Percutaneous Vertebroplasty in a Patient with Chronic Back Pain Caused by Multiple Schmorl’s Nodes: A Case Report
Abstract
:1. Introduction
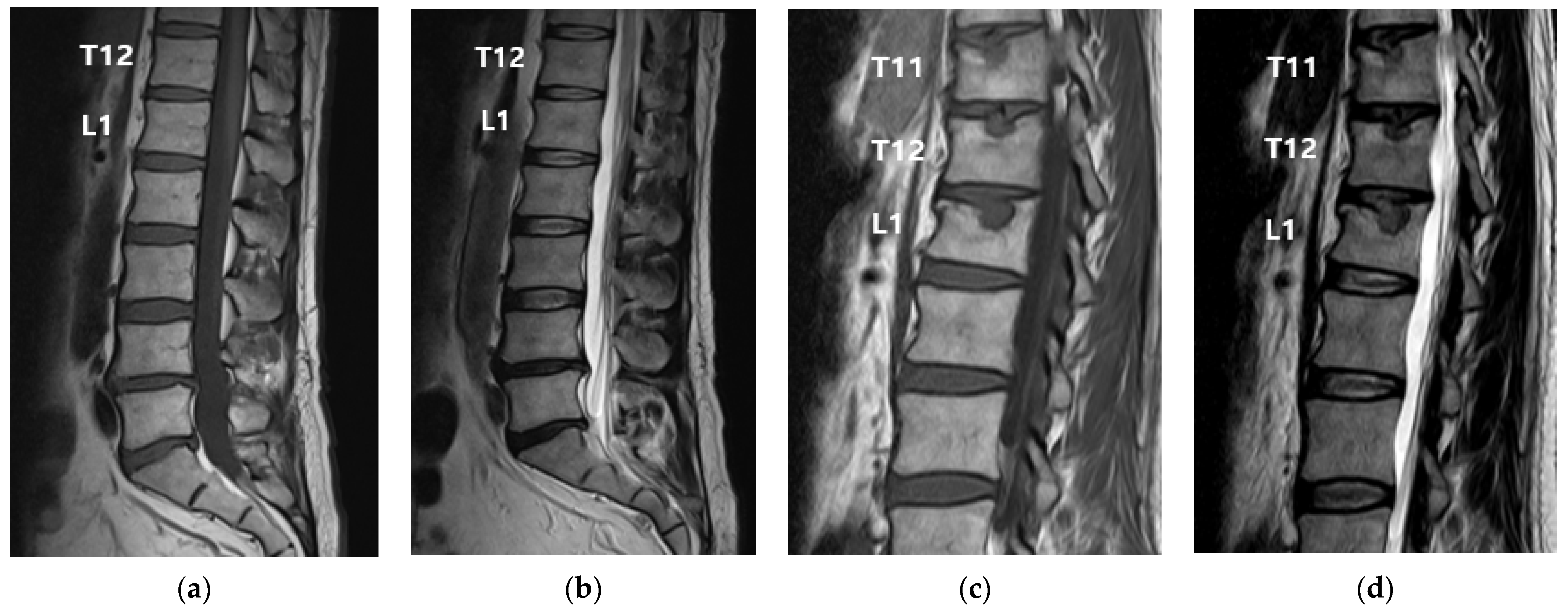
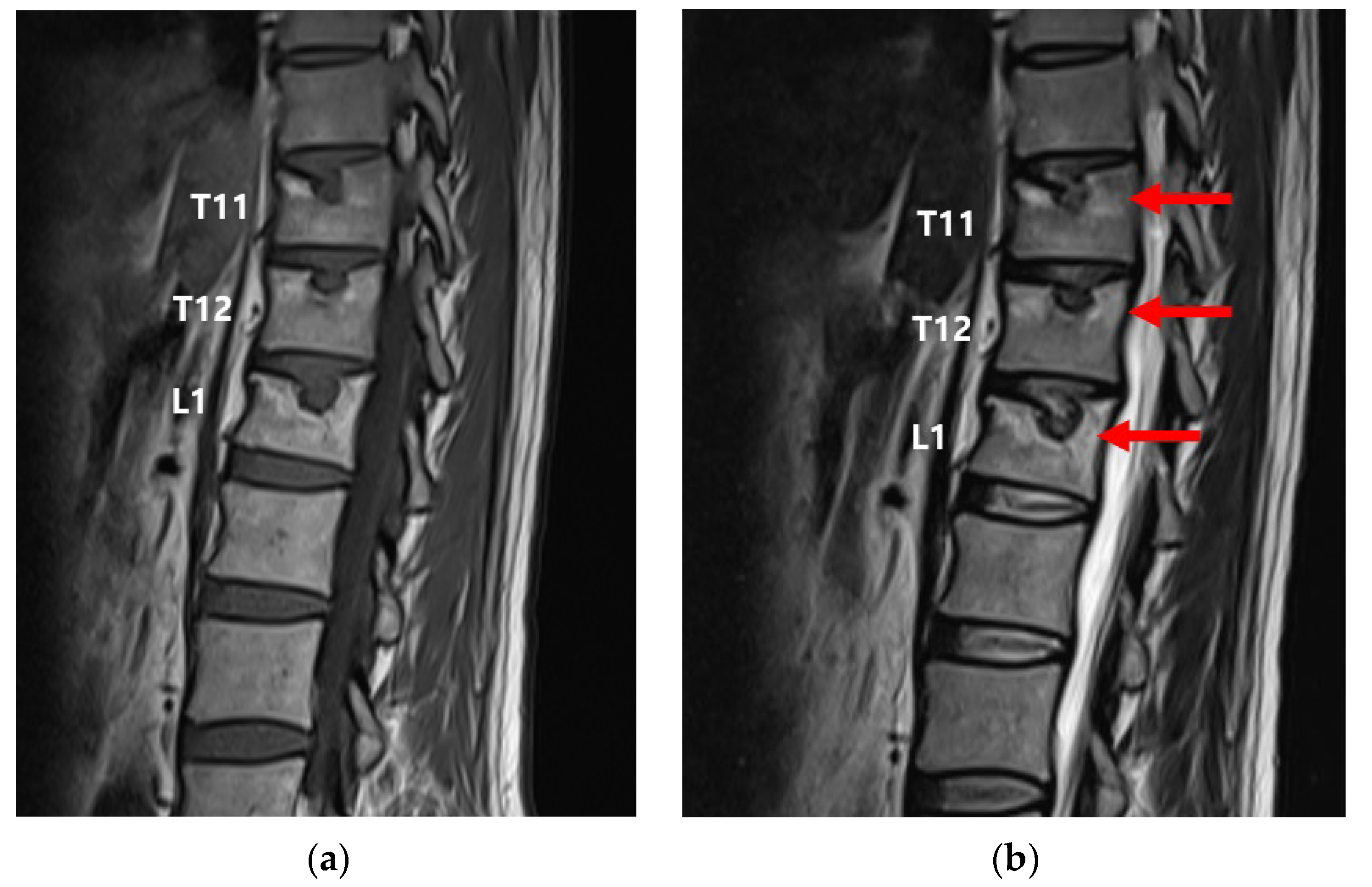
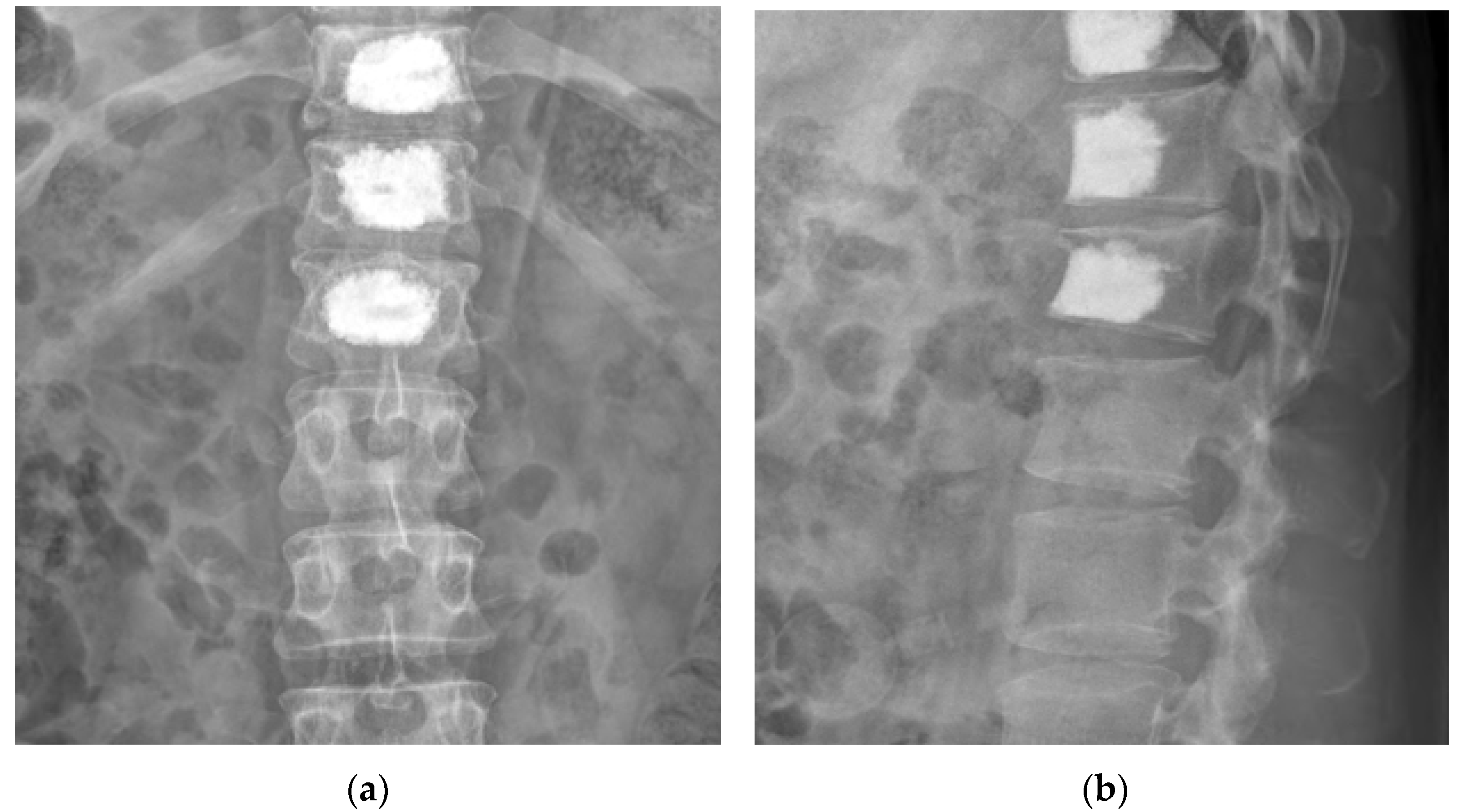
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kyere, K.A.; Than, K.D.; Wang, A.C.; Rahman, S.U.; Valdivia-Valdivia, J.M.; La Marca, F.; Park, P. Schmorl’s nodes. Eur. Spine J. 2012, 21, 2115–2121. [Google Scholar] [CrossRef]
- Peng, B.; Wu, W.; Hou, S.; Shang, W.; Wang, X.; Yang, Y. The pathogenesis of Schmorl’s nodes. J. Bone Joint. Surg Br. 2003, 85, 879–882. [Google Scholar] [CrossRef] [PubMed]
- Williams, F.M.; Manek, N.J.; Sambrook, P.N.; Spector, T.D.; Macgregor, A.J. Schmorl’s nodes: Common, highly heritable, and related to lumbar disc disease. Arthritis Rheum. 2007, 57, 855–860. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yin, P.; Yang, J.; Hai, Y. Percutaneous vertebroplasty (PVP) to treat a specialized type of endplate fractures around the Schmorl’s node: A prospective study of 65 patients. J. Orthop. Surg. Res. 2020, 15, 397. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Miyazaki, T.; Ohnari, H.; Takino, T.; Tomita, K. Schmorl’s nodes and low-back pain. Analysis of magnetic resonance imaging findings in symptomatic and asymptomatic individuals. Eur. Spine J. 1995, 4, 56–59. [Google Scholar] [CrossRef]
- Masala, S.; Pipitone, V.; Tomassini, M.; Massari, F.; Romagnoli, A.; Simonetti, G. Percutaneous vertebroplasty in painful schmorl nodes. Cardiovasc. Intervent. Radiol. 2006, 29, 97–101. [Google Scholar] [CrossRef]
- Hasegawa, K.; Ogose, A.; Morita, T.; Hirata, Y. Painful Schmorl’s node treated by lumbar interbody fusion. Spinal Cord 2004, 42, 124–128. [Google Scholar] [CrossRef]
- Jang, J.S.; Kwon, H.K.; Lee, J.J.; Hwang, S.M.; Lim, S.Y. Rami communicans nerve block for the treatment of symptomatic Schmorl’s nodes—A case report. Korean J. Pain 2010, 23, 262–265. [Google Scholar] [CrossRef]
- Liu, J.; Hao, L.; Zhang, X.; Shan, Z.; Li, S.; Fan, S.; Zhao, F. Painful Schmorl’s nodes treated by discography and discoblock. Eur. Spine J. 2018, 27, 13–18. [Google Scholar] [CrossRef]
- Phillips, F.M. Minimally invasive treatments of osteoporotic vertebral compression fractures. Spine 2003, 28, S45–S53. [Google Scholar] [CrossRef]
- Wu, H.T.; Morrison, W.B.; Schweitzer, M.E. Edematous Schmorl’s nodes on thoracolumbar MR imaging: Characteristic patterns and changes over time. Skeletal Radiol. 2006, 35, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Maynard, A.S.; Jensen, M.E.; Schweickert, P.A.; Marx, W.F.; Short, J.G.; Kallmes, D.F. Value of bone scan imaging in predicting pain relief from percutaneous vertebroplasty in osteoporotic vertebral fractures. AJNR Am. J. Neuroradiol. 2000, 21, 1807–1812. [Google Scholar] [PubMed]
- Jordan, E.; Choe, D.; Miller, T.; Chamarthy, M.; Brook, A.; Freeman, L.M. Utility of bone scintigraphy to determine the appropriate vertebral augmentation levels. Clin. Nucl. Med. 2010, 35, 687–691. [Google Scholar] [CrossRef]
- Kim, S.; Jang, S. Radicular pain caused by Schmorl’s node: A case report. Braz. J. Anesthesiol. 2018, 68, 322–324. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Li, F.C.; Huang, Y.J.; Teng, C.; Chen, W.S. Possible key role of the immune system in Schmorl’s nodes. Med. Hypotheses 2010, 74, 552–554. [Google Scholar] [CrossRef] [PubMed]
- Amoretti, N.; Guinebert, S.; Kastler, A.; Torre, F.; Andreani, O.; Foti, P.; Cornelis, F.; Theumann, N.; Hauger, O. Symptomatic Schmorl’s nodes: Role of percutaneous vertebroplasty. Open study on 52 patients. Neuroradiology 2019, 61, 405–410. [Google Scholar] [CrossRef]
- Cai, K.; Jiang, G.; Lu, B.; Zhang, K.; Luo, K. Bone cement distribution may significantly affect the efficacy of percutaneous vertebroplasty in treating symptomatic Schmorl’s nodes. BMC Musculoskelet. Disord. 2023, 24, 473. [Google Scholar] [CrossRef]
- Mattei, T.A.; Rehman, A.A. Schmorl’s nodes: Current pathophysiological, diagnostic, and therapeutic paradigms. Neurosurg. Rev. 2014, 37, 39–46. [Google Scholar] [CrossRef]
- Hershkovich, O.; Koch, J.E.; Grevitt, M.P. Schmorl Node-A Cause of Acute Thoracic Pain: A Case Report and Pathophysiological Mechanism. Int. J. Spine Surg. 2020, 14, 441–446. [Google Scholar] [CrossRef]
- Abu-Ghanem, S.; Ohana, N.; Abu-Ghanem, Y.; Kittani, M.; Shelef, I. Acute Schmorl node in the dorsal spine: An unusual cause of a sudden onset of severe back pain in a young female. Asian Spine J. 2013, 7, 131–135. [Google Scholar] [CrossRef]
- He, S.C.; Zhong, B.Y.; Zhu, H.D.; Fang, W.; Chen, L.; Guo, J.H.; Deng, G.; Teng, G.J. Percutaneous Vertebroplasty for Symptomatic Schmorl’s Nodes: 11 Cases with Long-term Follow-up and a Literature Review. Pain Physician 2017, 20, 69–76. [Google Scholar] [PubMed]
- Zhi-Yong, S.; Huan, Z.; Feng, L.; Nan-Ning, L.; Xiao-Yu, Z.; Bin, P.; Jun, L.; Zhong-Lai, Q.; Zhi-Ming, Z.; Hui-Lin, Y. A Retrospective Study of Percutaneous Balloon Kyphoplasty for the Treatment of Symptomatic Schmorl’s Nodes: 5-Year Results. Med. Sci. Monit. 2017, 23, 2879–2889. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.-J.; Jo, H.-J.; Lee, J.; Choi, S.-S.; Lee, C.-H. Percutaneous Vertebroplasty in a Patient with Chronic Back Pain Caused by Multiple Schmorl’s Nodes: A Case Report. Medicina 2023, 59, 1839. https://doi.org/10.3390/medicina59101839
Park H-J, Jo H-J, Lee J, Choi S-S, Lee C-H. Percutaneous Vertebroplasty in a Patient with Chronic Back Pain Caused by Multiple Schmorl’s Nodes: A Case Report. Medicina. 2023; 59(10):1839. https://doi.org/10.3390/medicina59101839
Chicago/Turabian StylePark, Hyung-Joon, Hyun-Ji Jo, Jaeeun Lee, Sang-Sik Choi, and Chung-Hun Lee. 2023. "Percutaneous Vertebroplasty in a Patient with Chronic Back Pain Caused by Multiple Schmorl’s Nodes: A Case Report" Medicina 59, no. 10: 1839. https://doi.org/10.3390/medicina59101839
APA StylePark, H.-J., Jo, H.-J., Lee, J., Choi, S.-S., & Lee, C.-H. (2023). Percutaneous Vertebroplasty in a Patient with Chronic Back Pain Caused by Multiple Schmorl’s Nodes: A Case Report. Medicina, 59(10), 1839. https://doi.org/10.3390/medicina59101839






