Arthroscopic Lower Trapezius Tendon Transfer for a Patient with Axillary Nerve Injury and Concomitant Rotator Cuff Tear: A Case Report and Technical Notes
Abstract
1. Introduction
2. Clinical Cases
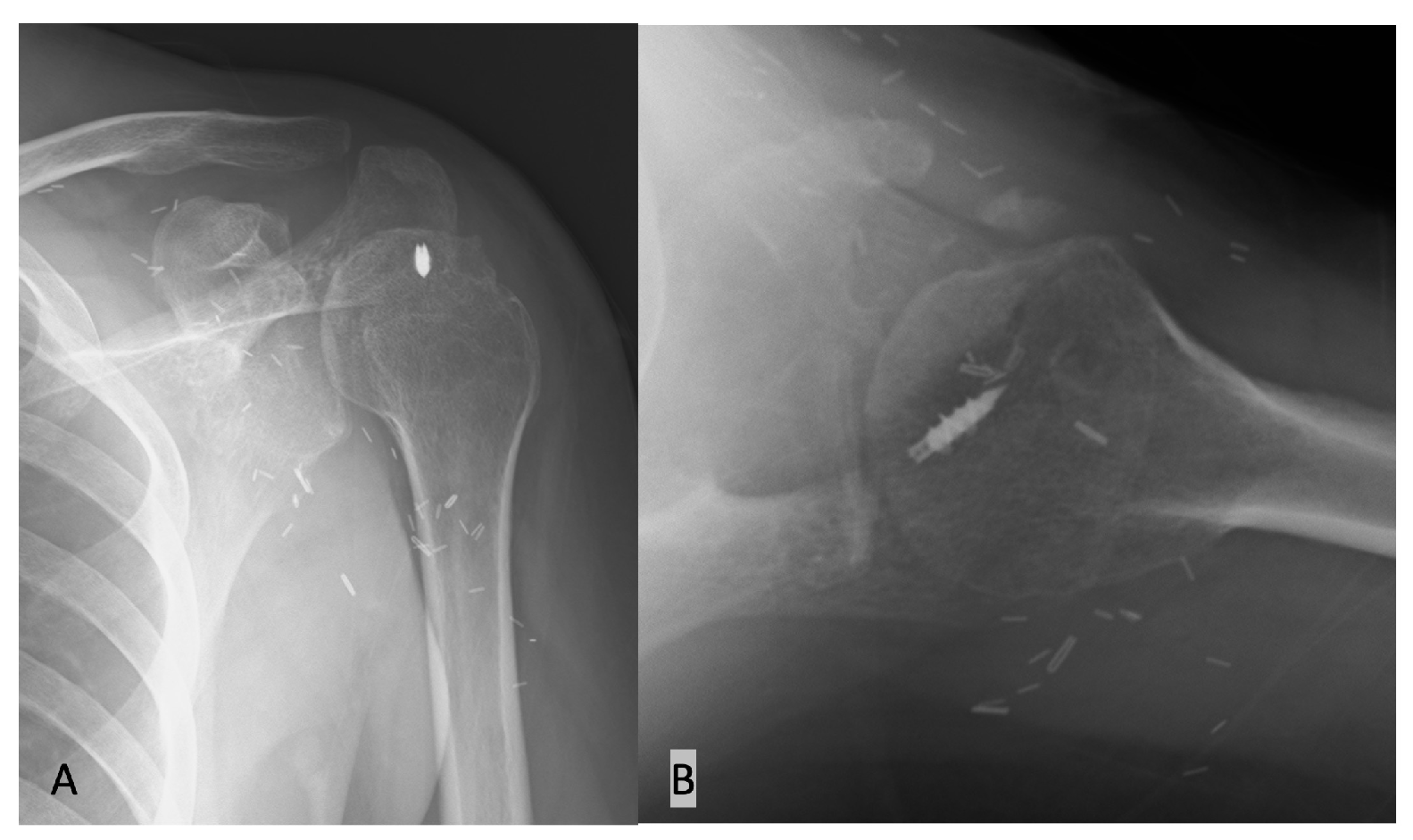
2.1. Case
2.2. Surgical Technique
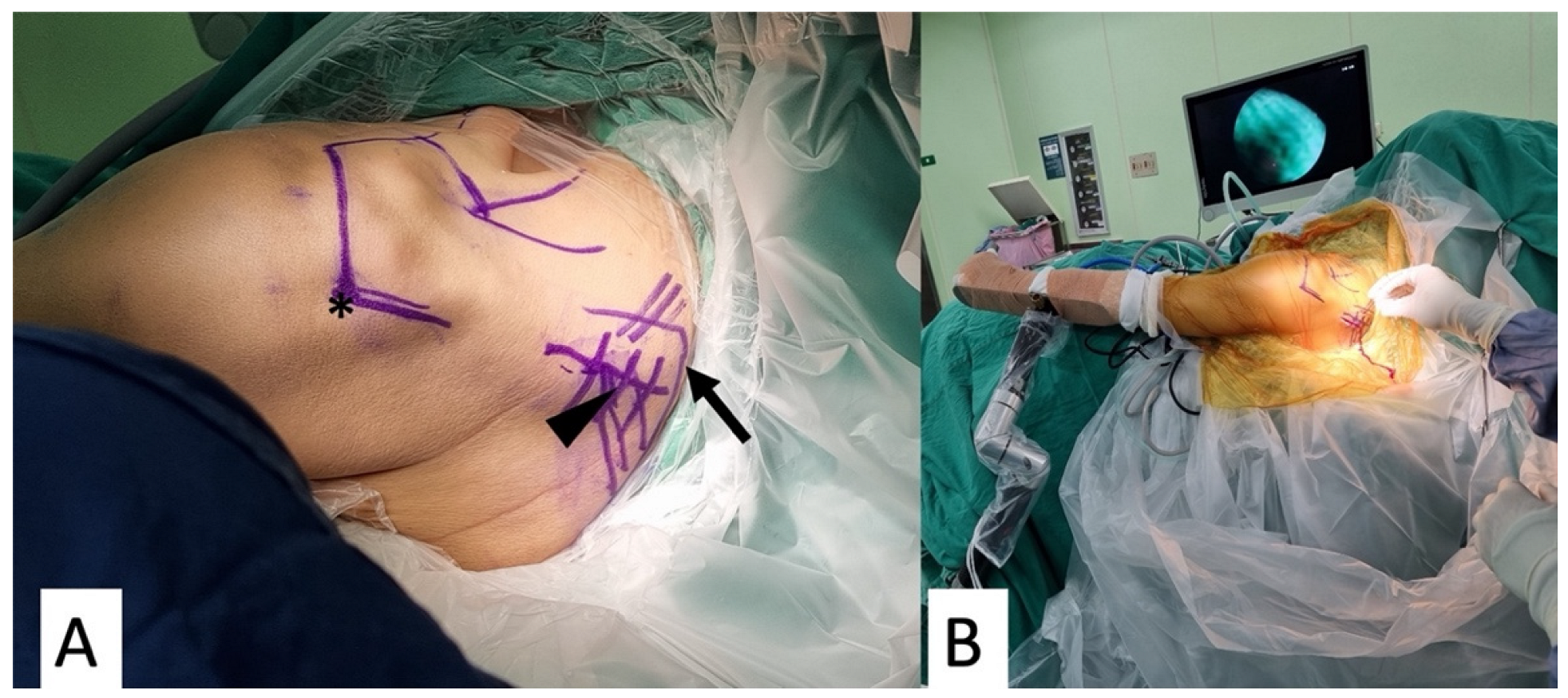
2.2.1. Patient Preparation
2.2.2. Graft Preparation
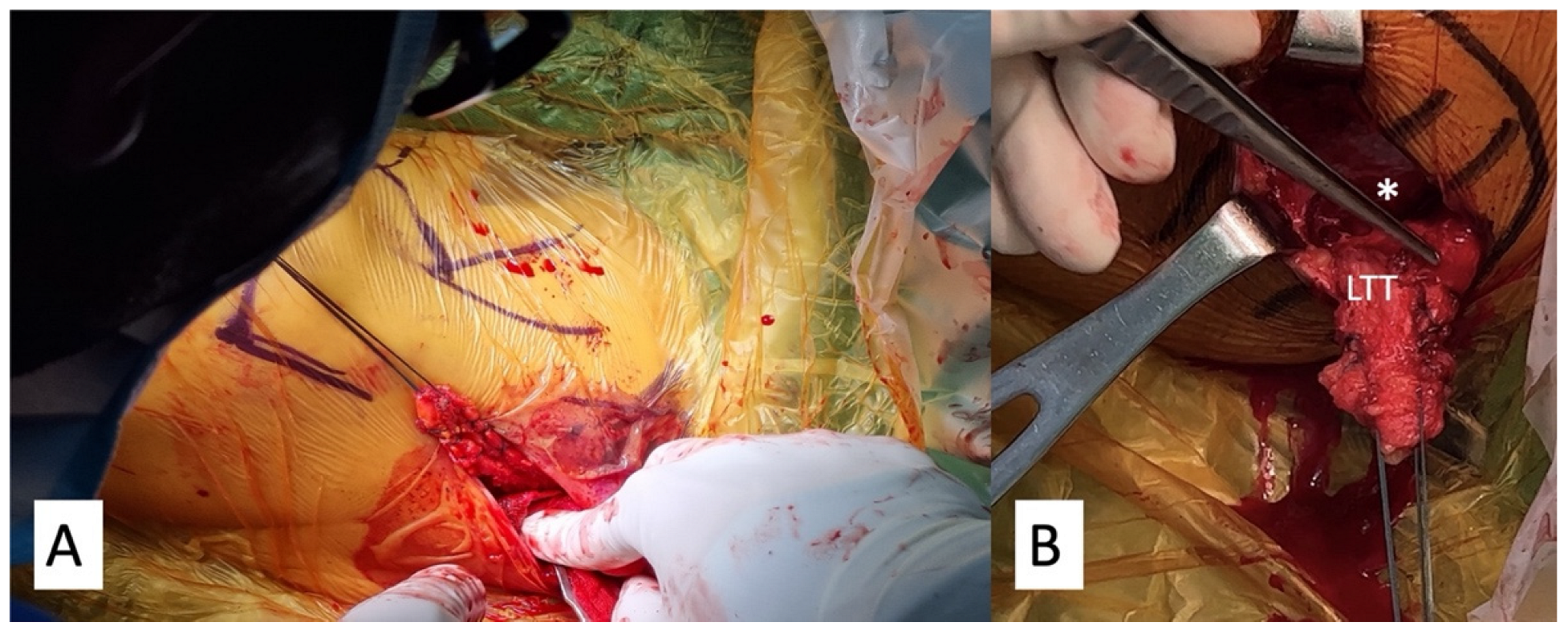
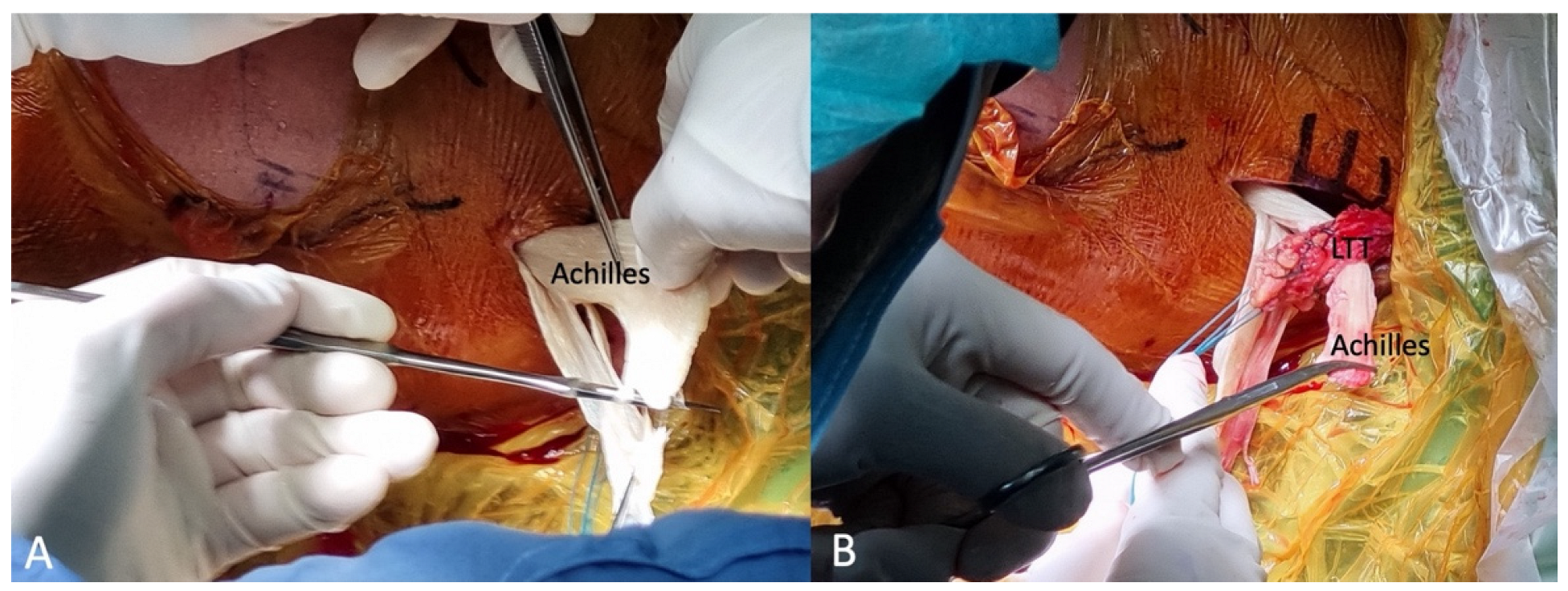
Lower Trapezius Tendon Harvest and Preparation
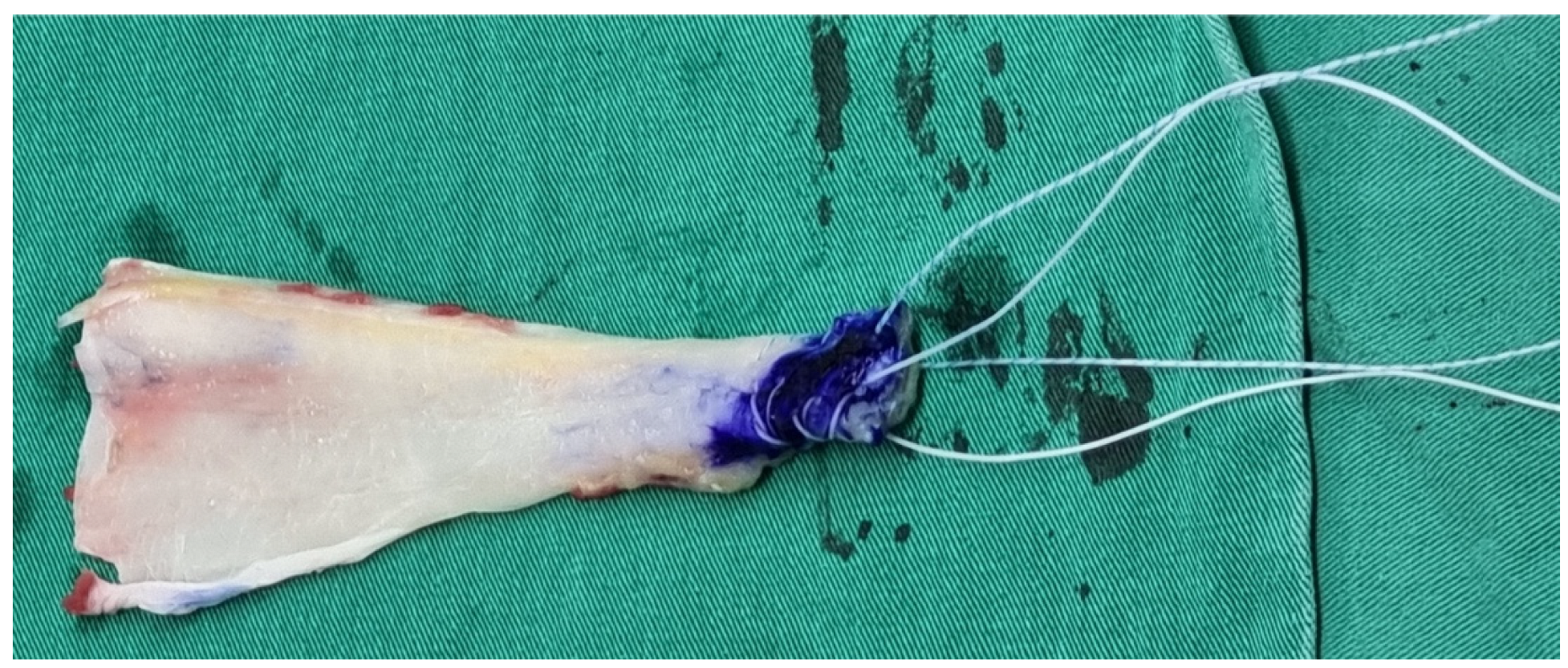
Achilles Allograft Tendon Preparation
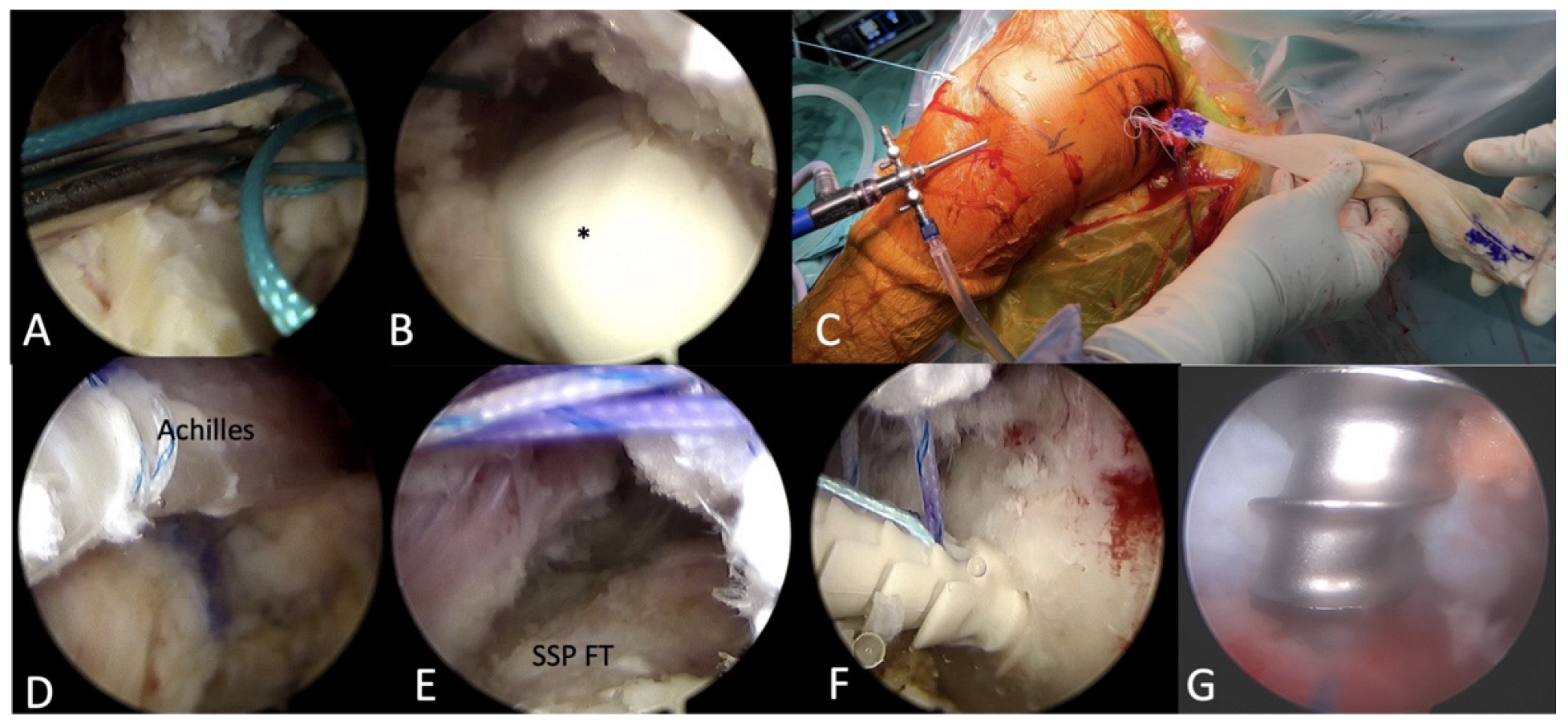
2.2.3. Arthroscopic Achilles Allograft Tendon Passage and Fixation
2.2.4. Merging the Achilles Allograft with LTT
2.3. Postoperative Protocol
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Noland, S.S.; Bishop, A.T.; Spinner, R.J.; Shin, A.Y. Adult Traumatic Brachial Plexus Injuries. J. Am. Acad. Orthop. Surg. 2019, 27, 705–716. [Google Scholar] [CrossRef]
- Hsueh, Y.H.; Tu, Y.K. Surgical reconstructions for adult brachial plexus injuries. Part I: Treatments for combined C5 and C6 injuries, with or without C7 injuries. Injury 2020, 51, 787–803. [Google Scholar] [CrossRef]
- Faglioni, W., Jr.; Siqueira, M.G.; Martins, R.S.; Heise, C.O.; Foroni, L. The epidemiology of adult traumatic brachial plexus lesions in a large metropolis. Acta Neurochir. (Wien) 2014, 156, 1025–1028. [Google Scholar] [CrossRef]
- Salama, M.O. Usama Role of Trapezius Transfer for Shoulder Reconstruction in Adult Traumatic Brachial Plexus Injuries. Int. Microsurg. J. 2018, 1, 3. [Google Scholar] [CrossRef]
- Gerber, C.; Blumenthal, S.; Curt, A.; Werner, C.M. Effect of selective experimental suprascapular nerve block on abduction and external rotation strength of the shoulder. J. Shoulder Elbow Surg. 2007, 16, 815–820. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Garg, R.; Earp, B.E.; Blazar, P.; Dyer, G.S.M. Shoulder Arthrodesis versus Upper Trapezius Transfer for Traumatic Brachial Plexus Injury: A Proportional Meta-Analysis. Adv. Orthop. 2021, 2021, 4445498. [Google Scholar] [CrossRef] [PubMed]
- Karki, D.; Muthukumar, V.; Dash, S.; Singh, A.K. Trapezius Transfer to Restore Shoulder Function in Traumatic Brachial Plexus Injury: Revisited and Modified. J. Hand Surg. Asian Pac. Vol. 2020, 25, 143–152. [Google Scholar] [CrossRef]
- Elhassan, B.T.; Wagner, E.R.; Spinner, R.J.; Bishop, A.T.; Shin, A.Y. Contralateral Trapezius Transfer to Restore Shoulder External Rotation Following Adult Brachial Plexus Injury. J. Hand Surg. Am. 2016, 41, e45–e51. [Google Scholar] [CrossRef]
- Elhassan, B.; Bishop, A.T.; Hartzler, R.U.; Shin, A.Y.; Spinner, R.J. Tendon transfer options about the shoulder in patients with brachial plexus injury. J. Bone Jt. Surg. Am. 2012, 94, 1391–1398. [Google Scholar] [CrossRef]
- Aibinder, W.R.; Elhassan, B.T. Lower trapezius transfer with Achilles tendon augmentation: Indication and clinical results. Obere Extrem. 2018, 13, 269–272. [Google Scholar] [CrossRef]
- Hartzler, R.U.; Barlow, J.D.; An, K.N.; Elhassan, B.T. Biomechanical effectiveness of different types of tendon transfers to the shoulder for external rotation. J. Shoulder Elbow Surg. 2012, 21, 1370–1376. [Google Scholar] [CrossRef] [PubMed]
- Elhassan, B.; Bishop, A.; Shin, A.; Spinner, R. Shoulder tendon transfer options for adult patients with brachial plexus injury. J. Hand Surg. Am. 2010, 35, 1211–1219. [Google Scholar] [CrossRef] [PubMed]
- Monreal, R.; Paredes, L.; Diaz, H.; Leon, P. Trapezius transfer to treat flail shoulder after brachial plexus palsy. J. Brachial Plex. Peripher. Nerve Inj. 2007, 2, 2. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Agrawal, N.K. Transfer of upper trapezius with clavicular segment for restoration of shoulder movements following injury to the brachial plexus. Plast. Aesthetic Res. 2015, 2, 346–349. [Google Scholar] [CrossRef]
- Bertelli, J.A. Upper and lower trapezius muscle transfer to restore shoulder abduction and external rotation in longstanding upper type palsies of the brachial plexus in adults. Microsurgery 2011, 31, 263–267. [Google Scholar] [CrossRef]
- Elhassan, B. Lower trapezius transfer for shoulder external rotation in patients with paralytic shoulder. J. Hand Surg. Am. 2014, 39, 556–562. [Google Scholar] [CrossRef]
- Ghoraishian, M.; Stone, M.A.; Elhassan, B.; Abboud, J.; Namdari, S. Techniques for lower trapezius tendon transfer for the management of irreparable posterosuperior rotator cuff tears. J. Orthop. 2020, 22, 331–335. [Google Scholar] [CrossRef]
- Ek, E.T.; Lording, T.; McBride, A.P. Arthroscopic-Assisted Lower Trapezius Tendon Transfer for Massive Irreparable Posterosuperior Rotator Cuff Tears Using an Achilles Tendon-Bone Allograft. Arthrosc. Tech. 2020, 9, e1759–e1766. [Google Scholar] [CrossRef]
- Elhassan, B.T.; Sanchez-Sotelo, J.; Wagner, E.R. Outcome of arthroscopically assisted lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tears. J. Shoulder Elbow Surg. 2020, 29, 2135–2142. [Google Scholar] [CrossRef]
- Crepaldi, B.E.; Neto, J.Q.L.; Rezende, M.R.; Junior, R.M.; Scarcella, D.S. Lower Trapezius Transfer for Patients with Brachial Plexus Injury. Hand 2019, 14, 179–186. [Google Scholar] [CrossRef]
- Elhassan, B.T.; Alentorn-Geli, E.; Assenmacher, A.T.; Wagner, E.R. Arthroscopic-Assisted Lower Trapezius Tendon Transfer for Massive Irreparable Posterior-Superior Rotator Cuff Tears: Surgical Technique. Arthrosc. Tech. 2016, 5, e981–e988. [Google Scholar] [CrossRef]
- Valenti, P.; Werthel, J.D. Lower trapezius transfer with semitendinosus tendon augmentation: Indication, technique, results. Obere Extrem. 2018, 13, 261–268. [Google Scholar] [CrossRef]
- Kany, J. Tendon transfers in rotator-cuff surgery. Orthop. Traumatol. Surg. Res. 2020, 106, S43–S51. [Google Scholar] [CrossRef]
- Herzberg, G.; Urien, J.P.; Dimnet, J. Potential excursion and relative tension of muscles in the shoulder girdle: Relevance to tendon transfers. J. Shoulder Elbow Surg. 1999, 8, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Elhassan, B.; Bishop, A.; Shin, A. Trapezius transfer to restore external rotation in a patient with a brachial plexus injury. A case report. J. Bone Jt. Surg. Am. 2009, 91, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Cartucho, A. Tendon transfers for massive rotator cuff tears. EFORT Open Rev. 2022, 7, 404–413. [Google Scholar] [CrossRef] [PubMed]
- Stoll, L.E.; Codding, J.L. Lower Trapezius Tendon Transfer for Massive Irreparable Rotator Cuff Tears. Orthop. Clin. N. Am. 2019, 50, 375–382. [Google Scholar] [CrossRef]
- Satbhai, N.G.; Doi, K.; Hattori, Y.; Sakamoto, S. Contralateral lower trapezius transfer for restoration of shoulder external rotation in traumatic brachial plexus palsy: A preliminary report and literature review. J. Hand Surg. Eur. Vol. 2014, 39, 861–867. [Google Scholar] [CrossRef]
- Elhassan, B.T.; Wagner, E.R.; Werthel, J.D. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J. Shoulder Elbow Surg. 2016, 25, 1346–1353. [Google Scholar] [CrossRef]
- Reddy, A.; Gulotta, L.V.; Chen, X.; Castagna, A.; Dines, D.M.; Warren, R.F.; Kontaxis, A. Biomechanics of lower trapezius and latissimus dorsi transfers in rotator cuff-deficient shoulders. J. Shoulder Elbow Surg. 2019, 28, 1257–1264. [Google Scholar] [CrossRef]
- Clouette, J.; Leroux, T.; Shanmugaraj, A.; Khan, M.; Gohal, C.; Veillette, C.; Henry, P.; Paul, R.A. The lower trapezius transfer: A systematic review of biomechanical data, techniques, and clinical outcomes. J. Shoulder Elbow Surg. 2020, 29, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Omid, R.; Heckmann, N.; Wang, L.; McGarry, M.H.; Vangsness, C.T., Jr.; Lee, T.Q. Biomechanical comparison between the trapezius transfer and latissimus transfer for irreparable posterosuperior rotator cuff tears. J. Shoulder Elbow Surg. 2015, 24, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- Desai, V.; Stambulic, T.; Daneshvar, P.; Bicknell, R.T. Lower trapezius tendon transfer for irreparable rotator cuff injuries: A scoping review. JSES Rev. Rep. Tech. 2023, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.H.; Yang, C.P.; Tang, H.C.; Weng, C.J.; Hsu, K.Y.; Chen, A.C.; Chan, Y.S. Arthroscopic-Assisted Lower Trapezius Tendon Transfer with Autologous Semitendinosus Tendon and Long Head of Biceps Superior Capsule Reconstruction for Massive Irreparable Posterosuperior Rotator Cuff Tears. Arthrosc. Tech. 2022, 11, e1251–e1259. [Google Scholar] [CrossRef]

| Indication | Contraindication |
|---|---|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loren, J.; Lu, C.-Y.; Yang, C.-P.; Hsu, K.-Y.; Cheng, Y.-H.; Sheu, H.; Chen, C.-Y.; Tang, H.-C.; Chuang, C.-A.; Chiu, C.-H. Arthroscopic Lower Trapezius Tendon Transfer for a Patient with Axillary Nerve Injury and Concomitant Rotator Cuff Tear: A Case Report and Technical Notes. Medicina 2023, 59, 1817. https://doi.org/10.3390/medicina59101817
Loren J, Lu C-Y, Yang C-P, Hsu K-Y, Cheng Y-H, Sheu H, Chen C-Y, Tang H-C, Chuang C-A, Chiu C-H. Arthroscopic Lower Trapezius Tendon Transfer for a Patient with Axillary Nerve Injury and Concomitant Rotator Cuff Tear: A Case Report and Technical Notes. Medicina. 2023; 59(10):1817. https://doi.org/10.3390/medicina59101817
Chicago/Turabian StyleLoren, Jeff, Chuieng-Yi (Johnny) Lu, Cheng-Pang Yang, Kuo-Yao Hsu, You-Hung Cheng, Huan Sheu, Chao-Yu Chen, Hao-Che Tang, Chieh-An Chuang, and Chih-Hao (Joe) Chiu. 2023. "Arthroscopic Lower Trapezius Tendon Transfer for a Patient with Axillary Nerve Injury and Concomitant Rotator Cuff Tear: A Case Report and Technical Notes" Medicina 59, no. 10: 1817. https://doi.org/10.3390/medicina59101817
APA StyleLoren, J., Lu, C.-Y., Yang, C.-P., Hsu, K.-Y., Cheng, Y.-H., Sheu, H., Chen, C.-Y., Tang, H.-C., Chuang, C.-A., & Chiu, C.-H. (2023). Arthroscopic Lower Trapezius Tendon Transfer for a Patient with Axillary Nerve Injury and Concomitant Rotator Cuff Tear: A Case Report and Technical Notes. Medicina, 59(10), 1817. https://doi.org/10.3390/medicina59101817








