Is Femoral Neck System a Valid Alternative for the Treatment of Displaced Femoral Neck Fractures in Adolescents? A Comparative Study of Femoral Neck System versus Cannulated Compression Screw
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Surgical Procedure
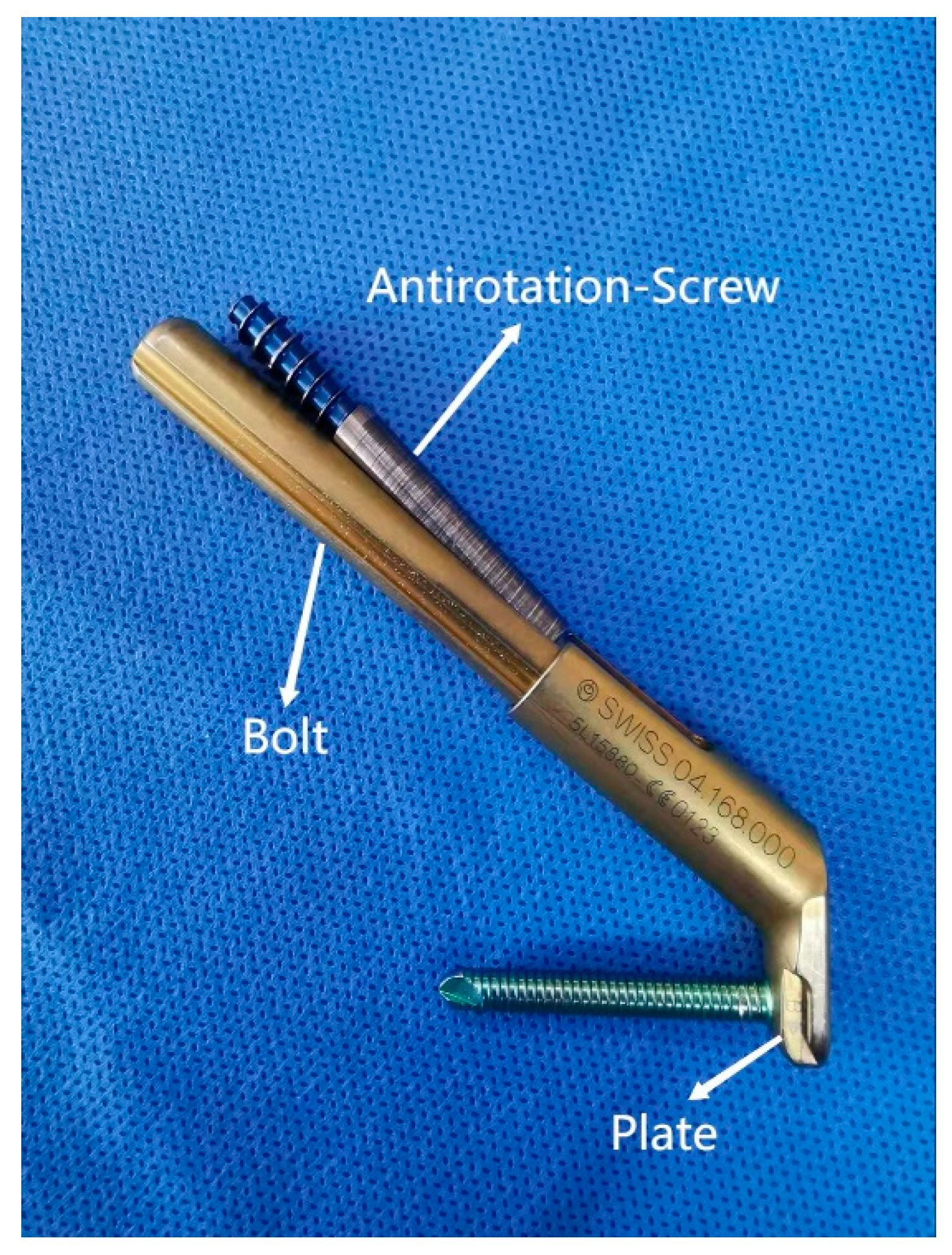
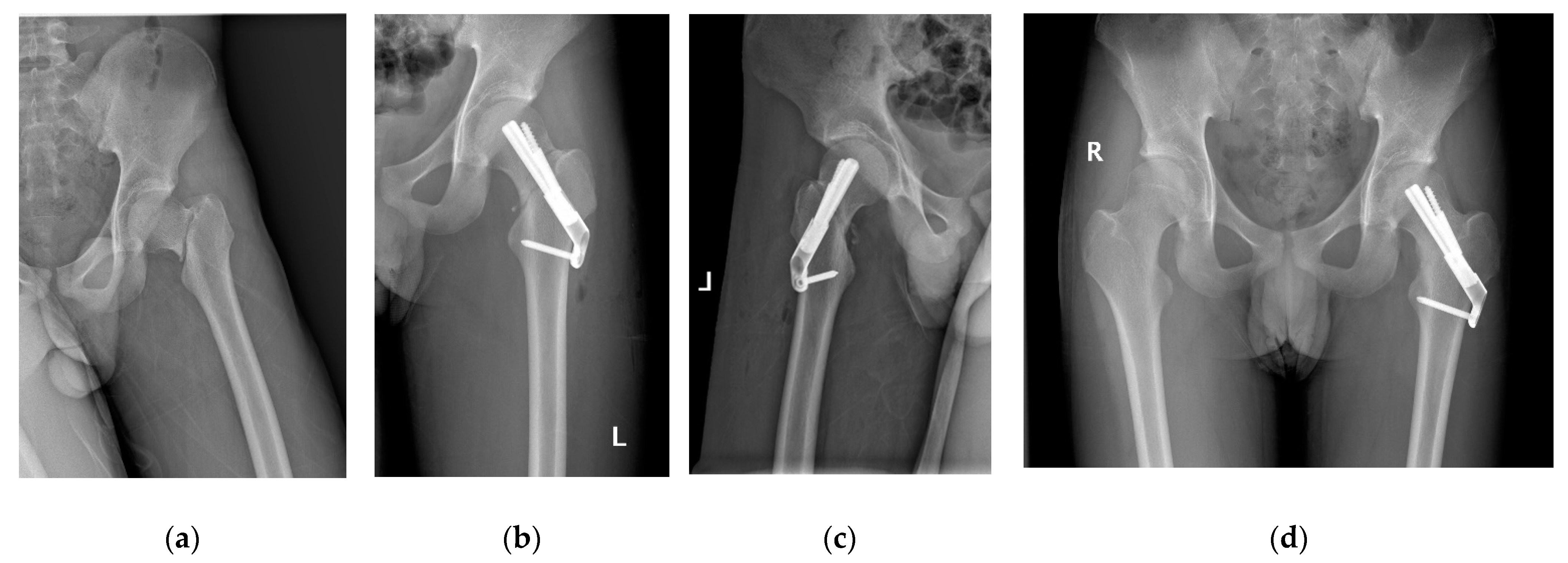
2.3. Femoral Neck System
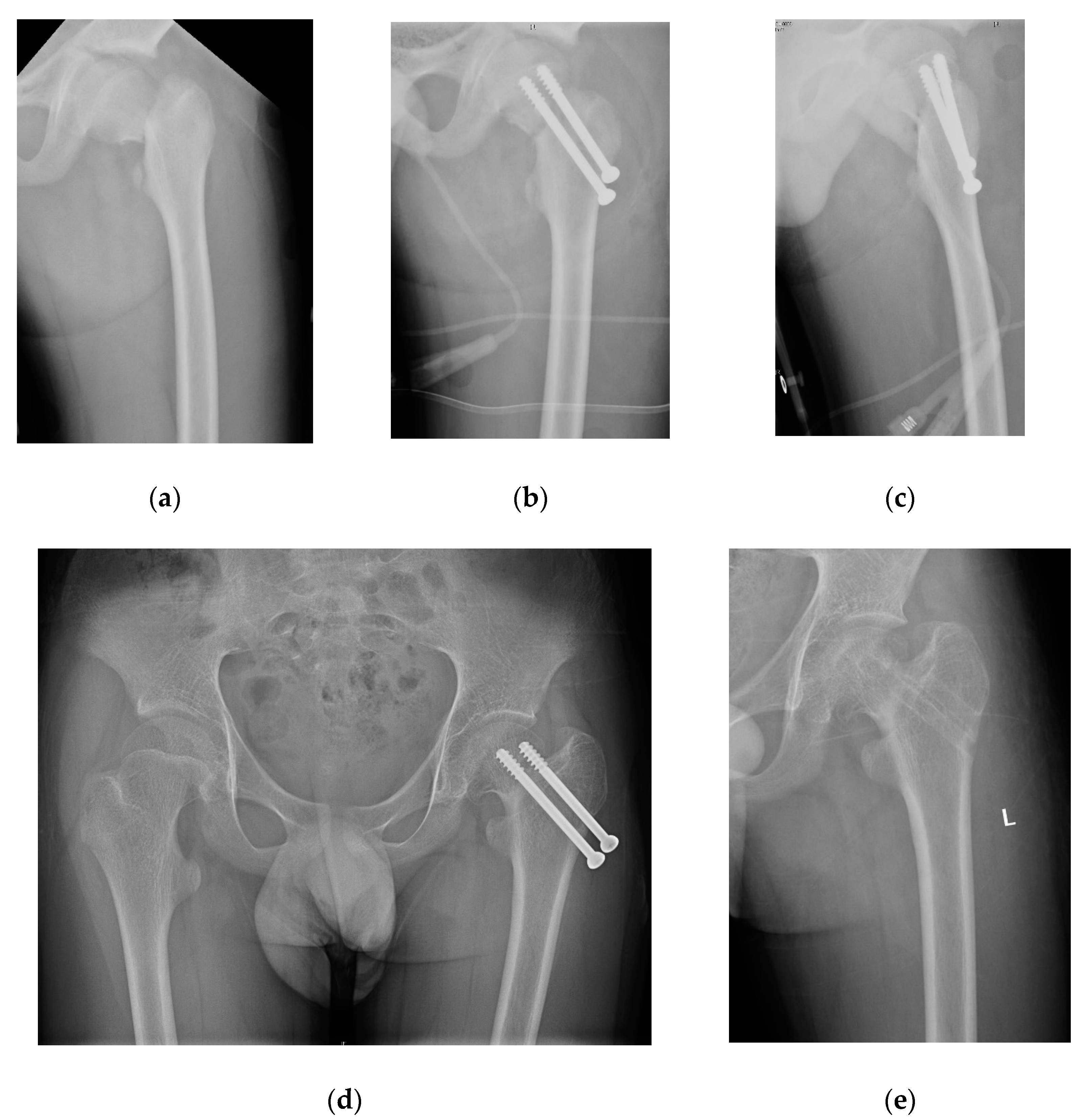
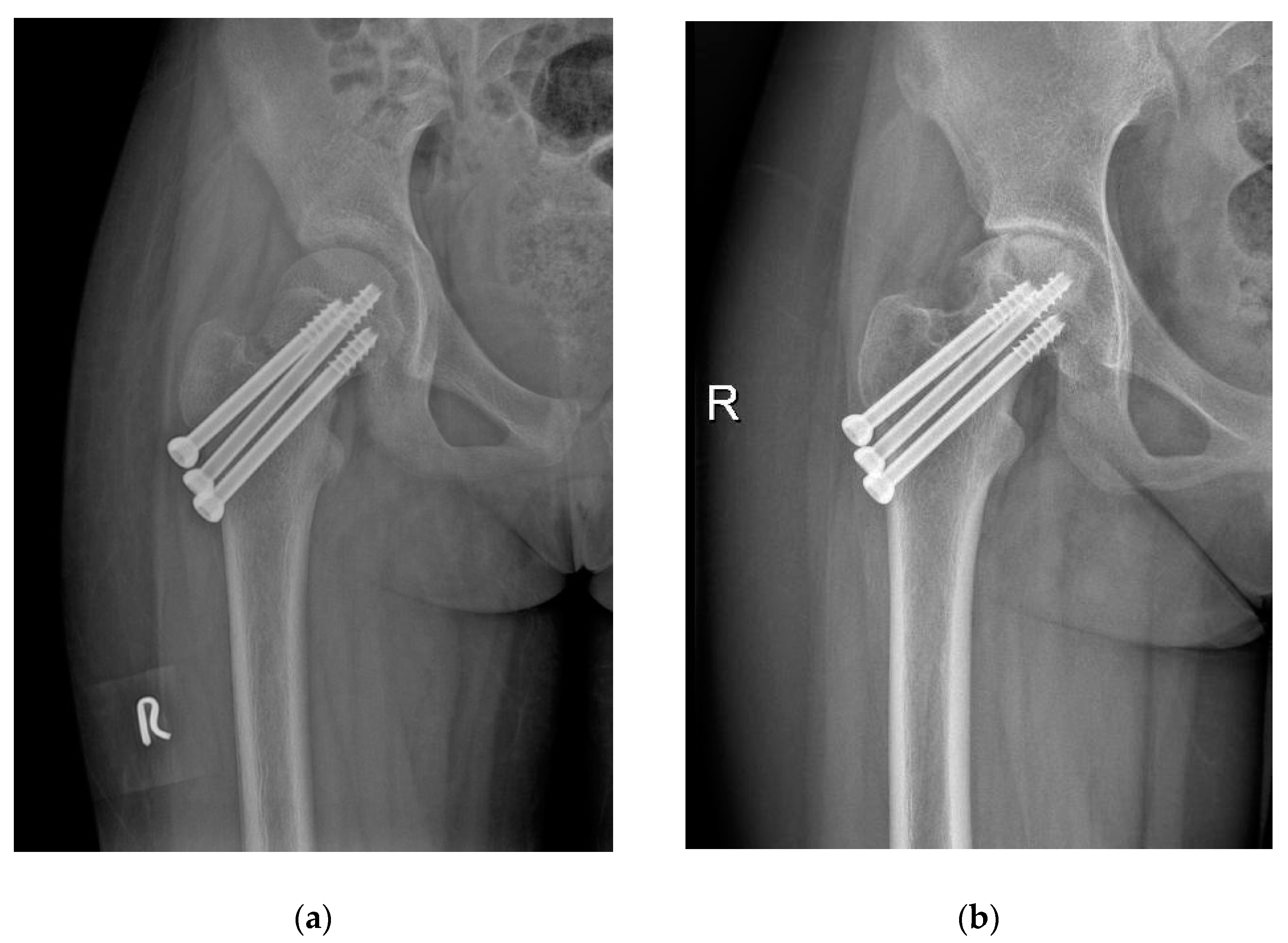
2.4. Cannulated Compression Screw
2.5. Perioperative Management
2.6. Radiographic Evaluation
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
References
- Patterson, J.T.; Tangtiphaiboontana, J.; Pandya, N.K. Management of Pediatric Femoral Neck Fracture. J. Am. Acad. Orthop. Surg. 2018, 26, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Barreto Rocha, D.F.; Horwitz, D.S.; Sintenie, J.B. Femoral Neck Fractures in Children: Issues, Challenges, and Solutions. J. Orthop. Trauma 2019, 8, S27–S32. [Google Scholar] [CrossRef] [PubMed]
- Bimmel, R.; Bakker, A.; Bosma, B.; Michielsen, J. Paediatric hip fractures: A systematic review of incidence, treatment options and complications. Acta. Orthop. Belg. 2010, 76, 7–13. [Google Scholar] [PubMed]
- Wang, W.T.; Li, Y.Q.; Guo, Y.M.; Li, M.; Mei, H.B.; Shao, J.F.; Xiong, Z.; Li, J.; Canavese, F.; Chen, S.Y. Risk factors for the development of avascular necrosis after femoral neck fractures in children: A review of 239 cases. Bone Jt. J. 2019, 101, 1160–1167. [Google Scholar] [CrossRef]
- Stoffel, K.; Zderic, I.; Gras, F.; Sommer, C.; Eberli, U.; Mueller, D.; Oswald, M.; Gueorguiev, B. Biomechanical Evaluation of the Femoral Neck System in Unstable Pauwels III Femoral Neck Fractures: A Comparison with the Dynamic Hip Screw and Cannulated Screws. J. Orthop. Trauma 2017, 31, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Schopper, C.; Zderic, I.; Menze, J.; Müller, D.; Rocci, M.; Knobe, M.; Shoda, E.; Richards, G.; Gueorguiev, B.; Stoffel, K. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J. Orthop. Translat. 2020, 24, 88–95. [Google Scholar] [CrossRef]
- He, C.; Lu, Y.; Wang, Q.; Ren, C.; Li, M.; Yang, M.; Xu, Y.; Li, Z.; Zhang, K.; Ma, T. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet. Disord. 2021, 22, 994. [Google Scholar] [CrossRef]
- Hu, H.; Cheng, J.; Feng, M.; Gao, Z.; Wu, J.; Lu, S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J. Orthop. Surg. Res. 2021, 16, 370. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.Q.; Li, Z.Q.; Xu, R.J.; She, Y.S.; Zhang, X.X.; Chen, G.X.; Yu, X. Comparison of Early Clinical Results for Femoral Neck System and Cannulated Screws in the Treatment of Unstable Femoral Neck Fractures. Orthop. Surg. 2021, 13, 1802–1809. [Google Scholar] [CrossRef]
- Cheung, P.W.H.; Canavese, F.; Chan, C.Y.W.; Wong, J.S.H.; Shigematsu, H.; Luk, K.D.K.; Cheung, J.P.Y. The Utility of a Novel Proximal Femur Maturity Index for Staging Skeletal Growth in Patients with Idiopathic Scoliosis. J. Bone Jt. Surg. Am. 2022, 104, 630–640. [Google Scholar] [CrossRef] [PubMed]
- Colonna, P.C. Fracture of the neck of the femur in childhood: A report of six cases. Ann. Surg. 1928, 88, 902–907. [Google Scholar] [CrossRef]
- Shen, M.; Wang, C.; Chen, H.; Rui, Y.F.; Zhao, S. An update on the Pauwels classification. J. Orthop. Surg. Res. 2016, 11, 161. [Google Scholar] [CrossRef] [Green Version]
- Song, K.S. Displaced fracture of the femoral neck in children: Open versus closed reduction. J. Bone Jt. Surg. Br. 2010, 92, 1148–1151. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Li, Y.; Xiong, Z.; Guo, Y.; Li, M.; Mei, H.; Shao, J.; Li, J.; Canavese, F.; Chen, S. Effect of the Number, Size, and Location of Cannulated Screws on the Incidence of Avascular Necrosis of the Femoral Head in Pediatric Femoral Neck Fractures: A Review of 153 Cases. J. Pediatr. Orthop. 2022, 42, 149–157. [Google Scholar] [CrossRef]
- Ratliff, A.H. Fractures of the neck of the femur in children. J. Bone Jt. Surg. Br. 1962, 44, 528–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zlowodzki, M.; Brink, O.; Switzer, J.; Wingerter, S.; Woodall, J., Jr.; Petrisor, B.A.; Kregor, P.J.; Bruinsma, D.R.; Bhandari, M. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: A multi-centre cohort study. J. Bone Jt. Surg. Br. 2008, 90, 1487–1494. [Google Scholar] [CrossRef]
- Chen, C.E.; Ko, J.Y.; Wang, C.J. Premature closure of the physeal plate after treatment of a slipped capital femoral epiphysis. Chang Gung Med. J. 2002, 25, 811–818. [Google Scholar]
- Haidukewych, G.J.; Rothwell, W.S.; Jacofsky, D.J.; Torchia, M.E.; Berry, D.J. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J. Bone Jt. Surg. Am. 2004, 86, 1711–1716. [Google Scholar] [CrossRef]
- Pavone, V.; Testa, G.; Riccioli, M.; Di Stefano, A.; Condorelli, G.; Sessa, G. Surgical treatment with cannulated screws for pediatric femoral neck fractures: A case series. Injury 2019, 50 (Suppl. S2), S40–S44. [Google Scholar] [CrossRef]
- Joeris, A.; Audigé, L.; Ziebarth, K.; Slongo, T. The Locking Compression Paediatric Hip Plate: Technical guide and critical analysis. Int. Orthop. 2012, 36, 2299–2306. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.Y.; Mei, H.B.; Guo, Y.M.; Shao, J.F.; Xu, H.W.; Li, J.; Jiang, F.; Nan, G.X.; Pan, Y.C. Efficacies of pediatric hip plating versus cannulated screw fixation for Delbet types II & III pediatric femoral neck fractures: A retrospective multicenter study. Chin. J. Pediatr. Surg. 2016, 37, 898–902. [Google Scholar] [CrossRef]
- Spence, D.; DiMauro, J.P.; Miller, P.E.; Glotzbecker, M.P.; Hedequist, D.J.; Shore, B.J. Osteonecrosis After Femoral Neck Fractures in Children and Adolescents: Analysis of Risk Factors. J. Pediatr. Orthop. 2016, 36, 111–116. [Google Scholar] [CrossRef] [PubMed]
| Variables | FNS (n = 28) | CCS (n = 30) | Statistic (t/χ2) | p Value |
|---|---|---|---|---|
| Age (years) | 14.5 ± 1.6 | 14.3 ± 1.5 | 0.394 | 0.695 |
| Sex | ||||
| Male | 19 (67.9%) | 22 (73.3%) | 0.210 | 0.647 |
| Female | 9 (32.1%) | 8 (26.7%) | ||
| Side | ||||
| Left | 16 (57.1%) | 13 (43.3%) | 1.105 | 0.293 |
| Right | 12 (42.9%) | 17 (56.7%) | ||
| Time from injury to surgery (days) | 3.2 ± 1.5 | 3.6 ± 1.9 | −0.869 | 0.389 |
| Mechanism of injury | ||||
| Traffic accident | 14 (50%) | 10 (33.3%) | 4.088 | 0.129 |
| Fall from height | 6 (21.4%) | 14 (46.7%) | ||
| Sports injury | 8 (28.6%) | 6 (20%) | ||
| Delbet–Colonna Type | ||||
| Delbet-II | 20 (71.4%) | 18 (60%) | 0.837 | 0.360 |
| Delbet-III | 8 (28.6%) | 12 (40%) | ||
| Pauwels type | ||||
| Pauwels-I | 2 (7.1%) | 8 (26.7%) | 4.402 | 0.111 |
| Pauwels-II | 18 (64.3%) | 13 (43.3%) | ||
| Pauwels-III | 8 (28.6%) | 9 (30%) | ||
| Initial displacement | ||||
| Type I | 2 (7.1%) | 4 (13.3%) | 0.914 | 0.633 |
| Type II | 14 (50%) | 16 (53.3%) | ||
| Type III | 12 (42.9%) | 10 (33.3%) | ||
| Variables | FNS (n = 28) | CCS (n = 30) | Statistics (t/χ2) | p Value |
|---|---|---|---|---|
| Reduction method | ||||
| CRIF | 20 (71.4%) | 24 (80%) | 0.581 | 0.446 |
| ORIF | 8 (28.6%) | 6 (20%) | ||
| Operation time (min) | 53.9 ± 10.6 | 50.0 ± 7.6 | 1.616 | 0.112 |
| Blood loss (mL) | 44.3 ± 7.8 | 16.7 ± 3.1 | 17.932 | 0.001 |
| Fluoroscopies (n) | 16.9 ± 4.7 | 16.0 ± 4.2 | −0.090 | 0.928 |
| Reduction quality | ||||
| Anatomical | 19 (67.9%) | 21 (20.7%) | 0.432 | 0.806 |
| Acceptable | 7 (25%) | 8 (26.7%) | ||
| Unacceptable | 2 (7.1%) | 1 (3.3%) | ||
| Variables | FNS (n = 28) | CCS (n = 30) | Statistics (t/χ2) | p Value |
|---|---|---|---|---|
| Follow-up time (months) | 16.3 ± 2.0 | 17.0 ± 2.5 | −1.208 | 0.232 |
| Consolidation time (weeks) | 10.5 ± 1.5 | 14.0 ± 2.2 | −7.054 | 0.000 |
| Functional evaluations | ||||
| Excellent | 15 (53.6%) | 7 (23.3%) | 7.009 | 0.030 |
| Good | 10 (35.7%) | 13 (43.3%) | ||
| Poor | 3 (10.7%) | 10 (33.3%) | ||
| Complications | ||||
| Femoral head necrosis | 4 (14.3%) | 8 (26.7%) | 1.353 | 0.245 |
| Neck shortening | 2 (7.1%) | 6 (20%) | 2.013 | 0.156 |
| Nail retreat | 0 (0%) | 5 (16.7%) | 5.107 | 0.024 |
| Premature epiphyseal closure | 3 (7.1%) | 3 (6.7%) | 0.008 | 0.929 |
| Coxa vara | 1 (3.6%) | 3 (10%) | 0.932 | 0.334 |
| Nonunion | 0 (0%) | 1 (3.3%) | 0.950 | 0.330 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, Y.; Canavese, F.; Nan, G.; Lin, R.; Huang, Y.; Pan, N.; Chen, S. Is Femoral Neck System a Valid Alternative for the Treatment of Displaced Femoral Neck Fractures in Adolescents? A Comparative Study of Femoral Neck System versus Cannulated Compression Screw. Medicina 2022, 58, 999. https://doi.org/10.3390/medicina58080999
Lu Y, Canavese F, Nan G, Lin R, Huang Y, Pan N, Chen S. Is Femoral Neck System a Valid Alternative for the Treatment of Displaced Femoral Neck Fractures in Adolescents? A Comparative Study of Femoral Neck System versus Cannulated Compression Screw. Medicina. 2022; 58(8):999. https://doi.org/10.3390/medicina58080999
Chicago/Turabian StyleLu, Yunan, Federico Canavese, Guoxin Nan, Ran Lin, Yuling Huang, Nuoqi Pan, and Shunyou Chen. 2022. "Is Femoral Neck System a Valid Alternative for the Treatment of Displaced Femoral Neck Fractures in Adolescents? A Comparative Study of Femoral Neck System versus Cannulated Compression Screw" Medicina 58, no. 8: 999. https://doi.org/10.3390/medicina58080999
APA StyleLu, Y., Canavese, F., Nan, G., Lin, R., Huang, Y., Pan, N., & Chen, S. (2022). Is Femoral Neck System a Valid Alternative for the Treatment of Displaced Femoral Neck Fractures in Adolescents? A Comparative Study of Femoral Neck System versus Cannulated Compression Screw. Medicina, 58(8), 999. https://doi.org/10.3390/medicina58080999







