IL-1 Beta—A Biomarker for Ischemic Stroke Prognosis and Atherosclerotic Lesions of the Internal Carotid Artery
Abstract
:1. Introduction
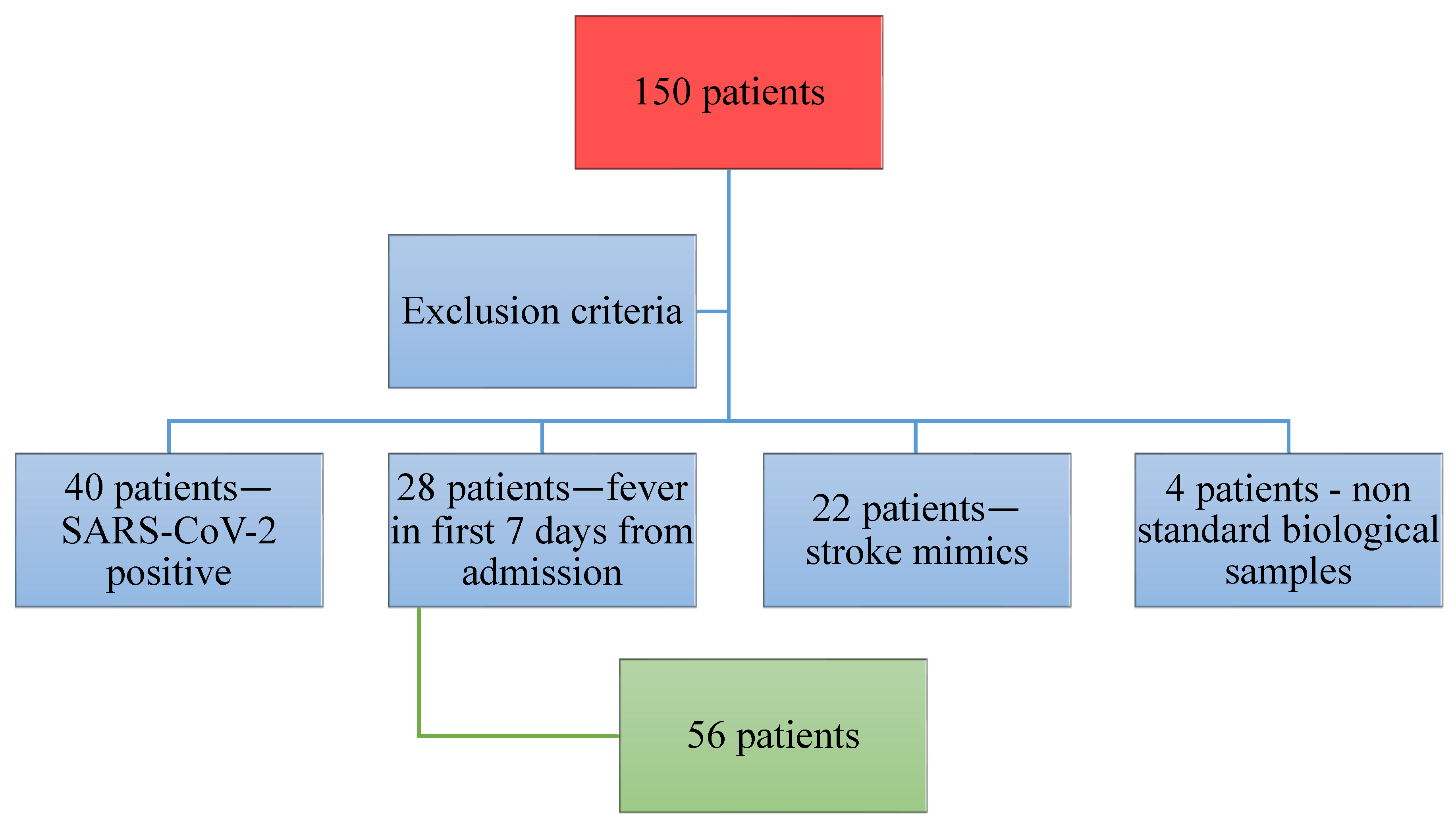
2. Materials and Methods
Study Design
- -
- Adult patients (from 33 to 94 years old) admitted to the Neurology Department, at Sibiu County Emergency Hospital, with diagnostic suspicion of ischemic stroke.
- -
- Neurological symptoms and signs strongly suggesting the onset of an ischemic stroke (within the last 24 h).
- -
- Cerebral imaging ruling out cerebral tumors or hemorrhagic stroke.
- -
- Any medical pathology that can trigger modification of inflammatory markers, such as infections, autoimmune diseases, neoplasia, and hematological disorders (lymphoma amd multiple myeloma).
- -
- Patients undergoing (in the last 30 days) corticosteroid or immunosuppressive therapy.
- -
- Patients diagnosed over the last 180 days with acute myocardial infarction, myocarditis, or acute ischemic stroke.
- -
- Patients who suffered brain traumatic injuries documented at the time of admission.
- a.
- Collection of biological samples and bio-marker measurement
- 0.
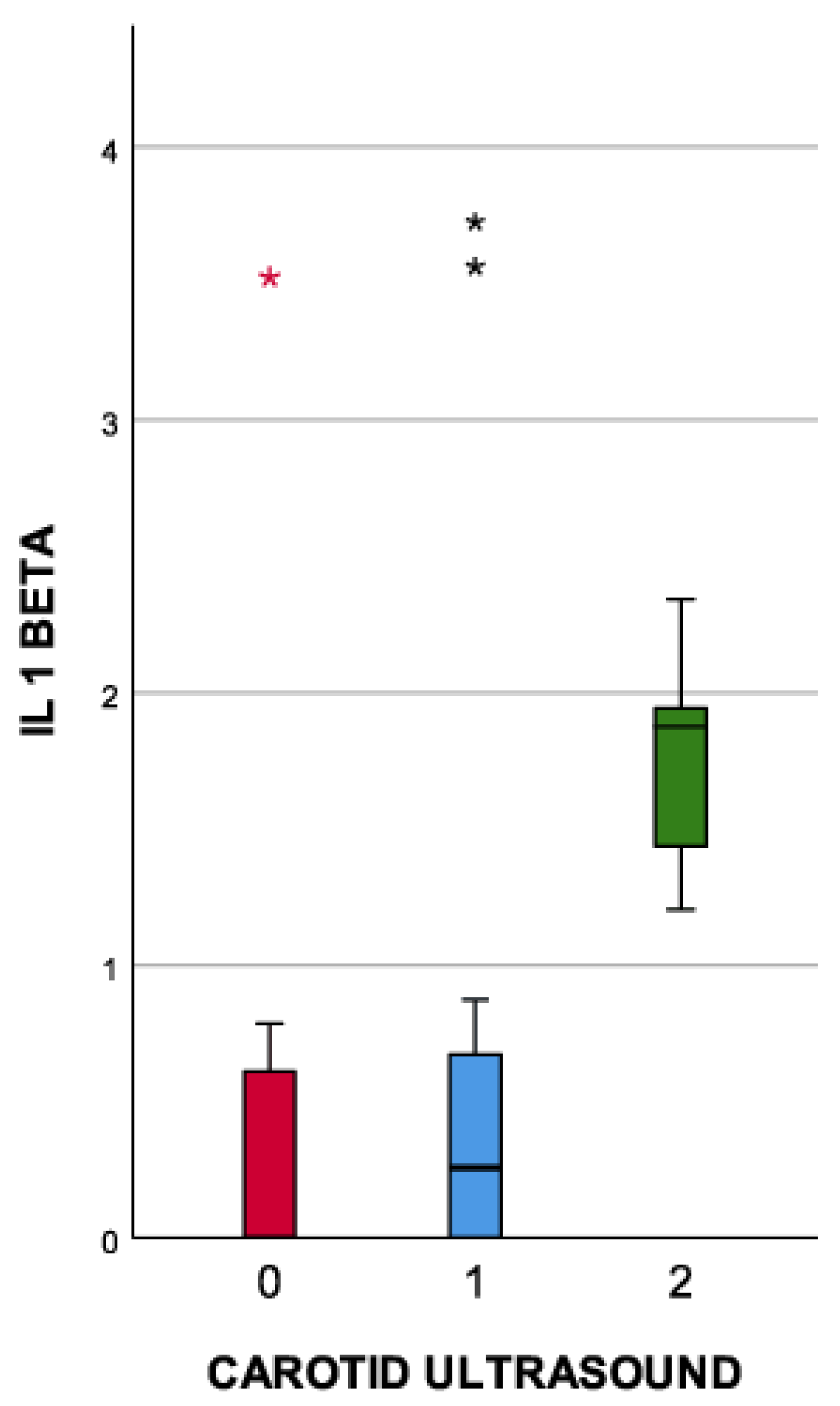
- Mild atherosclerotic lesions of the carotid artery.
- 1.
- Moderate atherosclerotic lesions of the carotid artery; internal carotid artery (ICA) stenosis 50–69%.
- 2.
- Severe atherosclerotic lesions of the carotid artery; internal carotid artery (ICA) stenosis greater than 70%.
- b.
- Statistical analysis
3. Results
- Mild atherosclerotic lesions of the carotid artery.
- Moderate atherosclerotic lesions of the carotid artery; internal carotid artery (ICA) stenosis 50–69%.
- Severe atherosclerotic lesions of the carotid artery; internal carotid artery (ICA) stenosis greater than 70%.
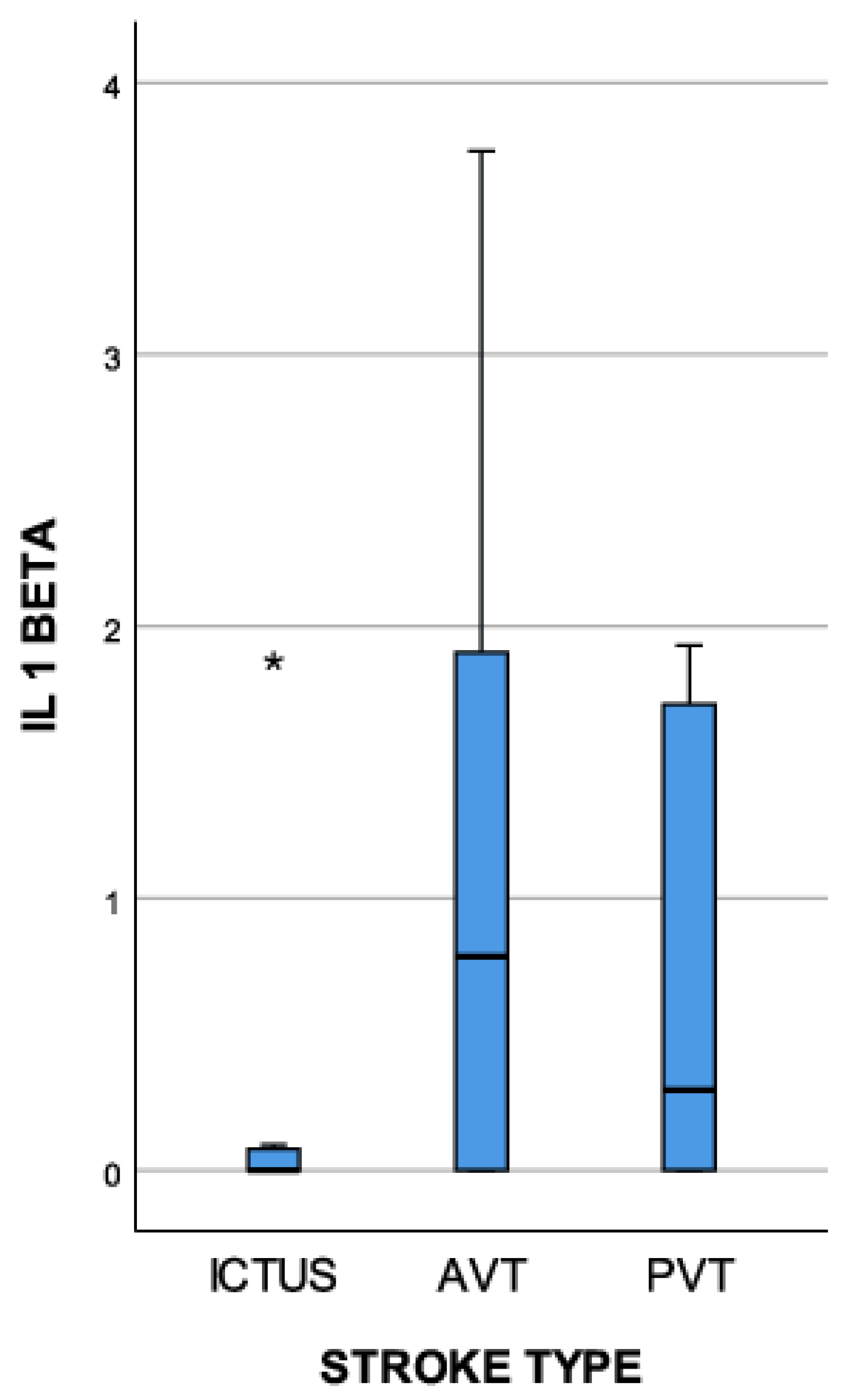
- Lacunar stroke—patients with cerebral ischemic lesions smaller than 10 mm.
- Anterior Vascular Territory (AVT)—patients with cerebral ischemia in the anterior vascular territory.
- Posterior Vascular Territory (PVT)—patients with cerebral ischemia in the posterior vascular territory.
4. Discussion
5. Limitations of the Study
- The number of patients included in the study was relatively small. IL-1 beta should be included in studies with bigger cohorts before being considered a therapeutic target. However, the cohort was sufficient for it to be considered as a prognostic marker for ischemic stroke and atherosclerotic lesions of the carotid arteries.
- Measurements in long-term dynamics should be performed to determine what happens with inflammation, neurological status, and atherosclerotic lesions of the carotid arteries over time.
- Whether or not obesity and chronic medication can influence the IL-1 beta plasma concentration should be examined. Research on this subject should be developed and continued.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jayaraj, R.L.; Azimullah, S.; Beiram, R.; Jalal, F.Y.; Rosenberg, G.A. Neuroinflammation: Friend and foe for ischemic stroke. J. Neuroinflamm. 2019, 16, 142. [Google Scholar] [CrossRef]
- Kim, J.; Kawabori, M.; Yenari, M. Innate inflammatory responses in stroke: Mechanisms and potential therapeutic targets. Curr. Med. Chem. 2014, 21, 2076–2097. [Google Scholar] [CrossRef]
- Denes, A.; Pinteaux, E.; Rothwell, N.J.; Allan, S.M. Interleukin-1 and stroke: Biomarker, harbinger of damage, and therapeutic target. Cerebrovasc. Dis. 2011, 32, 517–527. [Google Scholar] [CrossRef]
- Banwell, V.; Sena, E.S.; Macleod, M.R. Systematic review and stratified meta-analysis of the efficacy of interleukin-1 receptor antagonist in animal models of stroke. J. Stroke Cerebrovasc. Dis. 2009, 18, 269–276. [Google Scholar] [CrossRef]
- Pinteaux, E.; Trotter, P.; Simi, A. Cell-specific and concentration-dependent actions of interleukin-1 in acute brain inflammation. Cytokine 2009, 45, 1–7. [Google Scholar] [CrossRef]
- Libby, P. Inflammation in atherosclerosis—No longer a theory. Clin. Chem. 2021, 67, 131–142. [Google Scholar] [CrossRef]
- Nguyen, M.; Fernando, S.; Schwarz, N.; Tan, J.; Bursill, C.; Psaltis, P. Inflammation as a therapeutic target in atherosclerosis. J. Clin. Med. 2019, 8, 1109. [Google Scholar] [CrossRef]
- Rafieian-Kopaei, M.; Setorki, M.; Doudi, M.; Baradaran, A.; Nasri, H. Atherosclerosis: Process, indicators, risk factors and new hopes. Int. J. Prev. Med. 2014, 5, 927. [Google Scholar]
- Gregersen, I.; Halvorsen, B. Inflammatory Mechanisms in Atherosclerosis. Atherosclerosis-Yesterday, Today and Tomorrow; InTech: Houston, TX, USA, 2018. [Google Scholar]
- Chistiakov, D.A.; Kashirskikh, D.A.; Khotina, V.A.; Grechko, A.V.; Orekhov, A.N. Immune-inflammatory responses in atherosclerosis: The role of myeloid cells. J. Clin. Med. 2019, 8, 1798. [Google Scholar] [CrossRef]
- Mendiola, A.S.; Cardona, A.E. The IL-1β phenomena in neuroinflammatory diseases. J. Neural Transm. 2018, 125, 781–795. [Google Scholar] [CrossRef]
- Simats, A.; Liesz, A. Systemic inflammation after stroke: Implications for post-stroke comorbidities. EMBO Mol. Med. 2022, 14, e16269. [Google Scholar] [CrossRef]
- Krishnan, S.; O’boyle, C.; Smith, C.J.; Hulme, S.; Allan, S.M.; Grainger, J.R.; Lawrence, C.B. A hyperacute immune map of ischaemic stroke patients reveals alterations to circulating innate and adaptive cells. Clin. Exp. Immunol. 2021, 203, 458–471. [Google Scholar] [CrossRef]
- Jurcau, A.; Simion, A. Neuroinflammation in cerebral ischemia and ischemia/reperfusion injuries: From pathophysiology to therapeutic strategies. Int. J. Mol. Sci. 2021, 23, 14. [Google Scholar] [CrossRef]
- Boutin, H.; LeFeuvre, R.A.; Horai, R.; Asano, M.; Iwakura, Y.; Rothwell, N.J. Role of IL-1α and IL-1β in ischemic brain damage. J. Neurosci. 2001, 21, 5528–5534. [Google Scholar] [CrossRef]
- Smith, C.J.; Emsley, H.C.; Udeh, C.T.; Vail, A.; Hoadley, M.E.; Rothwell, N.J.; Tyrrell, P.J.; Hopkins, S.J. Interleukin-1 receptor antagonist reverses stroke-associated peripheral immune suppression. Cytokine 2012, 58, 384–389. [Google Scholar] [CrossRef]
- Pawluk, H.; Woźniak, A.; Grześk, G.; Kołodziejska, R.; Kozakiewicz, M.; Kopkowska, E.; Grzechowiak, E.; Kozera, G. The role of selected proinflammatory cytokines in pathogenesis of ischemic stroke. Clin. Interv. Aging 2020, 15, 469–484. [Google Scholar] [CrossRef]
- Smith, C.J.; Hulme, S.; Vail, A.; Heal, C.; Parry-Jones, A.R.; Scarth, S.; Hopkins, K.; Hoadley, M.; Allan, S.M.; Rothwell, N.J.; et al. SCIL-STROKE (subcutaneous interleukin-1 receptor antagonist in ischemic stroke) a randomized controlled phase 2 trial. Stroke 2018, 49, 1210–1216. [Google Scholar] [CrossRef]
- Emsley, H.C.; Smith, C.J.; Gavin, C.M.; Georgiou, R.F.; Vail, A.; Barberan, E.M.; Illingworth, K.; Scarth, S.; Wickramasinghe, V.; Hoadley, M.E.; et al. Clinical outcome following acute ischaemic stroke relates to both activation and autoregulatory inhibition of cytokine production. BMC Neurol. 2007, 7, 5. [Google Scholar] [CrossRef]
- Stone, M.J.; Hayward, J.A.; Huang, C.; Huma, Z.E.; Sanchez, J. Mechanisms of regulation of the chemokine-receptor network. Int. J. Mol. Sci. 2017, 18, 342. [Google Scholar] [CrossRef]
- Chiba, T.; Itoh, T.; Tabuchi, M.; Nakazawa, T.; Satou, T. Interleukin-1β accelerates the onset of stroke in stroke-prone spontaneously hypertensive rats. Mediat. Inflamm. 2012, 2012, 701976. [Google Scholar] [CrossRef]
- Faura, J.; Bustamante, A.; Miró-Mur, F.; Montaner, J. Stroke-induced immunosuppression: Implications for the prevention and prediction of post-stroke infections. J. Neuroinflammat. 2021, 18, 1–4. [Google Scholar]
- Planas, A.M.; Gómez-Choco, M.; Urra, X.; Gorina, R.; Caballero, M.; Chamorro, Á. Brain-derived antigens in lymphoid tissue of patients with acute stroke. J. Immunol. 2012, 188, 2156–2163. [Google Scholar] [CrossRef]
- Mai, W.; Liao, Y. Targeting IL-1β in the Treatment of Atherosclerosis. Front. Immunol. 2020, 11, 589654. [Google Scholar] [CrossRef] [PubMed]
- Gomez, D.; Baylis, R.A.; Durgin, B.G.; Newman, A.A.C.; Alencar, G.F.; Mahan, S.; Hilaire, C.S.; Müller, W.; Waisman, A.; Francis, S.E.; et al. Interleukin-1β has atheroprotective effects in advanced atherosclerotic lesions of mice. Nat. Med. 2018, 24, 1418–1429. [Google Scholar] [CrossRef] [PubMed]
- Galea, J.; Armstrong, J.; Gadsdon, P.; Holden, H.; Francis, S.E.; Holt, C.M. Interleukin-1β in coronary arteries of patients with ischemic heart disease. Arter. Thromb. Vasc. Biol. 1996, 16, 1000–1006. [Google Scholar] [CrossRef]
- Grebe, A.; Hoss, F.; Latz, E. NLRP3 inflammasome and the IL-1 pathway in atherosclerosis. Circ. Res. 2018, 122, 1722–1740. [Google Scholar] [CrossRef]
- Roth, S.; Cao, J.; Singh, V.; Tiedt, S.; Hundeshagen, G.; Li, T.; Boehme, J.D.; Chauhan, D.; Zhu, J.; Ricci, A.; et al. Post-injury immunosuppression and secondary infections are caused by an AIM2 inflammasome-driven signaling cascade. Immunity 2021, 54, 648–659. [Google Scholar] [CrossRef]
- Georgakis, M.K.; Bernhagen, J.; Heitman, L.H.; Weber, C.; Dichgans, M. Targeting the CCL2–CCR2 axis for atheroprotection. Eur. Hear. J. 2022, 43, 1799–1808. [Google Scholar] [CrossRef]
- Jiang, C.; Kong, W.; Wang, Y.; Ziai, W.; Yang, Q.; Zuo, F.; Li, F.; Wang, Y.; Xu, H.; Li, Q.; et al. Changes in the cellular immune system and circulating inflammatory markers of stroke patients. Oncotarget 2017, 8, 3553–3567. [Google Scholar] [CrossRef]
- Shimokawa, H.; Ito, A.; Fukumoto, Y.; Kadokami, T.; Nakaike, R.; Sakata, M.; Takayanagi, T.; Egashira, K.; Takeshita, A. Chronic treatment with interleukin-1 beta induces coronary intimal lesions and vasospastic responses in pigs in vivo. The role of platelet-derived growth factor. J. Clin. Investig. 1996, 97, 769–776. [Google Scholar] [CrossRef]
- Chamberlain, J.; Evans, D.; King, A.; Dewberry, R.; Dower, S.; Crossman, D.; Francis, S. Interleukin-1β and signaling of interleukin-1 in vascular wall and circulating cells modulates the extent of neointima formation in mice. Am. J. Pathol. 2006, 168, 1396–1403. [Google Scholar] [CrossRef]
- Elhage, R.; Maret, A.; Pieraggi, M.-T.; Thiers, J.C.; Arnal, J.F.; Bayard, F. Differential effects of interleukin-1 receptor antagonist and tumor necrosis factor binding protein on fatty-streak formation in apolipoprotein E–deficient mice. Circulation 1998, 97, 242–244. [Google Scholar] [CrossRef]
- Devlin, C.M.; Kuriakose, G.; Hirsch, E.; Tabas, I. Genetic alterations of IL-1 receptor antagonist in mice affect plasma cholesterol level and foam cell lesion size. Proc. Natl. Acad. Sci. USA 2002, 99, 6280–6285. [Google Scholar] [CrossRef]
- Kirii, H.; Niwa, T.; Yamada, Y.; Wada, H.; Saito, K.; Iwakura, Y.; Asano, M.; Moriwaki, H.; Seishima, M. Lack of interleukin-1β decreases the severity of atherosclerosis in ApoE-deficient mice. Arter. Thromb. Vasc. Biol. 2003, 23, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Duewell, P.; Kono, H.; Rayner, K.J.; Sirois, C.M.; Vladimer, G.; Bauernfeind, F.G.; Abela, G.S.; Franchi, L.; Nuñez, G.; Schnurr, M.; et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature 2010, 464, 1357–1361. [Google Scholar] [CrossRef] [PubMed]
- Manica-Cattani, M.; Bittencourt, L.; Rocha, M.; Algarve, T.; Bodanese, L.; Rech, R.; Machado, M.; Santos, G.; Gottlieb, M.; Schwanke, C.; et al. Association between interleukin-1 beta polymorphism (+3953) and obesity. Mol. Cell. Endocrinol. 2010, 314, 84–89. [Google Scholar] [CrossRef]
- Weir, C.B.; Jan, A. BMI Classification Percentile And Cut Off Points. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef] [PubMed]
- Tardif, J.C.; Kouz, S.; Waters, D.D.; Bertrand, O.F.; Diaz, R.; Maggioni, A.P.; Pinto, F.J.; Ibrahim, R.; Gamra, H.; Kiwan, G.S.; et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N. Engl. J. Med. 2019, 381, 2497–2505. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Everett, B.M.; Pradhan, A.; MacFadyen, J.G.; Solomon, D.H.; Zaharris, E.; Mam, V.; Hasan, A.; Rosenberg, Y.; Iturriaga, E.; et al. Low-dose methotrexate for the prevention of atherosclerotic events. N. Engl. J. Med. 2019, 380, 752–762. [Google Scholar] [CrossRef]
- Ridker, P.M. Closing the loop on inflammation and atherothrombosis: Why perform the CIRT and CANTOS trials? Trans. Am. Clin. Climatol. Assoc. 2013, 124, 174. [Google Scholar]
- Nidorf, S.M.; Eikelboom, J.W.; Budgeon, C.A.; Thompson, P.L. Low-dose colchicine for secondary prevention of cardiovascular disease. J. Am. Coll. Cardiol. 2013, 61, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Nidorf, S.M.; Fiolet, A.T.; Mosterd, A.; Eikelboom, J.W.; Schut, A.; Opstal, T.S.; The, S.H.; Xu, X.F.; Ireland, M.A.; Lenderink, T.; et al. Colchicine in patients with chronic coronary disease. N. Engl. J. Med. 2020, 383, 1838–1847. [Google Scholar] [CrossRef] [PubMed]
- Kelly, P.; Weimar, C.; Lemmens, R.; Murphy, S.; Purroy, F.; Arsovska, A.; Bornstein, N.M.; Czlonkowska, A.; Fischer, U.; Fonseca, A.C.; et al. Colchicine for prevention of vascular inflammation in Non-CardioEmbolic stroke (CONVINCE)–study protocol for a randomised controlled trial. Eur. Stroke J. 2021, 6, 222–228. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung, and Blood Institute (NHLBI). Rilonacept to Improve Artery Function in Patients with Atherosclerosis [ClinicalTrials.gov identifier NCT00417417]. US National Institutes of Health, Clinical Trials.gov. Available online: www.clinicaltrials.gov (accessed on 15 September 2023).
| AGE | 74 (70–80) |
| GENRE | |
| F | 28 (50%) |
| M | 28 (50%) |
| NIHSS (ADMISSION) | 7 (4–11) |
| NIHSS (DISCHARGE) | 5 (2–10) |
| IL-1 BETA (24 h) | 0.51 (0–1.56) |
| IL-1 BETA (DAY 7) | 0 (0–1.59) |
| CHOLESTEROL | 196 (55.79) |
| CAROTID ULTRASOUND | |
| 0 | 14 (25%) |
| 1 | 20 (35.71%) |
| 2 | 22 (39.29%) |
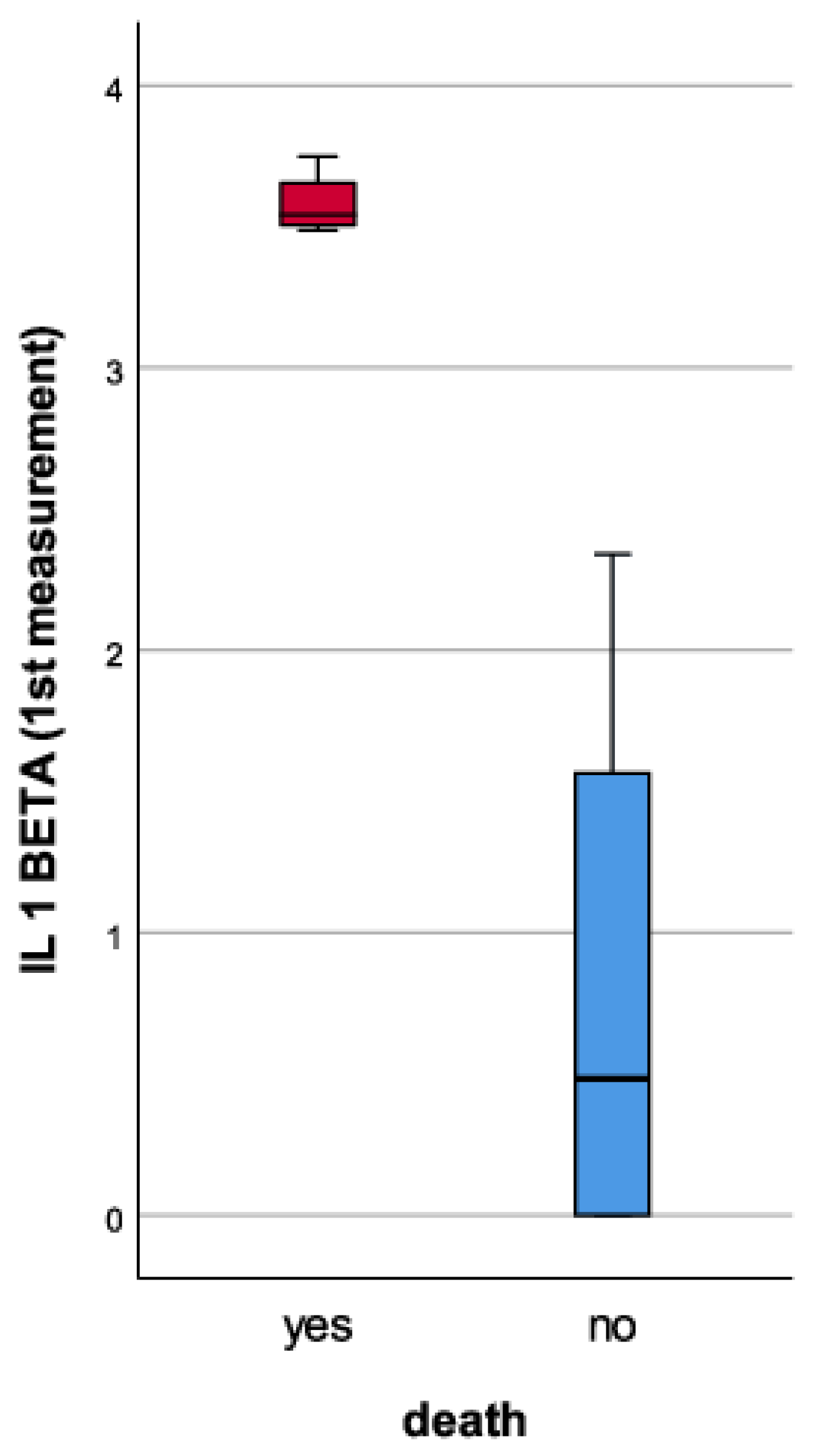
| Cut-Off | Se | Sp | AUC | 95% CI | SE | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| IL-1 BETA (2nd measurement) | 0.964 | 0.941 | 1 | 0.952 | 0.861 | 1 | 0.046 | <0.001 |
| IL-1 BETA (1st measurement) | 1.0375 | 0.941 | 1 | 0.964 | 0.894 | 1 | 0.035 | <0.001 |
| Trial Name | Study Design | Patient Number | Molecule | Results |
|---|---|---|---|---|
| The Canakinumab Anti-inflammatory Thrombosis Outcome Study CANTOS | Phase 3, multicenter, randomized, double-blind, placebo-controlled | 10,061 | Canakinumab—subcutaneous injection (50 mg, 150 mg, 300 mg) every 3 months vs. placebo | Benefits observed in the 150 mg treatment group |
| Colchicine Cardiovascular Outcomes Trial COLCOT | Phase 3 randomized, placebo-controlled | 4745 | Colchicine 0.5 mg/day vs. placebo | Benefits with serious adverse effects due to colchicine |
| Cardiovascular Inflammation Reduction Trial CIRT | Phase 3 multicenter, randomized, double-blind, placebo-controlled | 4786 | Oral methotrexate—1520 mg/weekly vs. placebo | No benefits |
| Low-Dose Colchicine Trial for Secondary Prevention of Cardiovascular Disease LODOCO | Phase 3 multicenter, randomized, double-blind, placebo-controlled | 532 | Colchicine 0.5 mg/day vs. placebo | Benefits, but major adverse effects |
| Low-Dose Colchicine Trial for Secondary Prevention of Cardiovascular Disease LODOCO2 | Phase 3 multicenter, randomized, double-blind, placebo-controlled | 5500 | Colchicine 0.5 mg/day vs. placebo | Benefits observed during long-term follow-up |
| Colchicine for prevention of vascular inflammation in non-cardioembolic stroke CONVINCE | Phase 3 multicenter, open-label, placebo-controlled | 2623 | Colchicine 0.5 mg/day vs. placebo | Ongoing |
| Subcutaneous Interleukin-1 Receptor Antagonist in Ischemic Stroke SCIL-STROKE | Phase 2, single-center, double-blind, randomized, placebo-controlled | 80 | Anakinra | Benefits—reduced inflammation |
| Rilonacept to improve artery function in patients with atherosclerosis | Phase 2, single-center, double-blind, randomized, placebo-controlled | 10 | Rilonacept | Benefits—reduced inflammation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Catană, M.-G.; Popențiu, I.-A.; Văleanu, M.; Roman-Filip, C.; Mihăilă, R.-G. IL-1 Beta—A Biomarker for Ischemic Stroke Prognosis and Atherosclerotic Lesions of the Internal Carotid Artery. Medicina 2023, 59, 1790. https://doi.org/10.3390/medicina59101790
Catană M-G, Popențiu I-A, Văleanu M, Roman-Filip C, Mihăilă R-G. IL-1 Beta—A Biomarker for Ischemic Stroke Prognosis and Atherosclerotic Lesions of the Internal Carotid Artery. Medicina. 2023; 59(10):1790. https://doi.org/10.3390/medicina59101790
Chicago/Turabian StyleCatană, Maria-Gabriela, Ioan-Adrian Popențiu, Mădălina Văleanu, Corina Roman-Filip, and Romeo-Gabriel Mihăilă. 2023. "IL-1 Beta—A Biomarker for Ischemic Stroke Prognosis and Atherosclerotic Lesions of the Internal Carotid Artery" Medicina 59, no. 10: 1790. https://doi.org/10.3390/medicina59101790
APA StyleCatană, M.-G., Popențiu, I.-A., Văleanu, M., Roman-Filip, C., & Mihăilă, R.-G. (2023). IL-1 Beta—A Biomarker for Ischemic Stroke Prognosis and Atherosclerotic Lesions of the Internal Carotid Artery. Medicina, 59(10), 1790. https://doi.org/10.3390/medicina59101790






