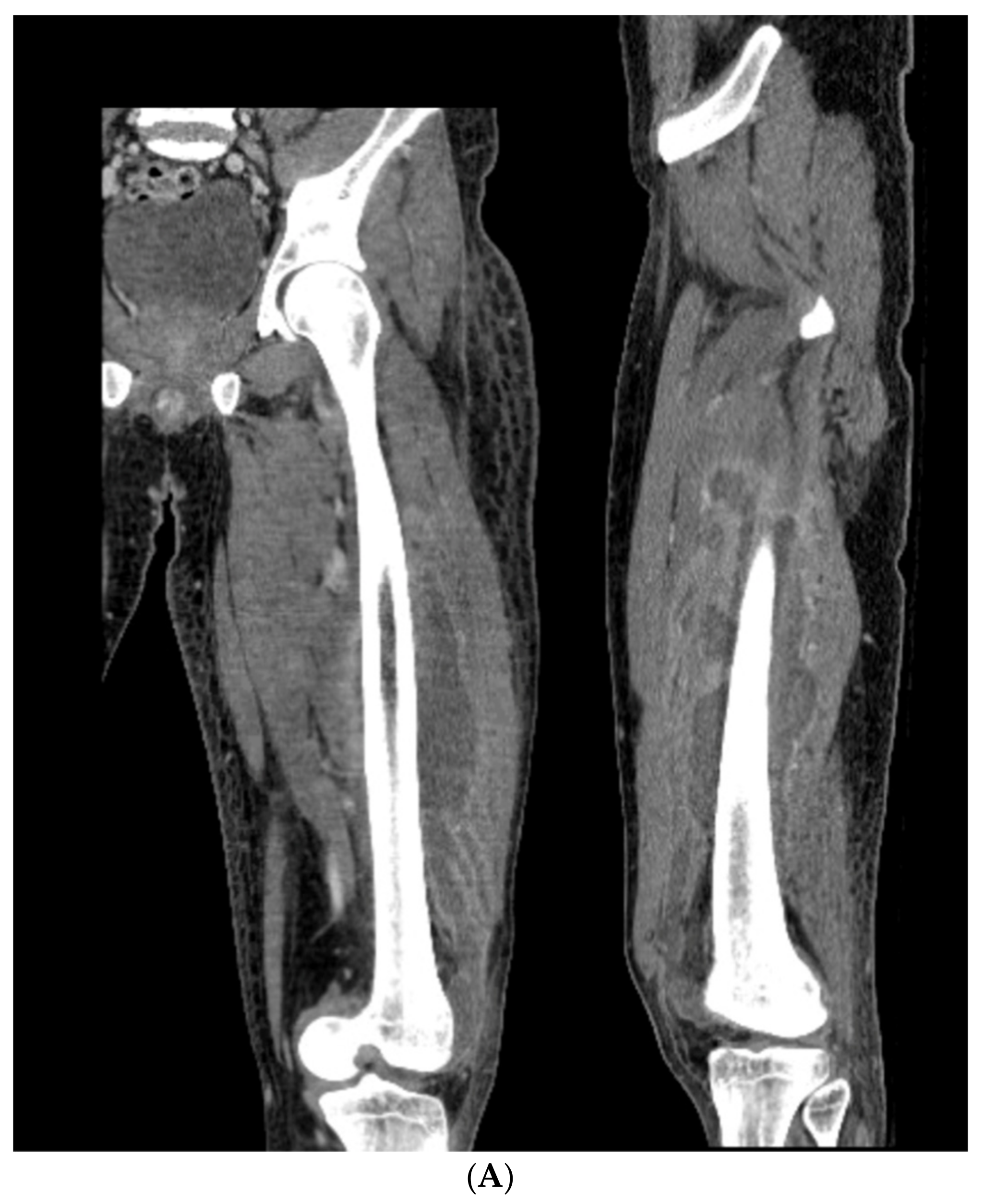
2.1. Preoperative: Physical Examination and Soft Tissue Envelope
A standard orthopedic exam for lower extremity deformity complaints will also include a gait analysis, as well as a range of motion assessment of both lower extremities. Attention to joint contracture as a cause of deformity should be noted and, if possible, addressed as part of the overall deformity correction. When moving attention specifically to the area of deformity, local and systemic factors inform the surgeon’s determination of a patient as a favorable host for this procedure [
7]. Soft tissue deformity accompanies all bony deformities. The more chronic in nature the malunion is, the stiffer the soft tissues become. Periosteal, fascial, and tendon structures become more fibrous, muscles atrophy, and correction of an angular deformity results in the elongation of soft tissue on one side of the deformity with shortening on the other side of the deformity. It is essential to determine whether this type of correction can even be considered with or without the aid of additional soft tissue releases. The tibia is particularly unforgiving on the medial side, and with the propensity for the limb to drift into varus, this is unfortunately the more common location for the concave side of a tibial misalignment. The ‘structure at risk’ concept as taught in distraction osteogenesis techniques is worth considering in acute corrections as well [
8]. Neurovascular and other soft tissue structures can be compromised not just with surgical exposure but also with the correction. In addition to typical comorbidities such as vascular disease and diabetes, a patient’s other risks should be acknowledged in order to stratify the patient as a surgical candidate. Nutritional and metabolic assessments and smoking status should be considered. Medications such as blood thinners, steroids, or immune suppression drugs require the surgeon to pause to consider their potential interactions, as does illicit drug use. Careful examination of the patient must include an assessment of prior incisions, prior flaps, skin grafts, and function of the limb proximal and distal to the deformity. Realizing that the approach required for this osteotomy requires a wide surgical exposure, significantly more so than a percutaneous transverse osteotomy, the surgeon must assume there will be influence from the patient’s comorbidities upon the procedure. Hence, the surgeon should preoperatively identify the potential complications and which options remain for salvage of the correction should the need arise after osteotomy. If the ‘worst case scenario’ for a wound complication is expected, a flap should be performed at the time of or immediately after surgery. For example, a varus tibia malunion with adherent skin over a previously granulated wound at the location of the osteotomy should be addressed in this fashion. Densely adherent wounds directly in the path of the exposure or correction should not be subject to this open approach without soft tissue contingency plans. The surgeon must counsel the patient of this prior to surgery, especially that these complications could occur remote to the time of osteotomy. The surgeon should either be facile with the required soft tissue technique or have immediately available someone who can provide this care. Without this approach, acute correction with a focal dome should not be attempted.
2.2. Preoperative: Deformity Analysis
Once a patient’s soft tissue is deemed appropriate for an acute focal dome osteotomy, the deformity analysis ensues.
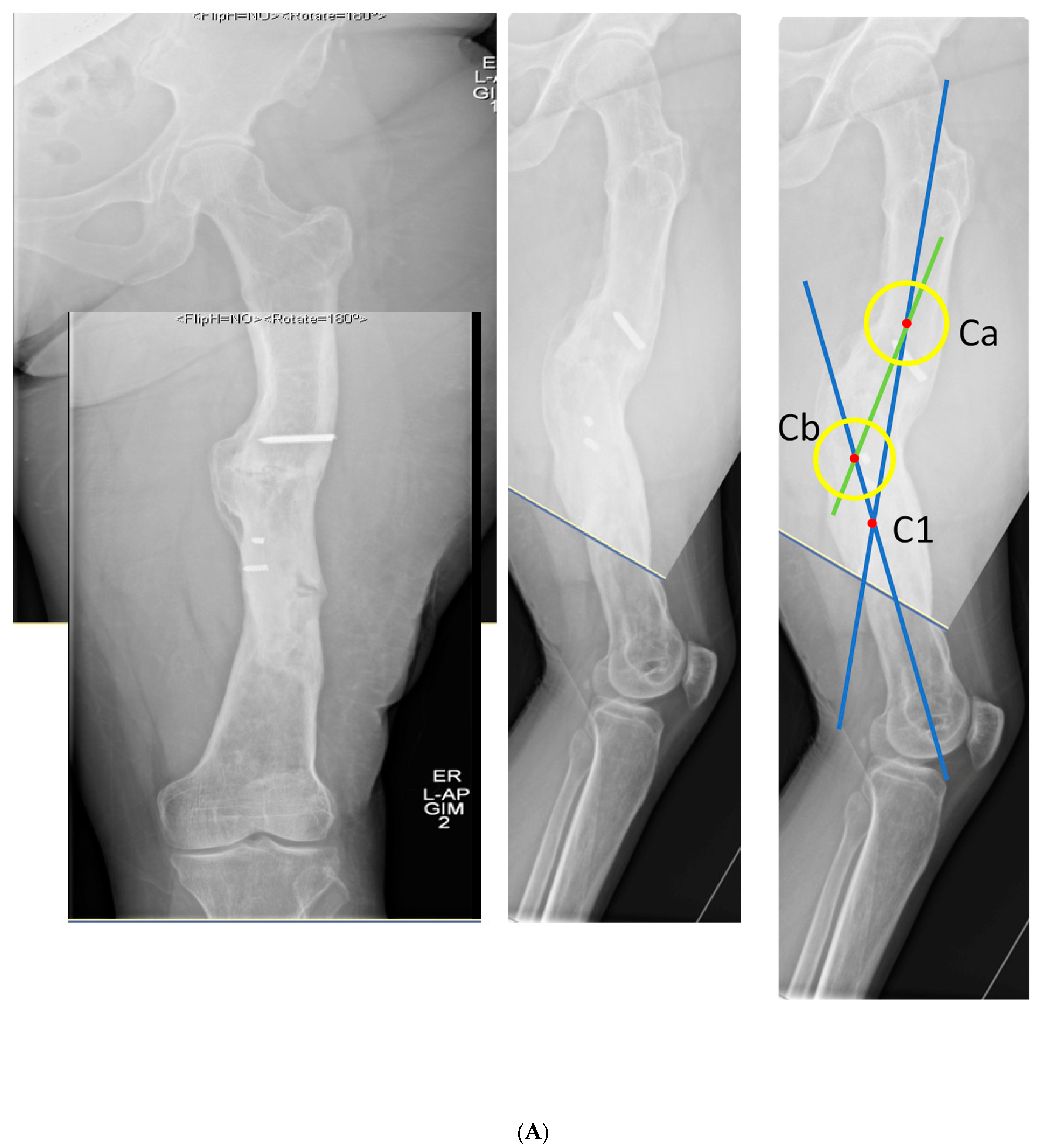
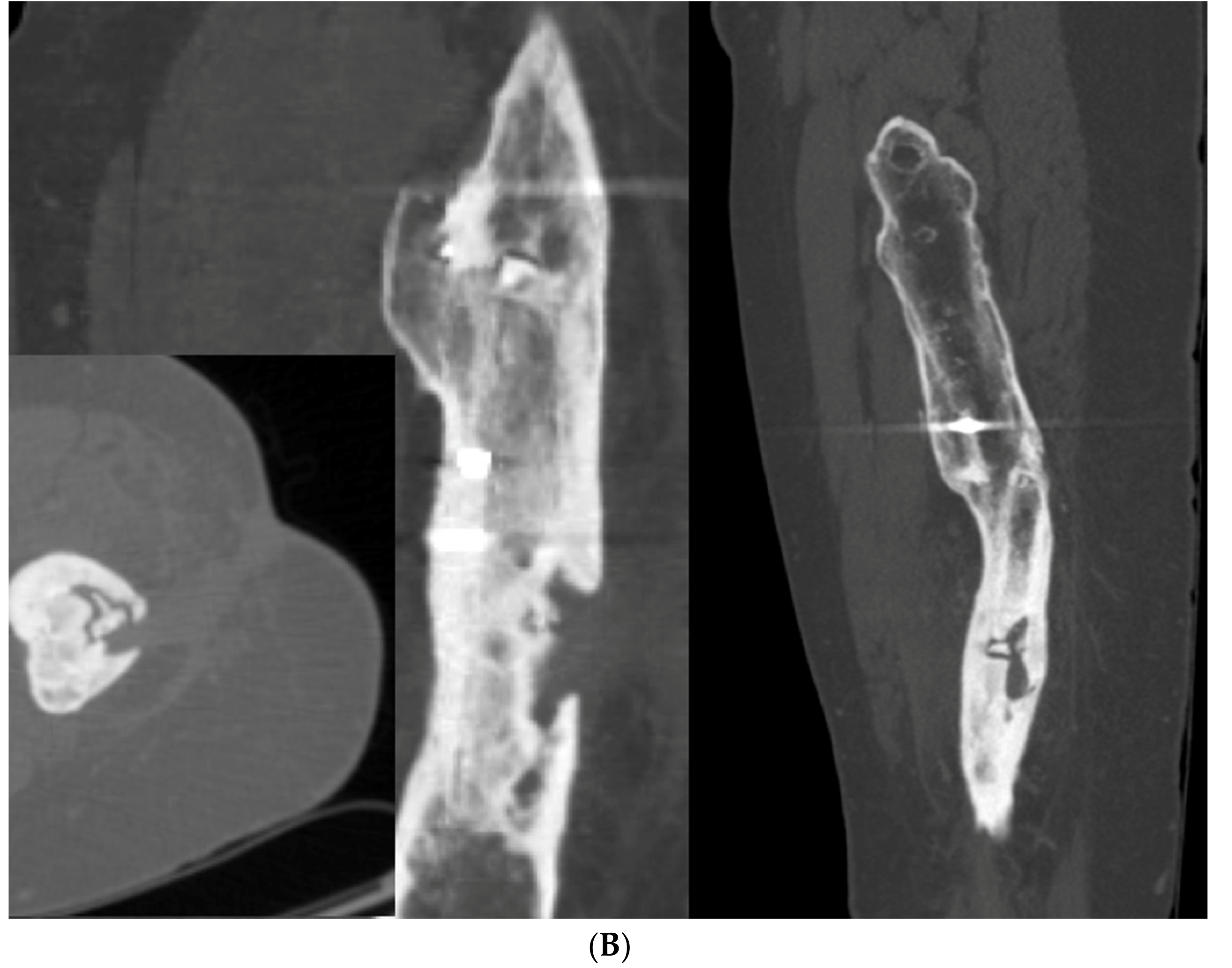
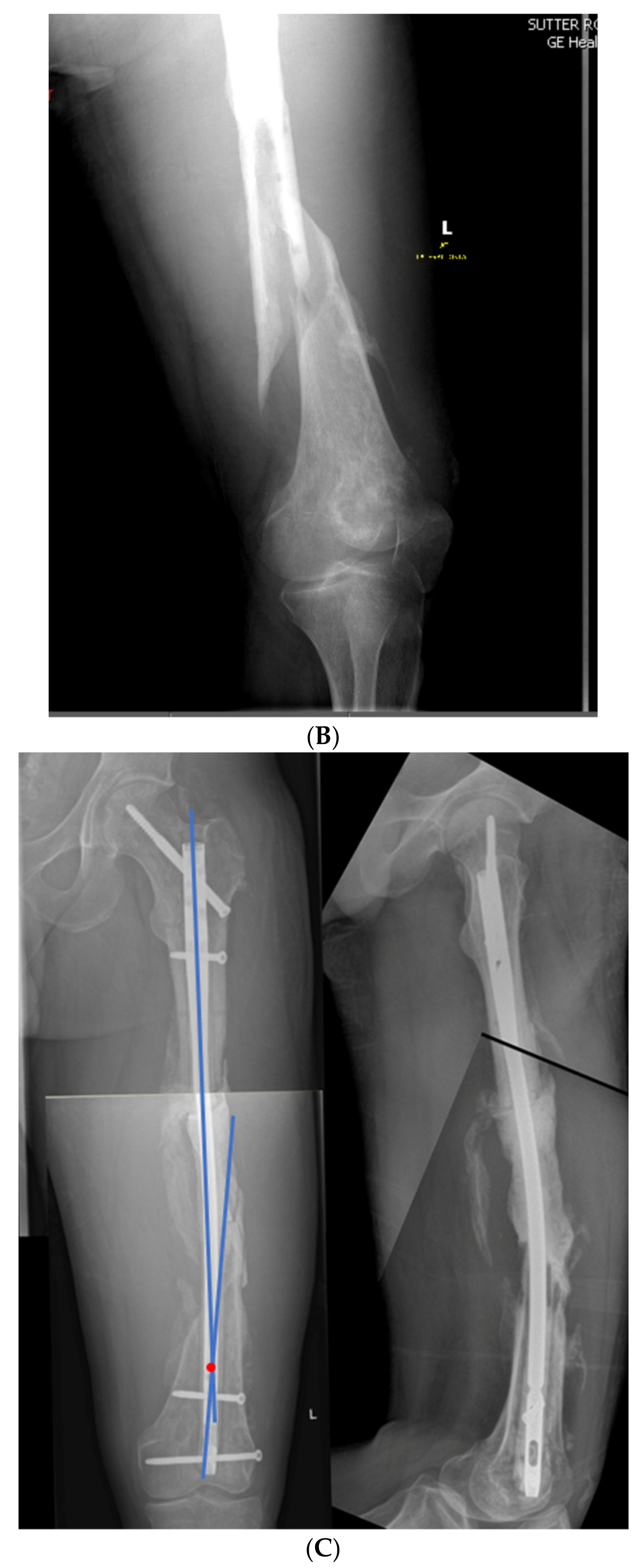
An ideal patient workup includes standing full-length anteroposterior and lateral projection X-rays. These allow the assessment of anatomic and mechanical axes. Leg length should be corrected with blocks to level the pelvis and knees oriented patella forward. When the patient with a deformity also has joint contracture, additional radiographs are obtained that are orthogonal to each bone (i.e., true AP of each femur and tibia). While the initial deformity analysis is done using mechanical axis deviation, once the deformity is identified as diaphyseal, the CORA method, as described by Paley, is used to characterize the deformity within the anatomical axis [
2]. A physical examination is conducted simultaneously to corroborate the deformity, leg length inequality, and rotational deformity. Again, it is important to note that the focal dome osteotomy does not address rotational deformity. If the patient has a rotational deformity in addition to their angular deformity, a true dome osteotomy can accommodate both angular and rotational deformities, though, with the current instrumentation, this may be more practically handled with other osteotomies such as a wedge osteotomy, a mathematically derived single-cut osteotomy, or a clamshell osteotomy [
6].
Understanding the deformity in the coronal and sagittal planes allows the surgeon to determine the true plane of an angular deformity. This should not be considered a multiplane deformity solely because it is present in both coronal and sagittal planes; there will be a single plane that is between the coronal and sagittal planes that will encompass the entire deformity, and orthogonal to this true deformity plane, there will be no deformity. This is considered the ‘no deformity view’.
The calculation of the true deformity and no deformity planes can easily be achieved. Once the coronal and sagittal plane deformity angles are determined, each of these values in the coronal and sagittal planes are plotted on an XY graph, as seen in
Figure 2. The hypotenuse of the triangle that is created with the coronal and sagittal magnitudes is the maximum deformity in degrees. The position of this maximum deformity is also obtained from this same graphical representation. The angle that is made between either the coronal or sagittal plane is the actual plane of deformity that exists between those planes. Perpendicular to this maximum deformity plane is where the no deformity plane will be found.
Once this true plane of deformity is determined, it is correlated with a physical examination where the true deformity can be confirmed. The maximum plane of the deformity must be surgically accessible. For example, if the patient has a pure coronal plane deformity, the surgical access to this deformity would be directly anterior or directly posterior in order to perform a focal dome osteotomy. If the plane is purely in the sagittal plane, access to the deformity would be directly medial or directly lateral. The surgeon knows that a direct posterior or direct lateral approach to the mid-tibia may not be physiologically possible without likely injury to the surrounding structures. When the true deformity is somewhere between the coronal and sagittal planes, the surgeon must associate this with the patient’s soft tissue envelope to determine if the trajectory of the osteotomy is possible. Once soft tissue feasibility is confirmed, the surgeon can continue to plan the osteotomy. If the ideal location of a focal dome osteotomy cannot be safely accessed, the surgeon must consider another form of correction.
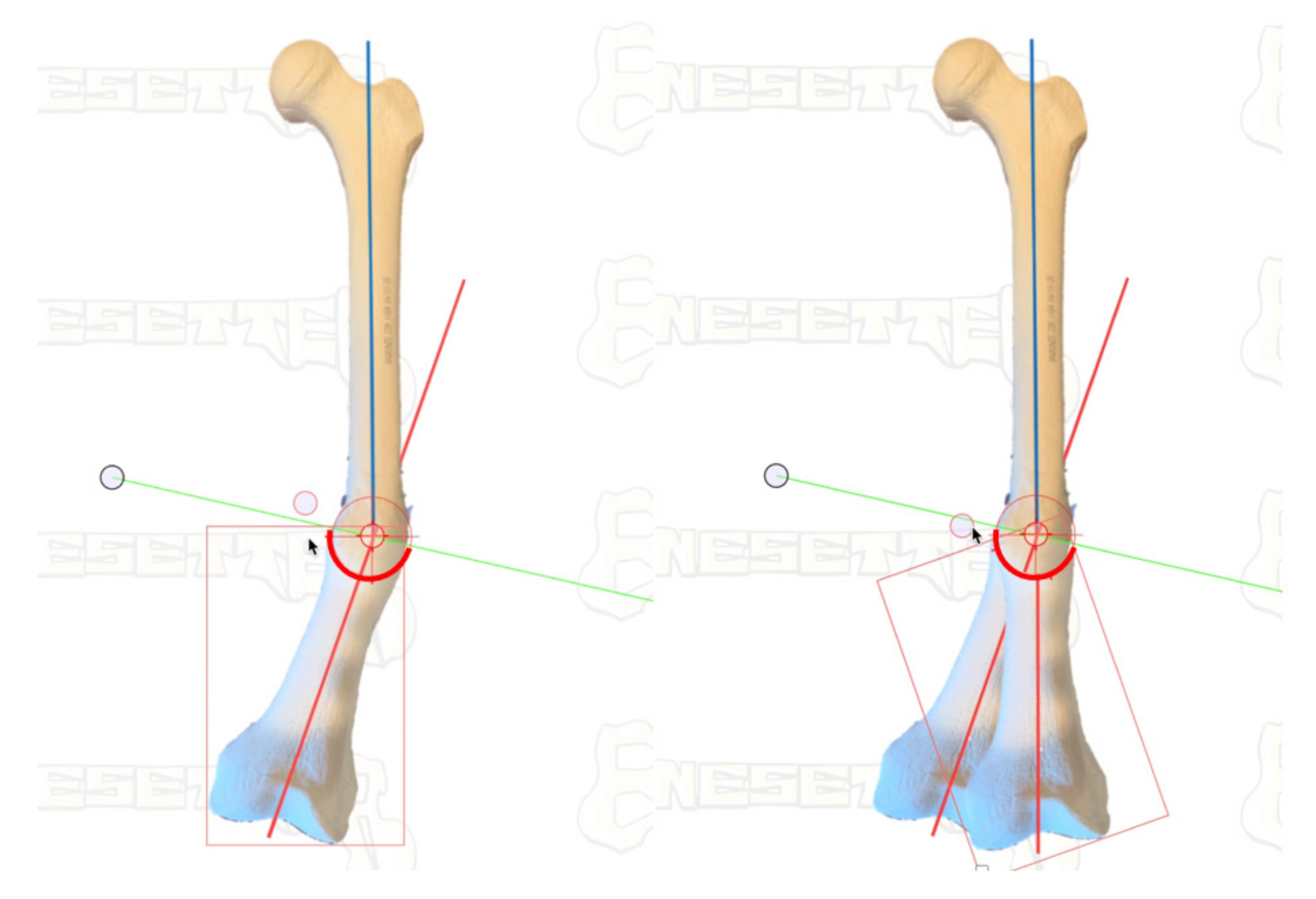
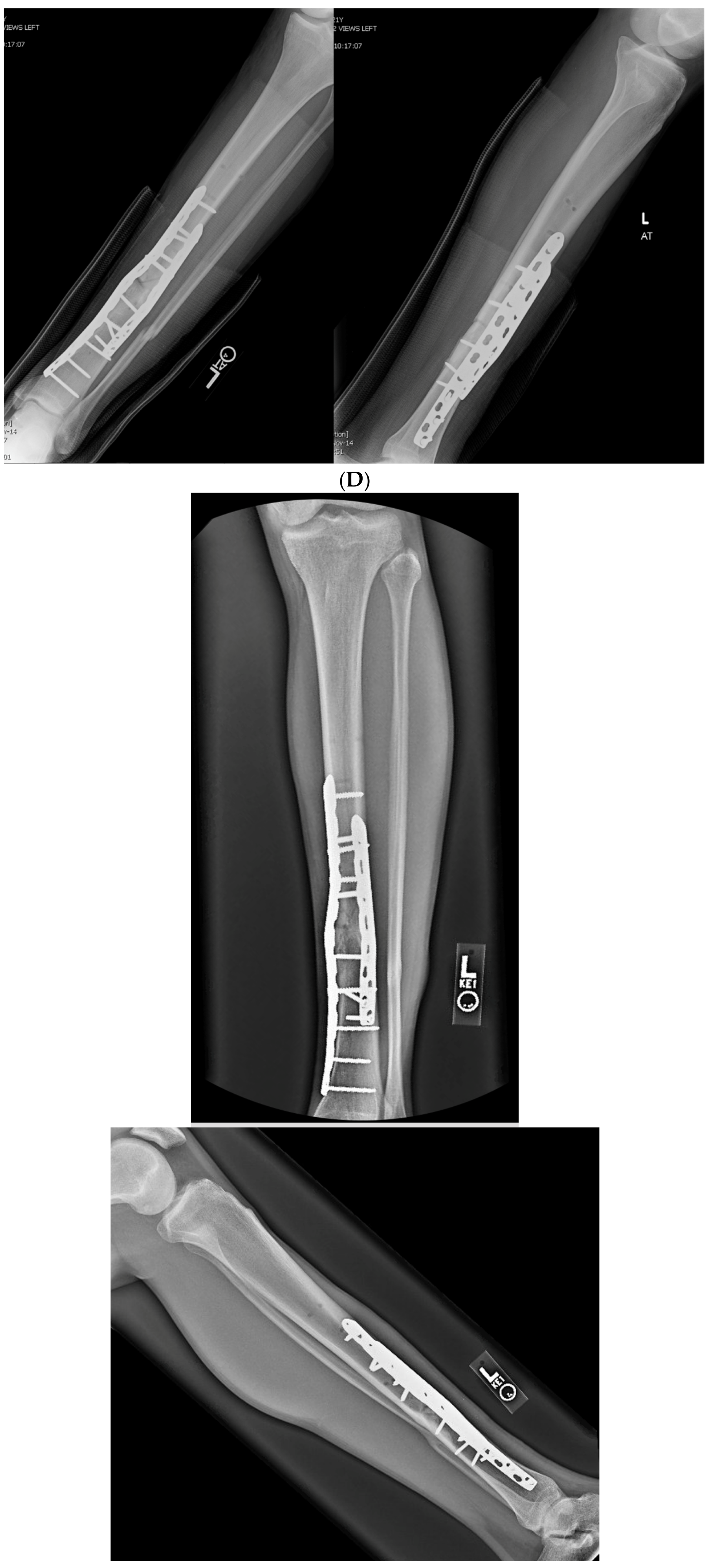
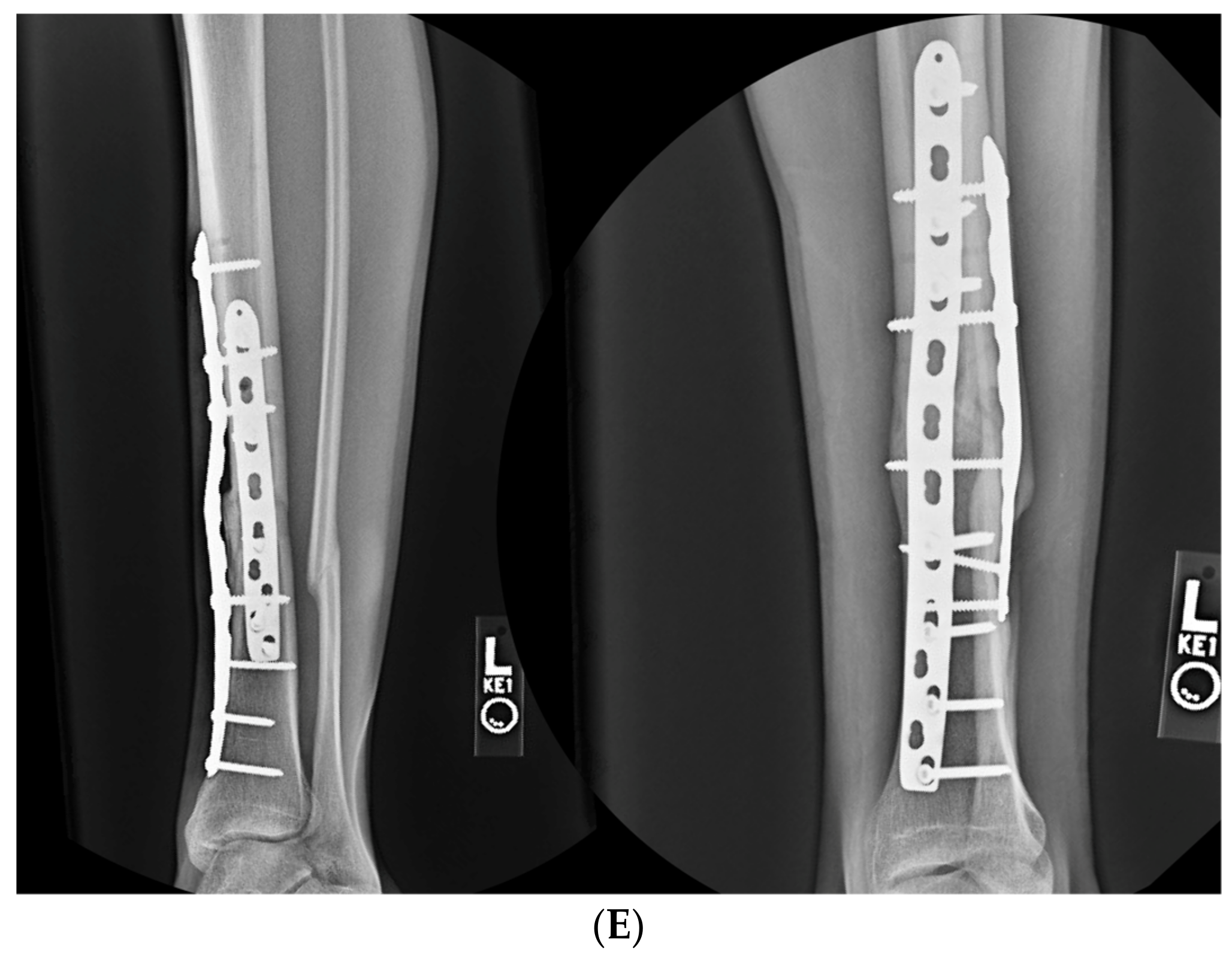
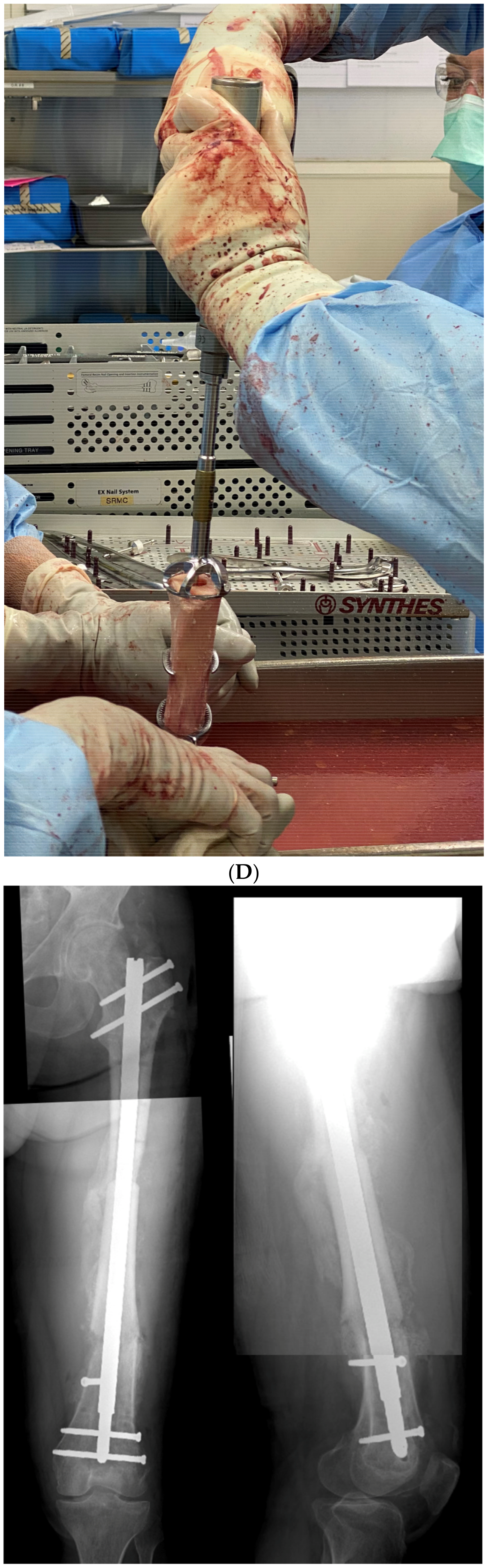
The focal dome osteotomy can be performed in one of several ways. In hard diaphyseal bone, multiple parallel drill holes can be drilled along an arc constrained by a radius at the center of rotation of angulation (CORA), obtained from preoperative planning. In softer metaphyseal bone, commercially available curved saw blades will reliably perform the focal dome osteotomy (Depuy-Synthes, West Chester, PA, USA). These saw blades do not perform well in cortical bone, as they generate heat with their fine, shallow teeth.
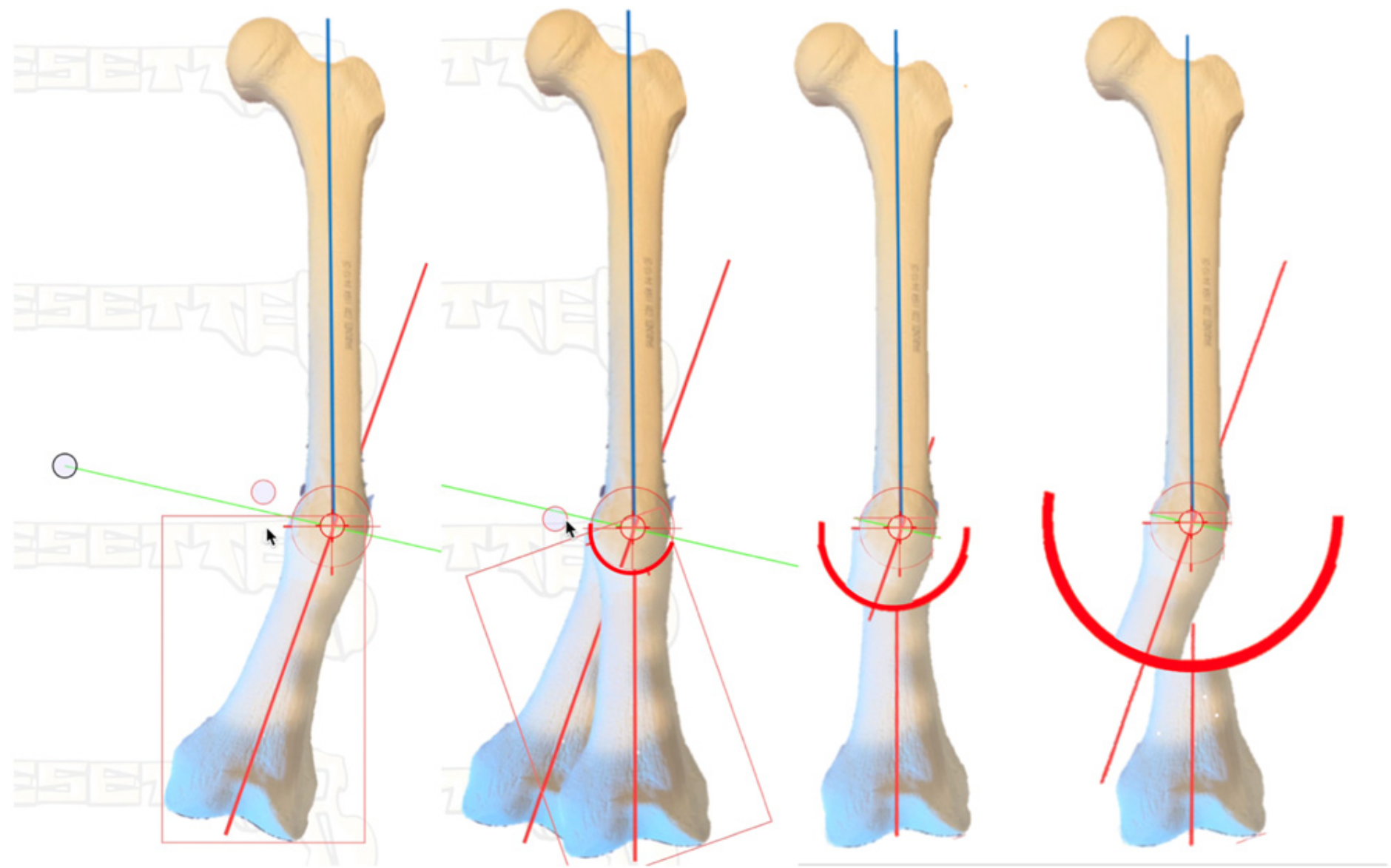
Figure 3 demonstrates a safe method in cortical bone. The CORA is identified from preoperative planning using the previously determined plane and magnitude of maximum deformity. At the center of the CORA, a drill bit is placed. Based on the diameter of the bone in this location, as well as the magnitude of deformity, the radius of the curvature is chosen. With pure angulation deformities (no translation), the optimum radius is the smallest radius that also accommodates the width of the bone at that level; the closer the osteotomy is to the CORA, the more options are available for internal fixation. When the radius is elongated, this brings the osteotomy further from the CORA, which makes intramedullary fixation more of a challenge due to the local deformity, though still correcting the axial alignment. This, however, may be necessary to allow for osteotomy in healthier bone or with an improved soft tissue envelope. The benefit of focal dome osteotomy is that, provided the deformity analysis is done correctly and the CORA is established with the drill bit, the radius can be used to afford correction if there is a sufficient contact area along the cut surfaces to stabilize the correction. That is, the higher the degree of correction required, the closer the cut will need to be to the CORA (
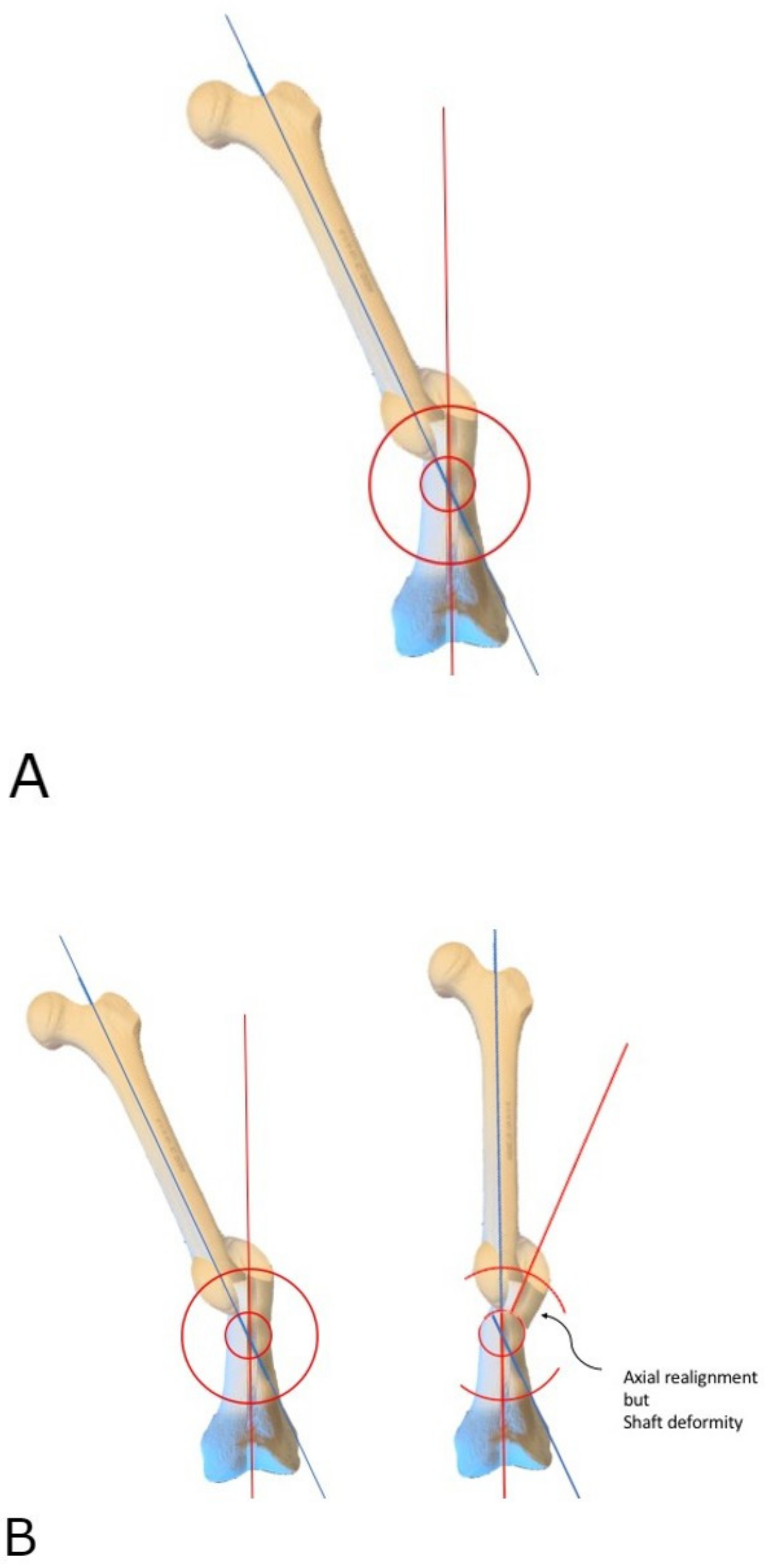
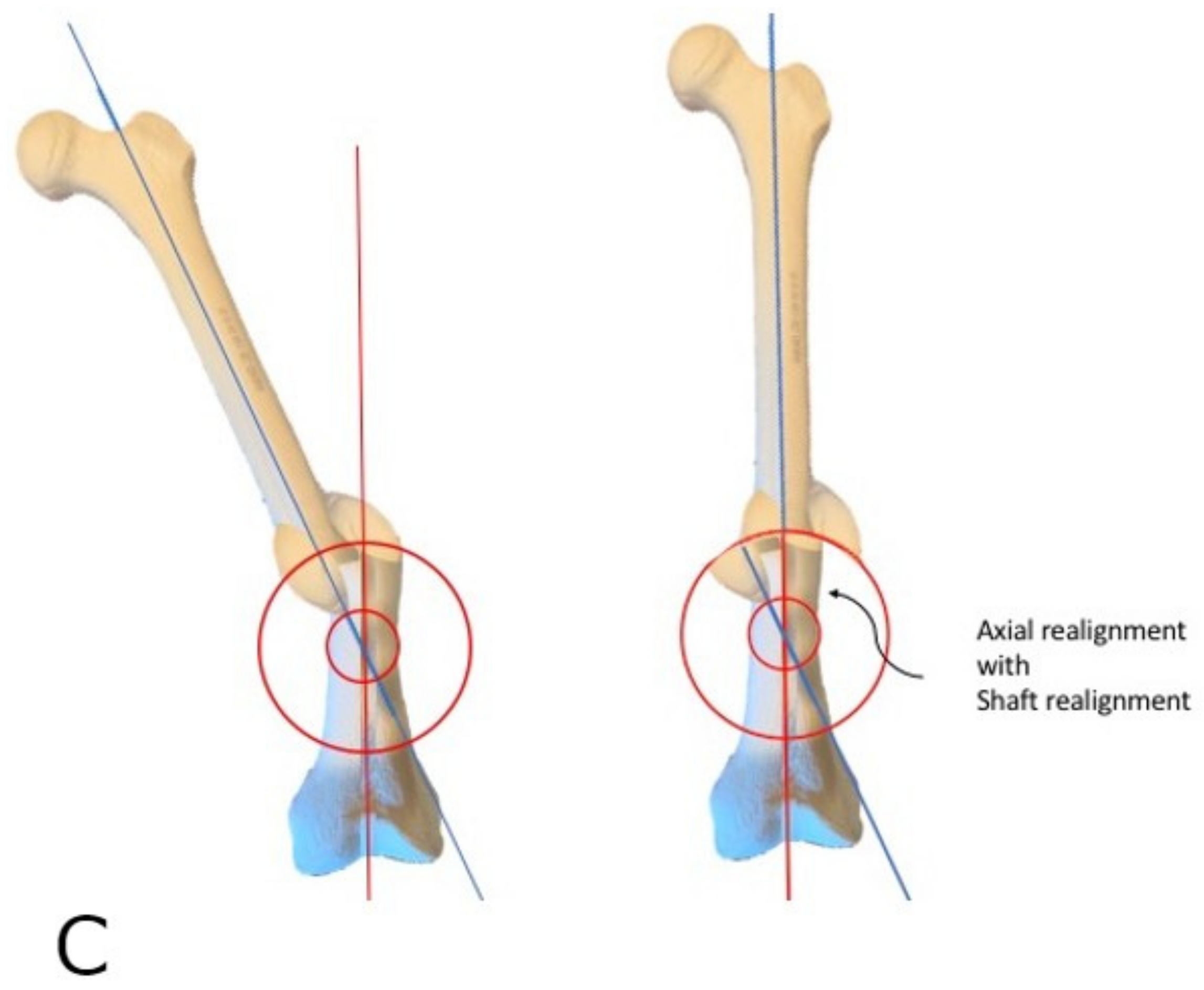
Figure 4). However, one exception is when addressing translation in addition to angulation, where larger radius focal dome osteotomy is preferred. This is discovered in the preoperative templating phase: when the CORA does not fall within the center of the deformity, translational deformity is present. This translation can be corrected with the focal dome, where CORA still defines the center, and the radius length is projected to the center of the actual deformity. Again, when the translation is also present, the osteotomy cut itself (not the CORA) is placed into the center of the deformity to minimize the residual deformity after correction (
Figure 5).
2.3. Surgical Correction
In cortical bone,
Figure 3 demonstrates a parallel drill guide used to drill multiple drill holes along the arc of the osteotomy (cannulated 6.5/7.3 screw system, Depuy-Synthes, West Chester, PA, USA). An absolutely sharp drill bit must be used and must be irrigated constantly, withdrawing the drill bit frequently to prevent overheating and damage to the cortex. This attention to detail is essential for a successful osteotomy in cortical bone. With more heat generated, more damage will occur, and the bone will require a longer healing time. This osteotomy necessitates sufficient surgical fixation and stability to resist loosening for the duration of bone healing.
Once the entire arc of the osteotomy is drilled, the space in between the drill bits can be cut using a low-energy method with a thin osteotome. This must be done extremely carefully so as to prevent escape of the osteotomy outside of the intended arc. Alternatively, a high-speed burr or small oscillating saw, also meticulously irrigated, can be used to initiate the connection between the drill holes, though completed by osteotome.
Supplementary Video S1 demonstrates this technique in further detail.
Once the osteotomy is completed, the correction can be obtained. The use of the universal distractor is valuable in these cases. The intramedullary canal should also be re-established to encourage union. This must be done with as little thermal energy and soft tissue damage imparted to the cortex as possible. Manual T-handle reamers and osteotomes, as well as curettes, should be used to re-establish the canal proximal and distal to the osteotomy. If the bone is extremely dense, a saline-irrigated high-speed burr or drill may be employed to initiate the canal, as little as possible and completed with hand instruments.
Once the soft tissue has allowed for correction and the alignment is achieved using either a universal distractor or other means, compression and fixation can be applied.
With osteotomies close to the CORA, intramedullary devices should preferentially be employed. More of the implant load is shared by the bone after correction. Upon nail insertion, the distractor can be used to apply compression, or nails with compression features can be selected. Many standard nails allow for intraoperative compression, and motorized nails allow progressive or cyclic compression. If the axis of the intramedullary reamer is not sufficiently collinear with the axis of each bone segment, a gap may be produced at the osteotomy. If this occurs, three remedies can be used: (1) widen the path for the intramedullary nail and/or choose a smaller diameter nail, (2) maintain the nail position and add autologous bone graft, and (3) remove the nail and apply compression plate fixation. Factors such as malunion location, bone health, and stability required will determine which option is best. While intramedullary nails are preferred in most cases where a canal can be established, there will be occasions where extramedullary fixation, such as plates, may be preferred. When the bone is extremely sclerotic, the amount of heat generated with the osteotomy is already significant. Adding heat upon soft tissue and bone trauma in order to create a large enough pathway for nail passage should divert the surgeon to choose extramedullary fixation, provided the soft tissue in that location can handle it without additional risk of wound complications.
Once compression is applied and the fracture is absolutely stable, the osteotomy can again be assessed for any bone defects or gaps. Should there be any critical gaps felt to impair fracture healing, these are grafted with autologous bone graft.
2.4. True Dome Osteotomy
The true dome osteotomy is a variation of the focal dome osteotomy. This involves creating two matching concave and convex surfaces. The benefits of a true dome over a focal dome are the forgiving nature of determining the maximum plane of deformity and, especially, the ability to add rotational correction to the osteotomy [
9]. The surgeon needs only to identify the location on the bone based on the CORA but not the plane and magnitude of deformity. This osteotomy provides superb stability during compression [
10].
Current technology allows for applying this method in bone regions where access to the diaphysis is safe and wide enough for the placement of hemispherical concave and convex reamers [
11].
The technique differs greatly in that after the CORA is determined, or in the case of a segmental defect where the bone end represents the CORA, a transverse osteotomy is first created, and the concave and convex reamers are then introduced on each side of the osteotomy. The reamers employed can be standard acetabular reamers to create the concave osteotomy shape, and humeral or femoral head resurfacing reamers are used for the convex surface (Aequalis, Tornier-Wright, Bloomington, MN, USA). In the case of a bulk diaphyseal graft, one side of each osteotomy is reamed ex vivo. Once each matching surface is reamed just enough to create the dome, the two surfaces are mated, and internal fixation is applied. Further reaming beyond that level only shortens the bone. Case 4 illustrates this technique.
Supplementary Video S2 accompanies this manuscript to further demonstrate the concept.