4. Discussion
In ancient TCM texts, the terms used to describe diseases related to IHD included “Xin Tong” (heartache), “Xin Jue” (heart syncope), “Zhu Xin Tong” (acute heartache), and “Zhen Xin Tong” (true heartache). In the oldest ancient pharmacopeia “Huangdi Neijing” (The Yellow Emperor’s Inner Canon, published in China, 99-26 B.C.), there are detailed descriptions of IHD: “For the true heartache, if your hands and feet become blue and reach your elbows and knees, the pain is severe. It usually occurs in the morning and fades in the evening, or it occurs in the evening and fades in the morning”. These descriptions of pain in the precordial area were attributed to poor qi and blood flow. In some cases, they mentioned pain in the shoulders and back, shortness of breath and wheezing, and an inability to lie down, all of which fell within the designation of “heartache”. These descriptions are similar to the clinical manifestations of coronary heart disease and angina pectoris.
In Western medicine, most diagnoses of coronary heart disease are based on the results of angiography or computer tomography. Due to the high risk of mortality, treatment often involves highly invasive emergency procedures. TCM is meant to prevent coronary artery obstruction and disease using non-invasive methods [
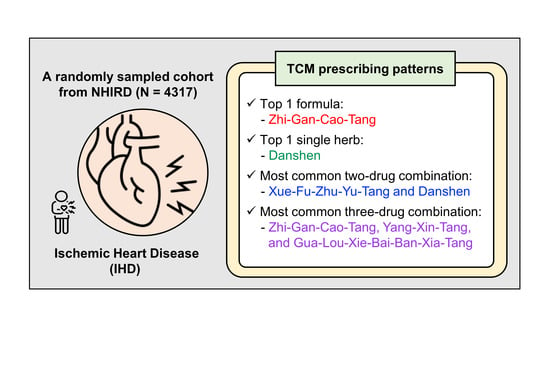
41]. This may also explain why we recorded 22,441 prescriptions for only 4317 subjects during the 18-year study period.
The most frequently prescribed single TCM was Danshen (dried root of
Salvia miltiorrhiza), which possesses a bitter taste and cold nature associated with the heart and liver meridians. It was classified as a top-grade medication in “Shennong Bencao Jing” (Shennong’s Classic of Materia Medica, published in China, 96-31 B.C.) for the treatment of heart and spleen disease, to clear the blood circulation system, relieve irritation, and replenish the Qi. Danshen has also been recommended for the treatment of angina pectoris in “Yi Xue Xiao Jin Zhen” (Medical Golden Needle, published in China, 1916). A number of recent scientific studies have examined the cardioprotective effects of Danshen (in crude form, in specific preparations for injection, or in pill form) [
42]. The constituents from Danshen include lipophilic components (tanshinone IIa and cryptotanshinone) as well as hydrophilic compounds (Sal-A and Sal-B), which have exhibited beneficial effects for the heart due to their anti-inflammatory, anti-oxidant, and anti-apoptotic properties [
43,
44,
45,
46]. Danshen is widely prescribed for the treatment of cardiovascular diseases, such as coronary heart disease, myocardial infarction, atherosclerosis, and angina pectoris [
47,
48,
49,
50].
Another frequently prescribed single TCM was Yujin (
Curcumae Longae Radix), which is the dry root of
Zingiberaceae cultivars, such as
Curcuma wenyujin,
Curcuma kwangsiensis,
Curcuma longa, and
Curcuma phaeocaulis. Yujin also possesses a bitter taste and cold nature associated with the heart, gut, and liver meridians. According to the “Bencao Beiyao” (Essentials of Materia Medica, published in China, 1694), Yujin can cool the heart and blood, disperse stagnation, and normalize the gallbladder to cure jaundice. Clinically, it is often used to treat chest, flank, and abdominal pain induced by Qi stagnation and blood stasis. A number of recent scientific studies have reported that Yujin activates blood flow and mediates blood stasis by inhibiting the aggregation of platelets, slowing the over-activation of the coagulation, and promoting blood circulation [
14]. Curcumin and curcumin-containing extracts of Yujin have also been shown to promote blood circulation, relieve pain, and protect against myocardial ischemia-reperfusion injury by inhibiting lipid peroxidation, augmenting endogenous antioxidants, and improving myocardial metabolism [
15,
51,
52].
Yanhusuo is the dry tuber of
Corydalis yanhusuo, which possesses an acrid-bitter taste and a warm nature associated with the heart, liver, and spleen. Traditionally, Yanhusuo has been used to promote blood circulation, invigorate the qi, and relieve pain. The ancient pharmacopeia “Leigong Paozhi Lun” (Master Lei’s Discourse on Drug Processing, published in China, 5th century) recommended the use of Yanhusuo “to treat dying heartache”. The “Bencao Gangmu” (Compendium of Materia Medica, 1593 A.D.) also reported on the therapeutic effects of Yanhusuo in treating blood and qi stagnation as well as pains throughout the body. Recent scientific studies have extracted alkaloids, such as dextrocorydine, tetrahydropalmatine, and protopine, which have been shown to have potent analgesic and antispasmodic effects on the central nervous system. Another alakaloid, l-Tetrahydropalmatine, exhibited cardioprotective effects against acute global cerebral ischemia-reperfusion injury by activating the PI3K/Akt/eNOS/NO pathway and decreasing the accumulation of inflammatory factors, such as TNF-α and MPO [
23]. Dehydrocorydaline alkaloid has been shown to ameliorate atherosclerosis in ApoE-/-mice via inflammatory inhibition targeting through macrophage p65- and ERK1/2-mediated pathways [
24].
Gegen possesses a flat, sweet taste and has been associated with the Yangming meridian and spleen meridian. Traditionally, it was used to uplift the qi in the stomach, enhance fluid production, and quench the thirst as well as promote sweating and relieve muscles tightness and fever. It has traditionally been used to treat spleen and stomach diseases as well as diarrhea. Recent scientific studies have demonstrated that Gegen can dilate coronary and cerebral blood vessels and increase blood flow. Gegen contains bioactive ingredients (e.g., puerarin) and other flavones and isoflavones, which have been shown to inhibit platelet aggregation and improve the metabolism of the ischemic myocardium [
53,
54]. A number of studies have reported on the cardioprotective potential of puerarin by reducing myocardial oxygen consumption and increasing coronary oxygen supply [
55]. Researchers have also reported that Gegen can reduce the area of myocardial infarction, reduce serum CK-MB activity, and reduce apoptotic cell death [
56]. Isoflavones from Gegen have also been shown to have anti-atherosclerosis effects. For example, daidzin and formononetin can lower serum cholesterol while genistein can lower triglyceride levels [
57]. A number of studies have confirmed that Gegen possesses cardioprotective, neuroprotective, vasodilatation, anti-oxidation, and anti-inflammatory effects. Other studies have demonstrated the effects of Gegen in preventing coagulation, protecting vascular endothelial cells, and preventing damage due to myocardial ischemia. It has even been shown to enhance insulin resistance and lower blood sugar levels. It is widely used in the treatment of cardiovascular disease and type 2 diabetes [
58].
The most popular TCM formula in this study was Zhi-Gan-Cao-Tang, which can be traced back to the ancient pharmacopeia “Shanghan Lun” (Treatise on Cold Pathogenic Diseases, published in China, c.a. 200–210). It has been recommended for the treatment of typhoid fever, pulse congestion, and heart palpitations, owing to the effects on replenishing qi, nourishing yin, and tonifying yang as well as rejuvenating the pulse. The main constituents are from Radix
Glycyrrhizae and Radix
Ginseng, glycyrrhizin and ginsenosides, all of which have been shown to improve the myocardial contractility and cardiac function by inhibiting of Na
+/K
+−ATPase [
29]. They have also been linked to the alleviation of oxidative stress in cardiomyocytes due to toxins or inflammation-associated vascular diseases, such as atherosclerosis [
30,
31].
The second most popular TCM formula in this study was Xue-Fu-Zhu-Yu-Tang, which can be traced back to the pharmacopeia “Yilin Gaicuo” (Correction of Errors in Medical Classics, published in China, 1830). This combination of 11 herbs is used mainly to promote blood circulation and remove blood stasis or as a supplement to soothe the liver or regulate the qi. Clinical applications include the treatment of blood stasis diseases, such as rheumatic heart disease, coronary heart disease, and angina pectoris, as well as chest contusion, intercostal neuralgia, chest pain of costochondritis, and sequelae of concussion. Pharmacological analysis has revealed that Xue-Fu-Zhu-Yu-Tang has anticoagulant and thrombolytic effects, including the dilation of peripheral blood vessels and coronary arteries to promote blood circulation [
59]. In blood stasis and chest pain, Chaihu (
Bupleurum chinense DC./
Bupleurum scorzonerifolium Willd.), Chuanxiong (
Ligusticum chuanxiong Hort.), and Chishao (
Paeonia lactiflora Pall./
Paeonia veitchii Lynch) have been linked to analgesic effects, while Chuanxiong, Chishao, Zhishi (
Citrus aurantium L.), and Gancao (
Glycyrrhiza uralensis Fisch./
Glycyrrhiza inflata Batalin/
Glycyrrhiza glabra L.) have been linked to the alleviation of smooth muscle spasms. Xue-Fu-Zhu-Yu-Tang has been shown to reduce the concentration of triglycerides in serum, decrease the ratio of TXA2/PGI2, and decrease the production of proinflammatory cytokines in rats fed a high cholesterol diet [
32]. Xue-Fu-Zhu-Yu-Tang has also been shown to reverse myocardial fibrosis in hypertensive rats by increasing myocardial cell protection and decreasing TGF-β1 mRNA and protein expression [
60]. In a swine phlegm and blood stasis type coronary heart disease model, Xue-Fu-Zhu-Yu-Tang combined with Gua-Lou-Xie-Bai-Ban-Xia-Tang was shown to have significant protective effects against myocardial apoptosis, upregulate Bcl-2 protein expression, and downregulate Bax, Caspase-3, and Caspase-9 protein expression [
34].
Another famous TCM formula, Sheng-Mai-Yin, can be traced back to the ancient pharmacopeia “Lantai Gueifan” (Lantai Standard, published in China, 1764). This formula, containing Panax ginseng, Ophiopogon japonicus, and Schisandra chinensis, is commonly used to deal with coronary heart disease, angina pectoris, viral myocarditis, heart failure, and other heart diseases. Recent scientific studies have reported that it can also have protective effects on the heart, such as reducing early ventricular contraction and paroxysmal tachycardia, by suppressing the sodium and potassium ATPase pumps of the myocardial cell membrane [
29]. Injections based on Sheng-Mai-Yin have been shown to promote the recovery of cardiac performance in patients who underwent bypass grafting of the coronary artery [
35].
The TCM formula Gua-Lou-Xie-Bai-Ban-Xia-Tang can be traced back to the pharmacopeia “Jingui Yaolue” (Synopsis of Golden Chamber, published in China, c.a. 205). This modification of Gua-Lou-Xie-Bai-Bai-Jiou-Tang through the addition of Banxia (
Pinellia ternata (Thunb.) Makino) is frequently prescribed for IHD. This formula contains the cold bitter Gualouren (
Trichosanthes kirilowii Maxim./
Trichosanthes rosthornii Harms), which is used to reduce phlegm and relieve chest tightness. It also contains the warm smooth Xiebai (
Allium macrostemon Bunge), which is used to promote yang qi and activate the blood. Another constituent, Banxia, is used to reduce dampness, limit phlegm production, and halt vomiting. Gua-Lou-Xie-Bai-Ban-Xia-Tang is meant for coronary heart disease involving qi deficiency, phlegm, and blood stasis and is clinically used for chest obstructive syndrome, such as coronary heart disease angina, intercostal neuralgia, arrhythmia, chest soft tissue injury, intercostal chondritis, and emphysema. Recent scientific evidence suggests that Gua-Lou-Xie-Bai-Ban-Xia-Tang could have cardioprotective effects in ischemia-reperfusion models, including the inhibition of NF-κB and inflammatory cytokines [
36]. It has also been shown to have protective effects against type II diabetes and acute myocardial ischemia by ameliorating oxidative stress and apoptosis via PI3K/Akt/eNOS suppression [
38].
The results of this study could be used as a reference for further in-depth research. Note however that the results of this study in no way attest to the efficacy of these TCMs. Due to the risk of potentially dangerous side effects, these herbs should not be taken without professional consultation or thorough diagnostic procedures. For instance, a few scientific studies have indicated safety concerns for Danshen, such as decreased appetite, abdominal discomfort, convulsions, allergy, and dystonia [
61].
This study was prone to inevitable errors, including inaccurate diagnoses. In many cases, patients with chest or heart discomfort receive a diagnosis of IHD (ICD9 diagnosis code: 410–414 and ICD10 diagnosis code: I20–I25) before undergoing a thorough examination. Or, for patients with IHD, only the other forms of heart disease (ICD9-CM diagnosis code 420–429 and ICD10 diagnosis code: I30–I52), chest pain (ICD9-CM diagnosis code 786.5 and ICD10 diagnosis code: R079), and other chest pain (ICD9-CM diagnosis code 786.59 and ICD10 diagnosis code: R0789) were declared in the NHI database, which also caused the error of case number reducing. Another source of error was the stacking of formulas with single TCMs, which increased the proportion of specific herbs. These errors are difficult to eliminate; however, they do not reduce the credibility of the research, due to the fact that these prescriptions were deemed effective by doctors in terms of medical theory and empirical use. In addition, this study was subject to a number of limitations. Identification of the best TCM formula for a specific patient should be based on careful analysis of all clinical information obtained through the four diagnostic methods (inspection, auscultation/olfaction, inquiry, and palpation) and focusing on the eight principal syndromes (Yin, Yang, outer, inner, cold, heat, deficiency, and actuality). We were unable to collect detailed medical records for each patient, and many IHD patients also underwent modern medical treatments, such that the efficacy of the TCMs could not be assessed objectively. Note also that in Taiwan, many Chinese herbal medicines or health foods containing Chinese herbal ingredients can be purchased directly from TCM pharmacies or drugstores, which makes it impossible to assess the effects of inadvertent drug interactions. For example, the combined use of Warfarin and herbal medicines, such as Danshen and Licorice (the major herb in Zhi-Gan-Cao-Tang), can over-activate the anticoagulant effect and lead to bleeding complications [
62]. Danshen has also been discovered to synergistically cooperate with other herbal medicines (such as Radix
Puerariae lobatae, and Danhong injection), or Western drugs (such as Atorvastatin) in the treatment of cardiovascular diseases [
61].