
| Current biological therapy duration (years) | 4 ± 3 | 3 ± 2 | 0.188 |
| Total biological therapy duration (years) | 5 ± 3 | 4 ± 3 | 0.251 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abenavoli, L.; Spagnuolo, R.; Scarlata, G.G.M.; Scarpellini, E.; Boccuto, L.; Luzza, F. Ultrasound Prevalence and Clinical Features of Nonalcoholic Fatty Liver Disease in Patients with Inflammatory Bowel Diseases: A Real-Life Cross-Sectional Study. Medicina 2023, 59, 1935. https://doi.org/10.3390/medicina59111935
Abenavoli L, Spagnuolo R, Scarlata GGM, Scarpellini E, Boccuto L, Luzza F. Ultrasound Prevalence and Clinical Features of Nonalcoholic Fatty Liver Disease in Patients with Inflammatory Bowel Diseases: A Real-Life Cross-Sectional Study. Medicina. 2023; 59(11):1935. https://doi.org/10.3390/medicina59111935
Chicago/Turabian StyleAbenavoli, Ludovico, Rocco Spagnuolo, Giuseppe Guido Maria Scarlata, Emidio Scarpellini, Luigi Boccuto, and Francesco Luzza. 2023. "Ultrasound Prevalence and Clinical Features of Nonalcoholic Fatty Liver Disease in Patients with Inflammatory Bowel Diseases: A Real-Life Cross-Sectional Study" Medicina 59, no. 11: 1935. https://doi.org/10.3390/medicina59111935
APA StyleAbenavoli, L., Spagnuolo, R., Scarlata, G. G. M., Scarpellini, E., Boccuto, L., & Luzza, F. (2023). Ultrasound Prevalence and Clinical Features of Nonalcoholic Fatty Liver Disease in Patients with Inflammatory Bowel Diseases: A Real-Life Cross-Sectional Study. Medicina, 59(11), 1935. https://doi.org/10.3390/medicina59111935










