Modular Digital and 3D-Printed Dental Models with Applicability in Dental Education
Abstract
1. Introduction
2. Materials and Methods
2.1. Obtaining the Modular Digital and 3D-Printed Dental Models
2.1.1. Digital Data Acquisition
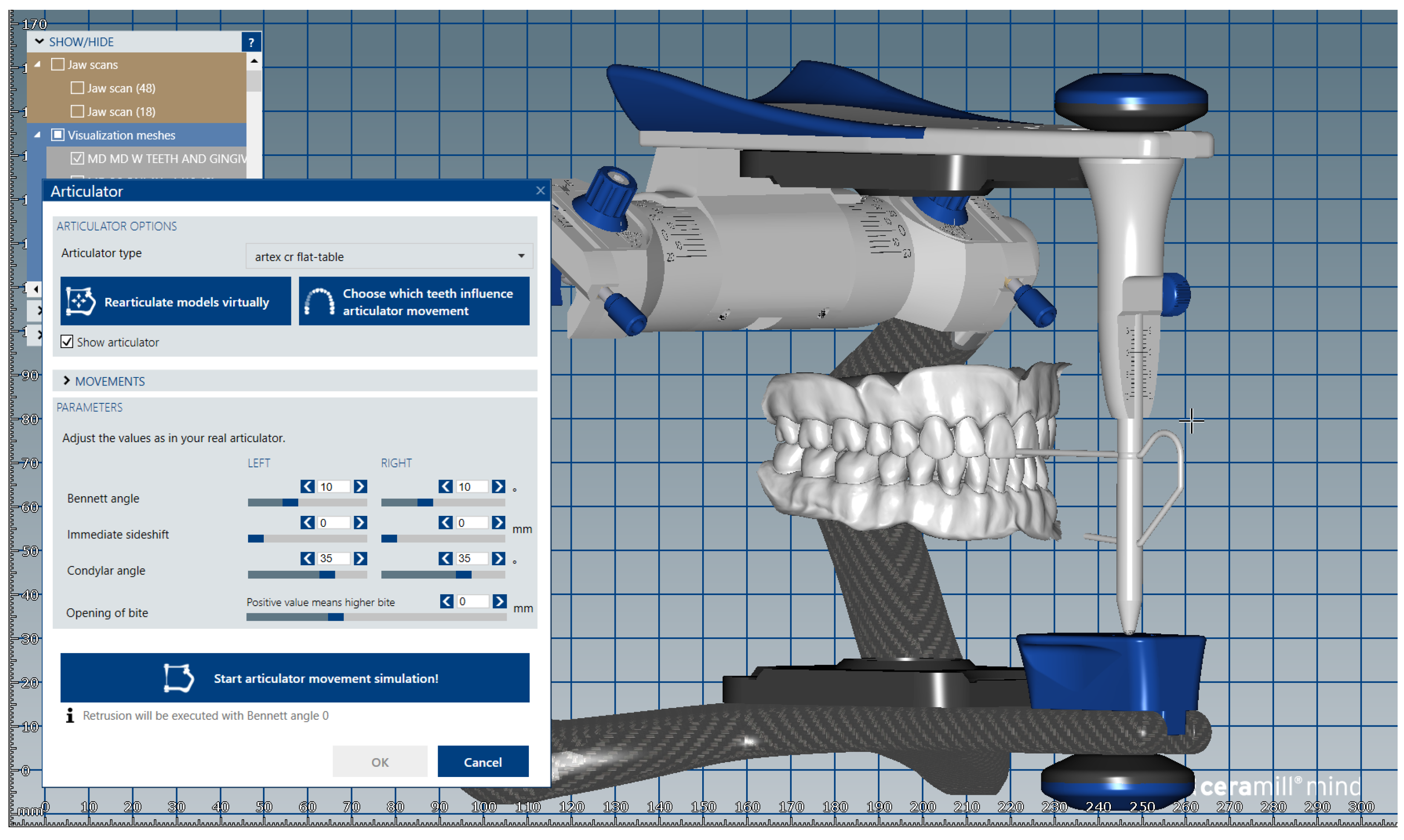
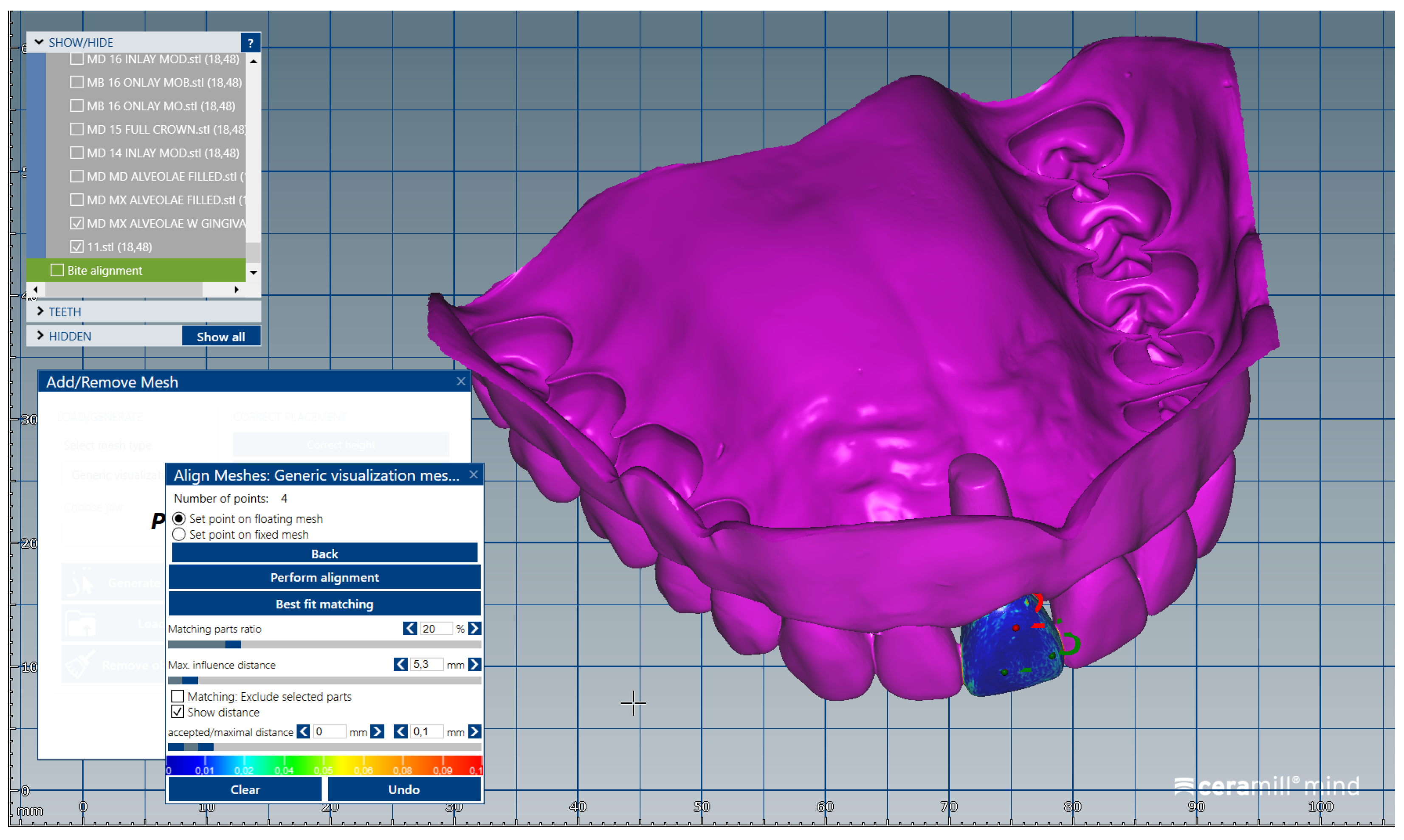
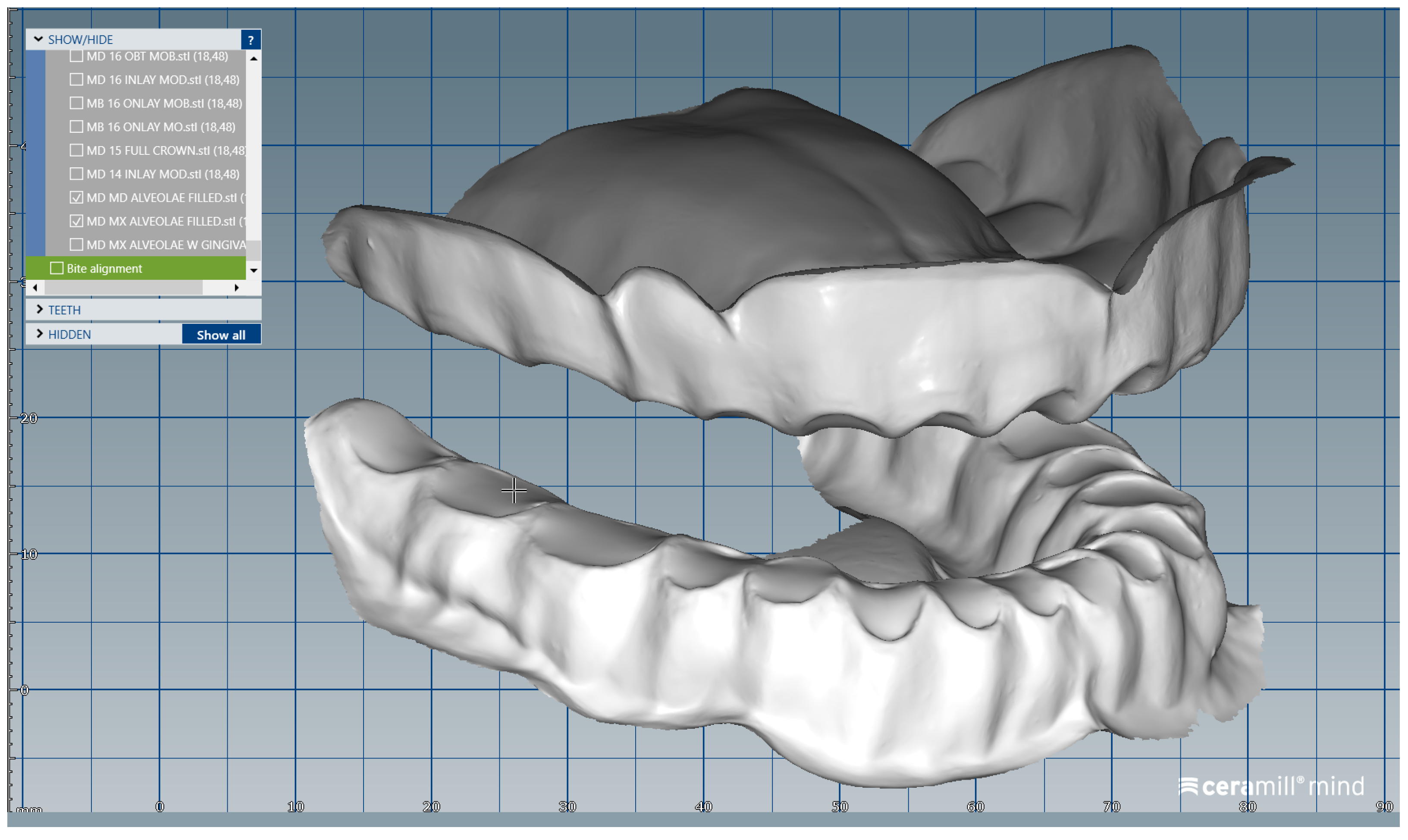
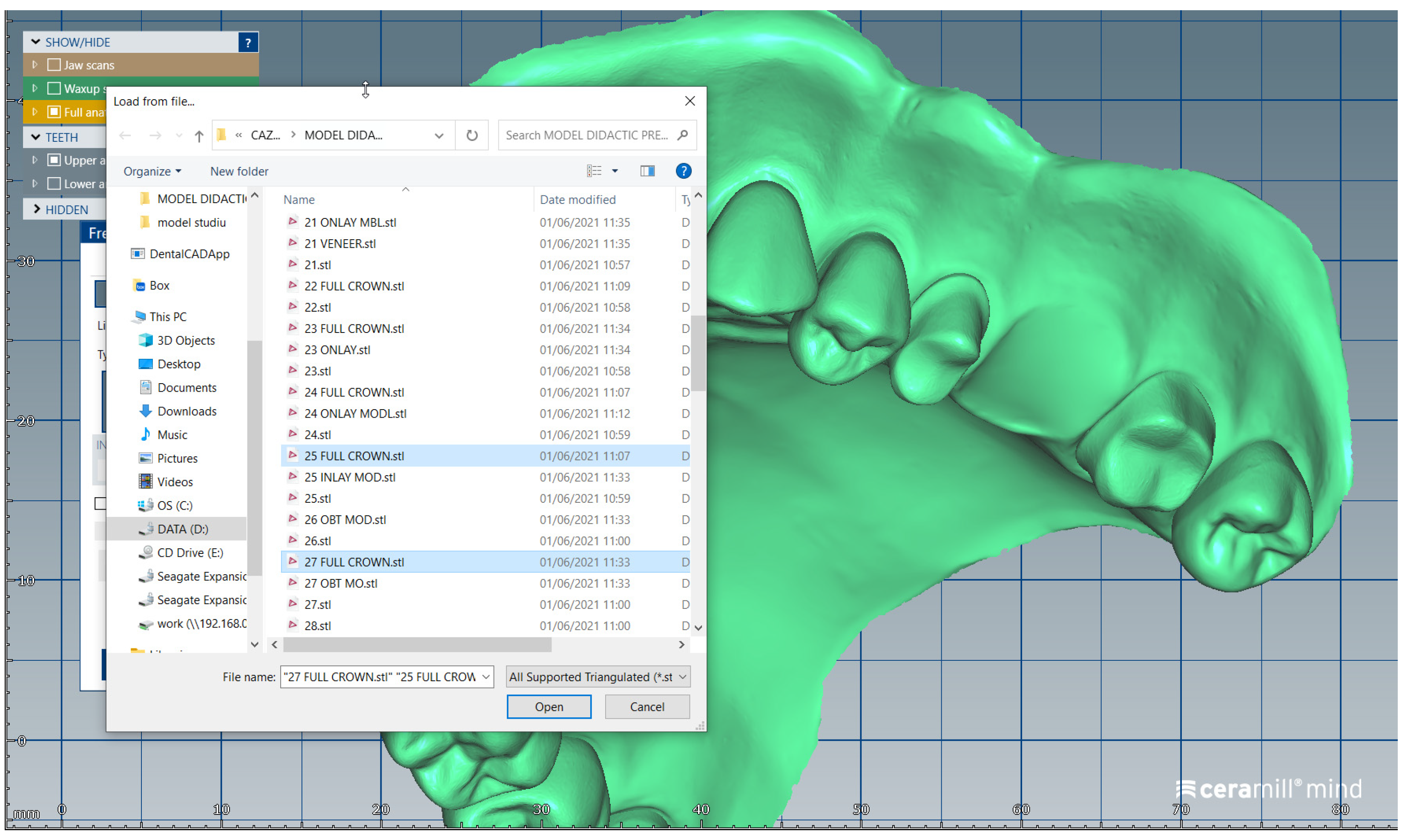
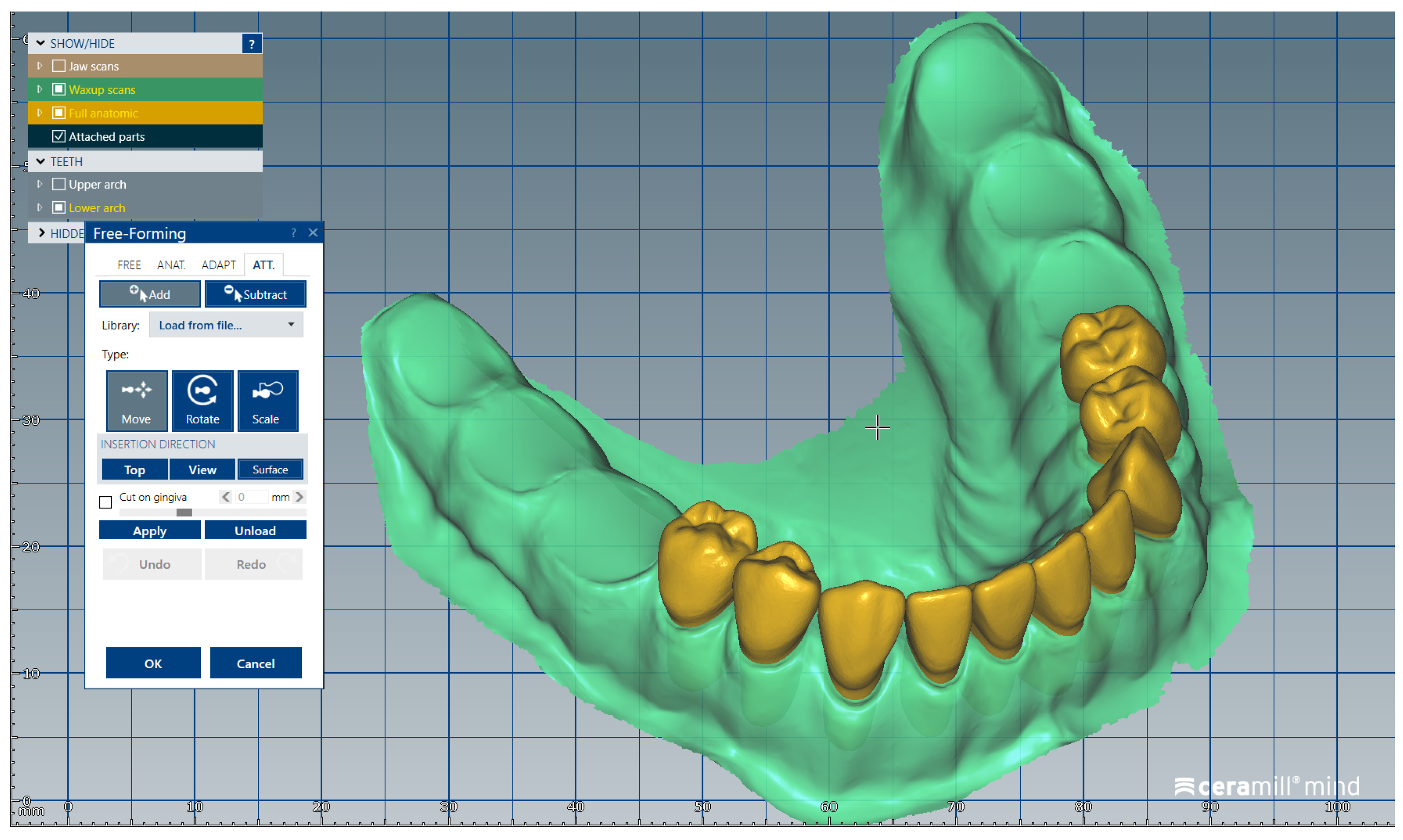
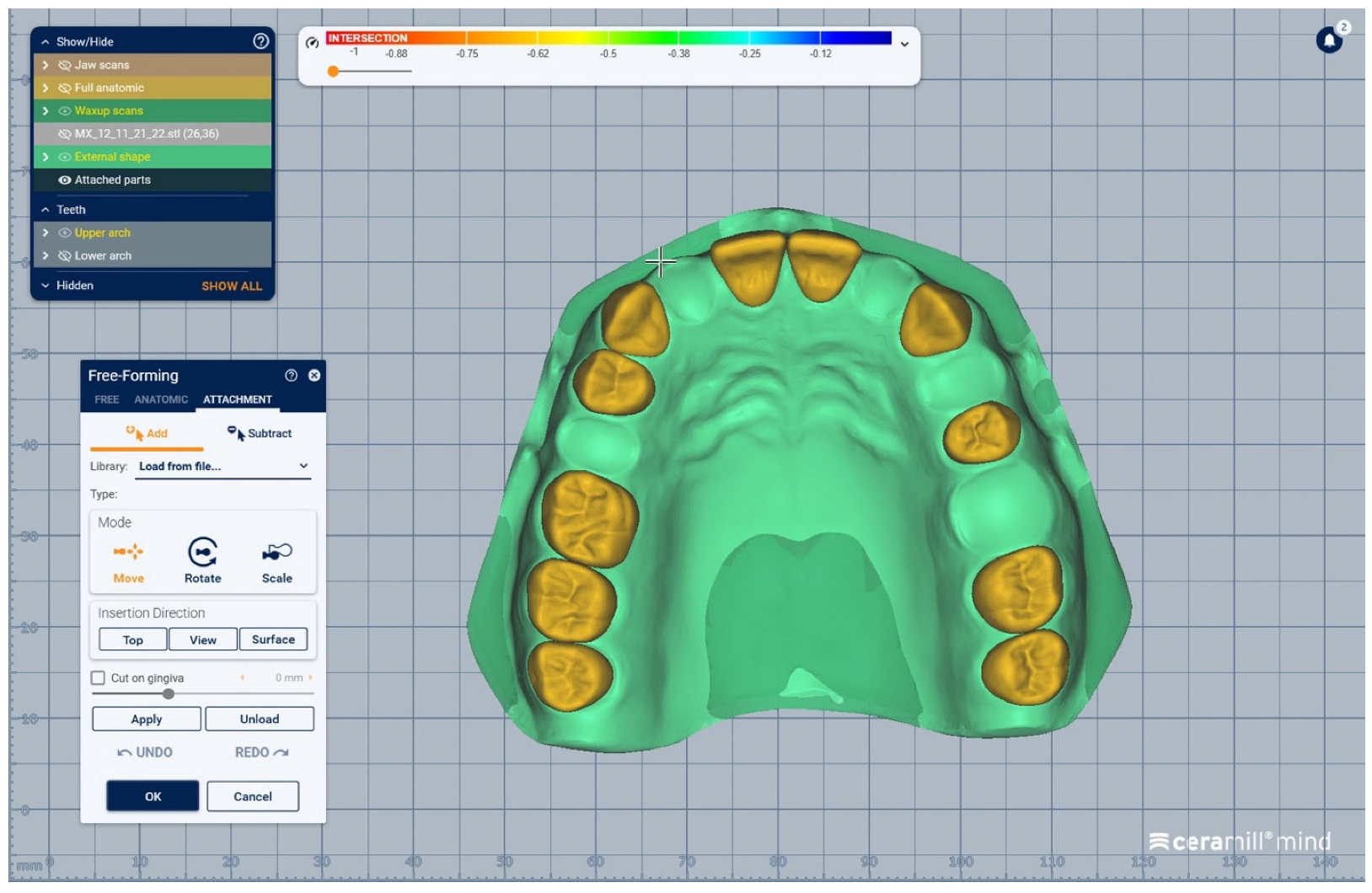
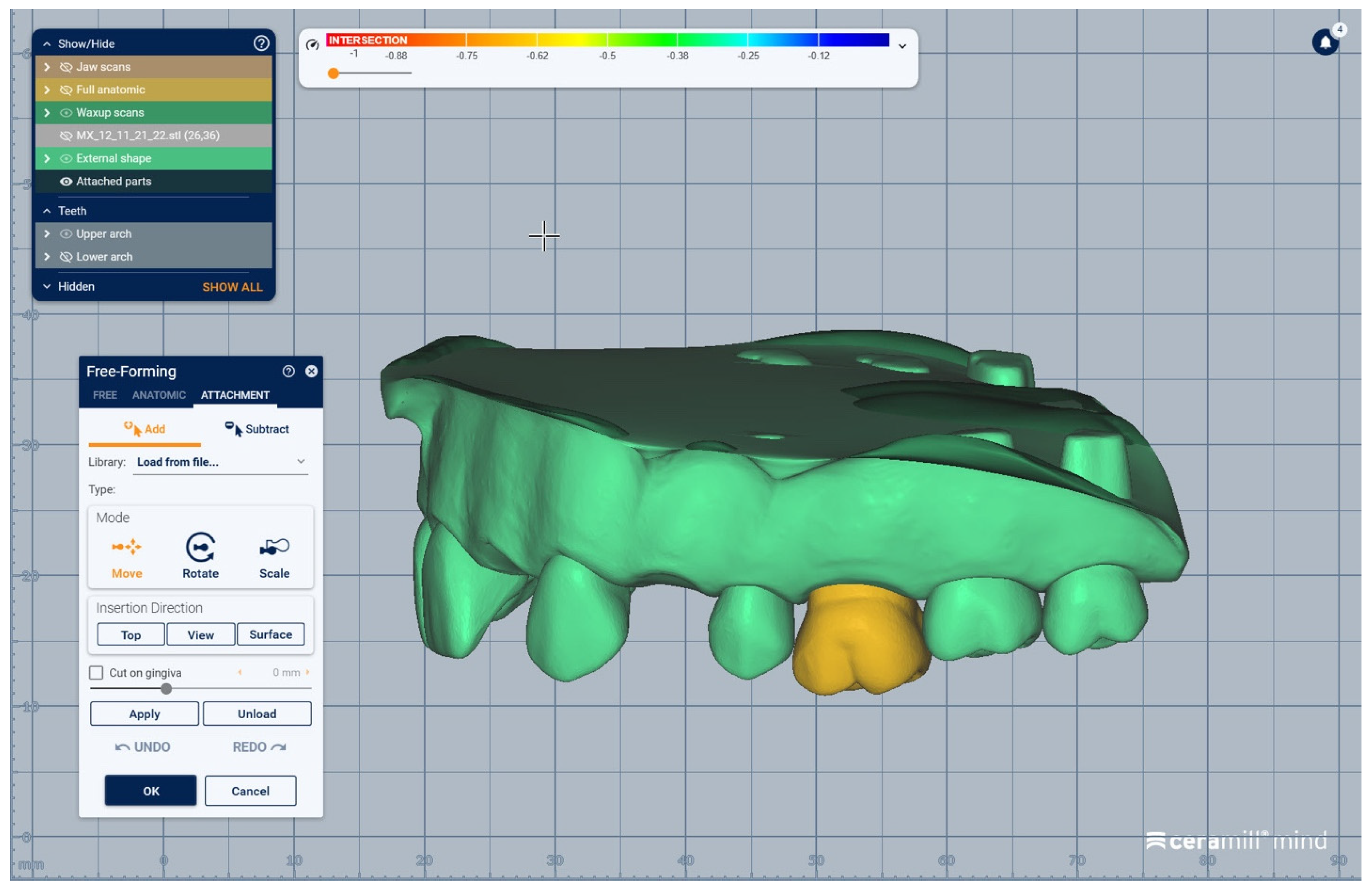
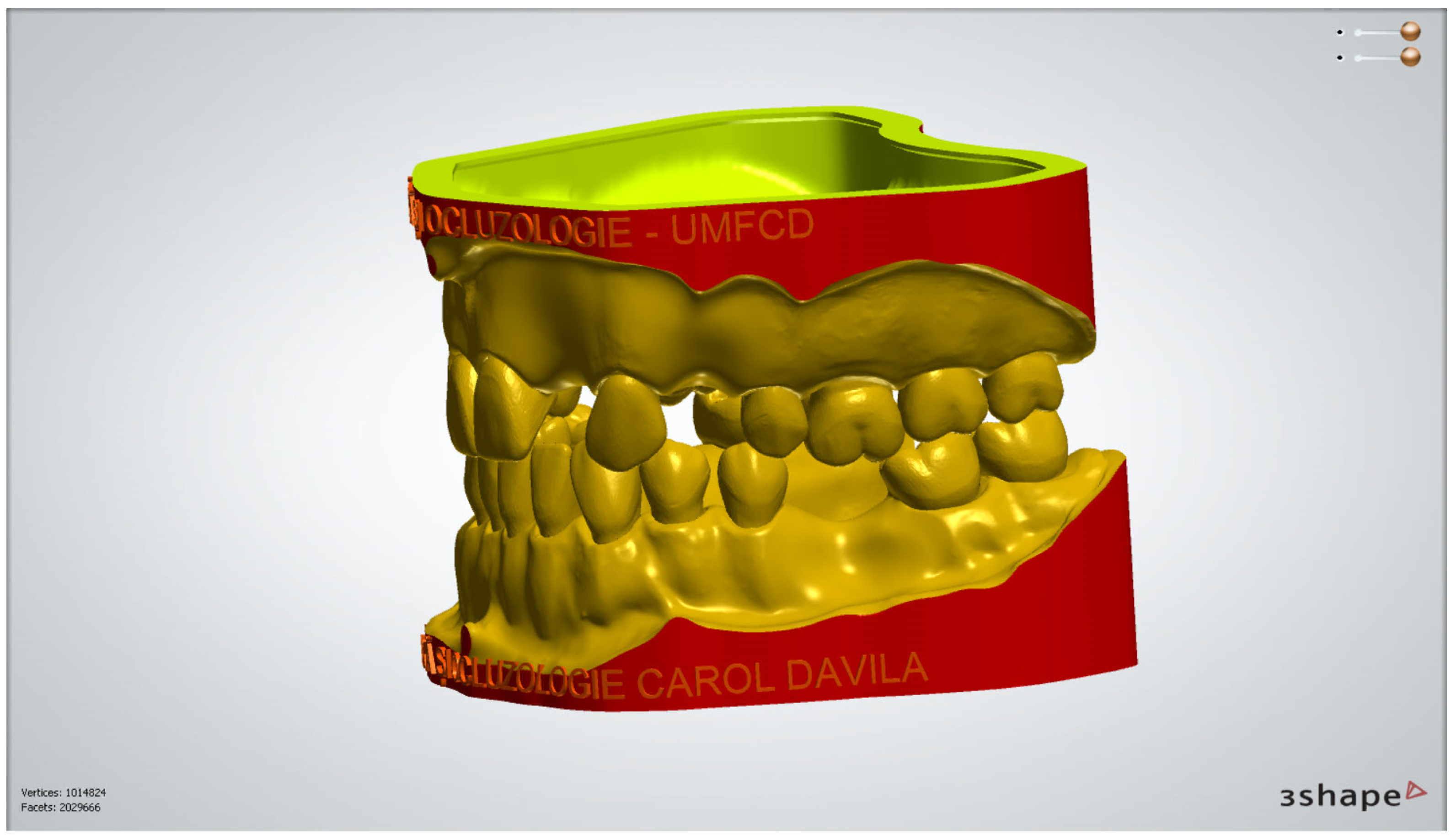
2.1.2. Design of the Modular Dental Models
2.1.3. Additive Manufacturing of the Dental Models
2.2. Evaluation of Undergraduate Students’ Opinion on the Use of Modular Digital and 3D-Printed Dental Models in University Dental Education
2.2.1. Survey Methodology and Ethical Approval
2.2.2. Selection of Participants
2.2.3. Survey Questionnaire
2.2.4. Data Analysis
3. Results
3.1. Modular Digital and 3D-Printed Dental Models
3.2. Students’ Opinion on the Use of Modular Digital and 3D-Printed Dental Models in University Dental Education
- –
- the most-selected answer for the functions of modular digital dental models (question 4) was the realistic simulation of various classes of partial edentulism (81%); corresponding to functions of 3D-printed dental models (question 11), the most-selected answer was option A (improvement of practical skills) (78.5%);
- –
- the most-selected answer for advantages of modular digital dental models in university training (question 5) was option A (3D visualization of details) (85.9%); in the same line, the most-selected answer for the advantages of 3D-printed dental models in university training (question 12) was option A (real/3D visualization of details) (82.9%);
- –
- the most-selected answer for advantages of modular digital dental models as a method of e-learning (question 6) was option A (easy access from various locations) (86.8%); in the case of 3D-printed dental models, the most-selected advantage was that the use of these 3D-printed models allows direct feedback to students from teachers (77.1%);
- –
- the most-selected answer for the disadvantages of modular digital dental models as a method of e-learning (question 7) was option D (limitation of direct interaction with patients) (69.3%); as for the 3D-printed dental models, the most-selected answer for their disadvantages was option B (hardness of the printed material is different from that of natural teeth) (91.7%);
- –
- most responses were affirmative to questions 8 (76.6%), 9 (82.9%) and 10 (91.7%),which are related to the virtual simulation method, and to questions 15 (84.9%), 16 (90.2%), and 17 (92.7%), which are related to the 3D-printed dental models. The students were asked if they feel better-prepared for their clinical activity by using the proposed methods (question 8 and 15), if the methods fits their way of learning (question 9 and 16) and if they are interested in further use of the proposed methods in university training (question 10 and 17). It can be noted that the questions related to 3D-printed dental models registered a slightly higher affirmative response percentage than the questions related to the virtual simulation method (modular digital models);
- –
- most of the students responded affirmatively to question 18 (obtaining virtual/3D-printed models from real clinical cases is an advantage) (96.6%), question 19 (usage of virtual/3D-printed models improves professional skills in digital technology and 3D-printing) (92.7%), and question 20 (development of virtual/3D-printed dental models would be of interest to future generations of students) (96.6%).
- –
- Students who selected option 4A (modular digital dental models allow realistic simulation of various classes of partial edentulism) were more frequently in their fourth academic year (85.7% vs. 74.4%) (p = 0.048);
- –
- Students who selected option 4C (modular digital dental models allow realistic simulation of alveolar ridge resorption) were more frequently in their fourth academic year (65.5% vs. 51.2%) (p = 0.044);
- –
- Students who selected option 4D (modular digital dental models allow realistic simulation of malpositioned teeth and destruction of dental crowns) were more frequently in their fourth academic year (76.5% vs. 61.6%) (p = 0.030);
- –
- Students who selected option 5D (modular digital dental models are a quick way to learn) were more frequently in their third academic year (46.5% vs. 27.7%) (p = 0.008);
- –
- Students who selected option 7C (modular digital dental models are limited in terms of direct interaction with teachers) were more frequently in their fourth academic year (64.7% vs. 47.7%) (p = 0.022);
- –
- Students who answered that modular digital dental models fit their way of learning (question 9) were more frequently in their third academic year (89.5% vs. 78.2%) (p = 0.039);
- –
- Students who selected option 12D (3D-printed dental models are a quick way to learn) were more frequently in their third academic year (45.3% vs. 28.6%) (p = 0.018);
- –
- Students who selected option 13B (3D-printed dental models allow direct interaction between students and teachers) were more frequently in their fourth academic year (59.7% vs. 40.7%) (p = 0.011);
- –
- Students who answered that virtual/3D-printed dental models would be of interest to future generations of students (question 20) were more frequently in their third academic year (100% vs. 94.1%) (p = 0.043).
- –
- Students who selected item 5A (modular digital dental models allow 3D visualization of details) more frequently also selected item 12A (3D-printed dental models allow 3D visualization of details) (90.6% vs. 62.9%) (p < 0.001);
- –
- Students who selected item 5B (modular digital dental models allow repeated virtual simulations) more frequently also selected item 12B (3D-printed dental models allow repeated attempts of various practical procedures) (81.9% vs. 36.1%) (p < 0.001);
- –
- Students who selected item 5C (modular digital dental models are an accessible and flexible method of learning) more rarely also selected item 12C (3D-printed dental models are an accessible and flexible method of learning) (78.8% vs. 43.8%) (p < 0.001);
- –
- Students who selected item 5D (modular digital dental models are a quick way to learn) more frequently also selected item 12D (3D-printed dental models are a quick way to learn) (68.5% vs. 17.4%) (p < 0.001);
- –
- Students who selected item 5E (modular digital dental models are a comfortable way of learning) more frequently also selected item 12E (3D-printed dental models are a comfortable way of learning) (67% vs. 26.5%) (p < 0.001);
- –
- Students who selected item 6C (modular digital dental models allow fast virtual feedback to students from teachers) more frequently also selected item 13C (3D-printed dental models allow direct feedback to students from teachers) (60.8% vs. 42.6%) (p = 0.030);
- –
- Students who answered that modular digital models are a good way to prepare for their clinical activity (question 8) more frequently also answered that 3D-printed dental models are a good way to prepare for their clinical activity (question 15) (83.3% vs. 38.7%) (p < 0.001);
- –
- Students who answered that modular digital models fit their way of learning (question 9) more frequently also answered that 3D-printed dental models fit their way of learning (question 16) (87.6% vs. 40%) (p < 0.001);
- –
- Students who answered that they are interested in further use of modular digital models (question 10) more frequently also answered that they are interested in further use of 3D-printed dental models (question 17) (95.3% vs. 46.7%) (p < 0.001);
- –
- Students who answered that obtaining virtual/3D-printed dental models from real clinical cases is an advantage (question 18) more frequently also answered that virtual/3D-printed dental models can help them improve their professional skills in digital technology and 3D-printing (question 19) (98.9% vs. 66.7%) (p < 0.001);
- –
- Students who answered that obtaining virtual/3D-printed dental models from real clinical cases is an advantage (question 18) more frequently also answered that development of virtual/3D-printed dental models would be of interest to future generations of students (question 20) (98.5% vs. 42.9%) (p < 0.001);
- –
- Students who answered that virtual/3D-printed dental models can help them improve their professional skills in digital technology and 3D-printing (question 19) more frequently also answered that development of virtual/3D-printed dental models would be of interest to future generations of students (question 20) (94.9% vs. 28.6%) (p < 0.001).
4. Discussion
5. Conclusions
- The present paper advances an alternative digital proposal dedicated to dental education of students in the domain of prosthodontics, allowing the creation digital modular dental models corresponding to various clinical situations of partial edentulism and to subsequently obtain 3D-printed dental models that can be used for students’ practical training. The suggested method stimulates students to project, create, previsualize and interact with modular didactic digital models and to perform repeated virtual simulation of any possible partial edentulism scenario; on the other hand, the 3D-printed models offer the possibility to enhance students’ practical skills.
- As we registered positive feedback from students participating in the survey, the proposed method could offer students at the pre-clinical stage of their education the opportunity to train and prepare themselves better for their future clinical activities.
- The proposed method could pave the way for various practical training applications in dental education, fostering its sustainability and encouraging interdisciplinary collaboration.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Revilla-León, M.; Jiang, P.; Sadeghpour, M.; Piedra-Cascón, W.; Zandinejad, A.; Özcan, M.; Krishnamurthy, V.R. Intraoral digital scans—Part 1: Influence of ambient scanning light conditions on the accuracy (trueness and precision) of different intraoral scanners. J. Prosthet. Dent. 2020, 124, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Bandiaky, O.N.; Le Bars, P.; Gaudin, A.; Hardouin, J.B.; Cheraud-Carpentier, M.; Mbodj, E.B.; Soueidan, A. Comparative assessment of complete-coverage, fixed tooth-supported prostheses fabricated from digital scans or conventional impressions: A systematic review and meta-analysis. J. Prosthet. Dent. 2020, 127, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Winkler, J.; Gkantidis, N. Trueness and precision of intraoral scanners in the maxillary dental arch: An In Vivo analysis. Sci. Rep. 2020, 10, 1172. [Google Scholar] [CrossRef] [PubMed]
- Nedelcu, R.; Olsson, P.; Nyström, I.; Rydén, J.; Thor, A. Accuracy and precision of 3 intraoral scanners and accuracy of conventional impressions: A novel in vivo analysis method. J. Dent. 2018, 69, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Bosniac, P.; Rehmann, P.; Wöstmann, B. Comparison of an indirect impression scanning system and two direct intraoral scanning systems In Vivo. Clin. Oral. Investig. 2018, 23, 2421–2427. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A. Current status and applications of additive manufacturing in dentistry: A literature-based review. J. Oral Biol. Craniofacial Res. 2019, 9, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D-printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef]
- Jockusch, J.; Özcan, M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent. Mater. J. 2020, 39, 345–354. [Google Scholar] [CrossRef]
- Nassani, M.; Ibraheem, S.; Shamsy, E.; Darwish, M.; Faden, A.; Kujan, O. A Survey of Dentists’ Perception of Chair-Side CAD/CAM Technology. Healthcare 2021, 9, 68. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D-printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Pituru, S.M.; Greabu, M.; Totan, A.; Imre, M.; Pantea, M.; Spinu, T.; Tancu, A.M.C.; Popoviciu, N.O.; Stanescu, I.-I.; Ionescu, E. A Review on the Biocompatibility of PMMA-Based Dental Materials for Interim Prosthetic Restorations with a Glimpse into Their Modern Manufacturing Techniques. Materials 2020, 13, 2894. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Bornstein, M.M.; Jung, R.E.; Ferrari, M.; Waltimo, T.; Zitzmann, N.U. Recent trends and future direction of dental research in the digital era. Int. J. Environ. Res. Public Health 2020, 17, 1987. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial intelligence in dentistry: Chances and challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Ho, D.; Quake, S.R.; McCabe, E.R.; Chng, W.J.; Chow, E.K.; Ding, X.; Gelb, B.D.; Ginsburg, G.S.; Hassenstab, J.; Ho, C.-M.; et al. Enabling Technologies for Personalized and Precision Medicine. Trends Biotechnol. 2020, 38, 497–518. [Google Scholar] [CrossRef] [PubMed]
- Grischke, J.; Johannsmeier, L.; Eich, L.; Griga, L.; Haddadin, S. Dentronics: Towards robotics and artificial intelligence in dentistry. Dent. Mater. 2020, 36, 765–778. [Google Scholar] [CrossRef]
- Neville, P.; van der Zande, M.M. Dentistry, E-health and digitalisation: A critical narrative review of the dental literature on digital technologies with insights from health and technology studies. Community Dent. Health J. 2020, 37, 51–58. [Google Scholar] [CrossRef]
- Barour, S.; Richert, R.; Virard, F.; Wulfman, C.; Iozzino, R.; Elbashti, M.; Naveau, A.; Ducret, M. Immersive 3D Educational Contents: A Technical Note for Dental Educators. Healthcare 2021, 9, 178. [Google Scholar] [CrossRef]
- Wulfman, C.; Bonnet, G.; Carayon, D.; Lance, C.; Fages, M.; Vivard, F.; Daas, M.; Rignon-Bret, C.; Naveau, A.; Millet, C.; et al. Digital removable complete denture: A narrative review. Fr. J. Dent. Med. 2020, 10, 1–9. [Google Scholar]
- Rekow, E.D. Digital Dentistry: The New State of the Art—Is It Disruptive or Destructive? Dent. Mater. 2020, 36, 9–24. [Google Scholar] [CrossRef]
- Kato, A.; Ziegler, A.; Utsumi, M.; Ohno, K.; Takeichi, T. Three-dimensional imaging of internal tooth structures: Applications in dental education. J. Oral Biosci. 2016, 58, 100–111. [Google Scholar] [CrossRef][Green Version]
- Schepke, U.; Palthe, M.E.V.W.; Meisberger, E.W.; Kerdijk, W.; Cune, M.S.; Blok, B. Digital assessment of a retentive full crown preparation—An evaluation of prepCheck in an undergraduate pre-clinical teaching environment. Eur. J. Dent. Educ. 2020, 24, 407–424. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, G.; Lance, C.; Bessadet, M.; Tamini, F.; Veyrune, J.-L.; Francois, O.; Nicolas, E. Teaching removable partial denture design: ‘METACIEL’, a novel digital procedure. Int. J. Med. Educ. 2018, 9, 24–25. [Google Scholar] [CrossRef] [PubMed]
- De Boer, I.R.; Wesselink, P.R.; Vervoorn, J.M. The creation of virtual teeth with and without tooth pathology for a virtual learning environment in dental education. Eur. J. Dent. Educ. 2013, 17, 191–197. [Google Scholar] [CrossRef] [PubMed]
- De Boer, I.R.; Wesselink, P.R.; Vervoorn, J.M. Student performance and appreciation using 3D vs. 2D vision in a virtual learning environment. Eur. J. Dent. Educ. 2015, 20, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Güth, J.F.; Ponn, A.; Mast, G.; Gernet, W.; Edelhoff, D. Description and evaluation of a new approach on pre-clinical implant dentistry education based on an innovative simulation model. Eur. J. Dent. Educ. 2010, 14, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Dixon, J.; Towers, A.; Martin, N.; Field, J. Re-defining the virtual reality dental simulator: Demonstrating concurrent validity of clinically relevant assessment and feedback. Eur. J. Dent. Educ. 2021, 25, 108–116. [Google Scholar] [CrossRef]
- Towers, A.; Field, J.; Stokes, C.; Maddock, S.; Martin, N. A scoping review of the use and application of virtual reality in pre-clinical dental education. Br. Dent. J. 2019, 226, 358–366. [Google Scholar] [CrossRef]
- Nassar, H.M.; Tekian, A. Computer simulation and virtual reality in undergraduate operative and restorative dental education: A critical review. J. Dent. Educ. 2020, 84, 812–829. [Google Scholar] [CrossRef]
- Sajdłowski, D.; Świątkowski, W.; Rahnama, M. Dental Education in COVID-19 Pandemic. World J. Surg. Res. 2021, 4, 1283. [Google Scholar]
- Jalali, P.; Glickman, G.N.; Umorin, M. Do didactics improve clinical skills: A retrospective educational study. Saudi Endod. J. 2021, 11, 31. [Google Scholar]
- Sjöström, M.; Brundin, M. The Effect of Extra Educational Elements on the Confidence of Undergraduate Dental Students Learning to Administer Local Anaesthesia. Dent. J. 2021, 9, 77. [Google Scholar] [CrossRef]
- McGleenon, E.L.; Morison, S. Preparing dental students for independent practice: A scoping review of methods and trends in undergraduate clinical skills teaching in the UK and Ireland. Br. Dent. J. 2021, 230, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Savoldi, F.; Yeung, A.W.K.; Tanaka, R.; Zadeh, L.S.M.; Montalvao, C.; Bornstein, M.M.; Tsoi, J.K.H. Dry skulls and cone beam computed tomography (CBCT) for teaching orofacial bone anatomy to undergraduate dental students. Anat. Sci. Educ. 2021, 14, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, S.; Nahar, P.; Shaikh, S.; Sayed, A.J.; Habibullah, M.A. Current perspectives of 3D-printing in dental applications. Braz. Dent. Sci. 2021, 24, 2481. [Google Scholar] [CrossRef]
- Coro-Montanet, G.; Monedero, M.J.P.; Ituarte, J.S.; Calvo, A.d.l.H. Train Strategies for Haptic and 3D Simulators to Improve the Learning Process in Dentistry Students. Int. J. Environ. Res. Public Health 2022, 19, 4081. [Google Scholar] [CrossRef]
- Murbay, S.; Neelakantan, P.; Chang, J.W.W.; Yeung, S. Evaluation of the introduction of a dental virtual simulator on the performance of undergraduate dental students in the pre-clinical operative dentistry course. Eur. J. Dent. Educ. 2020, 24, 5–16. [Google Scholar] [CrossRef]
- Zitzmann, N.U.; Matthisson, L.; Ohla, H.; Joda, T. Digital undergraduate education in dentistry: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 3269. [Google Scholar] [CrossRef]
- Mahrous, A.; Schneider, G.B.; Holloway, J.A.; Dawson, D.V. Enhancing student learning in removable partial denture design by using virtual three-dimensional models versus traditional two-dimensional drawings: A comparative study. J. Prosthodont. 2019, 28, 927–933. [Google Scholar] [CrossRef]
- Goodacre, C.J. Digital Learning Resources for Prosthodontic Education: The Perspectives of a Long-Term Dental Educator Regarding 4 Key Factors. J. Prosthodont. 2018, 27, 791–797. [Google Scholar] [CrossRef]
- Ferro, A.S.; Nicholson, K.; Koka, S. Innovative Trends in Implant Dentistry Training and Education: A Narrative Review. J. Clin. Med. 2019, 8, 1618. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; Peter, T.; Rüttermann, S.; Sader, R.; Seifert, L.B. 3D printed versus commercial models in undergraduate conservative dentistry training. Eur. J. Dent. Educ. 2022, 26, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Zaharia, C.; Gabor, A.G.; Gavrilovici, A.; Stan, A.T.; Idorasi, L.; Sinescu, C.; Negruțiu, M.L. Digital dentistry-3D printing applications. J. Interdiscip. Med. 2017, 2, 50–53. [Google Scholar] [CrossRef]
- Soares, P.V.; Milito, G.d.A.; Pereira, F.A.; Reis, B.R.; Soares, C.; Menezes, M.D.S.; Santos-Filho, P.C.D.F. Rapid prototyping and 3D-virtual models for operative dentistry education in Brazil. J. Dent. Educ. 2013, 77, 358–363. [Google Scholar] [CrossRef]
- Terry, A.; Liu, D.; Divnic-Resnik, T. The impact of an electronic guide on students’ self-directed learning in simulation clinic. Eur. J. Dent. Educ. 2021, 25, 86–99. [Google Scholar] [CrossRef] [PubMed]
- Schlenz, M.A.; Schmidt, A.; Wöstmann, B.; Krämer, N.; Schulz-Weidner, N. Students’ and lecturers’ perspective on the implementation of online learning in dental education due to SARS-CoV-2 (COVID-19): A cross-sectional study. BMC Med. Educ. 2020, 20, 354. [Google Scholar] [CrossRef]
- Shrivastava, K.J.; Nahar, R.; Parlani, S.; Murthy, V.J. A cross-sectional virtual survey to evaluate the outcome of online dental education system among undergraduate dental students across India amid COVID-19 pandemic. Eur. J. Dent. Educ. 2021, 26, 123–130. [Google Scholar] [CrossRef]
- Mladenovic, R.; Bukumiric, Z.; Mladenovic, K. Influence of a dedicated mobile application on studying traumatic dental injuries during student isolation. J. Dent. Educ. 2020, 85, 1131–1133. [Google Scholar] [CrossRef]
- Tang, L.; Cao, Y.; Liu, Z.; Qian, K.; Liu, Y.; Liu, Y.; Zhou, Y. Improving the quality of preclinical simulation training for dental students using a new digital real-time evaluation system. Eur. J. Dent. Educ. 2021, 25, 100–107. [Google Scholar] [CrossRef]
- Mino, T.; Kurosaki, Y.; Tokumoto, K.; Higuchi, T.; Nakanoda, S.; Numoto, K.; Tosa, I.; Kimura-Ono, A.; Maekawa, K.; Kim, T.H.; et al. Rating criteria to evaluate student performance in digital wax-up training using multi-purpose software. J. Adv. Prosthodont. 2022, 14, 203–211. [Google Scholar] [CrossRef]
- Lee, B.; Kim, J.; Shin, S.; Kim, J.; Park, J.; Kim, K.; Kim, S.; Shim, J. Dental students’ perceptions on a simulated practice using patient-based customised typodonts during the transition from preclinical to clinical education. Eur. J. Dent. Educ. 2022, 26, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.; Yang, Z.; Mongrain, R.; Leask, R.L.; Lachapelle, K. 3D-printing materials and their use in medical education: A review of current technology and trends for the future. BMJ Simul. Technol. Enhanc. Learn. 2018, 4, 27–40. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, Z.; Wu, D.; Bai, J. Current status and prospects of polymer powder 3D-printing technologies. Materials 2020, 13, 2406. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Sadeghpour, M.; Özcan, M. An update on applications of 3D-printing technologies used for processing polymers used in implant dentistry. Odontology 2020, 108, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Hotza, D.; Fredel, M.; Cruz, A.; Volpato, C. Materials and Manufacturing Techniques for Polymeric and Ceramic Scaffolds Used in Implant Dentistry. J. Compos. Sci. 2021, 5, 78. [Google Scholar] [CrossRef]
- Lambrecht, J.; Berndt, D.; Christensen, A.; Zehnder, M. Haptic model fabrication for undergraduate and postgraduate teaching. Int. J. Oral. Maxillofac. Surg. 2010, 39, 1226–1229. [Google Scholar] [CrossRef]
- Kröger, E.; Dekiff, M.; Dirksen, D. 3D-printed simulation models based on real patient situations for hands-on practice. Eur. J. Dent. Educ. 2017, 21, e119–e125. [Google Scholar] [CrossRef] [PubMed]
- Höhne, C.; Schwarzbauer, R.; Schmitter, M. 3D-printed teeth with enamel and dentin layer for educating dental students in crown preparation. J. Dent. Educ 2019, 83, 1457–1463. [Google Scholar] [CrossRef] [PubMed]
- Höhne, C.; Schmitter, M. 3D-printed Teeth for the Preclinical Education of Dental Students. J. Dent. Educ. 2019, 83, 1100–1106. [Google Scholar] [CrossRef]
- Boonsiriphant, P.; Al-Salihi, Z.; Holloway, J.A.; Schneider, G.B. The use of 3D-printed tooth preparation to assist in teaching and learning in preclinical fixed prosthodontics courses. J. Prosthod. 2019, 28, e545–e547. [Google Scholar] [CrossRef]
- Werz, S.M.; Zeichner, S.J.; Berg, B.-I.; Zeilhofer, H.-F.; Thieringer, F. 3D-printed surgical simulation models as educational tool by maxillofacial surgeons. Eur. J. Dent. Educ. 2018, 22, e500–e505. [Google Scholar] [CrossRef] [PubMed]
- Hanisch, M.; Kroeger, E.; Dekiff, M.; Timme, M.; Kleinheinz, J.; Dirksen, D. 3D-printed Surgical Training Model Based on Real Patient Situations for Dental Education. Int. J. Environ. Res. Public Health 2020, 17, 2901. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-Y.; Cho, J.-W.; Chang, N.-Y.; Chae, J.-M.; Kang, K.-H.; Kim, S.-C.; Cho, J.-H. Accuracy of three-dimensional printing for manufacturing replica teeth. Korean J. Orthod. 2015, 45, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Marty, M.; Broutin, A.; Vergnes, J.-N.; Vaysse, F. Comparison of student’s perceptions between 3D-printed models versus series models in paediatric dentistry hands-on session. Eur. J. Dent. Educ. 2019, 23, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Schlenz, M.A.; Michel, K.; Wegner, K.; Schmidt, A.; Rehmann, P.; Wostmann, B. Undergraduate dental students’ perspective on the implementation of digital dentistry in the preclinical curriculum: A questionnaire survey. BMC Oral. Health 2020, 20, 78. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Kim, J.; Jeong, Y.; Yun, M.; Lee, H. Comparison of digital and conventional assessment methods for a single tooth preparation and educational satisfaction. Eur. J. Dent. Educ. 2022, 1–9. [Google Scholar] [CrossRef]
- Ishida, Y.; Kuwajima, Y.; Kobayashi, T.; Yonezawa, Y.; Asack, D.; Nagai, M.; Kondo, H.; Ishikawa-Nagai, S.; Da Silva, J.; Lee, S.J. Current Implementation of Digital Dentistry for Removable Prosthodontics in US Dental Schools. Int. J. Dent. 2022, 2022, 7331185. [Google Scholar] [CrossRef] [PubMed]
- Sharab, L.; Adel, M.; Abualsoud, R.; Hall, B.; Albaree, S.; de Leeuw, R.; Kutkut, A. Perception, awareness, and attitude toward digital dentistry among pre-dental students: An observational survey. Bull. Natl. Res. Cent. 2022, 46, 246. [Google Scholar] [CrossRef]
- Zotti, F.; Cominziolli, A.; Pappalardo, D.; Rosolin, L.; Bertossi, D.; Zerman, N. Proposal for Introducing a Digital Aesthetic Dentistry Course in Undergraduate Program: Contents and Ways of Administration. Educ. Sci. 2022, 12, 441. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Hariri, N.H.; Jahangiri, L. Student’s perception of the impact of e-learning on dental education. J. Contemp. Dent. Pract. 2019, 20, 616–621. [Google Scholar] [CrossRef]
- Duane, B.; Dixon, J.; Ambibola, G.; Aldana, C.; Couglan, J.; Henao, D.; Daniela, T.; Veiga, N.; Martin, N.; Darragh, J.; et al. Embedding environmental sustainability within the modern dental curriculum—Exploring current practice and developing a shared understanding. Eur. J. Dent. Educ. 2021, 25, 541–549. [Google Scholar] [CrossRef]
- Cocârţă, D.; Prodana, M.; Demetrescu, I.; Lungu, P.; Didilescu, A. Indoor Air Pollution with Fine Particles and Implications for Workers’ Health in Dental Offices: A Brief Review. Sustainability 2021, 13, 599. [Google Scholar] [CrossRef]
- Joury, E.; Lee, J.; Parchure, A.; Mortimer, F.; Park, S.; Pine, C.; Ramasubbu, D.; Hillman, L. Exploring environmental sustainability in UK and US dental curricula and related barriers and enablers: A cross-sectional survey in two dental schools. Br. Dent. J. 2021, 230, 605–610. [Google Scholar] [CrossRef]
- Varvara, G.; Bernardi, S.; Bianchi, S.; Sinjari, B.; Piattelli, M. Dental education challenges during the COVID-19 pandemic period in Italy: Undergraduate student feedback, future perspectives, and the needs of teaching strategies for professional development. Healthcare 2021, 9, 454. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.-Y.; Hong, G.; Paganelli, C.; Phantumvanit, P.; Chang, W.-J.; Shieh, Y.-S.; Hsu, M.-L. Innovation of dental education during COVID-19 pandemic. J. Dent. Sci. 2021, 16, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Kui, A.; Jiglau, A.L.; Chisnoiu, A.; Negucioiu, M.; Balhuc, S.; Constantiniuc, M.; Buduru, S. A survey on dental students’ perception regarding online learning during COVID-19 pandemic. Med. Pharm. Rep. 2022, 95, 203–208. [Google Scholar] [CrossRef]
- Poudevigne, M.; Armstrong, E.S.; Mickey, M.; Nelson, M.A.; Obi, C.N.; Scott, A.; Thomas, N.; Thompson, T.N. What’s in Your Culture? Embracing Stability and the New Digital Age in Moving Colleges of Health Professions Virtually during the COVID-19 Pandemic: An Experiential Narrative Review. Educ. Sci. 2022, 12, 137. [Google Scholar] [CrossRef]
- Antoniadou, M.; Rahiotis, C.; Kakaboura, A. Sustainable Distance Online Educational Process for Dental Students during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 9470. [Google Scholar] [CrossRef] [PubMed]
- Wolgin, M.; Grabowski, S.; Elhadad, S.; Frank, W.; Kielbassa, A.M. Comparison of a prepCheck-supported self-assessment concept with conventional faculty supervision in a pre-clinical simulation environment. Eur. J. Dent. Educ. 2018, 22, e522–e529. [Google Scholar] [CrossRef]
- Iozzino, R.; Champin, P.-A.; Richert, R.; Bui, R.; Palombi, O.; Charlin, B.; Tamimi, F.; Ducret, M. Assessing decision-making in education of restorative and prosthetic dentistry: A pilot study. Int. J. Prosthodont. 2020, 34, 585–590. [Google Scholar] [CrossRef]
- Höhne, C.; Jentzsch, A.; Schmitter, M. The “Painting by Numbers Method” for education of students in crown preparation. Eur. J. Dent. Educ. 2020, 25, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Monterubbianesi, R.; Tosco, V.; Vitiello, F.; Orilisi, G.; Fraccastoro, F.; Putignano, A.; Orsini, G. Augmented, Virtual and Mixed Reality in Dentistry: A Narrative Review on the Existing Platforms and Future Challenges. Appl. Sci. 2022, 12, 877. [Google Scholar] [CrossRef]
- Moussa, R.; Alghazaly, A.; Althagafi, N.; Eshky, R.; Borzangy, S. Effectiveness of virtual reality and interactive simulators on dental education outcomes: Systematic review. Eur. J. Dent. 2022, 16, 14–31. [Google Scholar] [CrossRef]
- Imran, E.; Adanir, N.; Khurshid, Z. Significance of Haptic and Virtual Reality Simulation (VRS) in the Dental Education: A Review of Literature. Appl. Sci. 2021, 11, 10196. [Google Scholar] [CrossRef]





| Investigated Aspects | Questions (Q) and Possible Answers |
|---|---|
| (1) Socio-demo-graphic data | Q1. Please enter your age |
| Q2. Please enter your gender | |
| Q3. Please enter your study year | |
| (2) Modular digital dental models | Q4. Modular digital dental models allow the following: |
| a. realistic simulation of various classes of partial edentulism | |
| b. easy identification of various classes of partial edentulism | |
| c. realistic simulation of the alveolar ridges resorption of various degrees | |
| d. realistic simulation of malpositioned teeth and the destruction of dental crowns, of various degrees | |
| e. easy elaboration of various treatment plans | |
| Q5. The three main advantages of using modular digital dental models in my university training are as follows: | |
| a. it allows a 3D visualization of details, in contrast to 2D images | |
| b. it allows repeated virtual simulations (reiteration of virtual simulations) | |
| c. it is an accessible and flexible method of learning | |
| d. it is a quick way to learn | |
| e. it is a comfortable way of learning | |
| Q6. The three main advantages of using modular digital models as a method of e-learning in university dental education are as follows: | |
| a. it allows easy access from various locations | |
| b. it allows virtual interaction (synchronous and asynchronous) between students and teachers | |
| c. it allows fast virtual feedback to students from teachers | |
| d. it allows the storage of digital data for a long time | |
| e. it allows the evaluation of the program’s effectiveness (number of registered downloads) | |
| Q7. The three main disadvantages of using modular digital models as a method of e-learning in university dental education are as follows: | |
| a. it requires technological resources (dedicated electronic devices: computer, laptop etc.) | |
| b. it requires (minimum) experience in the field of computers/(minimum) digital skills | |
| c. limitation of direct interaction with teachers (face-to-face contact) | |
| d. limitation of direct interaction with patients | |
| e. dependence on internet connection | |
| Q8. Using the proposed virtual simulation method makes me feel better prepared for my clinical activity: | |
| a. Yes | |
| b. No | |
| Q9. The proposed virtual simulation method fits my way of learning: | |
| a. Yes | |
| b. No. | |
| Q10. I am interested in further use of the proposed virtual simulation method in my university training: | |
| a. Yes | |
| b. No | |
| (3) 3D-printed dental models | Q11. Practical training on 3D-printed dental models allows me the following: |
| a. to improve my practical skills | |
| b. to learn diverse practical procedures risk-free | |
| c. hands-on training under the supervision of teachers | |
| d. to better understand the performed procedures (dental preparations, impressions, wax-up procedures, interim restorations) | |
| e. good visualization of teeth (position, destruction) and edentulous areas | |
| Q12. The three main advantages of using 3D-printed dental models in my university training are as follows: | |
| a. it allows a real/3D visualization of the details, in contrast to the 2D images | |
| b. it allows repeated attempts of various practical procedures | |
| c. it is an accessible, flexible method of learning | |
| d. it is a quick way to learn | |
| e. it is a comfortable way of learning | |
| Q13. The three main advantages of using 3D-printed dental models in university dental education are as follows: | |
| a. 3D-printing of models is facilitated by the university | |
| b. it allows direct interaction between students and teachers | |
| c. it allows direct feedback to students from teachers | |
| d. 3D-printed models can be scanned and archived as digital models which allow virtual evaluation | |
| e. 3D-printed models can be used for practical training in various dental specialties in different years of study | |
| Q14. The three main disadvantages of using 3D-printed dental models in my university dental training are as follows: | |
| a. the colour of the printed material is different from that of natural teeth | |
| b. the hardness of the printed material is different from that of natural teeth | |
| c. the lightness of the printed material is different from that of natural teeth | |
| d. the absence of a gingival mask | |
| e. the 3D-printed models are brittle | |
| Q15. Practicing on 3D-printed dental models makes me feel better prepared for my clinical activity: | |
| a. Yes | |
| b. No | |
| Q16. The practical training on 3D-printed dental models fits my way of learning: | |
| a. Yes | |
| b. No | |
| Q17. I am interested in further use of 3D-printed dental models in my university training: | |
| a. Yes | |
| b. No | |
| (4) Aspects common to both modular digital and 3D-printed dental models | Q18. I believe that obtaining virtual and 3D-printed dental models from real clinical cases through the proposed methods is an advantage: |
| a. Yes | |
| b. No | |
| Q19. I believe that the use of the proposed methods in my university training can help me to improve my own professional skills in digital technology and 3D-printing: | |
| a. Yes | |
| b. No | |
| Q20. I think that the development of these teaching / learning methods (virtual and 3D-printed dental models) would be of interest to future generations of students: | |
| a. Yes | |
| b. No |
| Parameter | Value |
|---|---|
| Age (Mean ± SD, Median (IQR) | 22.31 ± 1.74, 22 (21–23) |
| Gender (No., %) | 153 (74.6%) Female, 52 (25.4%) Male |
| Year of study (No., %) | 86 (42%) Third year, 119 (58%) Fourth year |
| Question | Selected/Affirmative Answer (No., %) |
|---|---|
| Q4 | 4A-81%, 4B-79.5%, 4C-59.5%, 4D-70.2%, 4E-78% |
| Q5 | 5A-85.9%, 5B-68.3%, 5C-66.3%, 5D-35.6%, 5E-43.9% |
| Q6 | 6A-86.8%, 6B-76.6%, 6C-56.6%, 6D-64.4%, 6E-15.6% |
| Q7 | 7A-62.4%, 7B-55.6%, 7C-57.6%, 7D-69.3%, 7E-55.1% |
| Q8 | 48 (23.4%) Negative, 157 (76.6%) Affirmative |
| Q9 | 35 (17.1%) Negative, 170 (82.9%) Affirmative |
| Q10 | 17 (8.3%) Negative, 188 (91.7%) Affirmative |
| Q11 | 11A-78.5%, 11B-75.6%, 11C-54.6%, 11D-78%, 11E-62.9% |
| Q12 | 12A-82.9%, 12B-70.2%, 12C-35.6%, 12D-35.6%, 12E-42.9% |
| Q13 | 13A-53.2%, 13B-51.7%, 13C-77.1%, 13D-52.7%, 13E-64.9% |
| Q14 | 14A-61.5%, 14B-91.7%, 14C-58%, 14D-42.4%, 14E-44.4% |
| Q15 | 31 (15.1%) Negative, 174 (84.9%) Affirmative |
| Q16 | 20 (9.8%) Negative, 185 (90.2%) Affirmative |
| Q17 | 15 (7.3%) Negative, 190 (92.7%) Affirmative |
| Q18 | 7 (3.4%) Negative, 198 (96.6%) Affirmative |
| Q19 | 15 (7.3%) Negative, 190 (92.7%) Affirmative |
| Q20 | 7 (3.4%) Negative, 198 (96.6%) Affirmative |
| Age/Item | Q5-D | Q5-E | Q6-E | Q13-B | |
|---|---|---|---|---|---|
| Average ± SD | 22.48 ± 1.98 | 22.18 ± 1.78 | 22.22 ± 1.75 | 22.01 ± 1.07 | |
| Median (IQR) | 22 (22–23) | 22 (21–23) | 22 (21–23) | 22 (21–23) | |
| Mean Rank | 109.22 | 96.12 | 98.49 | 93.64 | |
| Selected | Average ± SD | 21.99 ± 1.15 | 22.47 ± 1.69 | 22.78 ± 1.66 | 22.58 ± 2.16 |
| Median (IQR) | 22 (21–23) | 22 (22–23) | 23 (22–23) | 22 (22–23) | |
| Mean Rank | 91.75 | 111.79 | 127.41 | 111.75 | |
| p * | 0.034 | 0.048 | 0.008 | 0.022 | |
| Selected Item /Year of Study | Third Year (N = 86) | Fourth Year (N = 119) | p * | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Q4-A | 64 | 74.4% | 102 | 85.7% | 0.048 |
| Q4-C | 44 | 51.2% | 78 | 65.5% | 0.044 |
| Q4-D | 53 | 61.6% | 91 | 76.5% | 0.030 |
| Q5-D | 40 | 46.5% | 33 | 27.7% | 0.008 |
| Q7-C | 41 | 47.7% | 77 | 64.7% | 0.022 |
| Q9 (Affirmative) | 77 | 89.5% | 93 | 78.2% | 0.039 |
| Q12-D | 39 | 45.3% | 34 | 28.6% | 0.018 |
| Q13-B | 35 | 40.7% | 71 | 59.7% | 0.011 |
| Q20 (Affirmative) | 86 | 100% | 112 | 94.1% | 0.043 |
| Item Q5-A /Q12-A | 12-A-Not Selected | 12-A-Selected | p* | ||
| No. | % | No. | % | ||
| 5-A-Not selected | 13 | 37.1% | 16 | 9.4% | <0.001 |
| 5-A-Selected | 22 | 62.9% | 154 | 90.6% | |
| Item Q5-B /Q12-B | 12-B-Not selected | 12-B-Selected | p* | ||
| No. | % | No. | % | ||
| 5-B-Not selected | 39 | 63.9% | 26 | 18.1% | <0.001 |
| 5-B-Selected | 22 | 36.1% | 118 | 81.9% | |
| Item Q5-C /Q12-C | 12-C-Not Selected | 12-C-Selected | p* | ||
| No. | % | No. | % | ||
| 5-C-Not selected | 28 | 21.2% | 41 | 56.2% | <0.001 |
| 5-C-Selected | 104 | 78.8% | 32 | 43.8% | |
| Item Q5-D /Q12-D | 12-D-Not Selected | 12-D-Selected | p* | ||
| No. | % | No. | % | ||
| 5-D-Not selected | 109 | 82.6% | 23 | 31.5% | <0.001 |
| 5-D-Selected | 23 | 17.4% | 50 | 68.5% | |
| Item Q5-E /Q12-E | 12-E-Not Selected | 12-E-Selected | p* | ||
| No. | % | No. | % | ||
| 5-E-Not selected | 86 | 73.5% | 29 | 33% | <0.001 |
| 5-E-Selected | 31 | 26.5% | 59 | 67% | |
| Item Q6-C /Q13-C | 13-C-Not Selected | 13-C-Selected | p* | ||
| No. | % | No. | % | ||
| 6-C-Not selected | 27 | 57.4% | 62 | 39.2% | 0.030 |
| 6-C-Selected | 20 | 42.6% | 96 | 60.8% | |
| Item Q8 /Q15 | 15-Negative | 15-Affirmative | p* | ||
| No. | % | No. | % | ||
| 8-Negative | 19 | 61.3% | 29 | 16.7% | <0.001 |
| 8-Affirmative | 12 | 38.7% | 145 | 83.3% | |
| Item Q9 /Q16 | 16-Negative | 16-Affirmative | p* | ||
| No. | % | No. | % | ||
| 9-Negative | 12 | 60% | 23 | 12.4% | <0.001 |
| 9-Affirmative | 8 | 40% | 162 | 87.6% | |
| Item Q10 /Q17 | 17-Negative | 17-Affirmative | p* | ||
| No. | % | No. | % | ||
| 10-Negative | 8 | 53.3% | 9 | 4.7% | <0.001 |
| 10-Affirmative | 7 | 46.7% | 181 | 95.3% | |
| Item Q18 /Q19 | 19-Negative | 19-Affirmative | p* | ||
| No. | % | No. | % | ||
| 18-Negative | 5 | 33.3% | 2 | 1.1% | <0.001 |
| 18-Affirmative | 10 | 66.7% | 188 | 98.9% | |
| Item Q18 /Q20 | 20-Negative | 20-Affirmative | p* | ||
| No. | % | No. | % | ||
| 18-Negative | 4 | 57.1% | 3 | 1.5% | <0.001 |
| 18-Affirmative | 3 | 42.9% | 195 | 98.5% | |
| Item Q19 /Q20 | 20-Negative | 20-Affirmative | p* | ||
| No. | % | No. | % | ||
| 19-Negative | 5 | 71.4% | 10 | 5.1% | <0.001 |
| 19-Affirmative | 2 | 28.6% | 188 | 94.9% | |
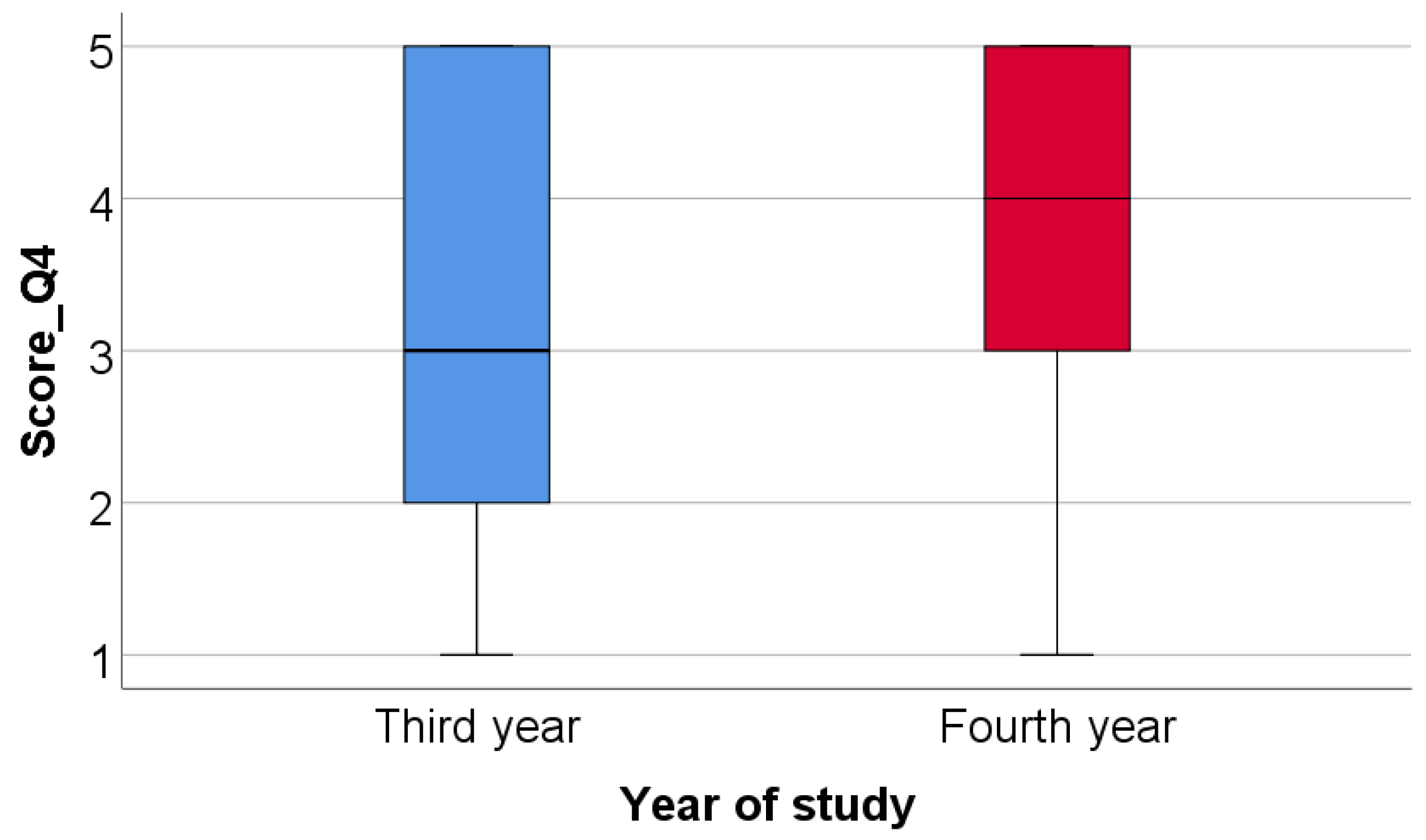
| Year of Study/Score_Q4 | Average ± SD | Median (IQR) | Mean Rank | p * |
|---|---|---|---|---|
| Third year | 3.42 ± 1.53 | 3 (2–5) | 93.76 | 0.046 |
| Fourth year | 3.87 ± 1.29 | 4 (3–5) | 109.68 |
| Correlation | p * |
|---|---|
| Score_Q4 (p < 0.001 **) × Score_Q11 (p < 0.001 **) | <0.001, R = 0.242 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petre, A.E.; Pantea, M.; Drafta, S.; Imre, M.; Țâncu, A.M.C.; Liciu, E.M.; Didilescu, A.C.; Pițuru, S.M. Modular Digital and 3D-Printed Dental Models with Applicability in Dental Education. Medicina 2023, 59, 116. https://doi.org/10.3390/medicina59010116
Petre AE, Pantea M, Drafta S, Imre M, Țâncu AMC, Liciu EM, Didilescu AC, Pițuru SM. Modular Digital and 3D-Printed Dental Models with Applicability in Dental Education. Medicina. 2023; 59(1):116. https://doi.org/10.3390/medicina59010116
Chicago/Turabian StylePetre, Alexandru Eugen, Mihaela Pantea, Sergiu Drafta, Marina Imre, Ana Maria Cristina Țâncu, Eduard M. Liciu, Andreea Cristiana Didilescu, and Silviu Mirel Pițuru. 2023. "Modular Digital and 3D-Printed Dental Models with Applicability in Dental Education" Medicina 59, no. 1: 116. https://doi.org/10.3390/medicina59010116
APA StylePetre, A. E., Pantea, M., Drafta, S., Imre, M., Țâncu, A. M. C., Liciu, E. M., Didilescu, A. C., & Pițuru, S. M. (2023). Modular Digital and 3D-Printed Dental Models with Applicability in Dental Education. Medicina, 59(1), 116. https://doi.org/10.3390/medicina59010116












