Pain Management during Office Hysteroscopy: An Evidence-Based Approach
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. The Effect of Anxiety, Duration of the Procedure and Operator Experience on Reported Procedural Pain during in Office Hysteroscopy
Recommendations for the Management of Women Undergoing Office Hysteroscopy
- Strategies aimed to reduce the anxiety level are useful to improve comfort and decrease pain during in office hysteroscopy (Level A).
- Waiting time before office hysteroscopy should be minimized as much as possible, since it is associated with increased pain levels (Level B).
- Procedural time should be reduced as much as possible, scheduling the patient for office hysteroscopy when the condition to be treated is suitable for the operator experience (Level A).
3.2. Neuronal and Anatomical Features of Pain in Patients with Endometriosis/Adenomyosis
Recommendations for Pain Management in Women with Known or Suspected Adenomyosis or Endometriosis Undergoing Outpatient Hysteroscopy
- Hysteroscopists should pay particular attention for pain management in women who experienced dysmenorrhea, since the level of pain could be significantly higher compared to women without dysmenorrhea (Level B).
- Women with known or suspected adenomyosis/endometriosis needs adequate pain management strategies before undergoing outpatient hysteroscopy, since the level of pain could be significantly higher compared to women without it (Level B).
3.3. Non-Pharmacological Strategies
Recommendations about Non-Pharmacological Strategies for Management of Pain in Women Undergoing Office Hysteroscopy—Before the Procedure
- The video-based multimedia information (MMI) administration before procedure is more efficient in anxiety reduction compared to traditional written information (Level B).
- Listening to music during the procedure provides pain and anxiety relief (Level B).
3.4. Pharmacological Strategies
Recommendations about Pharmacological Cervical Preparation/Ripening in Women Undergoing Office Hysteroscopy
- The ideal time and dose of dinoprostone administration should be 3 mg vaginally 12 h before office hysteroscopy rather than 3 h before the procedure. This timing is more efficient in reducing pain (VAS score), increase the ease of procedure, and patient’s satisfaction (Level A).
- Misoprostol administration before office hysteroscopy is considered efficient in facilitating cervical priming (Level B) and reducing procedural pain (Level A).
- Vaginal isoniazid is more efficient than misoprostol in cervical priming (Level B).
3.5. Technical Variables: Temperature and Pressure of the Distension Medium
Recommendations about Temperature and Pressure of the Distension Medium in Women Undergoing Outpatient Hysteroscopy—During the Procedure
- Using warm saline infusion (41 °C) during office hysteroscopy with the purpose of decreasing pain level during the procedure is not effective (Level B).
- The distention media infusion pressure is correlated to the pain perceived during hysteroscopy and should be at the lowest possible for achieving an adequate visualization (Level B).
- The use of normal saline as distention media is better than carbon dioxide in reducing postprocedural pain, with lower side-effects, and increased patient satisfaction (Level B).
3.6. The Role of Analgesic Administration
Recommendations for Analgesic Administration in Women Undergoing Office Hysteroscopy—During the Procedure
- Diclofenac sodium administration 1 h before office hysteroscopy is not effective in reducing pain during hysteroscopic procedures (Level B).
- Paracetamol and Ibuprofen administration 1 h before office hysteroscopy is not efficient in reducing pain during hysteroscopic procedures (Level B).
- Tramadol administration before hysteroscopy procedure is safe and efficient in reducing pain during and after diagnostic outpatient hysteroscopy (Level A).
4. Conclusions
5. Stakeholders’ Involvement and Applicability
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van Hanegem, N.; Prins, M.M.C.; Bongers, M.Y.; Opmeer, B.C.; Sahota, D.S.; Mol, B.W.J.; Timmermans, A. The Accuracy of Endometrial Sampling in Women with Postmenopausal Bleeding: A Systematic Review and Meta-Analysis. Eur. J. Obs. Gynecol. Reprod. Biol. 2016, 197, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Bosteels, J.; van Wessel, S.; Weyers, S.; Broekmans, F.J.; D’Hooghe, T.M.; Bongers, M.Y.; Mol, B.W.J. Hysteroscopy for Treating Subfertility Associated with Suspected Major Uterine Cavity Abnormalities. Cochrane Database Syst. Rev. 2018, 12, CD009461. [Google Scholar] [CrossRef]
- Vitale, S.G.; Laganà, A.S.; Caruso, S.; Garzon, S.; Vecchio, G.M.; La Rosa, V.L.; Casarin, J.; Ghezzi, F. Comparison of Three Biopsy Forceps for Hysteroscopic Endometrial Biopsy in Postmenopausal Patients (HYGREB-1): A Multicenter, Single-Blind Randomized Clinical Trial. Int. J. Gynaecol. Obs. 2021, 155, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.G. The Biopsy Snake Grasper Sec. VITALE: A New Tool for Office Hysteroscopy. J. Minim. Invasive Gynecol. 2020, 27, 1414–1416. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.G.; Sapia, F.; Rapisarda, A.M.C.; Valenti, G.; Santangelo, F.; Rossetti, D.; Chiofalo, B.; Sarpietro, G.; La Rosa, V.L.; Triolo, O.; et al. Hysteroscopic Morcellation of Submucous Myomas: A Systematic Review. BioMed Res. Int. 2017, 2017, 6848250. [Google Scholar] [CrossRef]
- Carugno, J.; Marbin, S.J.; LaganÀ, A.S.; Vitale, S.G.; Alonso, L.; DI Spiezio Sardo, A.; Haimovich, S. New Development on Hysteroscopy for Endometrial Cancer Diagnosis: State of the Art. Minerva Med. 2021, 112, 12–19. [Google Scholar] [CrossRef]
- Cignini, P.; Vitale, S.G.; Laganà, A.S.; Biondi, A.; La Rosa, V.L.; Cutillo, G. Preoperative Work-up for Definition of Lymph Node Risk Involvement in Early Stage Endometrial Cancer: 5-year follow-up. Updates Surg. 2017, 69, 75–82. [Google Scholar] [CrossRef]
- Raz, N.; Sigal, E.; Gonzalez Arjona, F.; Calidona, C.; Garzon, S.; Uccella, S.; Laganà, A.S.; Haimovich, S. See-and-Treat in-Office Hysteroscopy versus Operative Hysteroscopy for the Treatment of Retained Products of Conception: A Retrospective Study. J. Obs. Gynaecol. Res. 2022. [Google Scholar] [CrossRef]
- Garzon, S.; Laganà, A.S.; Di Spiezio Sardo, A.; Alonso Pacheco, L.; Haimovich, S.; Carugno, J.; Vitale, S.G.; Casarin, J.; Raffaelli, R.; Andrisani, A.; et al. Hysteroscopic Metroplasty for T-Shaped Uterus: A Systematic Review and Meta-Analysis of Reproductive Outcomes. Obs. Gynecol. Surv. 2020, 75, 431–444. [Google Scholar] [CrossRef]
- Esteban Manchado, B.; Lopez-Yarto, M.; Fernandez-Parra, J.; Rodriguez-Oliver, A.; Gonzalez-Paredes, A.; Laganà, A.S.; Garzon, S.; Haimovich, S. Office Hysteroscopic Metroplasty with Diode Laser for Septate Uterus: A Multicenter Cohort Study. Minim. Invasive Allied Technol. 2022, 31, 441–447. [Google Scholar] [CrossRef]
- Laganà, A.S.; Garzon, S.; Alkatout, I.; Hortu, İ.; Gitas, G.; Vitale, S.G.; Gubbini, G. Isthmocele: When Surgery is Both the Problem and the Solution. J. Investig. Surg. 2022, 35, 231–232. [Google Scholar] [CrossRef] [PubMed]
- Laganà, A.S.; Pacheco, L.A.; Tinelli, A.; Haimovich, S.; Carugno, J.; Ghezzi, F. Global Congress on Hysteroscopy Scientific Committee Optimal Timing and Recommended Route of Delivery after Hysteroscopic Management of Isthmocele? A Consensus Statement from the Global Congress on Hysteroscopy Scientific Committee. J. Minim. Invasive Gynecol. 2018, 25, 558. [Google Scholar] [CrossRef] [PubMed]
- Salazar, C.A.; Isaacson, K.B. Office Operative Hysteroscopy: An Update. J. Minim. Invasive Gynecol. 2018, 25, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Readman, E.; Hicks, L.; Porter, J.; Cameron, M.; Ellett, L.; Mcilwaine, K.; Manwaring, J.; Maher, P. Is Outpatient Hysteroscopy the New Gold Standard? Results from an 11 Year Prospective Observational Study. Aust. N. Z. J. Obs. Gynaecol. 2017, 57, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, A.; Smith, P.; Clark, T.J. Benchmarking Services in Outpatient Hysteroscopy (OPH): A Quality Improvement Project. Eur. J. Obs. Gynecol. Reprod. Biol. 2021, 259, 211–221. [Google Scholar] [CrossRef]
- Riemma, G.; Schiattarella, A.; Colacurci, N.; Vitale, S.G.; Cianci, S.; Cianci, A.; De Franciscis, P. Pharmacological and Non-Pharmacological Pain Relief for Office Hysteroscopy: An up-to-Date Review. Climacteric 2020, 23, 376–383. [Google Scholar] [CrossRef]
- Cicinelli, E. Hysteroscopy without Anesthesia: Review of Recent Literature. J. Minim. Invasive Gynecol. 2010, 17, 703–708. [Google Scholar] [CrossRef]
- Ireland, L.D.; Allen, R.H. Pain Management for Gynecologic Procedures in the Office. Obs. Gynecol. Surv. 2016, 71, 89–98. [Google Scholar] [CrossRef]
- Brouwers, M.C.; Kerkvliet, K.; Spithoff, K. AGREE next Steps Consortium The AGREE Reporting Checklist: A Tool to Improve Reporting of Clinical Practice Guidelines. BMJ 2016, 352, i1152. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE Working Group GRADE: An Emerging Consensus on Rating Quality of Evidence and Strength of Recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Gambadauro, P.; Navaratnarajah, R.; Carli, V. Anxiety at Outpatient Hysteroscopy. Gynecol. Surg. 2015, 12, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Burton, D.; King, A.; Bartley, J.; Petrie, K.J.; Broadbent, E. The Surgical Anxiety Questionnaire (SAQ): Development and Validation. Psychol. Health 2019, 34, 129–146. [Google Scholar] [CrossRef] [PubMed]
- Theunissen, M.; Peters, M.L.; Schouten, E.G.W.; Fiddelers, A.A.A.; Willemsen, M.G.A.; Pinto, P.R.; Gramke, H.-F.; Marcus, M.A.E. Validation of the Surgical Fear Questionnaire in Adult Patients Waiting for Elective Surgery. PLoS ONE 2014, 9, e100225. [Google Scholar] [CrossRef]
- Jawaid, M.; Mushtaq, A.; Mukhtar, S.; Khan, Z. Preoperative Anxiety before Elective Surgery. Neurosci. J. 2007, 12, 145–148. [Google Scholar]
- Gupta, J.K.; Clark, T.J.; More, S.; Pattison, H. Patient Anxiety and Experiences Associated with an Outpatient “One-Stop” “See and Treat” Hysteroscopy Clinic. Surg. Endosc. 2004, 18, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.G.; Caruso, S.; Ciebiera, M.; Török, P.; Tesarik, J.; Vilos, G.A.; Cholkeri-Singh, A.; Gulino, F.A.; Kamath, M.S.; Cianci, A. Management of Anxiety and Pain Perception in Women Undergoing Office Hysteroscopy: A Systematic Review. Arch. Gynecol. Obs. 2020, 301, 885–894. [Google Scholar] [CrossRef]
- Sorrentino, F.; Petito, A.; Angioni, S.; D’Antonio, F.; Severo, M.; Solazzo, M.C.; Tinelli, R.; Nappi, L. Impact of Anxiety Levels on the Perception of Pain in Patients Undergoing Office Hysteroscopy. Arch. Gynecol. Obs. 2021, 303, 999–1007. [Google Scholar] [CrossRef]
- Kokanali, M.K.; Cavkaytar, S.; Guzel, A.İ.; Topçu, H.O.; Eroğlu, E.; Aksakal, O.; Doğanay, M. Impact of Preprocedural Anxiety Levels on Pain Perception in Patients Undergoing Office Hysteroscopy. J. Chin. Med. Assoc. 2014, 77, 477–481. [Google Scholar] [CrossRef]
- Carta, G.; Palermo, P.; Marinangeli, F.; Piroli, A.; Necozione, S.; De Lellis, V.; Patacchiola, F. Waiting Time and Pain during Office Hysteroscopy. J. Minim. Invasive Gynecol. 2012, 19, 360–364. [Google Scholar] [CrossRef]
- Vitale, S.G.; Alonso Pacheco, L.; Haimovich, S.; Riemma, G.; De Angelis, M.C.; Carugno, J.; Lasmar, R.B.; Di Spiezio Sardo, A. Pain Management for In-Office Hysteroscopy. A Practical Decalogue for the Operator. J. Gynecol. Obs. Hum. Reprod. 2021, 50, 101976. [Google Scholar] [CrossRef]
- Zhang, X.; Lu, B.; Huang, X.; Xu, H.; Zhou, C.; Lin, J. Innervation of Endometrium and Myometrium in Women with Painful Adenomyosis and Uterine Fibroids. Fertil. Steril. 2010, 94, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Di Spiezio Sardo, A.; Florio, P.; Fernandez, L.M.S.; Guerra, G.; Spinelli, M.; Di Carlo, C.; Filippeschi, M.; Nappi, C. The Potential Role of Endometrial Nerve Fibers in the Pathogenesis of Pain during Endometrial Biopsy at Office Hysteroscopy. Reprod. Sci. 2015, 22, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Yadav, G.; Rao, M.; Gothwal, M.; Singh, P.; Kathuria, P.; Sharma, P.P. Detection of Nerve Fibers in the Eutopic Endometrium of Women with Endometriosis, Uterine Fibroids and Adenomyosis. Obs. Gynecol. Sci. 2021, 64, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Ignaszak-Kaus, N.; Duleba, A.J.; Mrozikiewicz, A.; Kurzawińska, G.; Różycka, A.; Hauke, J.; Gaca, M.; Pawelczyk, L.; Jagodziński, P.P.; Jędrzejczak, P. Relationship of Postoperativ.ve Pain and PONV after Minimally Invasive Surgery with the Serotonin Concentrations and Receptors’ Gene Polymorphisms. J. Pers. Med. 2021, 11, 833. [Google Scholar] [CrossRef]
- de Freitas Fonseca, M.; Sessa, F.V.; Resende, J.A.D.; Guerra, C.G.S.; Andrade, C.M.; Crispi, C.P. Identifying Predictors of Unacceptable Pain at Office Hysteroscopy. J. Minim. Invasive Gynecol. 2014, 21, 586–591. [Google Scholar] [CrossRef]
- Mazzon, I.; Favilli, A.; Grasso, M.; Horvath, S.; Bini, V.; Di Renzo, G.C.; Gerli, S. Pain in Diagnostic Hysteroscopy: A Multivariate Analysis after a Randomized, Controlled Trial. Fertil. Steril. 2014, 102, 1398–1403. [Google Scholar] [CrossRef]
- Neves, A.R.; Mairos, J.; Martino, P.D. How the Location of Intracavitary Lesions Influences Pain during Office Hysteroscopy. J. Minim. Invasive Gynecol. 2019, 26, 1334–1339. [Google Scholar] [CrossRef]
- Pegoraro, A.; Santos, M.E.; Takamori, J.T.; de Carvalho, W.d.A.P.; de Oliveira, R.; Barbosa, C.P.; van Nimwegen, Â. Prevalence and Intensity of Pain during Diagnostic Hysteroscopy in Women Attending an Infertility Clinic: Analysis of 489 Cases. Einstein 2020, 18, eAO4916. [Google Scholar] [CrossRef]
- Akca, A.; Yilmaz, G.; Esmer, A.C.; Yuksel, S.; Koroglu, N.; Cetin, B.A. Use of Video-Based Multimedia Information to Reduce Anxiety before Office Hysteroscopy. Wideochir. Inne. Tech. Maloinwazyjne 2020, 15, 329–336. [Google Scholar] [CrossRef]
- Angioli, R.; De Cicco Nardone, C.; Plotti, F.; Cafà, E.V.; Dugo, N.; Damiani, P.; Ricciardi, R.; Linciano, F.; Terranova, C. Use of Music to Reduce Anxiety during Office Hysteroscopy: Prospective Randomized Trial. J. Minim. Invasive Gynecol. 2014, 21, 454–459. [Google Scholar] [CrossRef]
- Law, H.Y.; Ng, D.Y.T.; Chung, C.D. Use of Music in Reducing Pain during Outpatient Hysteroscopy: Prospective Randomized Trial. J. Obs. Gynaecol. Res. 2021, 47, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Rund, N.M.A.; El Shenoufy, H.; Islam, B.A.; El Husseiny, T.; Nassar, S.A.; Mohsen, R.A.; Alaa, D.; Gad Allah, S.H.; Bakry, A.; Refaat, R.; et al. Determining the Optimal Time Interval between Vaginal Dinoprostone Administration and Diagnostic Office Hysteroscopy in Nulliparous Women: A Randomized, Double-Blind Trial. J. Minim. Invasive Gynecol. 2022, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Hameed, B.H.; Farhan, F.S. A Comparative Clinical Trial of Vaginal Misoprostol versus Intracervical Normal Saline Infiltration as a Cervical Ripening Agent at Time of Hysteroscopy. J. Obs. Gynaecol. Res. 2021, 47, 978–983. [Google Scholar] [CrossRef] [PubMed]
- Issat, T.; Beta, J.; Nowicka, M.A.; Maciejewski, T.; Jakimiuk, A.J. A Randomized, Single Blind, Placebo-Controlled Trial for the Pain Reduction during the Outpatient Hysteroscopy after Ketoprofen or Intravaginal Misoprostol. J. Minim. Invasive Gynecol. 2014, 21, 921–927. [Google Scholar] [CrossRef]
- Gokmen Karasu, A.F.; Aydin, S.; Ates, S.; Takmaz, T.; Comba, C. Administration of Rectal Cytotec versus Rectal Buscopan before Hysteroscopy. Minim. Invasive Allied Technol. 2022, 31, 94–98. [Google Scholar] [CrossRef]
- Haghighi, L.; Najmi, Z.; Rokhgireh, S.; Moradi, Y. Intravaginal Isonicotinic Acid Hydrazide (INH) versus Misoprostol for Cervical Ripening Prior to Hysteroscopy. Obs. Gynecol. Sci. 2020, 63, 514–520. [Google Scholar] [CrossRef]
- Ghamry, N.K.; Samy, A.; Abdelhakim, A.M.; Elgebaly, A.; Ibrahim, S.; Ahmed, A.A.; Abdelbaky, W.H.; Abdallah, K.M.; Badawy, M.A.; Mohammed, A.H.; et al. Evaluation and Ranking of Different Interventions for Pain Relief during Outpatient Hysteroscopy: A Systematic Review and Network Meta-Analysis. J. Obs. Gynaecol. Res. 2020, 46, 807–827. [Google Scholar] [CrossRef]
- Paulo, A.A.S.; Solheiro, M.H.R.; Paulo, C.O.S. Is Pain Better Tolerated with Mini-Hysteroscopy than with Conventional Device? A Systematic Review and Meta-Analysis: Hysteroscopy Scope Size and Pain. Arch. Gynecol. Obs. 2015, 292, 987–994. [Google Scholar] [CrossRef]
- De Silva, P.M.; Stevenson, H.; Smith, P.P.; Clark, T.J. Pain and Operative Technologies Used in Office Hysteroscopy: A Systematic Review of Randomized Controlled Trials. J. Minim. Invasive Gynecol. 2021, 28, 1699–1711. [Google Scholar] [CrossRef]
- Baradwan, S.; Khalil, M.; Alshahrani, M.S.; Albouq, B.; AlSghan, R.; Khadawardi, K.; Mohamed, D.F.; Yousef, D.H.; Kamal, S.H.M.; Abdel Halim, H.W.; et al. Warm Saline Effectiveness for Pain Relief in Office Hysteroscopy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Obs. Gynaecol. Res. 2022, 48, 1523–1530. [Google Scholar] [CrossRef]
- Shahid, A.; Pathak, M.; Gulumser, C.; Parker, S.; Palmer, E.; Saridogan, E. Optimum Uterine Filling Pressure for Outpatient Diagnostic Hysteroscopy: A Double-Blind, Randomized Controlled Trial. Reprod. Biomed. Online 2014, 28, 86–91. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Haggag, H.M.; Hassan, A.M.A. The Impact of Altering Filling Pressures in Diagnostic Outpatient Hysteroscopy on the Procedure Completion Rates and Associated Pain: A Randomised Double-Blind Controlled Trial. Aust. N. Z. J. Obs. Gynaecol. 2016, 56, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Amer-Cuenca, J.J.; Marín-Buck, A.; Vitale, S.G.; La Rosa, V.L.; Caruso, S.; Cianci, A.; Lisón, J.F. Non-Pharmacological Pain Control in Outpatient Hysteroscopies. Minim. Invasive Allied Technol. 2020, 29, 10–19. [Google Scholar] [CrossRef] [PubMed]
- De Silva, P.M.; Stevenson, H.; Smith, P.P.; Justin Clark, T. A Systematic Review of the Effect of Type, Pressure, and Temperature of the Distension Medium on Pain During Office Hysteroscopy. J. Minim. Invasive Gynecol. 2021, 28, 1148–1159.e2. [Google Scholar] [CrossRef]
- Cooper, N.A.M.; Smith, P.; Khan, K.S.; Clark, T.J. A Systematic Review of the Effect of the Distension Medium on Pain during Outpatient Hysteroscopy. Fertil. Steril. 2011, 95, 264–271. [Google Scholar] [CrossRef]
- Craciunas, L.; Sajid, M.S.; Howell, R. Carbon Dioxide versus Normal Saline as Distension Medium for Diagnostic Hysteroscopy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Fertil. Steril. 2013, 100, 1709–1714.e4. [Google Scholar] [CrossRef]
- Souza, C.A.B.; Genro, V.K.; Tarrasconi, D.V.; Oppermann, M.L.R.; Cunha Filho, J.S.L. Diclofenac versus a Combination of Hyoscine and Diclofenac for Outpatient Hysteroscopy: A Placebo Controlled Randomized Clinical Trial. Eur. J. Obs. Gynecol. Reprod. Biol. 2020, 247, 1–5. [Google Scholar] [CrossRef]
- Teran-Alonso, M.J.; De Santiago, J.; Usandizaga, R.; Zapardiel, I. Evaluation of Pain in Office Hysteroscopy with Prior Analgesic Medication: A Prospective Randomized Study. Eur. J. Obs. Gynecol. Reprod. Biol. 2014, 178, 123–127. [Google Scholar] [CrossRef]
- Hassan, A.; Haggag, H. Role of Oral Tramadol 50 Mg in Reducing Pain Associated with Outpatient Hysteroscopy: A Randomised Double-Blind Placebo-Controlled Trial. Aust. N. Z. J. Obs. Gynaecol. 2016, 56, 102–106. [Google Scholar] [CrossRef]
- Mattar, O.M.; Abdalla, A.R.; Shehata, M.S.A.; Ali, A.S.; Sinokrot, M.; Abdelazeim, B.A.; Taher, A.; Samy, A.; Mahmoud, M.; Abbas, A.M. Efficacy and Safety of Tramadol in Pain Relief during Diagnostic Outpatient Hysteroscopy: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Fertil. Steril. 2019, 111, 547–552. [Google Scholar] [CrossRef]
- De Silva, P.M.; Mahmud, A.; Smith, P.P.; Clark, T.J. Analgesia for Office Hysteroscopy: A Systematic Review and Meta-Analysis. J. Minim. Invasive Gynecol. 2020, 27, 1034–1047. [Google Scholar] [CrossRef] [PubMed]
- Keyhan, S.; Munro, M.G. Office diagnostic and operative hysteroscopy using local anesthesia only: An analysis of patient reported pain and other procedural outcomes. J. Minim. Invasive Gynecol. 2014, 21, 791–798. [Google Scholar] [CrossRef] [PubMed]
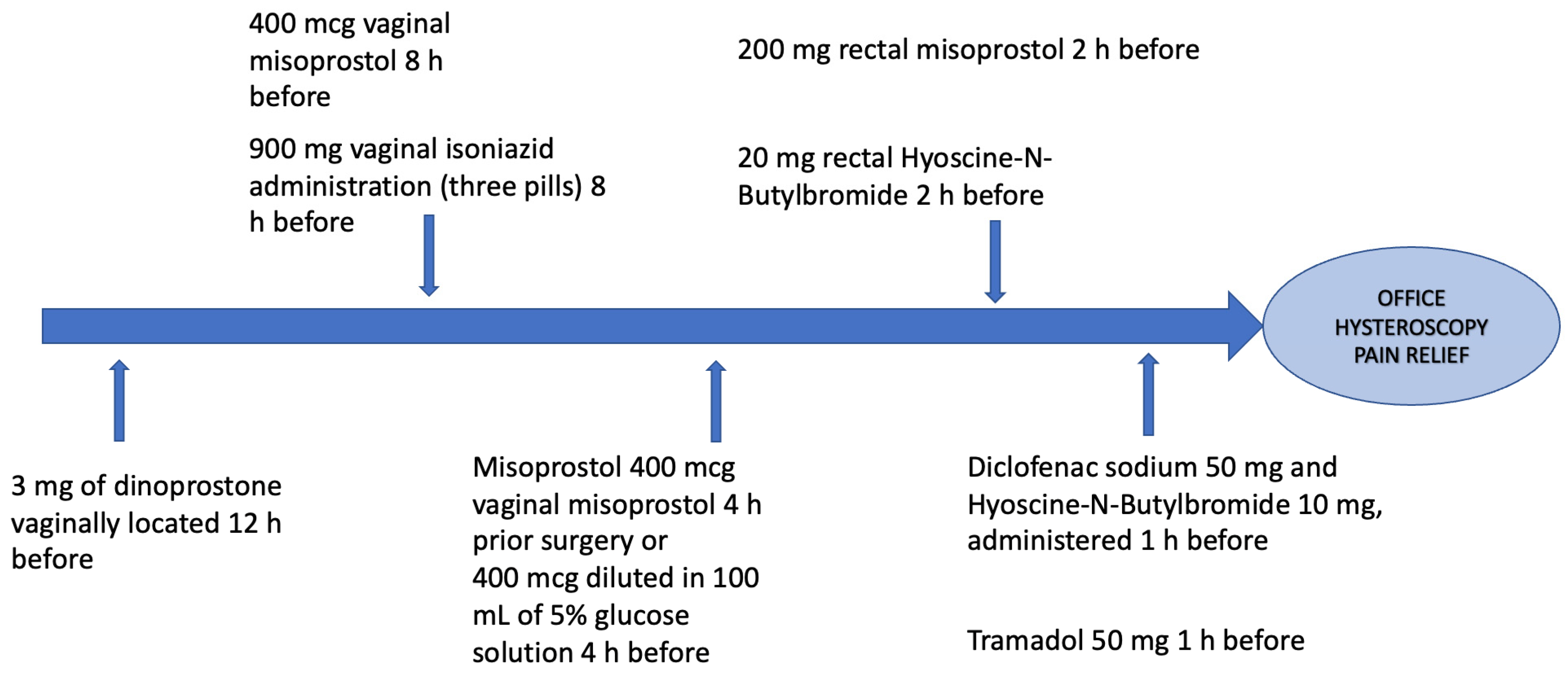
| Study | Drgus(s) | Administration |
|---|---|---|
| Rund et al. [42] | Dinoprostone | 3 mg of dinoprostone vaginally located 12 h before the office hysteroscopic procedure |
| Hameed and Farhan [43] Haghighi et al. [46] Issat et al. [44] Gokmen Karasu et al. [45] | Misoprostol | 400 mcg vaginal misoprostol 4 h prior surgery [43] or 8 h before surgery [46] or 400 mcg diluted in 100 mL of 5% glucose solution 4 h before procedure [44] or 200 mg rectal misoprostol 2 h before the procedure [45] |
| Gokmen Karasu et al. [45] | Hyoscine-n-butyl bromide | 20 mg rectal hyoscine-n-butyl bromide two hours pre-procedure |
| Haghighi et al. [46] | Isonicotinic acid hydrazide | 900 mg of vaginal isoniazid administration (three pills) 8 h before hysteroscopic setting |
| Souza et al. [57] | Hyoscine and diclofenac | Diclofenac sodium 50 mg and Hyoscine-N-Butylbromide 10 mg, administered 1 h before the procedure |
| Hassan and Haggag [59] | Tramadol | 50 mg one hour before outpatient hysteroscopy |
| Study | Parameter | Strategy |
| Carta et al. [29] | Pre-procedural waiting time | Reduction |
| Kokanali et al. [28] | Intra-procedural waiting time | Reduction |
| Akca et al. [39] | Video-based multimedia information | Administration before office hysteroscopy |
| Angioli et al. [40] | Music | Intraprocedural administration |
| Hameed and Farhan [43] | Intracervical saline infiltration | 10 mL of normal saline administered along the cervical circumference divided into about 10 injections avoiding sites located at hours 3 and 9 |
| Shahid et al. [51] Haggag and Hassan [52] | Medium Pressure | The lowest possible for achieving an adequate visualization |
| Craciunas et al. [56] | Type of medium | Normal saline |
| Amer-Cuenca et al. [53] | Transcutaneous electrical nerve stimulation (TENS) | After the procedure |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buzzaccarini, G.; Alonso Pacheco, L.; Vitagliano, A.; Haimovich, S.; Chiantera, V.; Török, P.; Vitale, S.G.; Laganà, A.S.; Carugno, J. Pain Management during Office Hysteroscopy: An Evidence-Based Approach. Medicina 2022, 58, 1132. https://doi.org/10.3390/medicina58081132
Buzzaccarini G, Alonso Pacheco L, Vitagliano A, Haimovich S, Chiantera V, Török P, Vitale SG, Laganà AS, Carugno J. Pain Management during Office Hysteroscopy: An Evidence-Based Approach. Medicina. 2022; 58(8):1132. https://doi.org/10.3390/medicina58081132
Chicago/Turabian StyleBuzzaccarini, Giovanni, Luis Alonso Pacheco, Amerigo Vitagliano, Sergio Haimovich, Vito Chiantera, Péter Török, Salvatore Giovanni Vitale, Antonio Simone Laganà, and Jose Carugno. 2022. "Pain Management during Office Hysteroscopy: An Evidence-Based Approach" Medicina 58, no. 8: 1132. https://doi.org/10.3390/medicina58081132
APA StyleBuzzaccarini, G., Alonso Pacheco, L., Vitagliano, A., Haimovich, S., Chiantera, V., Török, P., Vitale, S. G., Laganà, A. S., & Carugno, J. (2022). Pain Management during Office Hysteroscopy: An Evidence-Based Approach. Medicina, 58(8), 1132. https://doi.org/10.3390/medicina58081132











