Deviating from the Recommended Torque on Set Screws Can Reduce the Stability and Fatigue Life of Pedicle Screw Fixation Devices
Abstract
:1. Introduction
2. Materials and Methods
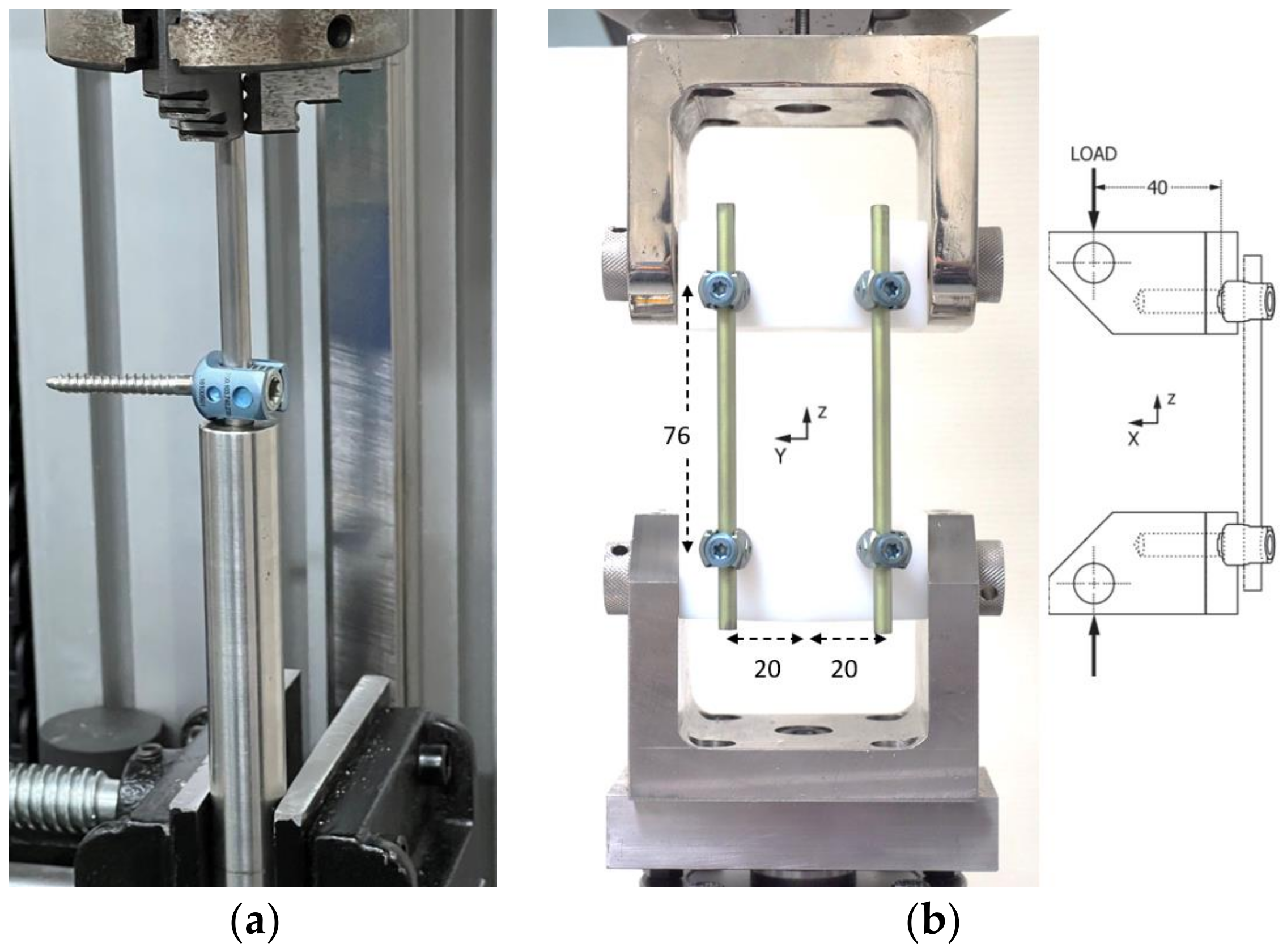
2.1. Axial Gipping Capacity (AGC) Testing
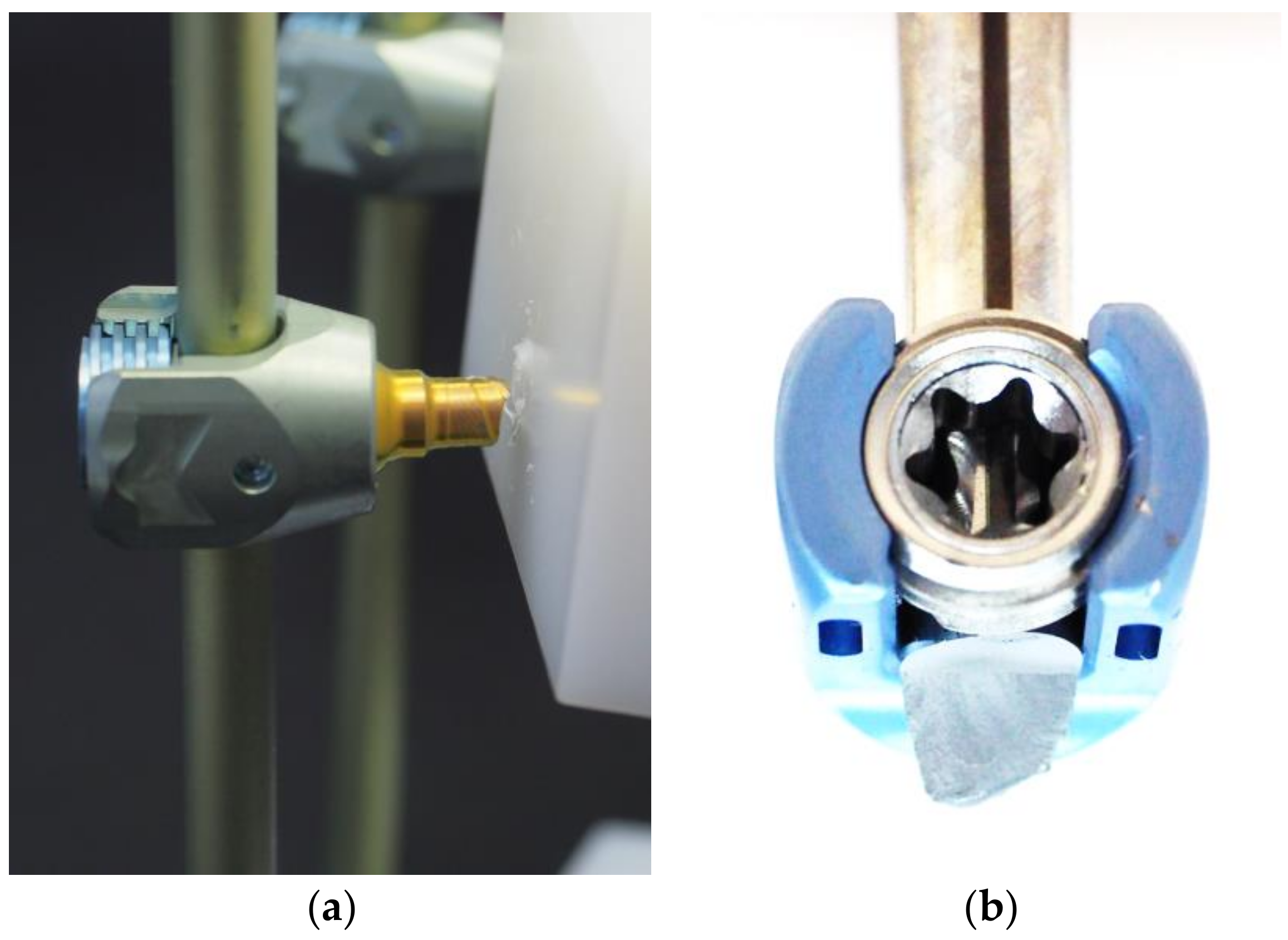
2.2. Dynamic Mechanical Testing of Bilateral Constructs
3. Results
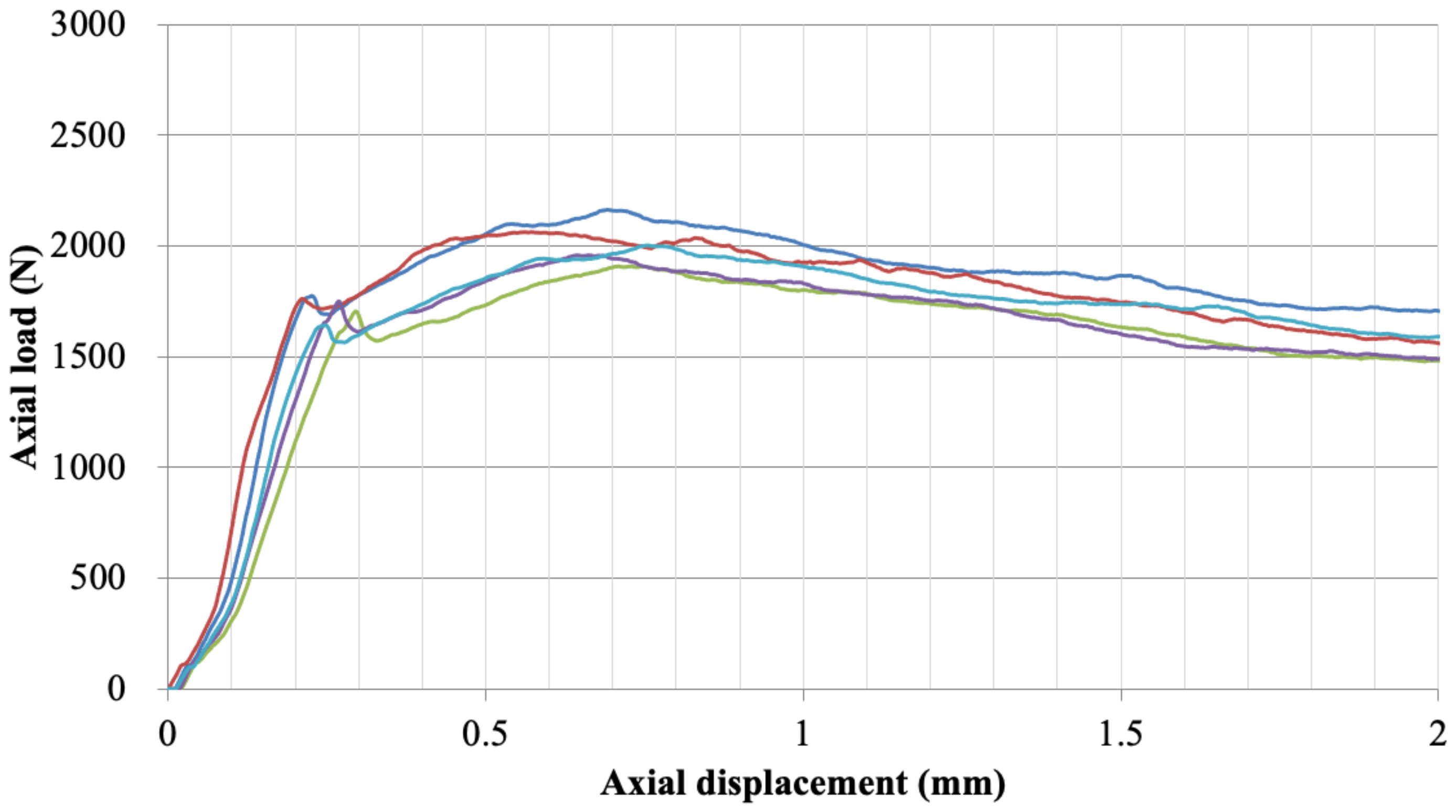
3.1. Axial Gripping Capacity
3.2. Dynamic Mechanical Testing of Bilateral Construct
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Groff, M.W.; Dailey, A.T.; Ghogawala, Z.; Resnick, D.K.; Watters, W.C.; Mummaneni, P.v.; Choudhri, T.F.; Eck, J.C.; Sharan, A.; Wang, J.C.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 12: Pedicle screw fixation as an adjunct to posterolateral fusion. J. Neurosurg. Spine 2014, 21, 75–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boos, N.; Webb, J.K. Pedicle screw fixation in spinal disorders: A European view. Eur. Spine J. 1997, 6, 2–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Landriel, F.; Guiroy, A.; Ciancio, A.M.; Taboada, N.; Menezes, C.; Gotfryd, A.; Kornfeld, S.; Hem, S. 20 tips to avoid and handle problems in the placement of percutaneous pedicle screws. World Neurosurg. 2021, 149, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Lykissas, M.G.; Giannoulis, D. Minimally invasive spine surgery for degenerative spine disease and deformity correction: A literature review. Ann. Transl. Med. 2018, 6, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, P.; Kumar, V.; John, R.; Sharma, R. Early loosening of spinal rod in a case of degenerative grade 1 spondylolisthesis treated with unilateral pedicle screw fixation and transforaminal cage for interbody fusion. J. Orthop. Case Rep. 2017, 7, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A. Improper coupling between inner nut and screw head leading to rod loosening and dislodgement. Rom. Neurosurg. 2014, 21, 245–246. [Google Scholar] [CrossRef]
- Krishnan, P.; Das, S. Implant disassembly due to pedicle screw nut loosening. J. Neurosci. Rural. Pract. 2021, 12, 813–814. [Google Scholar] [CrossRef]
- Vallee, M.C.; Conrad, H.J.; Basu, S.; Seong, W.J. Accuracy of friction-style and spring-style mechanical torque limiting devices for dental implants. J. Prosthet. Dent. 2008, 100, 86–92. [Google Scholar] [CrossRef]
- Jaarda, M.J.; Razzoog, M.E.; Gratton, D.G. Effect of preload torque on the ultimate tensile strength of implant prosthetic retaining screws. Implant. Dent. 1994, 3, 17–21. [Google Scholar] [CrossRef]
- Neiburger, E.J. Dentists’ age and manual dexterity. Are younger or older dentists better practitioners? Gen. Dent. 1994, 42, 88–90. [Google Scholar]
- Serhan, H.; Hammerberg, K.; O’Neil, M.; Sturm, P.; Mardjetko, S.; Crawford, A. Intraoperative techniques to reduce the potential of set-screw loosening in long spinal constructs: A static and fatigue biomechanical investigation. J. Spinal. Disord. Tech. 2010, 23, e31–e36. [Google Scholar] [CrossRef] [PubMed]
- Standard Test Method for Evaluating the Static and Fatigue Properties of Interconnection Mechanisms and Subassemblies Used in Spinal Arthrodesis Implants. Available online: https://www.astm.org/f1798-21.html (accessed on 29 March 2022).
- Standard Test Methods for Spinal Implant Constructs in a Vertebrectomy Model. Available online: https://www.astm.org/f1717-21.html (accessed on 29 March 2022).
- Kluck, D.G.; Farnsworth, C.L.; Jeffords, M.E.; Marino, N.E.; Yaszay, B.; Upasani, V.v.; Newton, P.O. Spinal rod gripping capacity: How do 5.5/6.0-mm dual-diameter screws compare? Spine Deform. 2020, 8, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Al-Otaibi, H.N. Intended and achieved torque of implant abutment’s screw using manual wrenches in simulated clinical setting. J. Contemp. Dent. Pract. 2016, 17, 897–901. [Google Scholar] [CrossRef] [PubMed]
- Zdeblick, T.A.; Kunz, D.N.; Cooke, M.E.; McCabe, R. Pedicle screw pullout strength. correlation with insertional torque. Spine 1993, 18, 1673–1676. [Google Scholar] [CrossRef]
- Okuyama, K.; Abe, E.; Suzuki, T.; Tamura, Y.; Chiba, M.; Sato, K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine 2000, 25, 858–864. [Google Scholar] [CrossRef]
- Voleti, P.B.; Shen, F.H.; Arlet, V. Failure of monoaxial pedicle screws at the distal end of scoliosis constructs: A case series. Spine Deform. 2014, 2, 110–121. [Google Scholar] [CrossRef]
- Liu, P.Y.; Lai, P.L.; Lin, C.L. A Biomechanical investigation of the retentive force of pedicle screw structures for different screw tulip designs. Clin. Biomech. 2019, 70, 23–30. [Google Scholar] [CrossRef]
- Ardura, F.; Chenaux, D.; Pascal-Moussellard, H.; Hessmann, M.H. Evaluation of the reduction, tightening and gripping performance of an innovative set screw technology for instrumented posterior lumbar fusion: A biomechanical study. Orthop. Traumatol. Surg. Res. 2021, 107, 102918. [Google Scholar] [CrossRef]
- Jutte, P.C.; Castelein, R.M. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur. Spine J. 2002, 11, 594–598. [Google Scholar] [CrossRef]
- Esses, S.I.; Sachs, B.L.; Dreyzin, V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine 1993, 18, 2231–2239. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lanman, T.H.; Higgs, G.; MacDonald, D.W.; Berven, S.H.; Isaza, J.E.; Phillips, E.; Steinbeck, M.J. Retrieval analysis of PEEK rods for posterior fusion and motion preservation. Eur. Spine J. 2013, 22, 2752–2759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, T.; Chen, K.; Lv, Y.; Yang, T.; Chen, K.; Lv, Y. Fatigue life analysis of fixed structure of posterior thoracolumbar pedicle screw. Engineering 2013, 5, 292–296. [Google Scholar] [CrossRef] [Green Version]
- La Barbera, L.; Galbusera, F.; Wilke, H.J.; Villa, T. Preclinical evaluation of posterior spine stabilization devices: Can the current standards represent basic everyday life activities? Eur. Spine J. 2016, 25, 2909–2918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
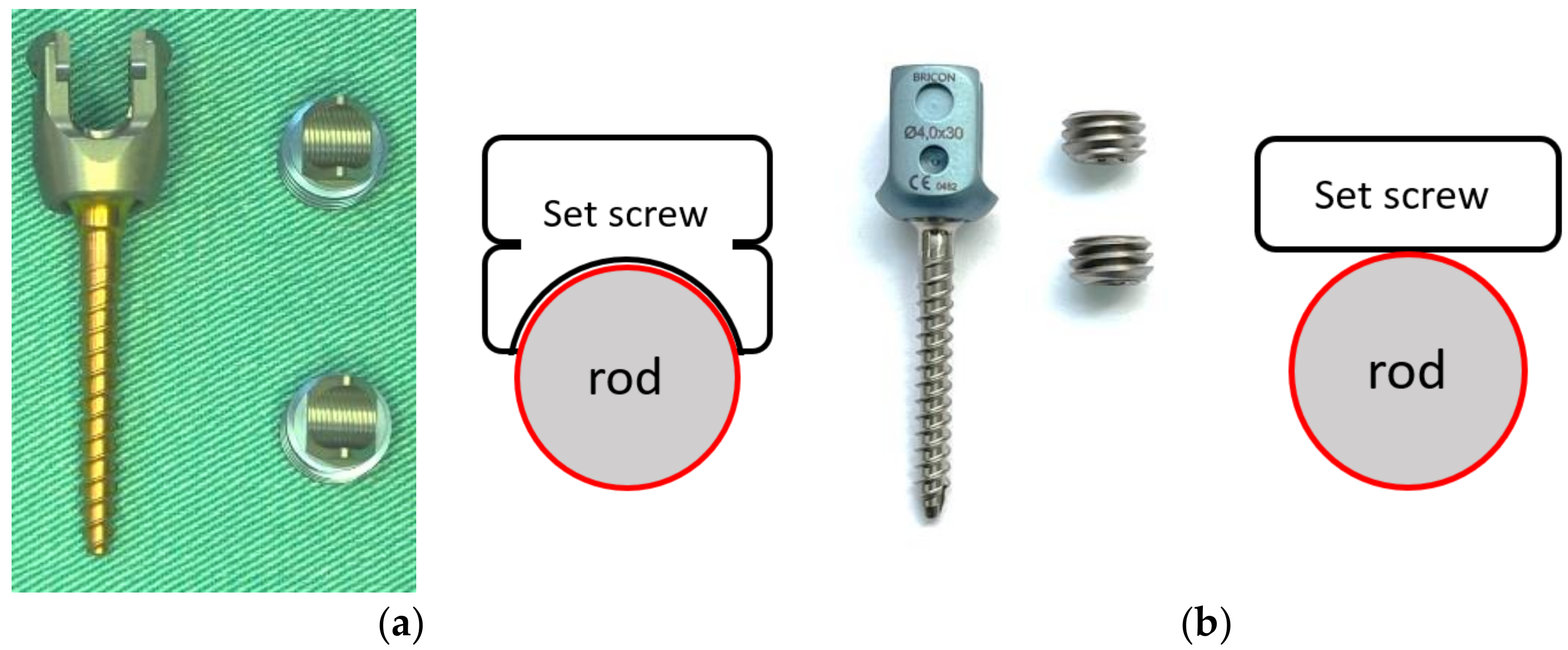
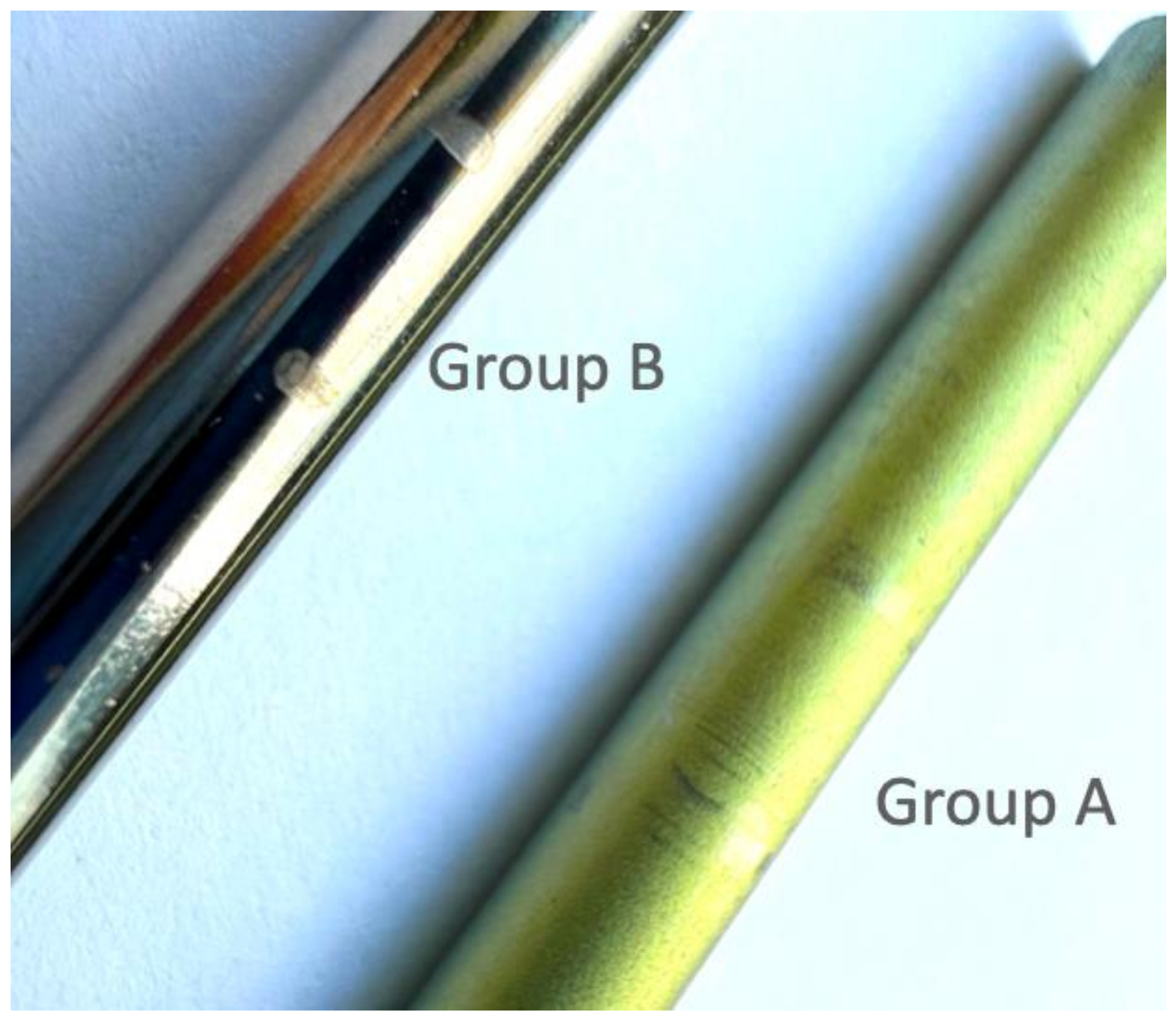
| Pedicle Screw | A (Matrix) * | B (OCTOPODA) ** |
|---|---|---|
| Rod material | Ti alloy | Ti alloy |
| Screw diameter (mm) | 4.0 | 4.0 |
| Screw length (mm) | 30 | 30 |
| Screw material | Ti alloy | Ti alloy |
| Set screw material | Ti alloy | Ti alloy |
| Tightening torque (Nm) | 9 (lower) 10 (Manufacturer recommended) 11 (higher) | 11 (lower) 12 (Manufacturer recommended) 13 (higher) |
| Group (Torque Value of Set Screw) | Mean | SD * | p Value ** |
|---|---|---|---|
| A (9 Nm) | 1940.23 | 102.10 | 0.123 compared to A (10 Nm) |
| A (10 Nm) | 2019.65 | 98.81 | - |
| A (11 Nm) | 2067.30 | 105.66 | 0.241 compared to A (10 Nm) |
| B (11 Nm) | 1651.23 | 88.05 | 0.031 |
| B (12 Nm) | 1775.70 | 94.78 | - |
| B (13 Nm) | 1818.97 | 69.25 | 0.216 |
| Sample No. Group A | Torque Value of Set Screw (Nm) | Range of Axial Force (N) | Cycles to Failure |
|---|---|---|---|
| 1 | 10 | 22~220 | 53,548 |
| 2 | 10 | 20~200 | 2,177,963 |
| 3 | 10 | 20~200 | 1,757,238 |
| 4 | 10 | 19~190 | Run-out |
| 5 | 10 | 19~190 | Run-out |
| 6 | 9 | 19~190 | Run-out |
| 7 | 9 | 19~190 | Run-out |
| 8 | 11 | 19~190 | Run-out |
| 9 | 11 | 19~190 | Run-out |
| 10 | 11 | 20~200 | 1,831,177 |
| 11 | 11 | 20~200 | 1,593,474 |
| Group (Torque Value of Set Screw) | * Fatigue Strength (N) | Maximum Axial Force (N) | Failure Patten If Did Not Run-Out |
|---|---|---|---|
| A (9 Nm) | 190 | 22~220 | Screw fracture |
| A (10 Nm) | |||
| A (11 Nm) | |||
| B (11 Nm) | 190 | 22~220 | Rod fracture |
| B (12 Nm) | |||
| B (13 Nm) | 170 | 19~190 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, L.-C.; Hsieh, Y.-Y.; Tsuang, F.-Y.; Chiang, Y.-F.; Chiang, C.-J. Deviating from the Recommended Torque on Set Screws Can Reduce the Stability and Fatigue Life of Pedicle Screw Fixation Devices. Medicina 2022, 58, 808. https://doi.org/10.3390/medicina58060808
Wu L-C, Hsieh Y-Y, Tsuang F-Y, Chiang Y-F, Chiang C-J. Deviating from the Recommended Torque on Set Screws Can Reduce the Stability and Fatigue Life of Pedicle Screw Fixation Devices. Medicina. 2022; 58(6):808. https://doi.org/10.3390/medicina58060808
Chicago/Turabian StyleWu, Lien-Chen, Yueh-Ying Hsieh, Fon-Yih Tsuang, Yueh-Feng Chiang, and Chang-Jung Chiang. 2022. "Deviating from the Recommended Torque on Set Screws Can Reduce the Stability and Fatigue Life of Pedicle Screw Fixation Devices" Medicina 58, no. 6: 808. https://doi.org/10.3390/medicina58060808
APA StyleWu, L.-C., Hsieh, Y.-Y., Tsuang, F.-Y., Chiang, Y.-F., & Chiang, C.-J. (2022). Deviating from the Recommended Torque on Set Screws Can Reduce the Stability and Fatigue Life of Pedicle Screw Fixation Devices. Medicina, 58(6), 808. https://doi.org/10.3390/medicina58060808






