Solitary Rectal Ulcer Syndrome Is Not Always Ulcerated: A Case Report
Abstract
:1. Introduction
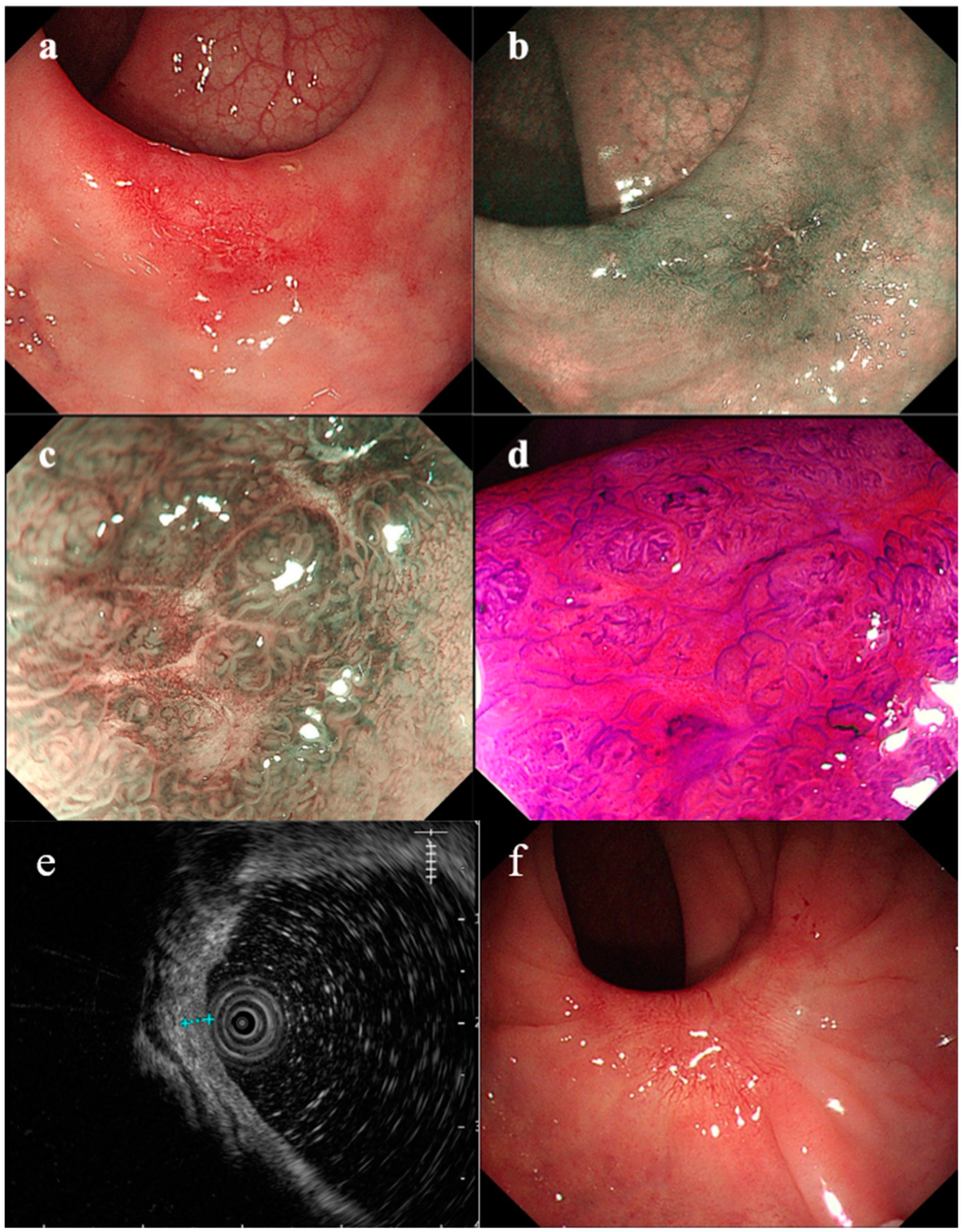
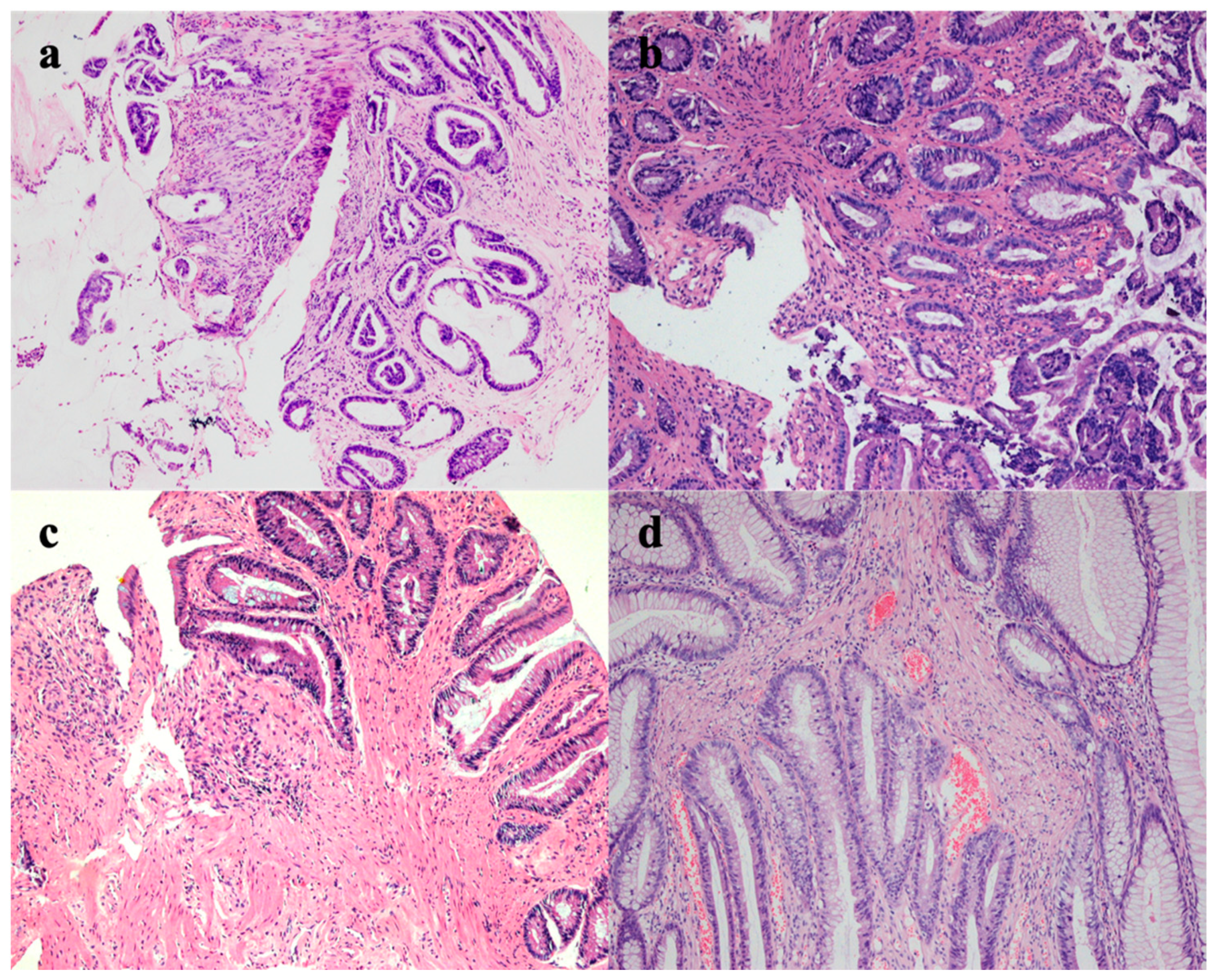
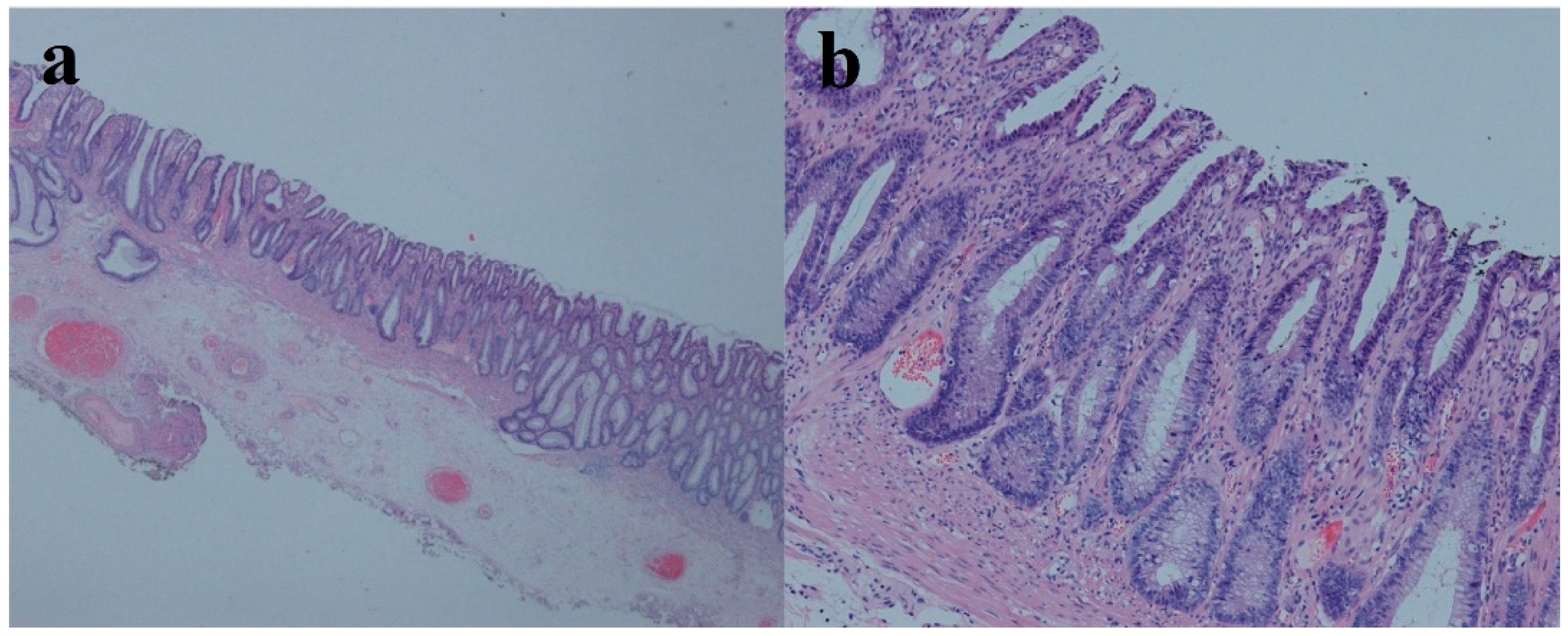
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Felt-Bersma, R.J.F.; Tiersma, E.S.M.; Cuesta, M.A. Rectal Prolapse, Rectal Intussusception, Rectocele, Solitary Rectal Ulcer Syndrome, and Enterocele. Gastroenterol. Clin. N. Am. 2008, 37, 645–668. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.; Parks, T.; Biggart, J. Solitary rectal ulcer syndrome in Northern Ireland. 1971–1980. Br. J. Surg. 1981, 68, 744–747. [Google Scholar] [CrossRef] [PubMed]
- Edden, Y.; Shih, S.; Wexner, S. Solitary rectal ulcer syndrome and stercoral ulcers. Gastroenterol. Clin. N. Am. 2009, 38, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.C.; Shen, R.R.; Qin, H.L.; Wang, Y. Solitary rectal ulcer syndrome: Clinical features, pathophysiology, diagnosis and treatment strategies. World J. Gastroenterol. 2014, 20, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Forootan, M.; Darvishi, M. Solitary rectal ulcer syndrome: A systematic review. Medicine 2018, 97, e0565. [Google Scholar] [CrossRef] [PubMed]
- Nagar, A. Isolated colonic ulcers: Diagnosis and management. Curr. Gastroenterol. Rep. 2007, 9, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Latos, W.; Kawczyk-Krupka, A.; Ledwoń, A.; Sieroń-Stołtny, K.; Sieroń, A. Solitary rectal ulcer syndrome-The role of autofluorescence colonoscopy. Photodiagn. Photodyn. Ther. 2007, 4, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Morio, O.; Meurette, G.; Desfourneaux, V.; D’Halluin, P.N.; Bretagne, J.F.; Siproudhis, L. Anorectal physiology in solitary ulcer syndrome: A case-matched series. Dis. Colon Rectum 2005, 48, 1917–1922. [Google Scholar] [CrossRef] [PubMed]
- Mueller, J.D.; Bethke, B.; Stolte, M. Colorectal de novo carcinoma: A review of its diagnosis, histopathology, molecular biology, and clinical relevance. Virchows Arch. Int. J. Pathol. 2002, 440, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Hurlstone, D.P.; Sanders, D.S.; Thomson, M. Detection and treatment of early flat and depressed colorectal cancer using high-magnification chromoscopic colonoscopy: A change in paradigm for Western endoscopists? Dig. Dis. Sci. 2007, 52, 1387–1393. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Chen, Z.; Dou, L.; Yang, Z.; Wang, G. Solitary Rectal Ulcer Syndrome Is Not Always Ulcerated: A Case Report. Medicina 2022, 58, 1136. https://doi.org/10.3390/medicina58081136
Liu Y, Chen Z, Dou L, Yang Z, Wang G. Solitary Rectal Ulcer Syndrome Is Not Always Ulcerated: A Case Report. Medicina. 2022; 58(8):1136. https://doi.org/10.3390/medicina58081136
Chicago/Turabian StyleLiu, Yi, Zhihao Chen, Lizhou Dou, Zhaoyang Yang, and Guiqi Wang. 2022. "Solitary Rectal Ulcer Syndrome Is Not Always Ulcerated: A Case Report" Medicina 58, no. 8: 1136. https://doi.org/10.3390/medicina58081136
APA StyleLiu, Y., Chen, Z., Dou, L., Yang, Z., & Wang, G. (2022). Solitary Rectal Ulcer Syndrome Is Not Always Ulcerated: A Case Report. Medicina, 58(8), 1136. https://doi.org/10.3390/medicina58081136




