Successful Ultrasound-Guided Superficial Cervical Plexus Block Treatment for Head and Neck Pain with an Unusually Delayed Onset Following Ventriculoperitoneal Shunt: A Case Report
Abstract
1. Introduction
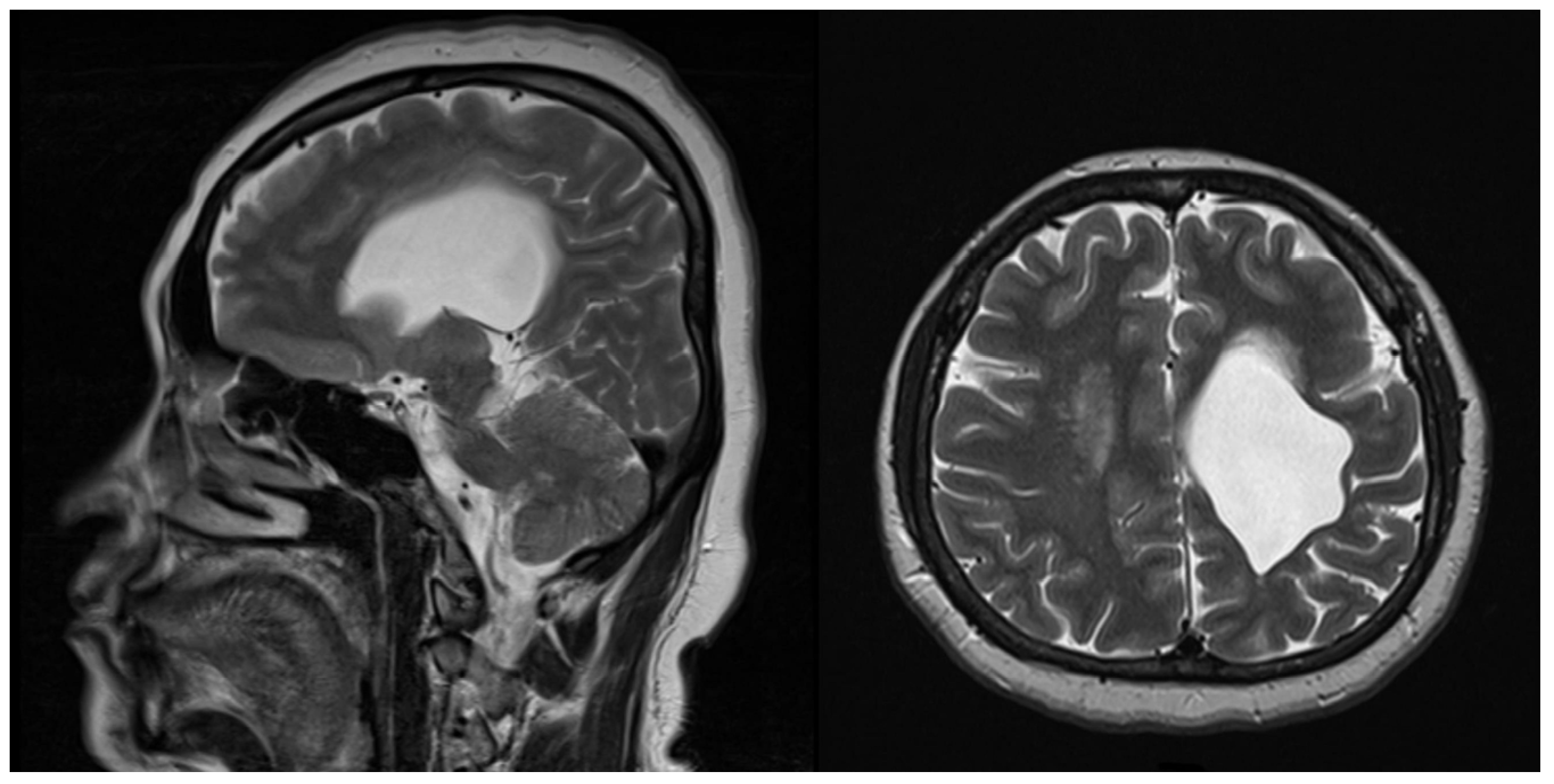
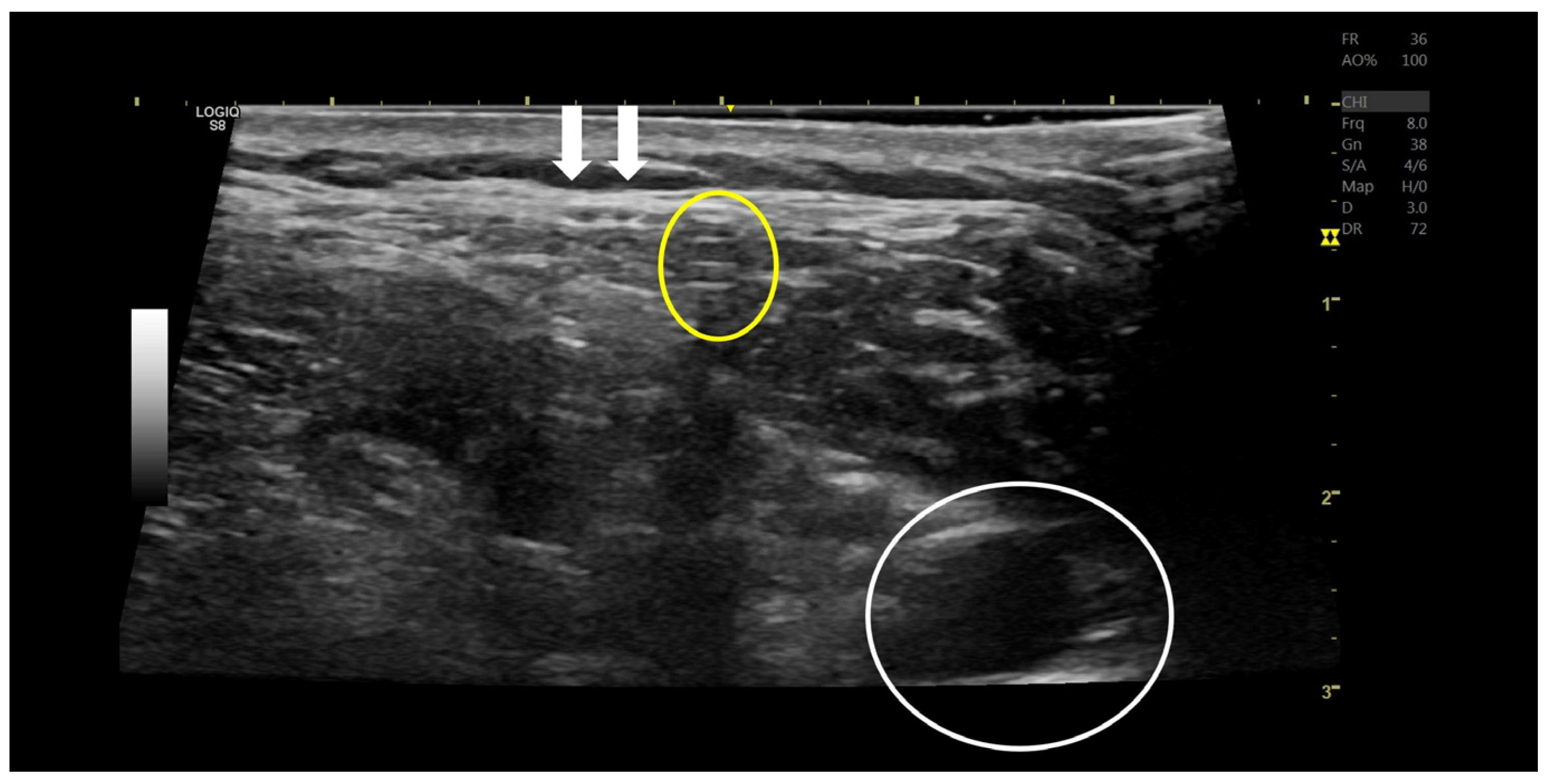
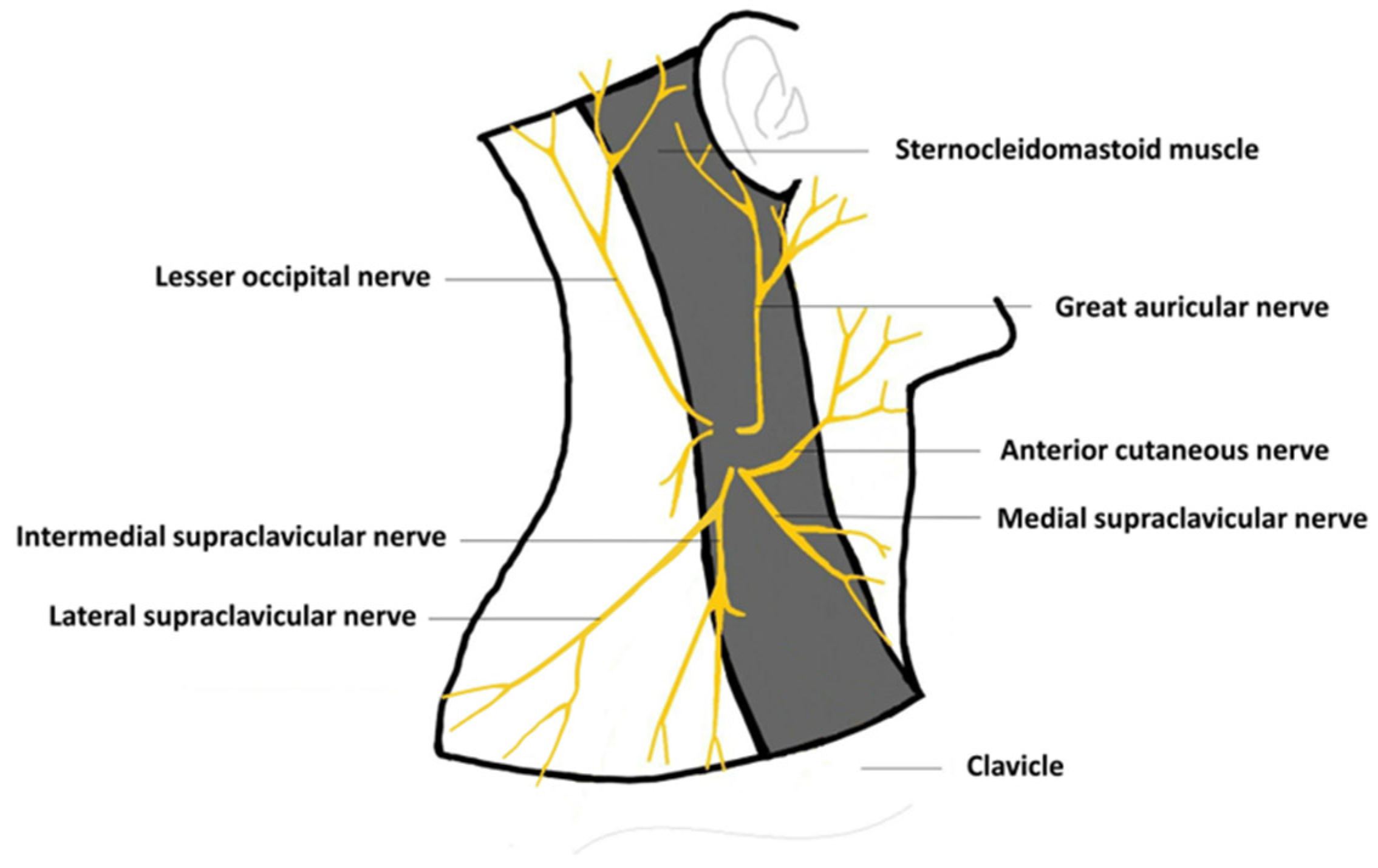
2. Case Description
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reddy, G.K.; Bollam, P.; Caldito, G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. 2014, 81, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Desai, V.R.; Sadrameli, S.S.; Jenson, A.V.; Asante, S.K.; Daniels, B.; Trask, T.W.; Britz, G. Ventriculoperitoneal shunt complications in an adult population: A comparison of various shunt designs to prevent overdrainage. Surg. Neurol. Int. 2020, 11, 269. [Google Scholar] [CrossRef] [PubMed]
- Korinek, A.M.; Fulla-Oller, L.; Boch, A.L.; Golmard, J.L.; Hadiji, B.; Puybasset, L. Morbidity of ventricular cerebrospinal fluid shunt surgery in adults: An 8-year study. Neurosurgery 2011, 68, 985–995. [Google Scholar] [CrossRef] [PubMed]
- Paff, M.; Alexandru-Abrams, D.; Muhonen, M.; Loudon, W. Ventriculoperitoneal shunt complications: A review. Interdiscip. Neurosurg. 2018, 13, 66–70. [Google Scholar] [CrossRef]
- Talamantes, Y.G.; Reséndiz, G.E.Á.; Grossgerge, E.K.; Vidales, J.C.B.; Hernandez, M.N.L. Superficial Cervical Plexus block and Ultrasound-guided styloid process infiltration in Eagle Syndrome. Anesth. Crit. Care 2021, 3, 21–28. [Google Scholar] [CrossRef]
- Lim, C.; O’Sullivan, M.G.J. Shoulder tip pain: An under-reported complication of ventriculoperitoneal shunt. Br. J. Neurosurg. 2005, 19, 354–356. [Google Scholar] [CrossRef]
- Acharya, R.; Ramachandran, C.S.; Singh, S. Laparoscopic management of abdominal complications in ventriculoperitoneal shunt surgery. J. Laparoendosc. Adv. Surg. Tech. 2001, 11, 167–170. [Google Scholar] [CrossRef]
- Ferras, M.; McCauley, N.; Stead, T.; Ganti, L.; Desai, B. Ventriculoperitoneal shunts in the emergency department: A Review. Cureus 2020, 12, e6857. [Google Scholar] [CrossRef]
- Nitin, B.; Gupta, M.; Singh, A. Pseudocyst in neck: A case report on rare complication of ventriculoperitoneal shunt. Case Rep. Otolaryngol. 2021, 2021, 6656506. [Google Scholar] [CrossRef]
- Tubbs, R.S.; Wellons, J.C., 3rd; Blount, J.P.; Grabb, P.A.; Oakes, W.J. Referred shoulder pain from ventriculoperitoneal shunts. Report of three cases. J. Neurosurg. 2005, 102 (Suppl. 2), 218–220. [Google Scholar] [CrossRef]
- Bakal, Ü.; Poyraz, A.K.; Tartar, T.; AkdenİZ, İ.; Sürme, M.B.; Çelik, S.; Saraç, M. A rare complication of ventriculoperitoneal shunt: Asymptomatic small bowel perforation. Istanb. Med. J. 2019, 20, 571–573. [Google Scholar] [CrossRef]
- Borkar, S.A.; Satyarthee, G.D.; Khan, R.N.; Sharma, B.S.; Mahapatra, A.K. Spontaneous extrusion of migrated ventriculoperitoneal shunt catheter through chest wall: A case report. Turk. Neurosurg. 2008, 18, 95–98. [Google Scholar] [PubMed]
- Aparici-Robles, F.; Molina-Fabrega, R. Abdominal cerebrospinal fluid pseudocyst: A complication of ventriculoperitoneal shunts in adults. J. Med. Imaging Radiat. Oncol. 2008, 52, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Santos de Oliveira, R.; Barbosa, A.; Vicente, Y.A.D.M.V.D.A.; Rubens Machado, H. An alternative approach for management of abdominal cerebrospinal fluid pseudocysts in children. Childs Nerv. Syst. 2007, 23, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Van Suijlekom, H.; Van Zundert, J.; Narouze, S.; Van Kleef, M.; Mekhail, N. 6 Cervicogenic headache. Pain Pract. 2010, 10, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Antonaci, F.; Bono, G.; Chimento, P. Diagnosing cervicogenic headache. J. Headache Pain 2006, 7, 145–148. [Google Scholar] [CrossRef][Green Version]
- Kessler, L.A.; Abla, A. Syndrome of the cervical plexus caused by high cervical nerve root compression. Neurosurgery 1991, 28, 506–509. [Google Scholar] [CrossRef]
- Oraee-Yazdani, S.; Kabiri, M.; Oraee-Yazdani, M.; Zali, A.R. Right upper quadrant abdominal pain due to malposition of the tip of the distal catheter of ventriculoperitoneal shunt. Interdiscip. Neurosurg. 2018, 14, 70–71. [Google Scholar] [CrossRef]
- Rizk, E.; Dias, M.S.; Verbrugge, J.; Boop, F.A. Intracardiac migration of a distal shunt catheter: An unusual complication of ventricular shunts. Report of 2 cases. J. Neurosurg. Pediatr. 2009, 3, 525–528. [Google Scholar] [CrossRef]
- Kullmann, M.; Khachatryan, M.; Schuhmann, M.U. Ultrasound-guided placement of ventricular catheters in first-time pediatric VP shunt surgery. Childs Nerv. Syst. 2018, 34, 465–471. [Google Scholar] [CrossRef]
- Beez, T.; Sarikaya-Seiwert, S.; Steiger, H.J.; Hänggi, D. Real-time ultrasound guidance for ventricular catheter placement in pediatric cerebrospinal fluid shunts. Childs Nerv. Syst. 2015, 31, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Connolly, E.S.; McKhann, G.M.; Huang, J.; Choudhri, T.F.; Komotar, R.J. Fundamentals of Operative Techniques in Neurosurgery; Thieme: New York, NY, USA, 2010. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, C.-Y.; Huang, Y.-Z.; Tsai, S.-T.; Wang, P.-K. Successful Ultrasound-Guided Superficial Cervical Plexus Block Treatment for Head and Neck Pain with an Unusually Delayed Onset Following Ventriculoperitoneal Shunt: A Case Report. Medicina 2023, 59, 1909. https://doi.org/10.3390/medicina59111909
Hu C-Y, Huang Y-Z, Tsai S-T, Wang P-K. Successful Ultrasound-Guided Superficial Cervical Plexus Block Treatment for Head and Neck Pain with an Unusually Delayed Onset Following Ventriculoperitoneal Shunt: A Case Report. Medicina. 2023; 59(11):1909. https://doi.org/10.3390/medicina59111909
Chicago/Turabian StyleHu, Ching-Yuan, Ying-Zhen Huang, Sheng-Tzung Tsai, and Po-Kai Wang. 2023. "Successful Ultrasound-Guided Superficial Cervical Plexus Block Treatment for Head and Neck Pain with an Unusually Delayed Onset Following Ventriculoperitoneal Shunt: A Case Report" Medicina 59, no. 11: 1909. https://doi.org/10.3390/medicina59111909
APA StyleHu, C.-Y., Huang, Y.-Z., Tsai, S.-T., & Wang, P.-K. (2023). Successful Ultrasound-Guided Superficial Cervical Plexus Block Treatment for Head and Neck Pain with an Unusually Delayed Onset Following Ventriculoperitoneal Shunt: A Case Report. Medicina, 59(11), 1909. https://doi.org/10.3390/medicina59111909





