Single Level Spondylolisthesis Associated Sagittal Plane Imbalance Corrected by Pre-Psoas Interbody Fusion Using Anterior Column Release with 30° Expandable Hyperlordotic Cage
Abstract
:1. Introduction
2. Report of Cases
2.1. Surgical Approach
2.2. ACR Cases Demographic and Pre-Operative Outcome
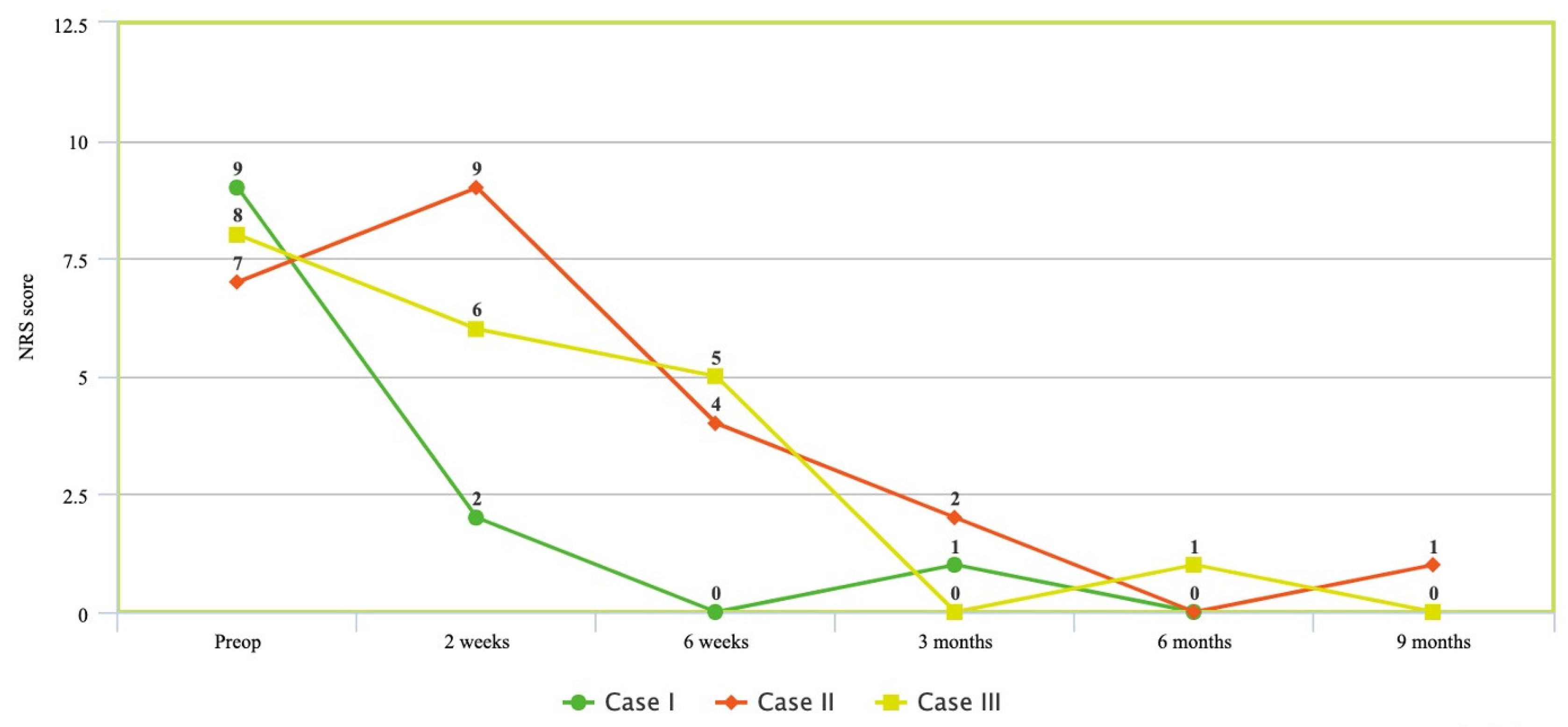
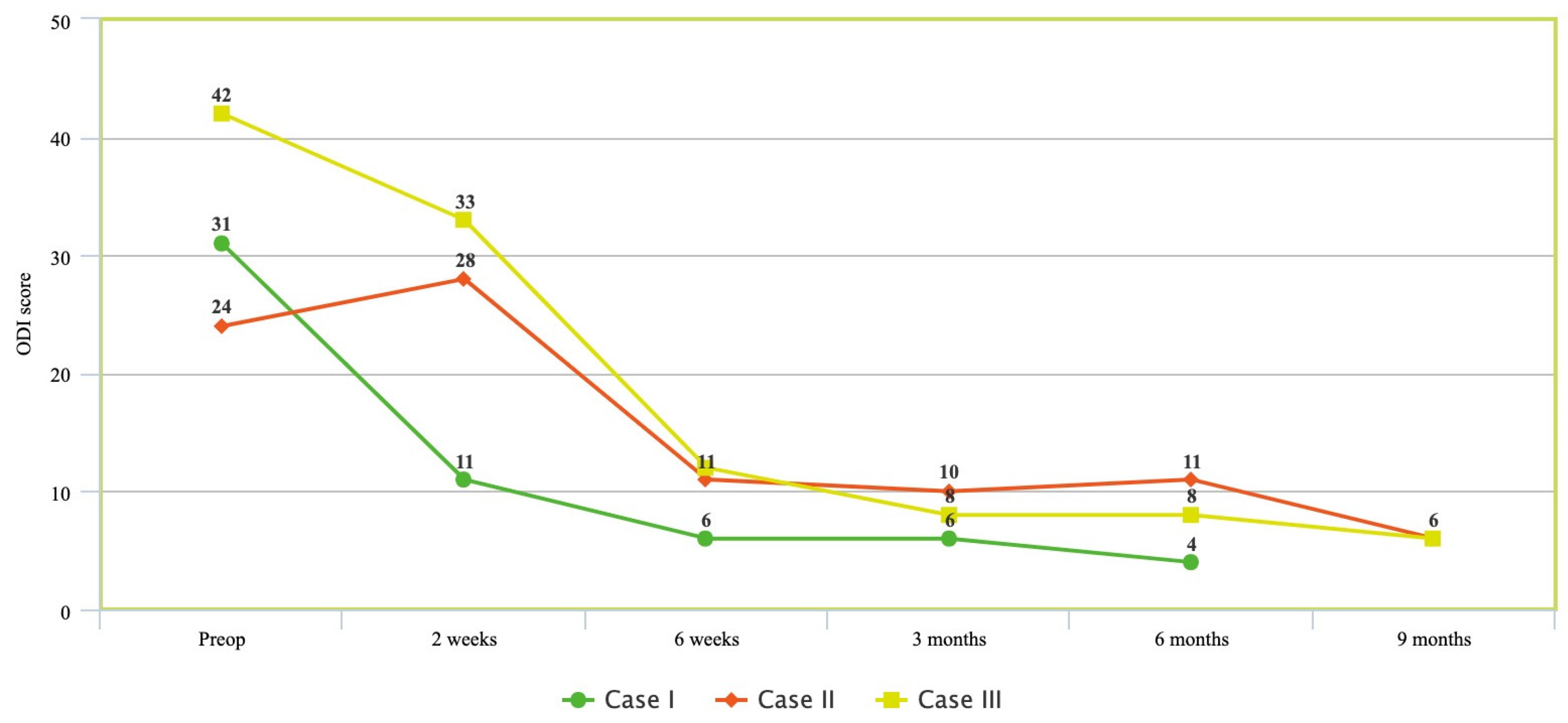
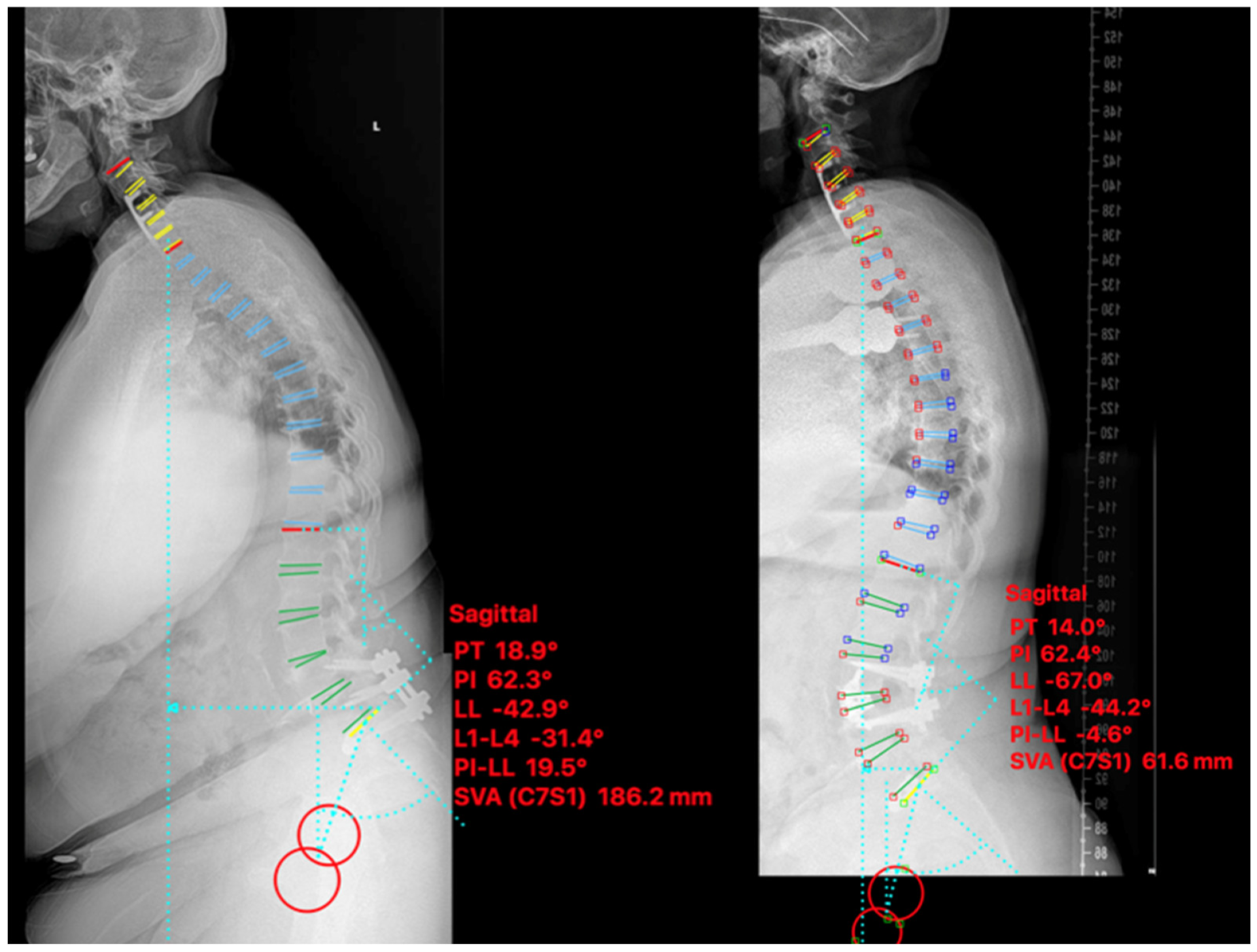
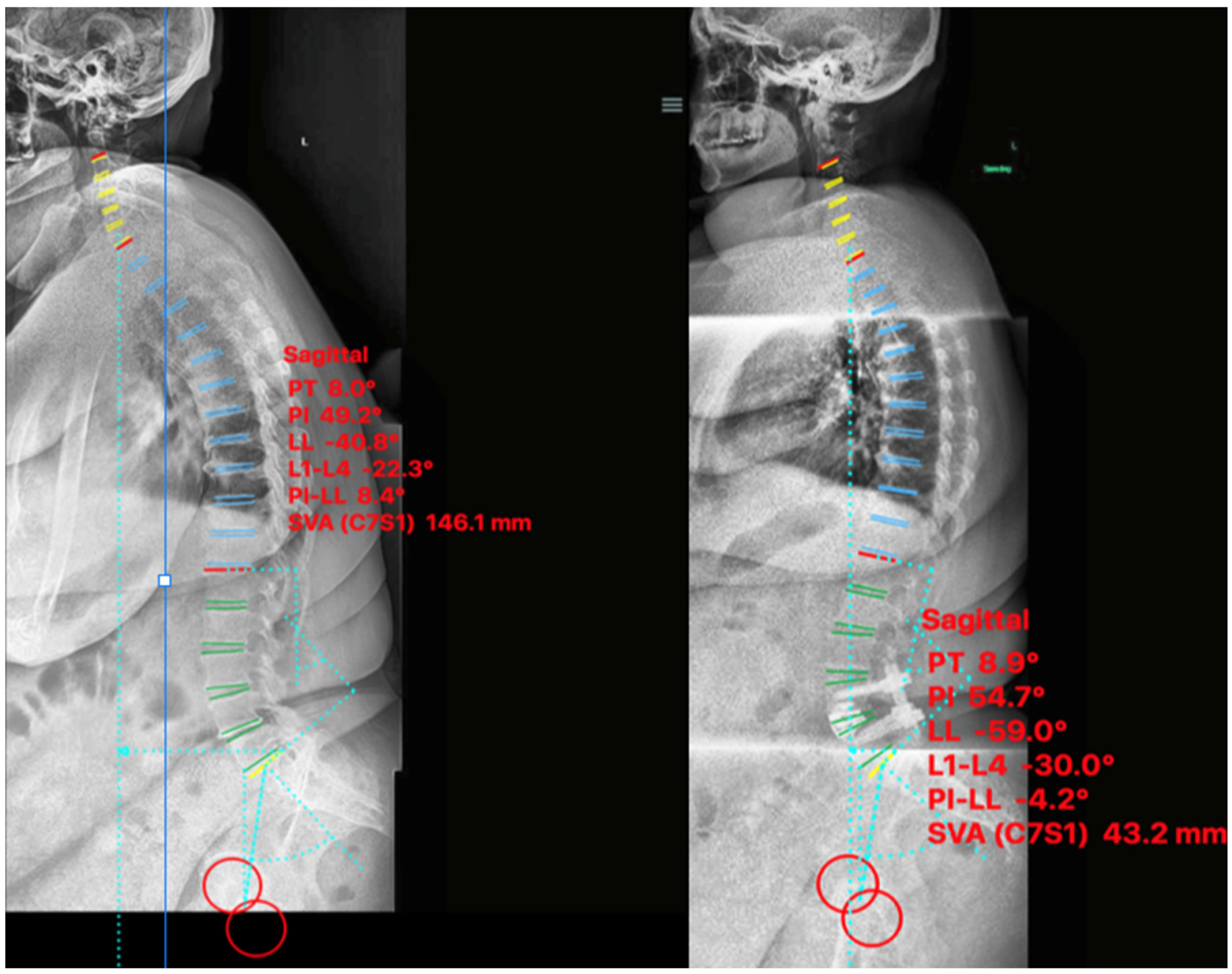
2.3. ACR Cases Functional and Radiographic Outcome
2.4. ACR Cases
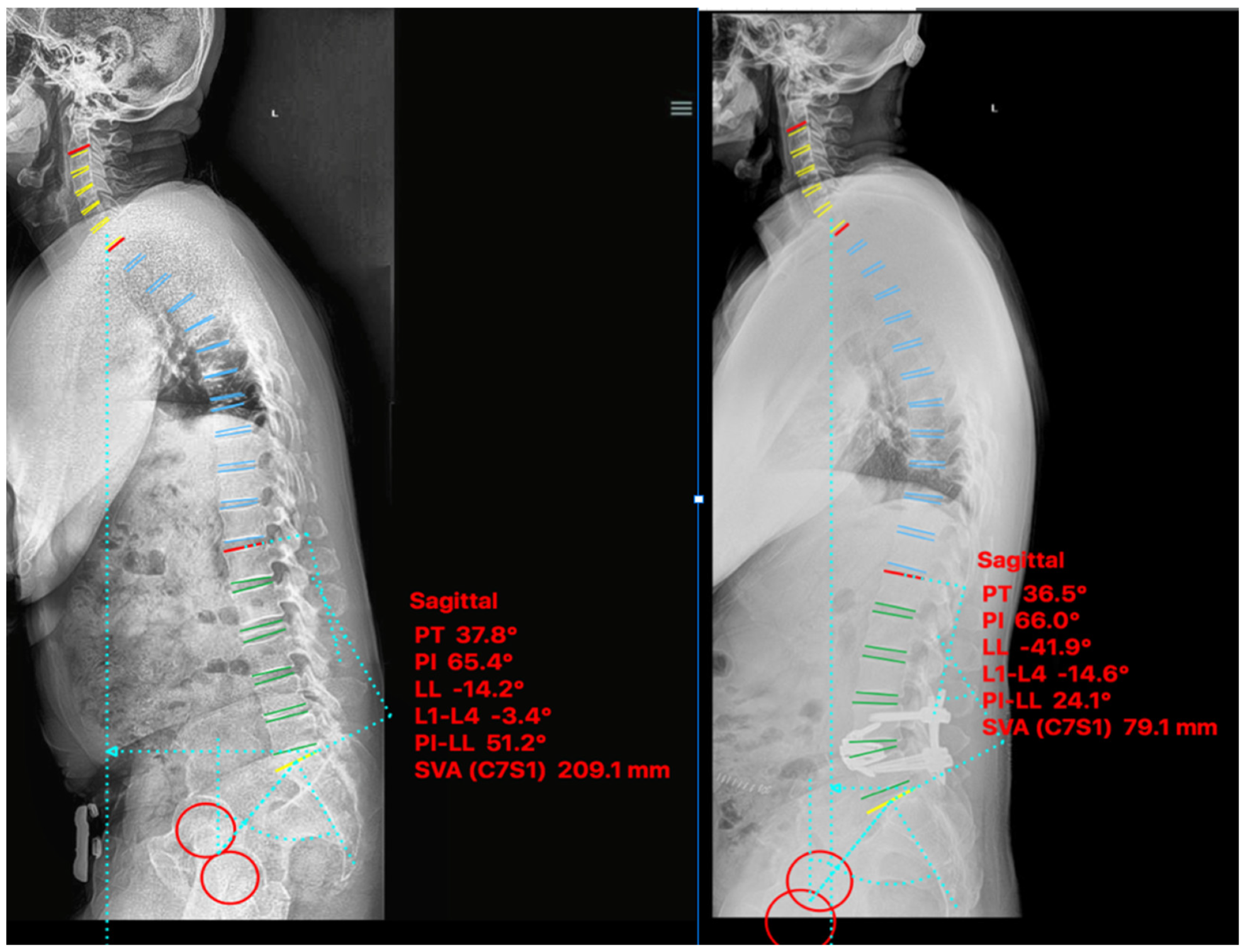
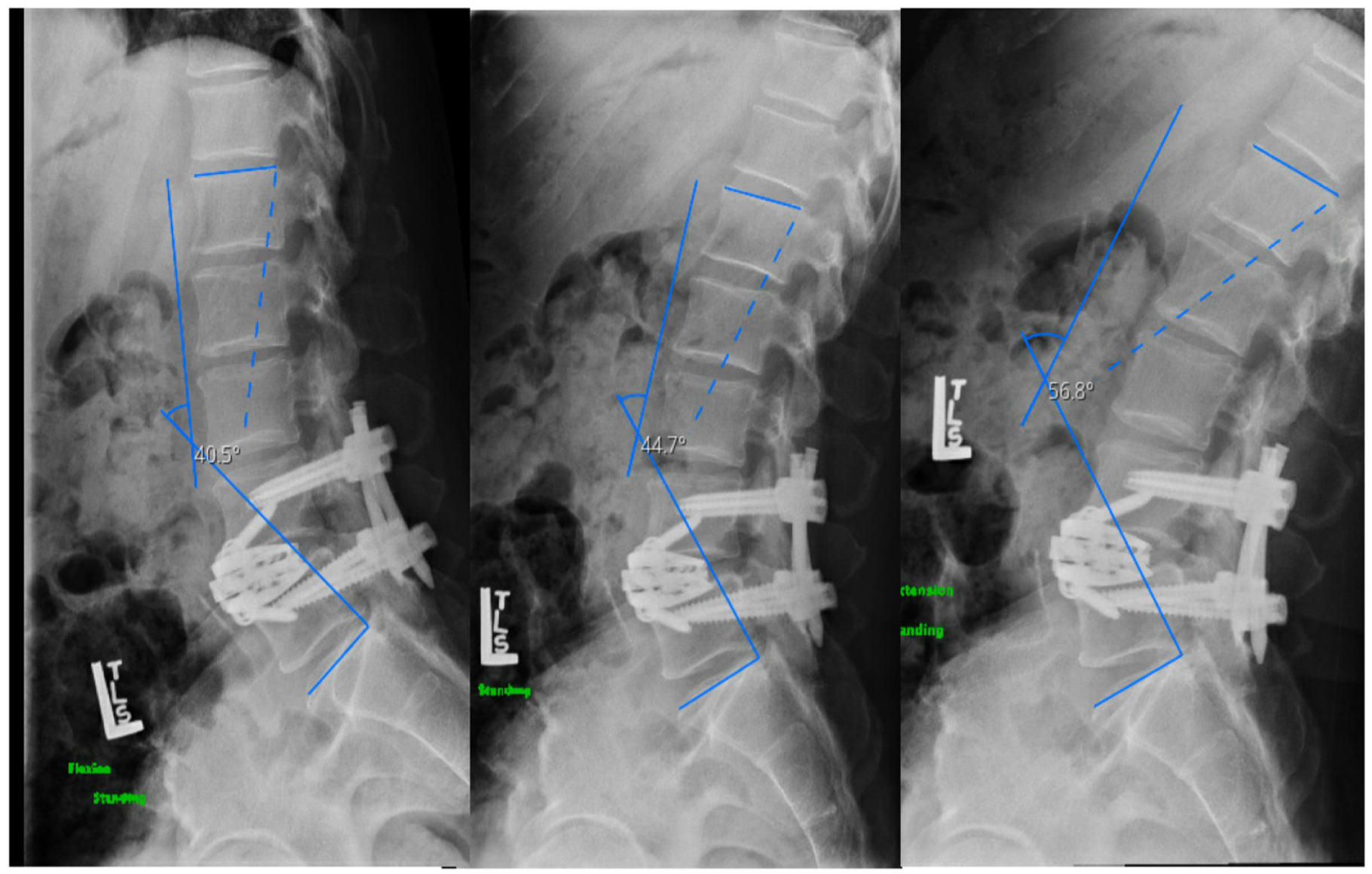
2.4.1. Case I
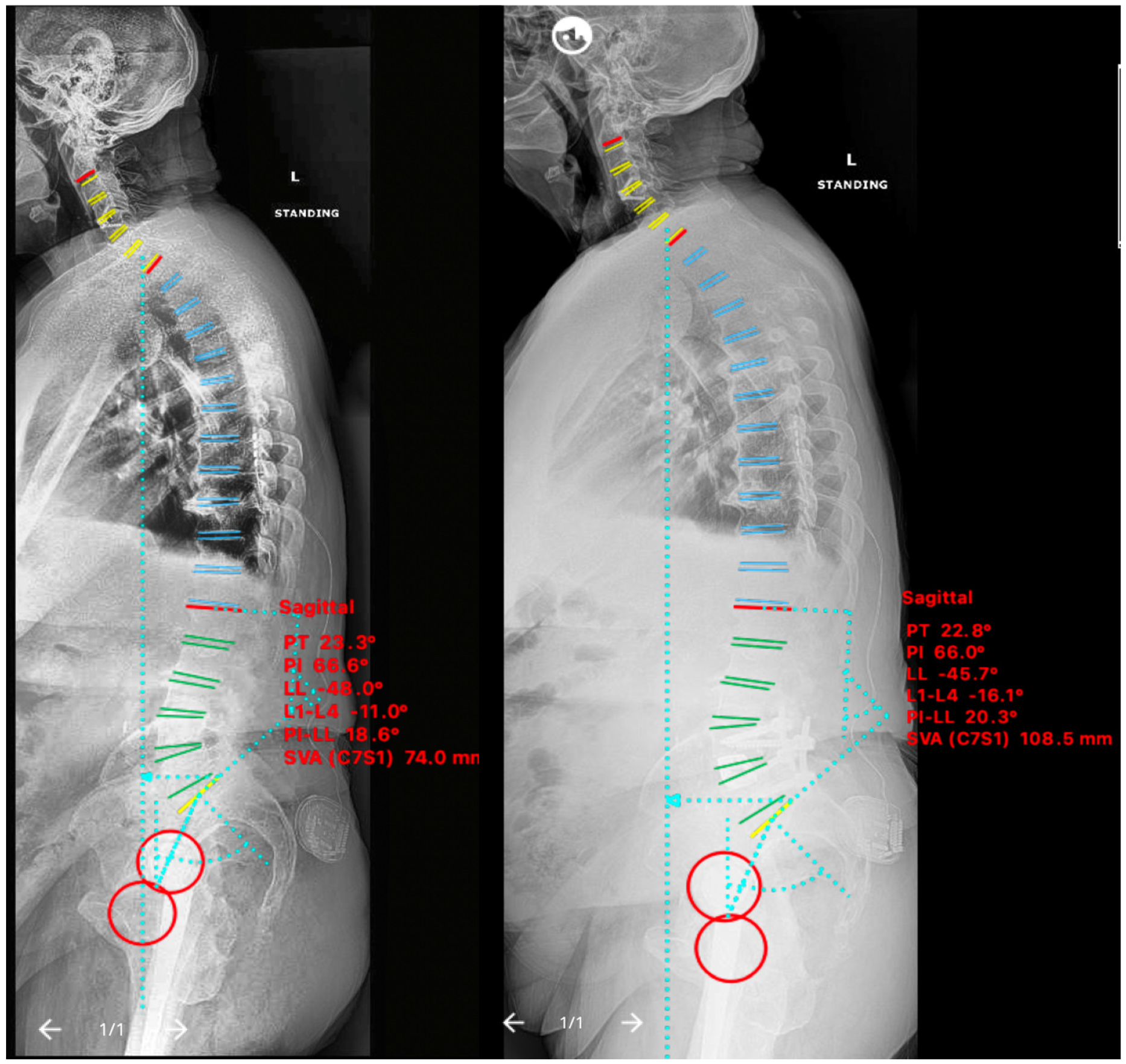
2.4.2. Case II
2.4.3. Case III
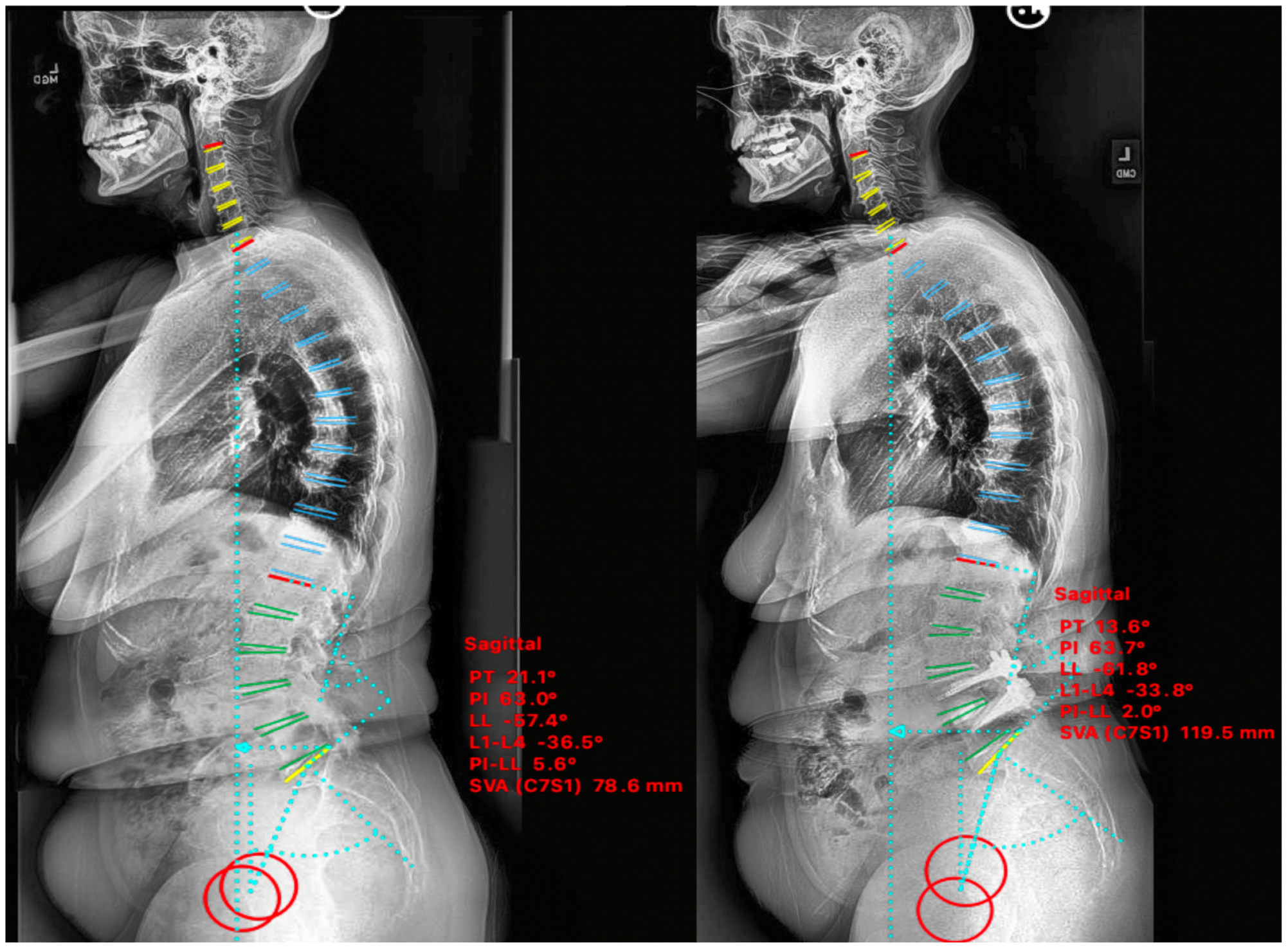
2.5. Non-ACR Cases
2.5.1. Case IV
2.5.2. Case V
3. Discussion
3.1. Historical Treatment of Sagittal Plane Imbalance
3.2. Minimally Invasive Surgery
3.3. Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Slikker, W.S.; Orías, A.A.E.; Shifflett, G.D.; Lee, J.Y.; Siemionow, K.; Gandhi, S.; Fogg, L.; Samartzis, D.; Inoue, N.; An, H.S. Image-Based Markers Predict Dynamic Instability in Lumbar Degenerative Spondylolisthesis. Neurospine 2020, 17, 221–227. [Google Scholar] [CrossRef]
- Drury, T.; Ames, E.; Costi, K.; Beynnon, B.; Hall, J. Degenerative spondylolisthesis in patients with neurogenic claudication effects functional performance and self-reported quality of life. Spine 2009, 34, 2812–2817. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, K.; Okamoto, M.; Hatsushikano, S.; Shimoda, H.; Sato, Y.; Watanabe, K. Etiology and clinical manifestations of double-level versus single-level lumbar degenerative spondylolisthesis. J. Orthop. Sci. 2019, 25, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Moon, B.G.; Kim, D.R.; Kim, J.S. Post-operative flat back: Contribution of posterior accessed lumbar interbody fusion and spinopelvic parameters. J. Korean Neurosurg. Soc. 2014, 56, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.S.; Lee, S.H.; Min, J.H.; Kim, S.K.; Han, K.M.; Maeng, D.H. Surgical treatment of failed back surgery syndrome due to sagittal imbalance. Spine 2007, 32, 3081–3087. [Google Scholar] [CrossRef] [PubMed]
- Aiki, H.; Ohwada, O.; Kobayashi, H.; Hayakawa, M.; Kawaguchi, S.; Takebayashi, T.; Yamashita, T. Adjacent segment stenosis after lumbar fusion requiring second operation. J. Orthop. Sci. 2005, 10, 490–495. [Google Scholar] [CrossRef]
- Rockville, M. Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS); Agency for Healthcare Research and Quality: Rockville, MD, USA, 2012.
- Zhu, W.-Y.; Zang, L.; Li, J.; Guan, L.; Hai, Y. A biomechanical study on proximal junctional kyphosis following long-segment posterior spinal fusion. Braz. J. Med. Biol. Res. 2019, 52, e7748. [Google Scholar] [CrossRef]
- Makhni, M.C.; Shillingford, J.N.; Laratta, J.L.; Hyun, S.-J.; Kim, Y.J. Restoration of Sagittal Balance in Spinal Deformity Surgery. J. Korean Neurosurg. Soc. 2018, 61, 167–179. [Google Scholar] [CrossRef]
- Xu, D.S.; Paluzzi, J.; Kanter, A.S.; Uribe, J.S. Anterior Column Release/Realignment. Neurosurg. Clin. N. Am. 2018, 29, 427–437. [Google Scholar] [CrossRef]
- Mundis, G.M.; Turner, J.D.; Kabirian, N.; Pawelek, J.; Eastlack, R.K.; Uribe, J.; Klineberg, E.; Bess, S.; Ames, C.; Deviren, V.; et al. Anterior Column Realignment Has Similar Results to Pedicle Subtraction Osteotomy in Treating Adults with Sagittal Plane Deformity. World Neurosurg. 2017, 105, 249–256. [Google Scholar] [CrossRef]
- Walker, C.T.; Farber, S.H.; Cole, T.S.; Xu, D.S.; Godzik, J.; Whiting, A.C.; Hartman, C.; Porter, R.W.; Turner, J.D.; Uribe, J. Complications for minimally invasive lateral interbody arthrodesis: A systematic review and meta-analysis comparing prepsoas and transpsoas approaches [published online ahead of print, 25 January 2019]. J. Neurosurg Spine 2019, 30, 446–460. [Google Scholar] [CrossRef] [PubMed]
- Gragnaniello, C.; Seex, K. Anterior to psoas (ATP) fusion of the lumbar spine: Evolution of technique facilitated by changes in equipment. J. Spine Surg. 2016, 2, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Saville, P.A.; Kadam, A.B.; Smith, H.E.; Arlet, V. Anterior hyperlordotic cages: Early experience and radiographic results. J. Neurosurg. Spine 2016, 25, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Patel, A.; Ungar, B.; Farcy, J.P.; Lafage, V. Adult spinal deformity-post-operative standing imbalance: How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 2010, 35, 2224–2231. [Google Scholar] [CrossRef]
- Savage, J.W.; Patel, A.A. Fixed sagittal plane imbalance. Glob. Spine J. 2014, 4, 287–296. [Google Scholar] [CrossRef]
- Glassman, S.D.; Bridwell, K.; Dimar, J.R.; Horton, W.; Berven, S.; Schwab, F. The impact of positive sagittal balance in adult spinal deformity. Spine 2005, 30, 2024–2029. [Google Scholar] [CrossRef]
- Mac-Thiong, J.-M.; Pinel-Giroux, F.-M.; De Guise, J.A.; Labelle, H. Comparison between constrained and non-constrained Cobb techniques for the assessment of thoracic kyphosis and lumbar lordosis. Eur. Spine J. 2007, 16, 1325–1331. [Google Scholar] [CrossRef]
- Lafage, V.; Schwab, F.; Patel, A.; Hawkinson, N.; Farcy, J.P. Pelvic tilt and truncal inclination: Two key radiographic parameters in the setting of adults with spinal deformity. Spine 2009, 34, E599–E606. [Google Scholar] [CrossRef]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J. Bone Jt. Surg. Am. 2005, 87, 260–267. [Google Scholar] [CrossRef]
- Schwab, F.J.; Ungar, B.; Blondel, B.; Buchowski, J.; Coe, J.; Deinlein, D.; DeWald, C.; Mehdian, H.; Shaffrey, C.; Tribus, C.; et al. Scoliosis Research Society-Schwab adult spinal deformity classification: A validation study. Spine 2012, 37, 1077–1082. [Google Scholar] [CrossRef]
- Schwab, F.J.; Blondel, B.; Bess, S.; Hostin, R.; Shaffrey, C.I.; Smith, J.S.; Boachie-Adjei, O.; Burton, D.C.; Akbarnia, B.A.; Mundis, G.M.; et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: A prospective multicenter analysis. Spine 2013, 38, E803–E812. [Google Scholar] [CrossRef] [PubMed]
- Merrill, R.K.; Kim, J.S.; Leven, D.M.; Kim, J.H.; Cho, S.K. Beyond Pelvic Incidence-Lumbar Lordosis Mismatch: The Importance of Assessing the Entire Spine to Achieve Global Sagittal Alignment. Glob. Spine J. 2017, 7, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Park, S.W.; Ko, M.J.; Kim, Y.B.; Le Huec, J.C. Correction of marked sagittal deformity with circumferential minimally invasive surgery using oblique lateral interbody fusion in adult spinal deformity. J. Orthop. Surg. Res. 2020, 15, 13. [Google Scholar] [CrossRef] [PubMed]
- Tannoury, T.; Kempegowda, H.; Haddadi, K.; Tannoury, C. Complications Associated with Minimally Invasive Anterior to the Psoas (ATP) Fusion of the Lumbosacral Spine. Spine 2019, 44, E1122–E1129. [Google Scholar] [CrossRef]
- Mummaneni, P.V.; Park, P.; Shaffrey, C.I.; Wang, M.Y.; Uribe, J.S.; Fessler, R.G.; Chou, D.; Kanter, A.S.; Okonkwo, D.O.; Mundis, G.M.; et al. The MISDEF2 algorithm: An updated algorithm for patient selection in minimally invasive deformity surgery. J. Neurosurg. Spine SPI 2019, 32, 221–228. [Google Scholar] [CrossRef]
- Champagne, P.-O.; Walsh, C.; Diabira, J.; Plante, M.; Wang, Z.; Boubez, G.; Shedid, D. Sagittal Balance Correction Following Lumbar Interbody Fusion: A Comparison of the Three Approaches. Asian Spine J. 2019, 13, 450–458. [Google Scholar] [CrossRef]
- Barone, G.; Scaramuzzo, L.; Zagra, A.; Giudici, F.; Perna, A.; Proietti, L. Adult Spinal Deformity: Effectiveness of Interbody Lordotic Cages to Restore Disc Angle and Spino-Pelvic Parameters through Completely Mini Invasive Trans-Psoas and Hybrid Approach. Eur. Spine J. 2017, 26 (Suppl. S4), 457–463. [Google Scholar] [CrossRef]
- Uribe, J.S.; Harris, J.E.; Beckman, J.M.; Turner, A.W.L.; Mundis, G.M.; Akbarnia, B.A. Finite element analysis of lordosis restoration with anterior longitudinal ligament release and lateral hyperlordotic cage placement. Eur. Spine J. 2015, 24 (Suppl. S3), 420–426. [Google Scholar] [CrossRef]
| Case No. | Age | Sex | Smoker | BMI | Prior ins. | EBL (mL) | ORT (min) | LOS (days) |
|---|---|---|---|---|---|---|---|---|
| 1 | 67 | Female | Yes | 45 | Yes | 300 | 195 | 4 |
| 2 | 64 | Female | No | 49 | No | 200 | 190 | 2 |
| 3 | 58 | Male | No | 27 | No | 300 | 170 | 3 |
| Case | LL° Mean | LL° SD | SVA Mean | SVA SD | PI-LL° Mean | PI-LL° SD |
|---|---|---|---|---|---|---|
| Pre. | −32.6 | 16.0 | 180.5 | 31.9 | 26.4 | 22.2 |
| Post. | −56.0 | 12.8 | 61.3 | 18.0 | 5.1 | 16.5 |
| Case No. | Level | Arthro. | Ant ins. | Post ins. | Cage Type | Cage Size (mm) | Allograft | Autograft |
|---|---|---|---|---|---|---|---|---|
| 1 | L3-4 | Yes | Yes | Yes | Expandable | 11–20 × 20 × 45 | Yes | Yes |
| 2 | L4-5 | Yes | Yes | Yes | Expandable | 11–20 × 20 × 50 | Yes | No |
| 3 | L4-5 | Yes | Yes | Yes | Expandable | 11–20 × 20 × 55 | Yes | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mathkour, M.; Shapiro, S.Z.; Scullen, T.; Werner, C.; Kilgore, M.D.; Chavarro, V.S.; Denis, D.R. Single Level Spondylolisthesis Associated Sagittal Plane Imbalance Corrected by Pre-Psoas Interbody Fusion Using Anterior Column Release with 30° Expandable Hyperlordotic Cage. Medicina 2022, 58, 1172. https://doi.org/10.3390/medicina58091172
Mathkour M, Shapiro SZ, Scullen T, Werner C, Kilgore MD, Chavarro VS, Denis DR. Single Level Spondylolisthesis Associated Sagittal Plane Imbalance Corrected by Pre-Psoas Interbody Fusion Using Anterior Column Release with 30° Expandable Hyperlordotic Cage. Medicina. 2022; 58(9):1172. https://doi.org/10.3390/medicina58091172
Chicago/Turabian StyleMathkour, Mansour, Stephen Z. Shapiro, Tyler Scullen, Cassidy Werner, Mitchell D. Kilgore, Velina S. Chavarro, and Daniel R. Denis. 2022. "Single Level Spondylolisthesis Associated Sagittal Plane Imbalance Corrected by Pre-Psoas Interbody Fusion Using Anterior Column Release with 30° Expandable Hyperlordotic Cage" Medicina 58, no. 9: 1172. https://doi.org/10.3390/medicina58091172
APA StyleMathkour, M., Shapiro, S. Z., Scullen, T., Werner, C., Kilgore, M. D., Chavarro, V. S., & Denis, D. R. (2022). Single Level Spondylolisthesis Associated Sagittal Plane Imbalance Corrected by Pre-Psoas Interbody Fusion Using Anterior Column Release with 30° Expandable Hyperlordotic Cage. Medicina, 58(9), 1172. https://doi.org/10.3390/medicina58091172





