Revision of a Failed Primary Total Hip Arthroplasty following Excessive Reaming with a Medial Cup Protrusion
Abstract
:1. Introduction
2. Methods and Patients
2.1. Patient Selection
2.2. Clinical and Radiographic Assessment
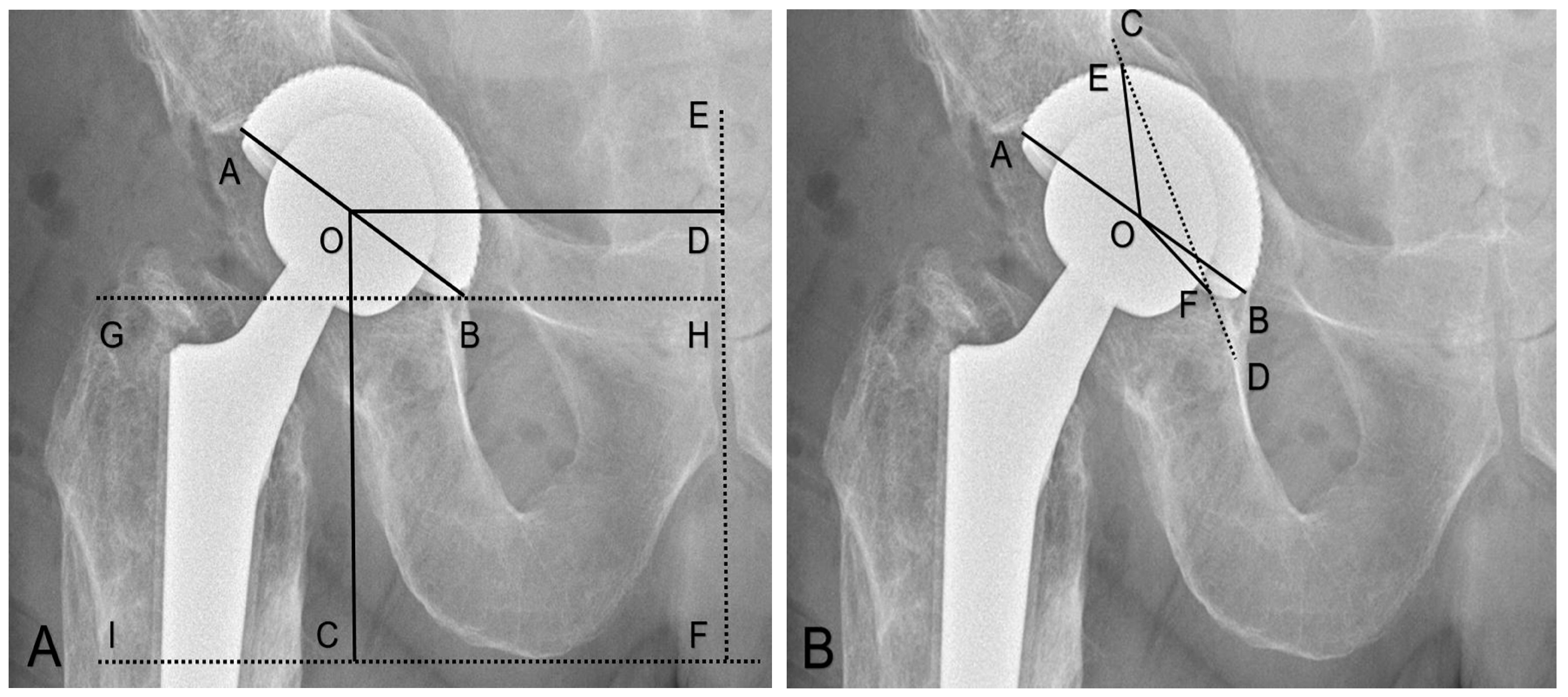
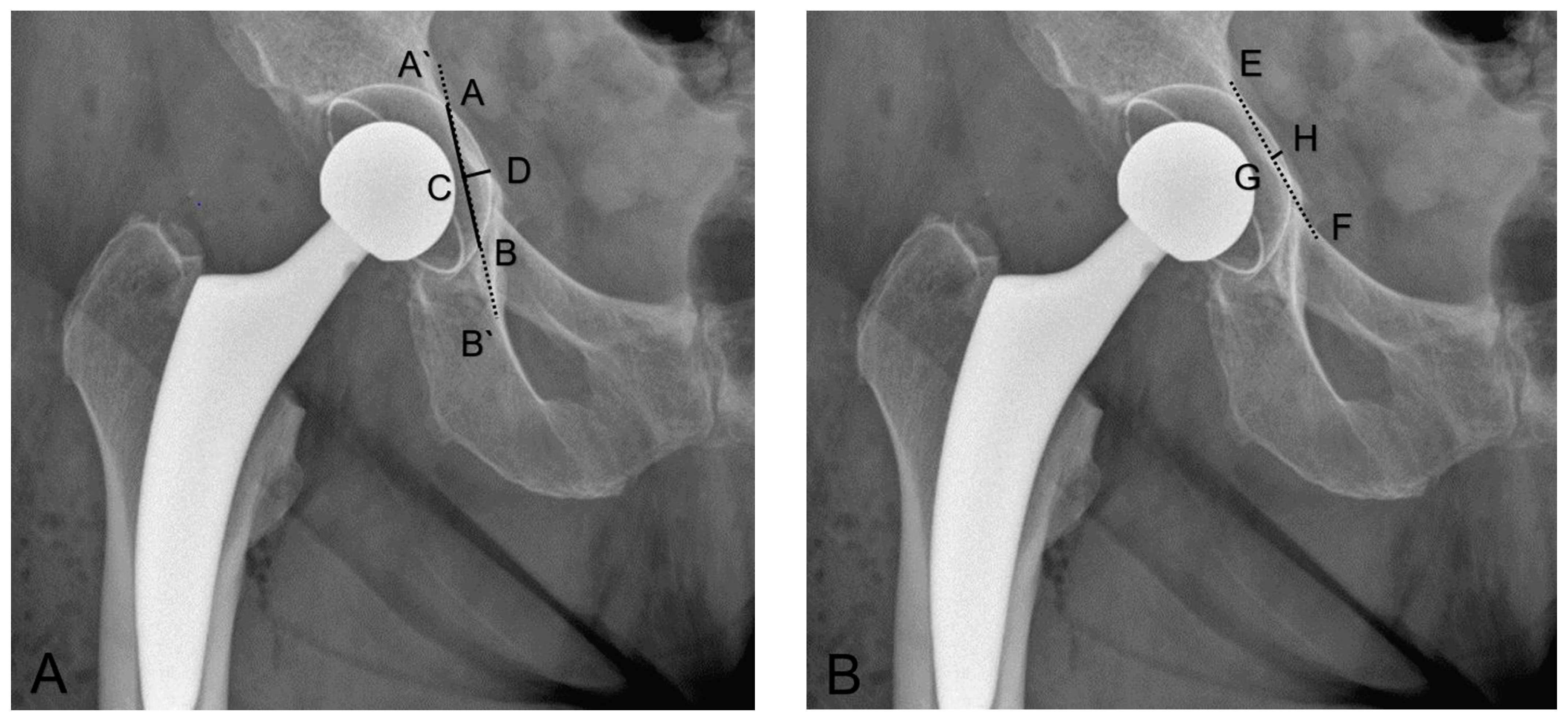
2.2.1. Cup Positioning
2.2.2. Cup Migration at Follow-up
2.2.3. Fracture Healing
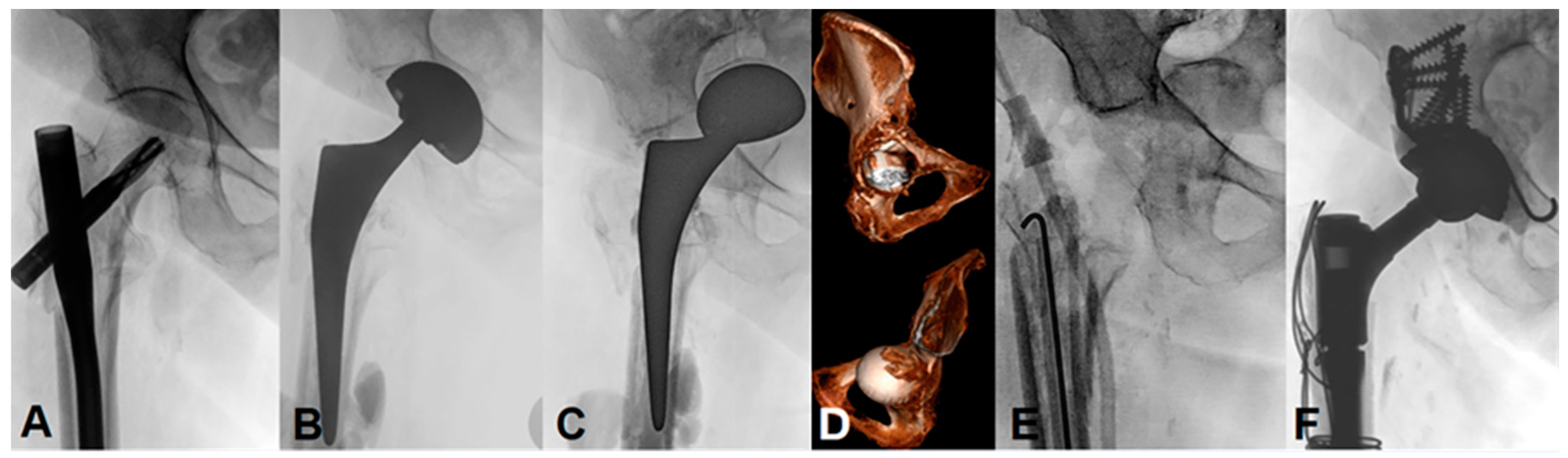
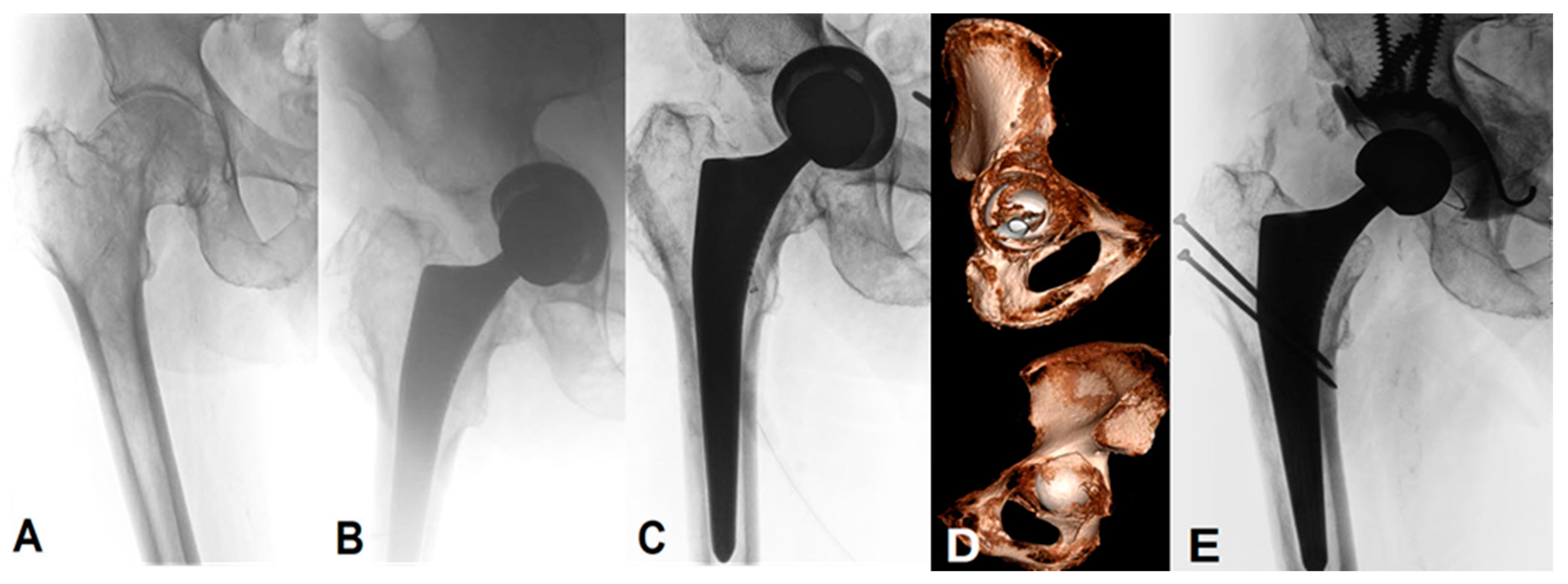
2.3. Surgical Procedure
2.4. Statistical Analysis
3. Results
3.1. Clinical Outcomes
3.2. Radiographic Outcomes
3.2.1. Cup Positioning directly after the primary THA
3.2.2. Cup Migration in the Follow-up
3.2.3. Fracture Healing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davidson, D.; Pike, J.; Garbuz, D.; Duncan, C.P.; Masri, B.A. Intraoperative periprosthetic fractures during total hip arthroplasty. Evaluation and management. J. Bone Jt. Surg. Am. 2008, 90, 2000–2012. [Google Scholar] [CrossRef] [PubMed]
- Charnley, J. Total hip replacement by low-friction arthroplasty. Clin. Orthop. Relat. Res. 1970, 72, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.E. Total hip prostheses. Clin. Orthop. Relat. Res. 1970, 72, 46–68. [Google Scholar] [PubMed]
- Mandelli, F.; Tiziani, S.; Schmitt, J.; Werner, C.M.L.; Simmen, H.P.; Osterhoff, G. Medial acetabular wall breach in total hip arthroplasty—Is full-weight-bearing possible? Orthop. Traumatol. Surg. Res. 2018, 104, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Yun, H.H.; Cheon, S.H.; Im, J.T.; Koh, Y.Y. Periprosthetic occult acetabular fracture: An unknown side effect of press-fit techniques in primary cementless total hip arthroplasty. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 1411–1419. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, P.F.; Hozack, W.J.; Callaghan, J.J.; Kim, Y.S.; Berry, D.J.; Hanssen, A.D.; LeWallen, D.G. Acetabular fracture associated with cementless acetabular component insertion: A report of 13 cases. J. Arthroplast. 1999, 14, 426–431. [Google Scholar] [CrossRef]
- Haidukewych, G.J.; Jacofsky, D.J.; Hanssen, A.D.; Lewallen, D.G. Intraoperative fractures of the acetabulum during primary total hip arthroplasty. J. Bone Jt. Surg. Am. 2006, 88, 1952–1956. [Google Scholar]
- Hasegawa, K.; Kabata, T.; Kajino, Y.; Inoue, D.; Tsuchiya, H. Periprosthetic Occult Fractures of the Acetabulum Occur Frequently During Primary THA. Clin. Orthop. Relat. Res. 2017, 475, 484–494. [Google Scholar] [CrossRef]
- Della Valle, C.J.; Momberger, N.G.; Paprosky, W.G. Periprosthetic fractures of the acetabulum associated with a total hip arthroplasty. Instr. Course Lect. 2003, 52, 281–290. [Google Scholar]
- Salvati, E.A.; Bullough, P.; Wilson, P.D., Jr. Intrapelvic protrusion of the acetabular component following total hip replacement. 1975. Clin. Orthop. Relat. Res. 2006, 453, 8–12. [Google Scholar] [CrossRef]
- Benazzo, F.; Formagnana, M.; Bargagliotti, M.; Perticarini, L. Periprosthetic acetabular fractures. Int. Orthop. 2015, 39, 1959–1963. [Google Scholar] [CrossRef] [PubMed]
- Acharya, M.; Elnahal, W.A. Strategies of management of traumatic periprosthetic acetabular fractures around a pre-existing total hip arthroplasty. J. Clin. Orthop. Trauma 2020, 11, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Pascarella, R.; Sangiovanni, P.; Cerbasi, S.; Fantasia, R.; Consonni, O.; Zottola, V.; Panella, A.; Moretti, B. Periprosthetic acetabular fractures: A New classification proposal. Injury 2018, 49 (Suppl. 3), S65–S73. [Google Scholar] [CrossRef] [PubMed]
- Simon, P.; von Roth, P.; Perka, C. Treatment algorithm of acetabular periprosthetic fractures. Int. Orthop. 2015, 39, 1995–2003. [Google Scholar] [CrossRef]
- Gibon, E.; Kerboull, L.; Courpied, J.P.; Hamadouche, M. Acetabular reinforcement rings associated with allograft for severe acetabular defects. Int. Orthop. 2019, 43, 561–571. [Google Scholar] [CrossRef]
- Hourscht, C.; Abdelnasser, M.K.; Ahmad, S.S.; Kraler, L.; Keel, M.J.; Siebenrock, K.A.; Klenke, F.M. Reconstruction of AAOS type III and IV acetabular defects with the Ganz reinforcement ring: High failure in pelvic discontinuity. Arch. Orthop. Trauma Surg. 2017, 137, 1139–1148. [Google Scholar] [CrossRef]
- Yeung, Y.; Chiu, K.Y.; Yau, W.P.; Tang, W.M.; Cheung, W.Y.; Ng, T.P. Assessment of the proximal femoral morphology using plain radiograph-can it predict the bone quality? J. Arthroplast. 2006, 21, 508–513. [Google Scholar] [CrossRef]
- Sink, E.L.; Leunig, M.; Zaltz, I.; Gilbert, J.C.; Clohisy, J. Reliability of a complication classification system for orthopaedic surgery. Clin. Orthop. Relat. Res. 2012, 470, 2220–2226. [Google Scholar] [CrossRef]
- Grevenstein, D.; Vidovic, B.; Baltin, C.; Eysel, P.; Spies, C.K.; Unglaub, F.; Oppermann, J. The Proximal Femoral Bone Geometry in Plain Radiographs. Arch. Bone Jt. Surg. 2020, 8, 675–681. [Google Scholar]
- Tannast, M.; Hanke, M.S.; Zheng, G.; Steppacher, S.D.; Siebenrock, K.A. What are the radiographic reference values for acetabular under- and overcoverage? Clin. Orthop. Relat. Res. 2015, 473, 1234–1246. [Google Scholar] [CrossRef]
- D’Antonio, J.A.; Capello, W.N.; Borden, L.S.; Bargar, W.L.; Bierbaum, B.F.; Boettcher, W.G.; Steinberg, M.E.; Stulberg, S.D.; Wedge, J.H. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin. Orthop. Relat. Res. 1989, 243, 126–137. [Google Scholar] [CrossRef]
- Letournel, E. Acetabulum Fractures: Classification and Management. J. Orthop. Trauma 2019, 33 (Suppl. 2), S1–S2. [Google Scholar] [CrossRef] [PubMed]
- Meermans, G.; Van Doorn, J.; Kats, J.-J. Restoration of the centre of rotation in primary total hip arthroplasty. Bone Jt. J. 2016, 98-B, 1597–1603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukushi, J.I.; Kawano, I.; Motomura, G.; Hamai, S.; Kawaguchi, K.I.; Nakashima, Y. Does hip center location affect the recovery of abductor moment after total hip arthroplasty? Orthop. Traumatol. Surg. Res. 2018, 104, 1149–1153. [Google Scholar] [CrossRef]
- Park, Y.S.; Shin, W.C.; Lee, S.M.; Kwak, S.H.; Bae, J.Y.; Suh, K.T. The best method for evaluating anteversion of the acetabular component after total hip arthroplasty on plain radiographs. J. Orthop. Surg. Res. 2018, 13, 66. [Google Scholar] [CrossRef] [PubMed]
- Mou, P.; Liao, K.; Chen, H.L.; Yang, J. Controlled fracture of the medial wall versus structural autograft with bulk femoral head to increase cup coverage by host bone for total hip arthroplasty in osteoarthritis secondary to developmental dysplasia of the hip: A retrospective cohort study. J. Orthop. Surg. Res. 2020, 15, 561. [Google Scholar] [CrossRef]
- Zha, G.C.; Sun, J.Y.; Guo, K.J.; Zhao, F.C.; Pang, Y.; Zheng, X. Medial Protrusio Technique in Cementless Total Hip Arthroplasty for Developmental Dysplasia of the Hip: A Prospective 6- to 9-Year Follow-up of 43 Consecutive Patients. J. Arthroplast. 2016, 31, 1761–1766. [Google Scholar] [CrossRef]
- Berry, D.J.; Lewallen, D.G.; Hanssen, A.D.; Cabanela, M.E. Pelvic discontinuity in revision total hip arthroplasty. J. Bone Jt. Surg. Am. 1999, 81, 1692–1702. [Google Scholar] [CrossRef]
- Leunig, M.; Nho, S.J.; Turchetto, L.; Ganz, R. Protrusio acetabuli: New insights and experience with joint preservation. Clin. Orthop. Relat. Res. 2009, 467, 2241–2250. [Google Scholar] [CrossRef]
- Gerber, A.; Pisan, M.; Zurakowski, D.; Isler, B. Ganz reinforcement ring for reconstruction of acetabular defects in revision total hip arthroplasty. J. Bone Jt. Surg. Am. 2003, 85, 2358–2364. [Google Scholar] [CrossRef]
- Takigami, I.; Ito, Y.; Mizoguchi, T.; Shimizu, K. Pelvic Discontinuity Caused by Acetabular Overreaming during Primary Total Hip Arthroplasty. Case Rep. Orthop. 2011, 2011, 939202. [Google Scholar] [CrossRef]
- Desai, G.; Ries, M.D. Early postoperative acetabular discontinuity after total hip arthroplasty. J. Arthroplast. 2011, 26, 1517.e17–1517.e19. [Google Scholar] [CrossRef] [PubMed]
- Dorr, L.D.; Tawakkol, S.; Moorthy, M.; Long, W.; Wan, Z. Medial protrusio technique for placement of a porous-coated, hemispherical acetabular component without cement in a total hip arthroplasty in patients who have acetabular dysplasia. J. Bone Jt. Surg Am. 1999, 81, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.L.; Nam, K.W.; Yoo, J.J.; Kim, Y.M.; Kim, H.J. Cotyloplasty in cementless total hip arthroplasty for an insufficient acetabulum. Clin. Orthop. Surg. 2010, 2, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Miles, A.W.; McNamee, P.B. Strain gauge and photoelastic evaluation of the load transfer in the pelvis in total hip replacement: The effect of the position of the axis of rotation. Proc. Inst. Mech. Eng. H 1989, 203, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Hedley, A.K.; Kabo, M.; Kim, W.; Coster, I.; Amstutz, H.C. Bony ingrowth fixation of newly designed acetabular components in a canine model. Clin. Orthop. Relat. Res. 1983, 176, 12–23. [Google Scholar] [CrossRef]
- Margalit, K.A.; Hayashi, K.; Jackson, J.; Kim, S.Y.; Garcia, T.C.; Wiggans, K.T.; Aiken, S.; Stover, S.M. Biomechanical evaluation of acetabular cup implantation in cementless total hip arthroplasty. Vet. Surg. 2010, 39, 818–823. [Google Scholar] [CrossRef]
- Kunze, K.N.; Bovonratwet, P.; Polce, E.M.; Paul, K.; Sculco, P.K. Comparison of Surgical Time, Short-term Adverse Events, and Implant Placement Accuracy Between Manual, Robotic-assisted, and Computer-navigated Total Hip Arthroplasty: A Network Meta-analysis of Randomized Controlled Trials. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2022, 6, e21.00200. [Google Scholar] [CrossRef]
- Migliorini, F.; Cuozzo, F.; Oliva, F.; Eschweiler, J.; Hildebrand, F.; Maffulli, N. Imageless navigation for primary total hip arthroplasty: A meta-analysis study. J. Orthop. Traumatol. 2022, 23, 21. [Google Scholar] [CrossRef]
- SIRIS. Swiss National Hip & Knee Joint Registry—Report: 2020 Annual Report of the SIRIS Registry Hip & Knee, 2012–2019; SIRIS: Thun, Switzerland, 2020; Volume 3604. [Google Scholar]
- Mears, D.C. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J. Am. Acad. Orthop. Surg. 1999, 7, 128–141. [Google Scholar] [CrossRef]
| No. | Age | Gender | BMI (kg/m2) | Coxa Profunda | CBR-Index | Fracture IS | Follow-up (m) | Fracture Type AAOS | AC Involvement | PC Involvement |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 80 | f | 33 | + | 0.52 | - | 8 | IIA | - | - |
| 2 | 86 | m | 26 | - | 0.47 | - | 12 | III | + | - |
| 3 | 84 | f | 19 | + | 0.53 | - | 8 | III | - | + |
| 4 | 82 | m | 25 | + | 0.43 | - | 7 | IIB | - | - |
| 5 | 78 | f | 23 | + | 0.49 | - | 63 | III | + | - |
| 6 | 62 | m | 28 | - | 0.51 | + | 6 | IIB | - | - |
| 7 | 60 | m | 24 | + | 0.43 | + | 37 | IV | + | + |
| No. | Ilioischial Overlap (mm) | Length of Overlap (mm) | Iliopectineal Distance (mm) | Rate of Medial Protrusion (%) | ΔH-COR (mm) | ΔV-COR (mm) | Inclination (°) | Anteversion (°) |
|---|---|---|---|---|---|---|---|---|
| 1 | 14.0 | 51.4 | −3.0 | 65 | 17 | 7 | 55 | 16 |
| 2 | 5.3 | 37.9 | 0.0 | 40 | 26 | 4 | 42 | 45 |
| 3 | 3.5 | 26.8 | −1.0 | 27 | 17 | 7 | 25 | 26 |
| 4 | 19.8 | 56.1 | −10.5 | 70 | 35 | 10 | 45 | 13 |
| 5 | 6.1 | 35.5 | −2.1 | 50 | 21 | 0 | 53 | 27 |
| 6 | 10.0 | 41.3 | −3.4 | 46 | 16 | 16 | 28 | 13 |
| 7 | 18.6 | 52.6 | −3.5 | 56 | 8 | 10 | 38 | 15 |
| Parameter | PI | PR | p-Value (PI vs. PR) | FU | ΔFU-PR | p-Value (PR vs. FU) |
|---|---|---|---|---|---|---|
| Iliopectineal distance (mm) | −3.36 ± 3.15 (−10.5–0) | 11 ± 7.2 (1.6–24) | 0.015 | 13.3 ± 6.4 (7–25) | 1.6 ± 2.2 (0–6) | 0.062 |
| ΔH-COR (mm) | 20.0 ± 7.9 (8–35) | 9.9 ± 5.2 (1–17) | 0.015 | 10.9 ± 4.6 (6–20) | 1 ± 5.7 (−8–7) | 0.333 |
| ΔV-COR (mm) | 7.7 ± 4.7 (0–16) | 5.7 ± 3.7 (1–11) | 0.468 | 5 ± 3.5 (0–10) | −0.7 ± 2.5 (−5–3) | 0.271 |
| Inclination (°) | 40.9 ± 10.6 (25–55) | 41.6 ± 6.6 (31–54) | 0.937 | 42.3 ± 7.3 (33–55) | 0.7 ± 2.5 (−2–6) | 0.312 |
| Anteversion (°) | 22.1 ± 10.8 (13–45) | 16.7 ± 7.5 (9–32) | 0.234 | 15.0 ± 7.0 (4–27) | −1.7 ± 4.5 (−10–4) | 0.109 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ivanova, S.; Vuillemin, N.; Hapa, O.; Siebenrock, K.A.; Keel, M.J.B.; Tosounidis, T.H.; Bastian, J.D. Revision of a Failed Primary Total Hip Arthroplasty following Excessive Reaming with a Medial Cup Protrusion. Medicina 2022, 58, 1254. https://doi.org/10.3390/medicina58091254
Ivanova S, Vuillemin N, Hapa O, Siebenrock KA, Keel MJB, Tosounidis TH, Bastian JD. Revision of a Failed Primary Total Hip Arthroplasty following Excessive Reaming with a Medial Cup Protrusion. Medicina. 2022; 58(9):1254. https://doi.org/10.3390/medicina58091254
Chicago/Turabian StyleIvanova, Silviya, Nicolas Vuillemin, Onur Hapa, Klaus A. Siebenrock, Marius J. B. Keel, Theodoros H. Tosounidis, and Johannes D. Bastian. 2022. "Revision of a Failed Primary Total Hip Arthroplasty following Excessive Reaming with a Medial Cup Protrusion" Medicina 58, no. 9: 1254. https://doi.org/10.3390/medicina58091254
APA StyleIvanova, S., Vuillemin, N., Hapa, O., Siebenrock, K. A., Keel, M. J. B., Tosounidis, T. H., & Bastian, J. D. (2022). Revision of a Failed Primary Total Hip Arthroplasty following Excessive Reaming with a Medial Cup Protrusion. Medicina, 58(9), 1254. https://doi.org/10.3390/medicina58091254








