Development of the Interstitial Cystitis Self-Help and Medical Resources Scale (ICSR) for Women with Interstitial Cystitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Setting
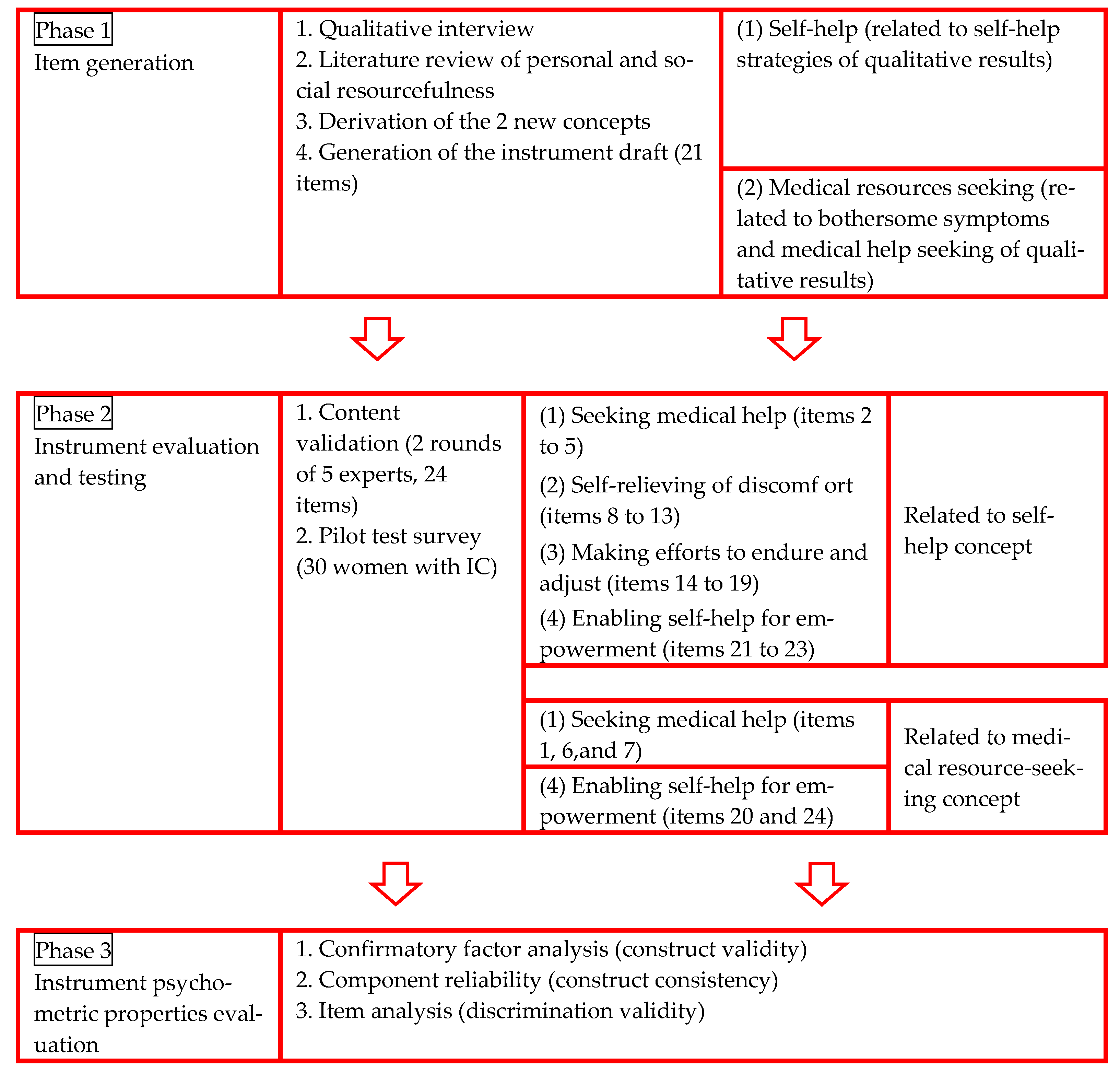
2.2. Instrument Development
- Qualitative interview: We assessed the self-perception of symptoms, medical-help-seeking behaviors, and self-help strategies for women with IC. We recruited 68 women with IC, 98.5% of whom did not have ulcerative IC (Hunner’s lesions), and about 72.1% of the patients indicated that their symptoms interfered with their daily activities. The interview guide was developed based on a literature review of resourcefulness concepts, and a 1-to-1 interview format was adopted to collect the data. Three important themes were identified in the interviews: (1) bothersome symptoms—all-day bladder pain, lower urinary tract symptoms, and deteriorated quality of life; (2) medical-help-seeking—exhaustion and frustration; and (3) self-help strategies—coexisting with IC or feeling helpless [3].
- Literature review of the concepts: findings from a literature review led to the proposal of 2 concepts, namely, personal resourcefulness and social resourcefulness.
- Derivation of 2 new concepts: Based on the qualitative inquiry results and the literature review, we derived 2 new concepts: self-help, which indicated the ability to adapt self-control skills to cope with their disease, and seeking medical resources, which illustrated the ability to use medical resources to cope with the disease. The bothersome symptoms and medical-help-seeking themes were related to the concept of medical resources seeking, and the self-help strategies theme was related to the concept of self-help.
- Generation of the instrument draft: the first version of the scale was drafted, which comprised 21 questions, including 19 closed questions and 2 open questions.
- Content validation: Two rounds of 5 expert panels were conducted, and as a result, 3 statements were added. These statements were (1) “when I have urinary discomfort, I will seek medical help immediately”; (2) “when I have urinary discomfort, I will seek complementary and alternative medicine immediately, including folk medicine, pray to the gods, and seek to ascertain by divination”; and (3) “when I feel urinary discomfort and pain, I try to take dietary supplementation suggestions from others or by searching the internet, including dried longan, red dates, or ginger tea.” Therefore, after 2 rounds of expert panels, the revised version of the ICSR included 24 questions: 22 closed questions and 2 open questions. The 4 constructs and their items were defined as follows: (1) seeking medical help (items 1 to 7), (2) self-relieving of discomfort (items 8 to 13), (3) making efforts to endure and adjust (items 14 to 19), and (4) enabling self-help for empowerment (items 20 to 24). The 4 constructs of the ICSR related to the second phase and the 2 newly derived concepts of our study were as follows: (1) seeking medical help (items 2 to 5), self-relieving of discomfort (items 8 to 13), making efforts to endure and adjust (items 14 to 19), and enabling self-help for empowerment (items 21 to 23) were related to the concept of self-help; (2) seeking medical help (items 1, 6, and 7) and enabling self-help for empowerment (items 20 and 24) were related to the concept of medical-resource-seeking. Experts used the item-level content validity index (I-CVI) to judge each item as relevant or clear, the scale-level content validity index (S-CVI) to judge each construct as relevant or clear, and the S-CVI average (S-CVI/Ave) to judge the overall scale as relevant or clear [15,16,17]. The I-CVI, S-CVI, and S-CVI/Ave were all 1.00, which illustrated that the overall scale was relevant and clear.
- Pilot test survey: A pilot study of 30 women with IC was conducted to evaluate the participants’ understanding of each item. Overall, the women indicated that each item was clear [15].
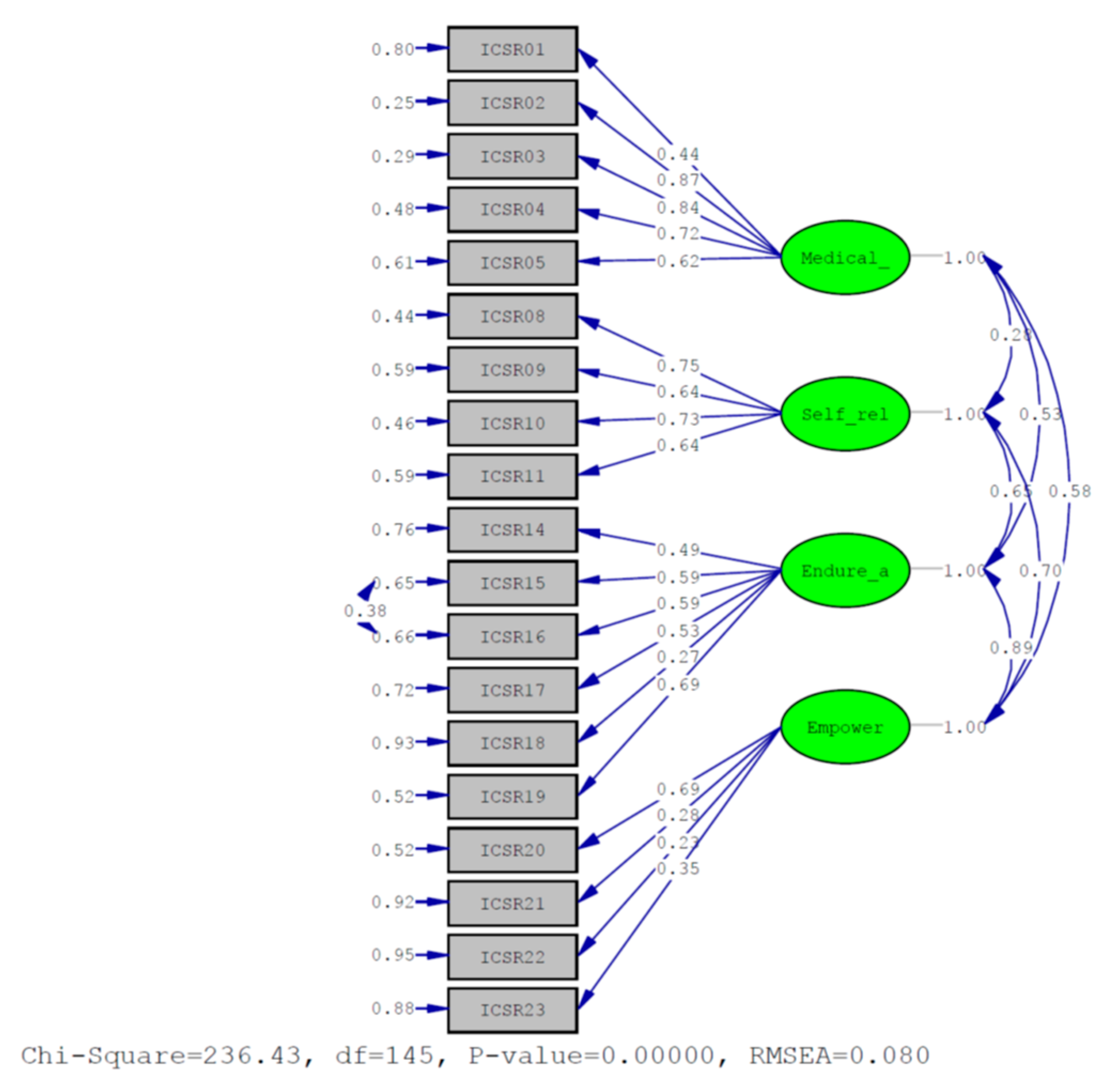
- CFA was used to examine how the item scores from the participants’ responses resulted in goodness-of-fit measures of the factor structure, which indicated good construct validity [18].
- Component reliability (CR) was used to assess the internal consistency of the participants’ responses for each construct, which was measured using Cronbach’s α, so that unreliable items could be adjusted or removed if necessary [18].
- Comparisons of extreme groups of item analysis were used to assess the differences between the participants in the high-scoring group and the low-scoring group, which indicated good discrimination validity [18].
2.3. Data Analysis
3. Results
3.1. Demographics
3.2. Validity and Reliability
3.2.1. Content Validity
3.2.2. Construct Validity
3.2.3. Construct Reliability
3.2.4. Discrimination Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Constructs and Items | Strongly Disagreed | Disagreed | Agreed | Strongly Agreed |
| A.Seeking medical help | ||||
| 1. If I do not feel better regarding my urinary problems, I will transfer to another hospital or physician for examination. | □ | □ | □ | □ |
| 2. I worry about drug addiction after taking medicine. | □ | □ | □ | □ |
| 3.I worry about adverse effects after taking medicine. | □ | □ | □ | □ |
| 4. I am afraid that when I discontinue my medicine, I will experiencerecurrence of my urinary problem. | □ | □ | □ | □ |
| 5. I feel inconvenienced by taking medicine when I go out, and I feel it disturbs my emotions. | □ | □ | □ | □ |
| B. Self-relieving of discomforts | ||||
| 6. I found that when I pay attention to a task, the feeling of pain or discomfort is relieved. | □ | □ | □ | □ |
| 7. I found that when I am doing some activities, including walking, jogging, riding a bicycle, or yoga, the feeling of pain or discomfort is relieved. | □ | □ | □ | □ |
| 8. I found that when I message my abdomen, the feeling of pain or discomfort is relieved. | □ | □ | □ | □ |
| 9. I found that when I lie in bed, the feeling of pain or discomfort is relieved. | □ | □ | □ | □ |
| C. Making efforts to endure and adjust | ||||
| 10. I will choose a job that offers a replacement orsubstitute, including packer, restaurant server, office work, or store staff, to cope with my frequent urination. | □ | □ | □ | □ |
| 11. When I go out, I choose to go to the restroom conveniently to cope with my frequent urinary discomfort. | □ | □ | □ | □ |
| 12. when I travel a long time, I choose to take the useful utility of toilet, including take the metro, train, high speed rail | □ | □ | □ | □ |
| 13. I can tolerate diapers or sanitary napkins to cope with my frequent urination discomfort. | □ | □ | □ | □ |
| 14. I will drink more water or soup in the daytime to cope with my urinary problem. | □ | □ | □ | □ |
| 15. I will endure the inconvenience of going to the restroom frequently to cope with my frequent urination. | □ | □ | □ | □ |
| D. Enabling self-help for empowerment | ||||
| 16. I will follow the advice of healthcare providers to resolve my urinary problems. | □ | □ | □ | □ |
| 17. I will try to not hold my urine for a long time when I have a lot of work to do and need the toilet badly. | □ | □ | □ | □ |
| 18. I will not eat food that can stimulate the bladder, including caffeine, tea, alcohol, chocolate, spice, or cranberry, to cope with urinary discomfort. | □ | □ | □ | □ |
| 19. I will try to do something for relief or to make me happy, including watch a movie, take a bath, sign a song, or listen to music, when I feel pain or discomfort from my urinary problem. | □ | □ | □ | □ |
References
- Malde, S.; Palmisani, S.; Al-Kaisy, A.; Sahai, A. Guideline of guidelines: Bladder pain syndrome. BJU Int. 2018, 122, 729–743. [Google Scholar] [CrossRef] [PubMed]
- Rahnama’I, M.S.; Javan, A.; Vyas, N.; Lovasz, S.; Singh, N.; Cervigni, M.; Pandey, S.; Wyndaele, J.J.; Taneja, R. Bladder pain syndrome and interstitial cystitis beyond horizon: Reports from the global interstitial cystitis/bladder pain society (GIBS) meeting 2019 Mumbai-India. Anesth. Pain Med. 2020, 10, e101848–e101856. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.C.; Liu, C.Y.; Liao, C.Y.; Tsao, L.I. Self-perception of symptoms, medical help seeking, and self-help strategies of women with interstitial cystitis/painful bladder syndrome. Low. Urin. Tract Symptoms 2020, 12, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, M. A schedule for assessing self-control behaviors: Preliminary findings. Behav. Ther. 1980, 11, 109–121. [Google Scholar] [CrossRef]
- Braden, C.J. A test of self-help model: Learned response to chronic illness experience. Nurs. Res. 1990, 39, 42–44. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, M. Role of learned resourcefulness in self-control of health behavior. In Learned Resourcefulness: On Coping Skills, Self-Control, and Adaptive Behavior, 1st ed.; Rosenbaum, M., Ed.; Springer Publishing Company: New York, NY, USA, 1990; Volume 1, pp. 3–25. [Google Scholar]
- Nadler, A. Help-seeking behavior as a coping resource. In Learned Resourcefulness: On Coping Skills, Self-Control, and Adaptive Behavior, 1st ed.; Rosenbaum, M., Ed.; Springer Publishing Company: New York, NY, USA, 1990; Volume 1, pp. 127–164. [Google Scholar]
- Zauszniewski, J.A. Learned resourcefulness: A conceptual analysis. Issues Ment. Health Nurs. 1995, 16, 13–31. [Google Scholar] [CrossRef] [PubMed]
- Zauszniewski, J.A.; Lai, C.Y.; Tithiphontumrong, S. Development and testing of the resourcefulness scale for older adults. Nurs. Meas. 2006, 14, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Kanter, G.; Volpe, K.A.; Dunivan, G.C.; Cichowski, S.B.; Jeppson, P.C.; Rogers, R.G.; Komesu, Y.M. Important role of physicians in addressing psychological aspects of interstitial cystitis/bladder pain syndrome (IC/BPS): A qualitative analysis. Int. Urogynecol. J. 2017, 28, 249–256. [Google Scholar] [CrossRef]
- Kirkham, A.; Swainston, K. Women’s experiences of interstitial cystitis/painful bladder syndrome. West. J. Nurs. Res. 2022, 44, 125–132. [Google Scholar] [CrossRef] [PubMed]
- McKernan, L.C.; Walsh, C.G.; Reynolds, W.S.; Crofford, L.J.; Dmochowski, R.R.; Williams, D.A. Psychosocial co-morbidities in interstitial cystitis/bladder pain syndrome (IC/BPS): A systematic review. Neurourol. Urodyn. 2017, 37, 926–941. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare. Statistics of Inpatients and Outpatients. Available online: https://dep.mohw.gov.tw/DOS/lp-1922-113.html (accessed on 3 September 2019).
- Anderson, J.C.; Gerbing, D.W. Structure equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Waltz, C.F.; Strickland, O.L.; Lenz, E.R. Measurement in Nursing and Health Research, 5th ed.; Springer Publishing company: New York, NY, USA, 2016; pp. 91–393. [Google Scholar]
- Yusoff, M.S.B. ABC of content validation and content validity index calculation. EIMJ 2019, 11, 49–54. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T.; Owen, S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S. Applied Multivariate Techniques; John Wiley & Sons: New York, NY, USA, 1996; pp. 144–181. [Google Scholar]
- Bagozzi, R.P.; Yi, Y. On the evaluation of structural equation models Academic of structural equation models. Acad. Mark. Sci. 1988, 16, 76–94. [Google Scholar]
| Variable | n (%) | Median (Min 1–Max 2) | Mean ± SD 3 |
|---|---|---|---|
| Age (years) | 61.50 (21.00–73.00) | 55.56 ± 13.92 | |
| Self-perceived bothersome IC 4 symptoms (years) | 2.00 (0.50–10.00) | 3.24 ± 3.19 | |
| Married status | |||
| Unmarried | 11 (11.0) | ||
| Married | 80 (80.0) | ||
| Divorced and widowed | 9 (9.0) | ||
| Education | |||
| Under senior high school | 53 (53.0) | ||
| Associate degree | 16 (16.0) | ||
| College or university or above | 31 (31.0) | ||
| Religion | |||
| None | 49 (49.0) | ||
| Buddhism | 33 (33.0) | ||
| Taoism | 9 (9.0) | ||
| Christianity or Catholicism | 9 (9.0) | ||
| Occupation | |||
| Yes | 49 (49.0) | ||
| No | 51 (51.0) |
| Four-Factor Model | RMSEA 1 | PNFI 2 | SRMR 3 | GFI 4 | AGFI 5 | PGFI 6 |
|---|---|---|---|---|---|---|
| Score | 0.080 | 0.83 | 0.094 | 0.93 | 0.91 | 0.71 |
| Construct of ICSR | Number of Items | Component Reliability |
|---|---|---|
| Seeking medical help | 5 | 0.83 |
| Self-relieving of discomfort | 4 | 0.79 |
| Making efforts to endure and adjust | 6 | 0.75 |
| Enabling self-help for empowerment | 4 | 0.42 |
| Items | t-Value | p-Value |
|---|---|---|
| 1. If I do not feel better regarding my urinary problems, I will transfer to another hospital or physician for examination. | 2.943 | 0.005 |
| 2. I worry about drug addiction after taking medicine. | 5.877 | <0.001 |
| 3. I worry about adverse effects after taking medicine. | 6.009 | <0.001 |
| 4. I am afraid that when I discontinue my medication, I will experience recurrence of my urinary problem. | 4.501 | <0.001 |
| 5. I feel inconvenienced by taking medicine when I go out, and I feel it disturbs my emotions. | 5.039 | <0.001 |
| 8. I found that when I pay attention to a task, the feeling of pain or discomfort is relieved. | 6.899 | <0.001 |
| 9. I found that when I am doing some activities, including walking, jogging, riding a bicycle, or yoga, the feeling of pain or discomfort is relieved. | 5.049 | <0.001 |
| 10. I found that when I message my abdomen, the feeling of pain or discomfort is relieved. | 4.915 | <0.001 |
| 11. I found that when I lie in bed, the feeling of pain or discomfort is relieved. | 3.921 | <0.001 |
| 14. I will choose a job that offers a replacement or substitute, including packer, restaurant server, office work, or store staff, to cope with my frequent urination. | 4.948 | <0.001 |
| 15. when I go out, I choose to go to the restroom conveniently to cope with my frequent urinary discomfort. | 5.007 | <0.001 |
| 16. when I travel a long time, I choose to take the useful utility of toilet, including take the metro, train, high speed rail | 5.975 | <0.001 |
| 17. I can tolerate diapers or sanitary napkins to cope with my frequent urinary discomfort. | 4.633 | <0.001 |
| 18. I will drink more water or soup in the daytime to cope with my urinary problem. | 2.521 | 0.015 |
| 19. I will endure the inconvenience of going to the restroom frequently to cope with my frequent urination. | 6.488 | <0.001 |
| 20. I will follow the advise of healthcare providers to resolve my urinary problems. | 6.104 | <0.001 |
| 21. I will try to not hold my urine for a long time while I have a lot of work to do and I need the toilet badly. | 1.347 | 0.189 |
| 22. I will not eat food that can stimulate the bladder, including caffeine, tea, alcohol, chocolate, spicy, or cranberry, to cope with urinary discomfort. | 2.759 | 0.008 |
| 23. I will try to do something for relief or to make me happy, including watch a movie, take a bath, sign a song, or listen to music, when I feel pain or discomfort from my urinary problem. | 4.735 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, H.-C.; Tsao, L.-I.; Liao, C.-H.; Liu, C.-Y. Development of the Interstitial Cystitis Self-Help and Medical Resources Scale (ICSR) for Women with Interstitial Cystitis. Medicina 2022, 58, 1183. https://doi.org/10.3390/medicina58091183
Chen H-C, Tsao L-I, Liao C-H, Liu C-Y. Development of the Interstitial Cystitis Self-Help and Medical Resources Scale (ICSR) for Women with Interstitial Cystitis. Medicina. 2022; 58(9):1183. https://doi.org/10.3390/medicina58091183
Chicago/Turabian StyleChen, Hui-Chun, Lee-Ing Tsao, Chun-Hou Liao, and Chieh-Yu Liu. 2022. "Development of the Interstitial Cystitis Self-Help and Medical Resources Scale (ICSR) for Women with Interstitial Cystitis" Medicina 58, no. 9: 1183. https://doi.org/10.3390/medicina58091183
APA StyleChen, H.-C., Tsao, L.-I., Liao, C.-H., & Liu, C.-Y. (2022). Development of the Interstitial Cystitis Self-Help and Medical Resources Scale (ICSR) for Women with Interstitial Cystitis. Medicina, 58(9), 1183. https://doi.org/10.3390/medicina58091183





