Evaluation of the Effectiveness of Dry Needling in the Treatment of Myogenous Temporomandibular Joint Disorders
Abstract
:1. Background and Objectives
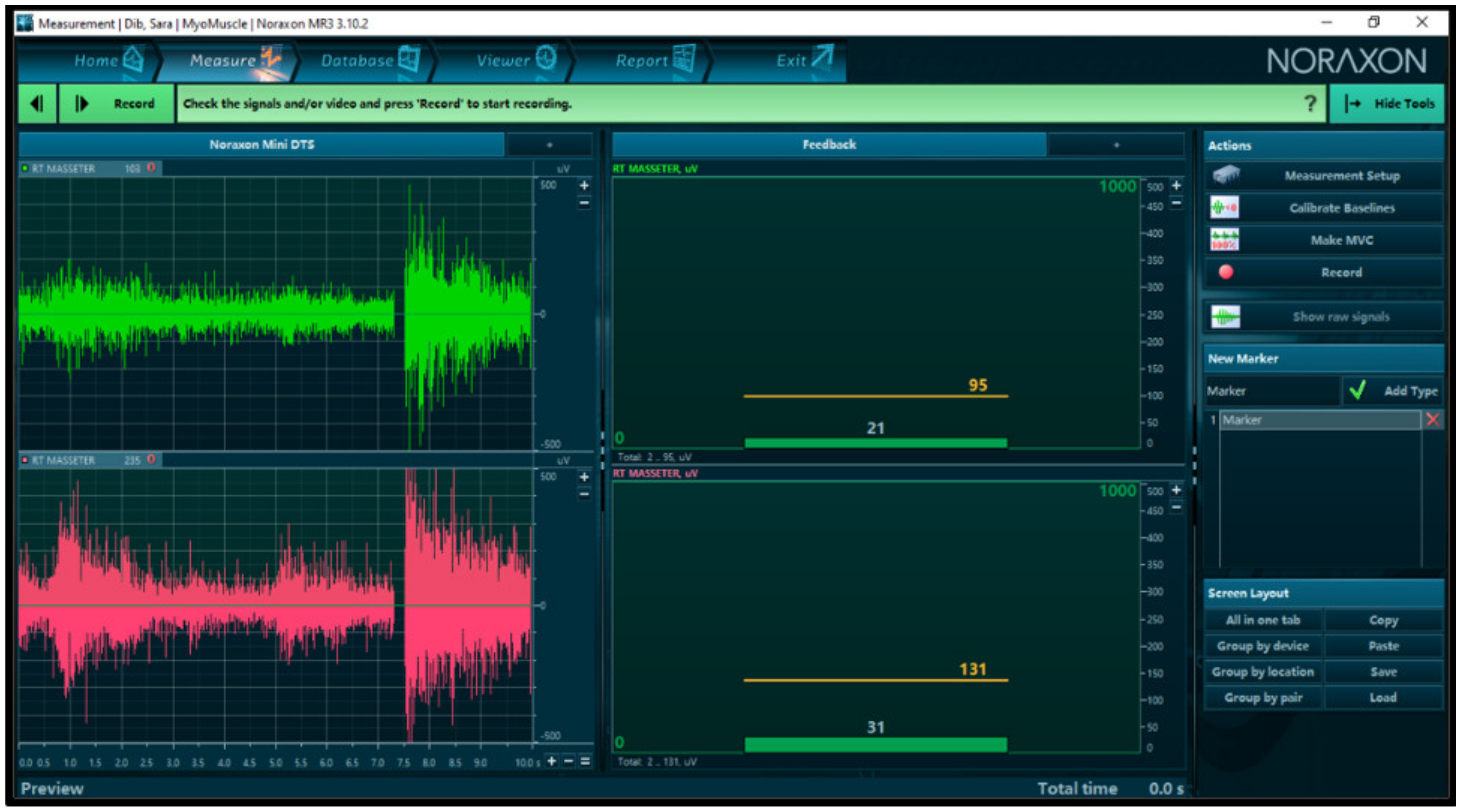
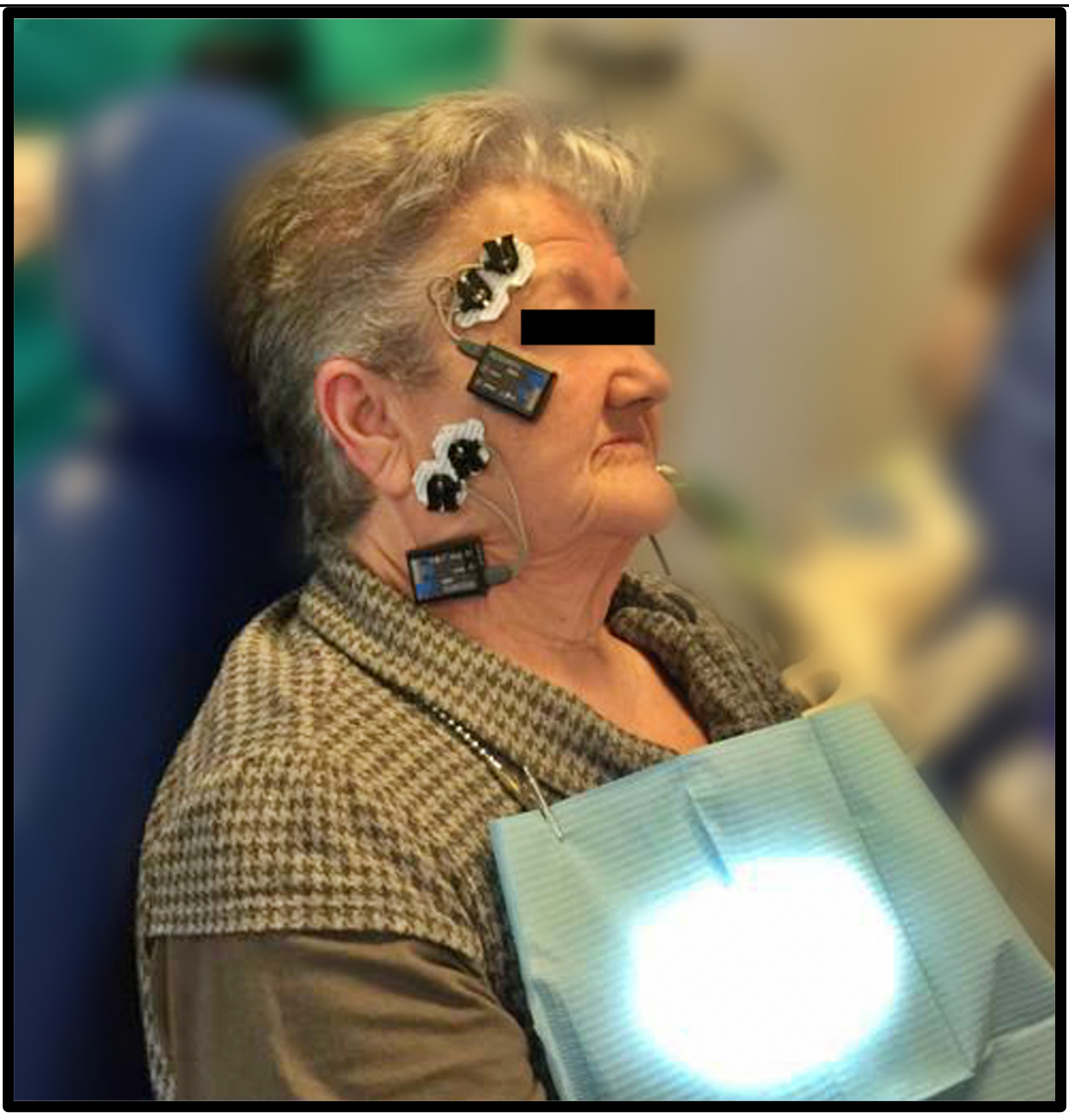
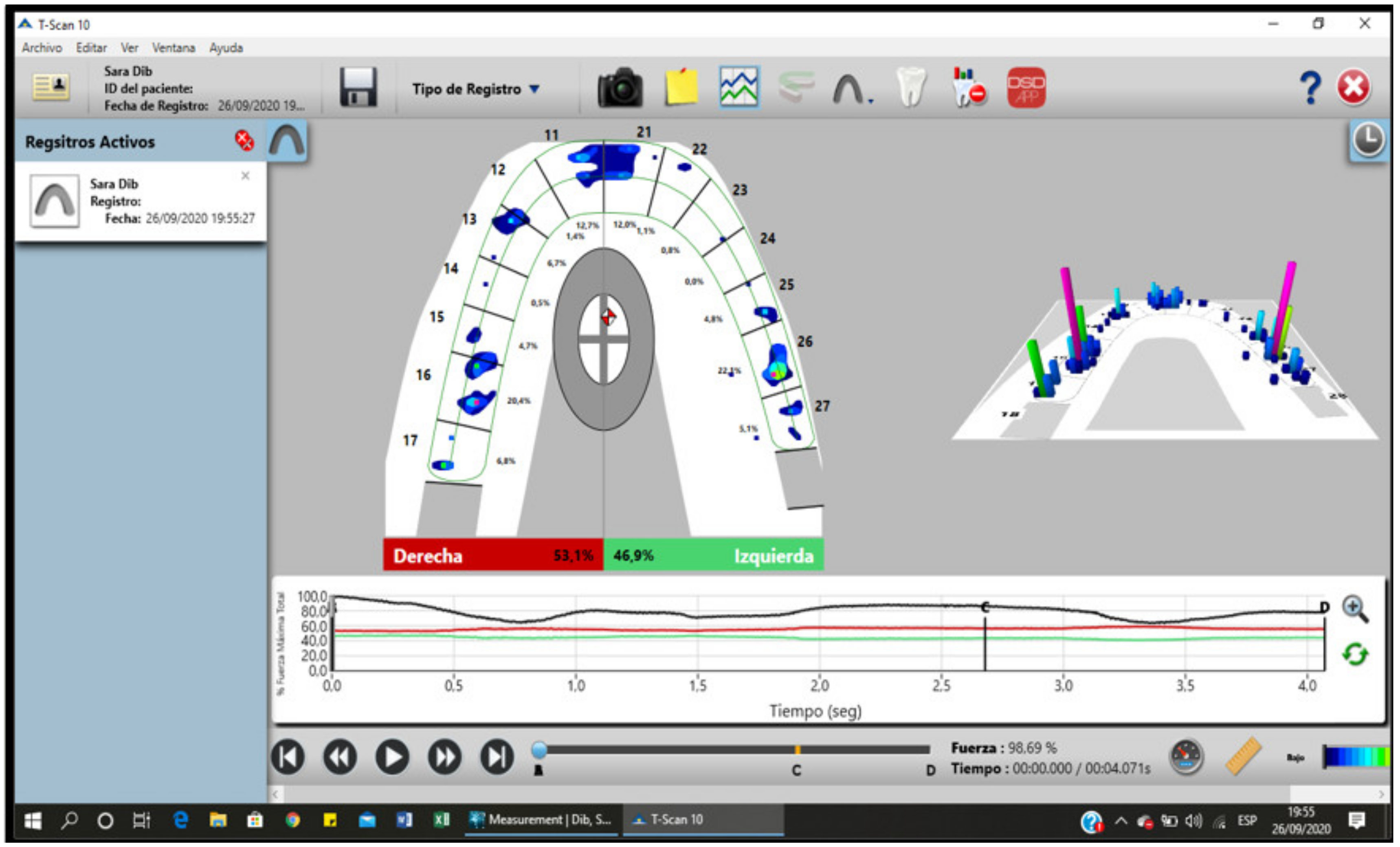
2. Materials and Methods
2.1. Intervention
2.2. Data Analysis
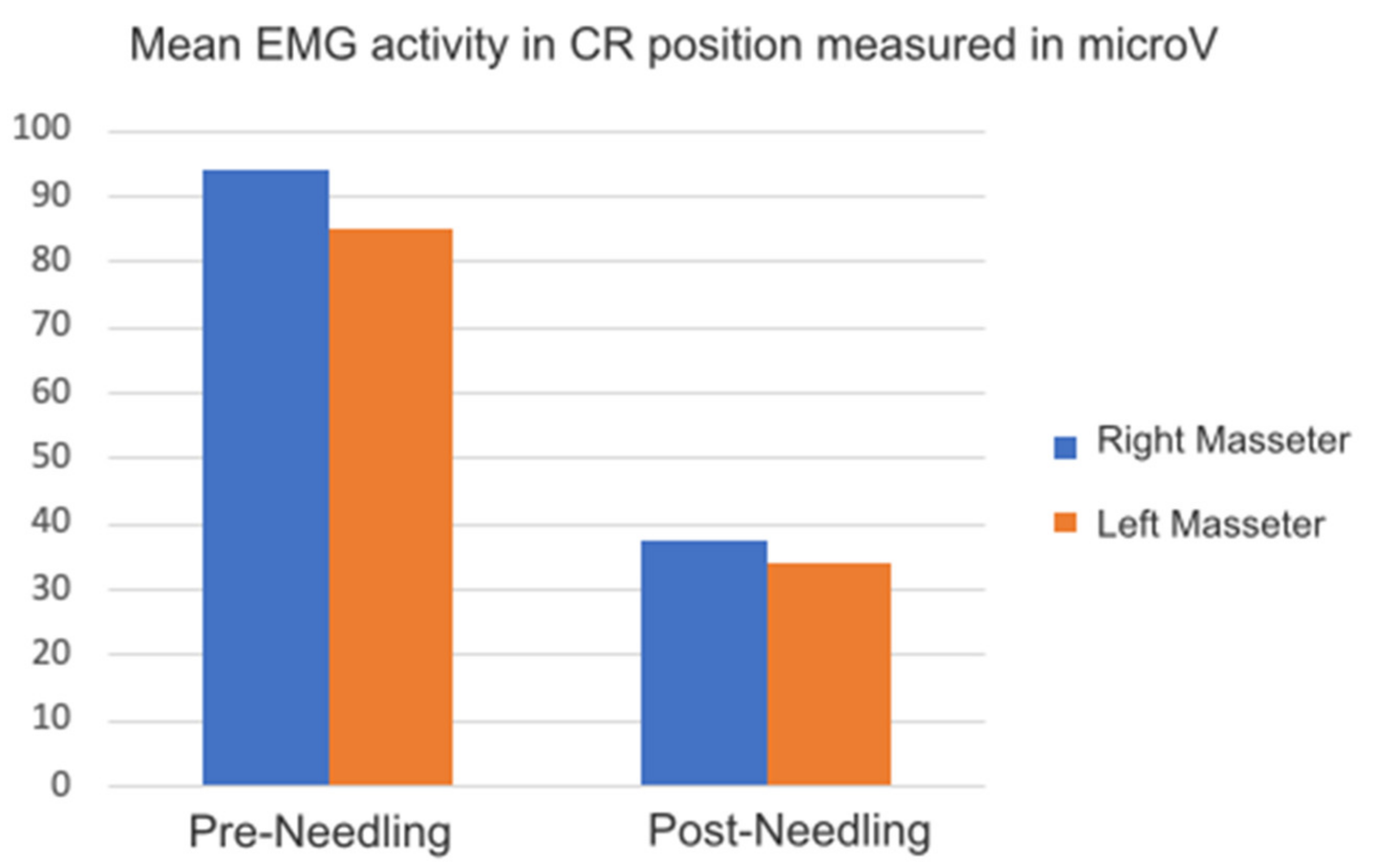
3. Results
4. Discussion
5. Conclusions
- A significant reduction in facial pain and a reduction in muscle activity after needling trigger points.
- A significant variation in the static position and in the trajectory of the movement of the jaw, determined through digital occlusion control using Tec-Scan (occlusal digital analysis).
- A reduction in the asymmetry of the arch when opening and closing the mouth in the centric relation with an increase in the maximum mouth opening after needling.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CR | Central relationship |
| CR-L | Central Relationship through long sheets |
| CR-P | Central Relationship through the first point of occlusal contact |
| DDN | Deep dry puncture |
| DT | Mandibular disclusion time |
| EMG | Electro-miography |
| EVA | Visual Analogue scale |
| MI | Maximum intercuspidation |
| P | Protrusive position |
| PP | Placebo puncture |
| RDC | Research diagnostic criteria |
| RM | Mandibular rest |
| TMJ | Temporomandibular joint |
| T-MI | Time to reach maximum occlusive force |
| Uv | Micro-volt |
References
- Montero, J.; Llodra, J.C.; Bravo, M. Prevalence of the signs and symptoms of temporomandibular disorders among Spanish adults and seniors according to five national surveys performed between 1993 and 2015. J. Oral Facial Pain Headache 2018, 32, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Lobbezoo, F.; Naeije, M. Bruxism is mainly regulated centrally, not peripherally. J. Oral Rehabil. 2001, 28, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Conti, P.C.; Costa, Y.M.; Gonçalves, D.A.; Svensson, P. Headaches and myofascial temporomandibular disorders: Overlapping entities, separate managements? J. Oral Rehabil. 2016, 43, 702–715. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, G.E. Epidemiology and treatment need for temporomandibular disorders. J. Orofac. Pain 1999, 13, 232–237. [Google Scholar]
- Mehta, N.R.; Correa, L.P. Oral appliance therapy and temporomandibular disorders. Sleep Med. Clin. 2018, 13, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Liapaki, A.; Thamm, J.R.; Ha, S.; Monteiro, J.L.G.C.; McCain, J.P.; Troulis, M.J.; Guastaldi, F.P.S. Is there a difference in treatment effect of different intra-articular drugs for temporomandibular joint osteoarthritis? A systematic review of randomized controlled trials. Int. J. Oral Maxillofac. Surg. 2021, 50, 1233–1243. [Google Scholar] [CrossRef]
- Ferreira, N.; Masterson, D.; Lopes de Lima, R.; de Souza, B.; Oliveira, A.T.; Kelly da Silva Fidalgo, T.; Carvalho, A.C.P.; DosSantos, M.F.; Grossmann, E. Efficacy of viscosupplementation with hyaluronic acid in temporomandibular disorders: A systematic review. J. Craniomaxillofac. Surg. 2018, 46, 1943–1952. [Google Scholar] [CrossRef]
- Awan, K.H.; Patil, S. The role of transcutaneous electrical nerve stimulation in the management of temporomandibular joint disorder. J. Contemp. Dent. Pract. 2015, 16, 984–986. [Google Scholar] [CrossRef]
- Zotti, F.; Albanese, M.; Rodella, L.F.; Nocini, P.F. Platelet-rich plasma in treatment of temporomandibular joint dysfunctions: Narrative review. Int. J. Mol. Sci. 2019, 20, 277. [Google Scholar] [CrossRef] [Green Version]
- Renapurkar, S.K. Surgical versus nonsurgical management of degenerative joint disease. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 291–297. [Google Scholar] [CrossRef]
- American Society of Temporomandibular Joint Surgeons. Guidelines for diagnosis and management of disorders involving the temporomandibular joint and related musculoskeletal structures. Cranio 2003, 21, 68–76. [Google Scholar] [CrossRef]
- Fricton, J. Myogenous temporomandibular disorders: Diagnostic and management considerations. Dent. Clin. N. Am. 2007, 51, 61–83. [Google Scholar] [CrossRef]
- Mayoral Del Moral, O. Dry needling treatments for myofascial trigger points. J. Musculoskelet. Pain 2010, 18, 411–416. [Google Scholar] [CrossRef]
- Karakurum, B.; Karaalin, O.; Coskun, O.; Dora, B.; Ucler, S.; Inan, L. The ‘dry-needle technique’: Intramuscular stimulation in tension-type headache. Cephalalgia 2001, 21, 813–817. [Google Scholar] [CrossRef]
- Hong, C.-Z. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am. J. Phys. Med. Rehabil. 1994, 73, 256–263. [Google Scholar] [CrossRef]
- Chen, J.T.; Chung, K.C.; Hou, C.R.; Kuan, T.S.; Chen, S.M.; Hong, C.Z. Inhibitory effect of dry needling on the spontaneous electrical activity recorded from myofascial trigger spots of rabbit skeletal muscle. Am. J. Phys. Med. Rehabil. 2001, 80, 729–735. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Carnero, J.; La Touche, R.; Ortega-Santiago, R.; Galan-del-Rio, F.; Pesquera, J.; Ge, H.Y.; Fernández-de-Las-Peñas, C. Short-term effects of dry needling of active myofascial trigger points in the masseter muscle in patients with temporomandibular disorders. J. Orofac. Pain 2010, 24, 106–112. [Google Scholar] [PubMed]
- Gonzalez-Perez, L.M.; Infante-Cossio, P.; Granados-Nunez, M.; Urresti-Lopez, F.J.; Lopez-Martos, R.; Ruiz-Canela-Mendez, P. Deep dry needling of trigger points located in the lateral pterygoid muscle: Efficacy and safety of treatment for management of myofascial pain and temporomandibular dysfunction. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e326–e333. [Google Scholar] [CrossRef] [PubMed]
- Blasco-Bonora, P.M.; Martín-Pintado-Zugasti, A. Effects of myofascial trigger point dry needling in patients with sleep bruxism and temporomandibular disorders: A prospective case series. Acupunct. Med. 2017, 35, 69–74. [Google Scholar] [CrossRef]
- McMillan, A.S.; Nolan, A.; Kelly, P.J. The efficacy of dry needling and procaine in the treatment of myofascial pain in the jaw muscles. J. Orofac. Pain 1997, 11, 307–314. [Google Scholar]
- Lopez-Martos, R.; Gonzalez-Perez, L.M.; Ruiz-Canela-Mendez, P.; Urresti-Lopez, F.J.; Gutierrez-Perez, J.L.; Infante-Cossio, P. Randomized, double-blind study comparing percutaneous electrolysis and dry needling for the management of temporomandibular myofascial pain. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e454–e462. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Perez, L.M.; Infante-Cossio, P.; Granados-Nuñez, M.; Urresti-Lopez, F.J. Treatment of temporomandibular myofascial pain with deep dry needling. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e781–e785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dib, A.; Montero, J.; Sanchez, J.M.; López-Valverde, A. Electromyographic and patient-reported outcomes of a computer-guided occlusal adjustment performed on patients suffering from chronic myofascial pain. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e135–e143. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Doig, G.S.; Simpson, F. Randomization and allocation concealment: A practical guide for researchers. J. Crit. Care 2005, 20, 187–191. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis of the Behavioural Sciences, 2nd ed.; Lawrence Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Fernández-Carnero, J.; Gilarranz-de-Frutos, L.; León-Hernández, J.V.; Pecos-Martin, D.; Alguacil-Diego, I.; Gallego-Izquierdo, T.; Martín-Pintado-Zugasti, A. Effectiveness of different deep dry needling dosages in the treatment of patients with cervical myofascial pain: A pilot RCT. Am. J. Phys. Med. Rehabil. 2017, 96, 726–733. [Google Scholar] [CrossRef]
- Abbaszadeh-Amirdehi, M.; Ansari, N.N.; Naghdi, S.; Olyaei, G.; Nourbakhsh, M.R. Neurophysiological and clinical effects of dry needling in patients with upper trapezius myofascial trigger points. J. Bodyw. Mov. Ther. 2017, 21, 48–52. [Google Scholar] [CrossRef]
- Martin-Pintado-Zugasti, A.; Rodríguez-Fernández, A.L.; Fernandez-Carnero, J. Postneedling soreness after deep dry needling of a latent myofascial trigger point in the upper trapezius muscle: Characteristics, sex differences and associated factors. J. Back Musculoskelet. Rehabil. 2016, 29, 301–308. [Google Scholar] [CrossRef]
- Dar, G.; Hicks, G.E. The immediate effect of dry needling on multifidus muscles´ function in healthy individuals. J. Back Musculoskelet. Rehabil. 2016, 29, 273–278. [Google Scholar] [CrossRef]
- Fuentes-Gallardo, I.; Perez-Muñoz, M.; Mayoral-Del-Moral, O.; Lluch-Girbés, E.; Prieto-Valiente, L.; Falla, D. Effectiveness of dry needling for chronic nonspecific neck pain: A randomizes, single-blinded, clinical trial. Pain 2016, 157, 1905–1917. [Google Scholar]
- Cerezo-Téllez, E.; Lacomba, M.T.; Fuentes-Gllardo, I.; Mayoral-del-Moral, O.; Rodrigo-Medina, B.; Gutiérrez Ortega, C. Dry needling of the trapezius muscle in office workers with neck pain: A randomized clinical trial. J. Man. Manip. Ther. 2016, 24, 223–232. [Google Scholar] [CrossRef] [Green Version]
- Calvo-Lobo, C.; Pacheco-da-Costa, S.; Hita-Herranz, E. Efficacy of deep dry needling on latent myofascial trigger points in older adults with nonspecific shoulder pain: A randomized, controlled clinical trial pilot study. J. Geriatr. Phys. Ther. 2017, 40, 63–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez-Mila, Z.; Salom-Moreno, J.; Fernandez-de-las-Peñas, C. Effects of dry needling on post-stroke spasticity, motor function and stability limits: A randomized clinical trial. Acupunct. Med. 2018, 36, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Gattie, E.; Cleland, J.A.; Snodgrass, S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: A systematic review and meta-analysis. J. Orthop. Sports Phys. Ther. 2017, 47, 133–149. [Google Scholar] [CrossRef] [PubMed]
- Arias-Buría, J.L.; Fernández-de-Las-Peñas, C.; Palacios-Ceña, M.; Koppenhaver, S.L.; Salom-Moreno, J. Exercises and dry needling for subacromial pain syndrome: A randomized parallel-group trial. J. Pain 2017, 18, 11–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arias-Buría, J.L.; Martín-Saborido, C.; Cleland, J.; Koppenhaver, S.L.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C. Cost-effectiveness evaluation of the inclusion of dry needling into an exercise program for subacromial pain syndrome: Evidence from a randomized clinical trial. Pain Med. 2018, 19, 2336–2347. [Google Scholar] [CrossRef]
- Espí-López, G.V.; Serra-Añó, P.; Vicent-Ferrando, J.; Sánchez-Moreno-Giner, M.; Arias-Buría, J.L.; Cleland, J.; Fernandez-De-Las-Penas, C. Effectiveness of inclusion of dry needling in a multimodal therapy program for patellofemoral pain: A randomized parallel-group trial. J. Orthop. Sports Phys. Ther. 2017, 47, 392–440. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Romero, E.A.; Pecos-Martín, D.; Calvo-Lobo, C.; Ochoa-Sáez, V.; Burgos-Caballero, V.; Fernández-Carnero, J. Effects of dry needling in an exercise program for older adults with knee osteoarthritis: A pilot clinical trial. Medicine 2018, 97, e11255. [Google Scholar] [CrossRef]
- Dunning, J.; Butts, R.; Young, I.; Mourad, F.; Galante, V.; Bliton, P.; Tanner, M.; Fernández-de-Las-Peñas, C. Periosteal electrical dry needling as an adjunct to exercise and manual therapy for knee osteoarthritis: A multicenter randomized clinical trial. Clin. J. Pain 2018, 34, 1149–1158. [Google Scholar] [CrossRef]
- Cagnie, B.; Dewitte, V.; Barbe, T.; Timmermans, F.; Delrue, N.; Meeus, M. Physiologic effects of dry needling. Curr. Pain Headache Rep. 2013, 17, 348. [Google Scholar] [CrossRef]
- Gerwin, R.D.; Dommerholt, J.; Shah, J.P. An expansion of Simons‘ integrated hypothesis of trigger point formation. Curr. Pain Headache Rep. 2004, 8, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.W.; Hsieh, Y.L.; Kao, M.J.; Hong, J.Z. Remote influences of acupuncture on the pain intensity and the amplitude changes of endplate noise in the myofascial trigger point of the upper trapezius muscle. Arch. Phys. Med. Rehabil. 2009, 90, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.G.; Liu, L.; Huang, Q.M.; Nguyen, T.T.; Ma, Y.T.; Zhao, J.M. Decreased spontaneous electrical activity and acetylcholine at myofascial trigger spots after dry needling treatment: A pilot study. Evid.-Based Complementary Alternat. Med. 2017, 2017, 3938191. [Google Scholar] [CrossRef] [PubMed]
- Abbaszadeh-Amirdehi, M.; Ansari, N.N.; Naghdi, S.; Olyaei, G.; Nourbakhsh, M.R. Therapeutic effects of dry needling in patients with upper trapezius myofascial trigger points. Acupunct. Med. 2017, 35, 85–92. [Google Scholar] [CrossRef] [Green Version]
- Cagnie, B.; Barbe, T.; De Ridder, E.; Van Oosterwijck, J.; Cools, A.; Danneels, L. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. J. Manip. Physiol. Ther. 2012, 35, 685–691. [Google Scholar] [CrossRef]
- Dommerholt, J. Dry needling: Peripheral and central considerations. J. Man. Manip. Ther. 2011, 19, 223–237. [Google Scholar] [CrossRef] [Green Version]
- Butts, R.; Dunning, J.; Perreault, T.; Mourad, F.; Grubb, M. Peripheral and spinal mechanisms of pain and dry needling mediated analgesia: A clinical resource guide for health care professionals. Int. J. Phys. Med. Rehabil. 2016, 4, 2. [Google Scholar] [CrossRef] [Green Version]
- Chou, L.W.; Kao, M.J.; Lin, J.G. Probable mechanisms of needling therapies for myofascial pain control. Evid.-Based Complementary Alternat. Med. 2012, 2012, 705327. [Google Scholar] [CrossRef]
- Hsieh, Y.L.; Yang, S.A.; Yang, C.C.; Chou, L.W. Dry needling at myofascial trigger spots of rabbit skeletal muscles modulates the biochemicals associated with pain, inflammation, and hypoxia. Evid.-Based Complementary Alternat. Med. 2012, 2012, 342165. [Google Scholar] [CrossRef]
- Hsieh, Y.L.; Kao, M.J.; Kuan, T.S.; Chen, S.M.; Chen, J.T.; Hong, C.Z. Dry needling to a key myofascial trigger point may reduce the irritability of satellite MTrPs. Am. J. Phys. Med. Rehabil. 2007, 86, 397–403. [Google Scholar] [CrossRef]
- Tsai, C.T.; Hsieh, L.F.; Kuan, T.S.; Kao, M.J.; Chou, L.W.; Hong, C.Z. Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am. J. Phys. Med. Rehabil. 2010, 89, 133–140. [Google Scholar] [CrossRef]
- Hsieh, Y.L.; Chou, L.W.; Joe, Y.S.; Hong, C.Z. Spinal cord mechanism involving the remote effects of dry needling on the irritability of myofascial trigger spots in rabbit skeletal muscle. Arch. Phys. Med. Rehabil. 2011, 92, 1098–1105. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, Y.L.; Yang, S.A.; Liu, S.Y.; Chou, L.W.; Honc, C.Z. Remote dose-dependent effects of dry needling at distant myofascial trigger spots of rabbit skeletal muscles on reduction of substance P levels of proximal muscle and spinal cords. BioMed Res. Int. 2014, 2014, 982121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srbely, J.Z.; Dickey, J.P.; Lee, D.; Lowerison, M. Dry needle stimulation of myofascial trigger points evokes segmental anti-nociceptive effects. J. Rehabil. Med. 2010, 42, 463–468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Audette, J.F.; Wang, F.; Smith, H. Bilateral activation of motor unit potentials with unilateral needle stimulation of active myofascial trigger points. Am. J. Phys. Med. Rehabil. 2004, 83, 368–374. [Google Scholar] [CrossRef]
- Chae, Y.; Chang, D.S.; Lee, S.H.; Jung, W.M.; Lee, I.S.; Jackson, S.; Kong, J.; Lee, H.; Park, H.J.; Lee, H.; et al. Inserting needles into the body: A meta-analysis of brain activity associated with acupuncture needle stimulation. J. Pain 2013, 14, 215–222. [Google Scholar] [CrossRef]
- Niddam, D.M.; Chan, R.C.; Lee, S.H.; Yeh, T.C.; Hsieh, J.C. Central modulation of pain evoked from myofascial trigger point. Clin. J. Pain 2007, 23, 440–448. [Google Scholar] [CrossRef] [Green Version]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother. Theory Pract. 2016, 32, 332–355. [Google Scholar] [CrossRef]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical activity and exercise for chronic pain in adults: An overview of cochrane reviews. Cochrane Database Syst. Rev. 2017, 4, CD011279. [Google Scholar]
- Brunner, E.; De Herdt, A.; Minguet, P.; Baldew, S.S.; Probst, M. Can cognitive behavioural therapy-based strategies be integrated into physiotherapy for the prevention of chronic low back pain? A systematic review. Dis. Rehabil. 2013, 35, 1–10. [Google Scholar] [CrossRef]
- Williams, A.C.; Eccleston, C.; Morley, S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst. Rev. 2012, 11, CD007407. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Mairesse, O.; Neu, D.; Leysen, L.; Danneels, L.; Cagnie, B.; Meeus, M.; Moens, M.; Ickmans, K.; Goubert, D. Sleep disturbances in chronic pain: Neurobiology, assessment and treatment in physical therapist practice. Phys. Ther. 2018, 98, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Lluch Girbes, E.; Meeus, M.; Baert, I.; Balancing, N.J. “Hands-on” with “hands-off” physical therapy interventions for the treatment of central sensitization pain in osteoarthritis. Man. Ther. 2015, 20, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15. [Google Scholar] [CrossRef] [PubMed]
- Kosek, E.; Cohen, M.; Baron, R.; Gebhart, G.F.; Mico, J.A.; Rice, A.S.; Rief, W.; Sluka, A.K. Do we need a third mechanistic descriptor for chronic pain states? Pain 2016, 157, 1382–1386. [Google Scholar] [CrossRef]
- Fernández de Las Peñas, C.; Dommerholt, J. Myofascial trigger points: Peripheral or central phenomenon? Curr. Rheumatol. Rep. 2014, 16, 395. [Google Scholar] [CrossRef]
- Malfliet, A.; Kregel, J.; Coppieters, I.; De Pauw, R.; Meeus, M.; Roussel, N.; Cagnie, B.; Danneels, L.; Nijs, J. Effect of pain neuroscience education combined with cognition-targeted motor control training on chronic spinal pain: A randomized clinical trial. JAMA Neurol. 2018, 75, 808–817. [Google Scholar] [CrossRef]



| Mean Pre- | Deviation Pre- | Mean Post- | Deviation Post- | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Cont. | Interv. | Cont. | Interv. | |||||
| Right | Left | Right | Left | Right | Left | Right | Left | |||||
| RM | 19 | 20.36 | 19.31 | 25.05 | 21 | 15.8 | 23.71 | 17.65 | 20.06 | 12.76 | 40.27 | 18.04 |
| MI | 130.73 | 125.55 | 227.83 | 248.22 | 229 | 228.75 | 112.86 | 90.71 | 402.1 | 402.25 | 222.34 | 168.37 |
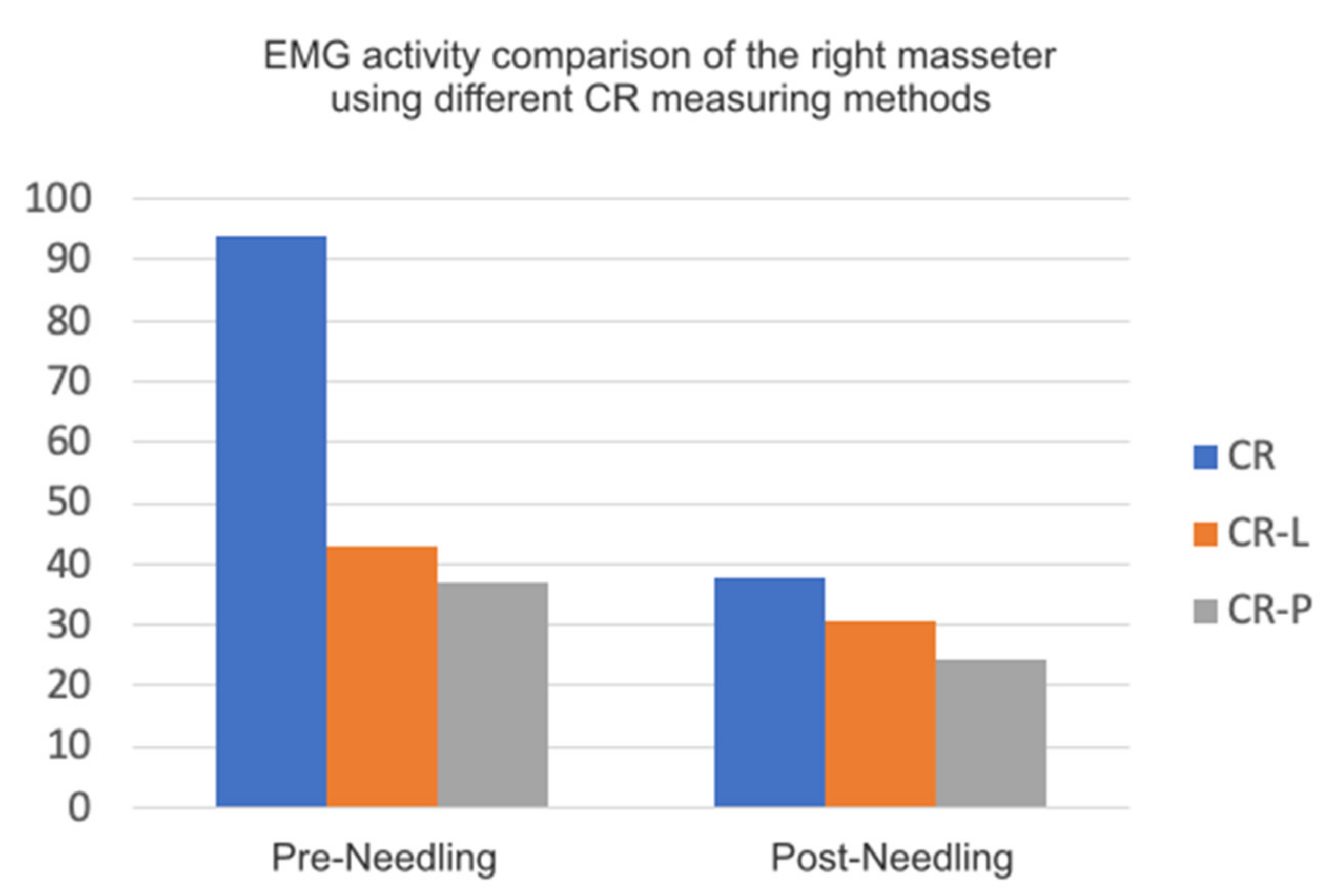
| CR | 94 | 85 | 73.5 | 68.38 | 94 | 70.50 | 37.71 | 34.14 | 150.70 | 106.34 | 58.71 | 49.14 |
| CR-L | 42.91 | 36.91 | 66.96 | 53.86 | 92 | 70 | 30.50 | 28.3 | 64.3 | 52.5 | 35.3 | 30.45 |
| CR-P | 36.91 | 33 | 54.83 | 46.77 | 35 | 30 | 24.4 | 20 | 50.30 | 40.23 | 45.5 | 35.45 |
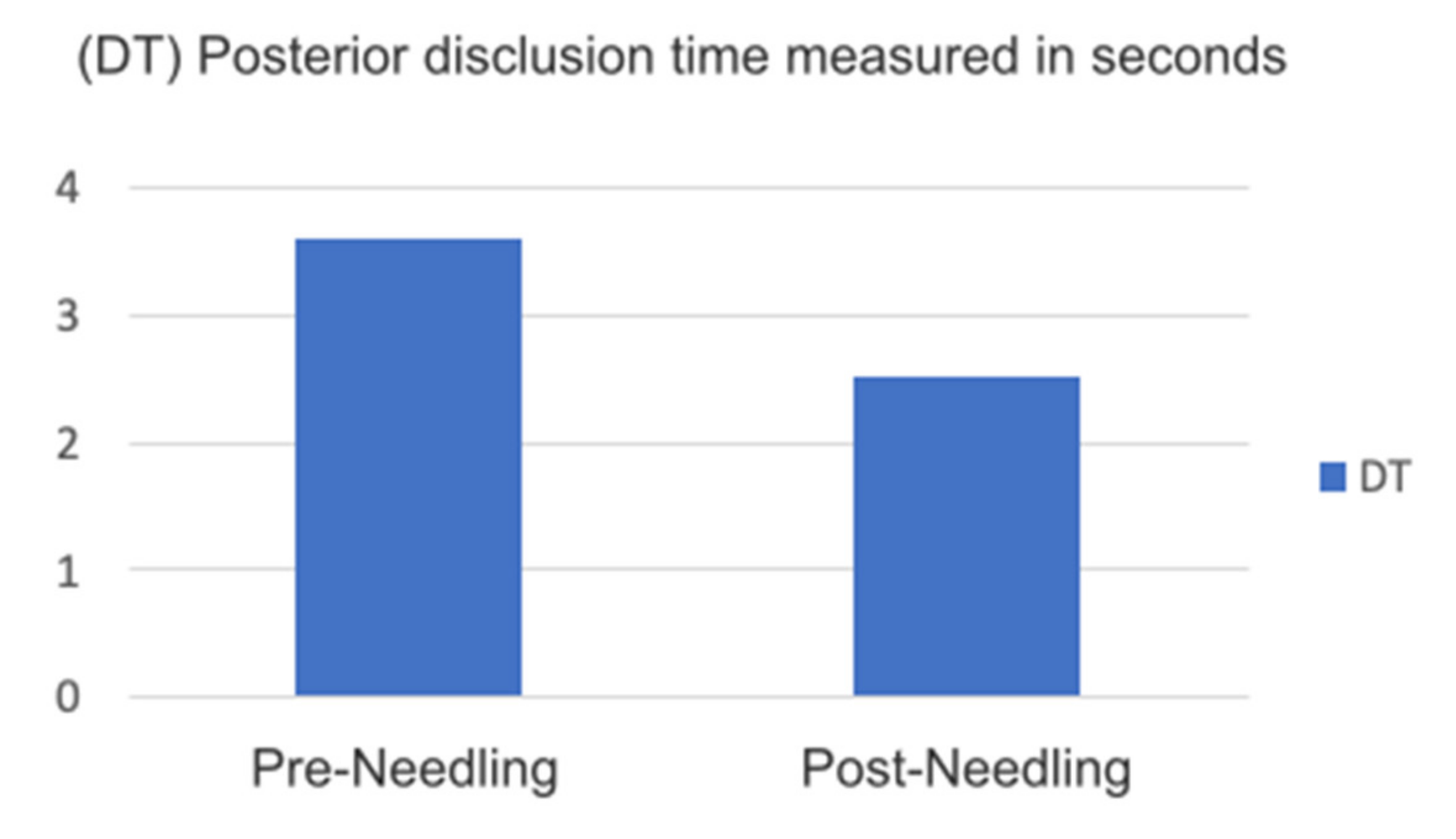
| DT | 3.59 | 1.74 | 3.45 | 2.09 | 0.5 | 1.3 | ||||||
| P | 94.82 | 81 | 147.46 | 160.41 | 174.50 | 98.75 | 64.57 | 51.43 | 255.03 | 147.54 | 123.92 | 87.74 |
| T-MI | 0.87 | 1.21 | 0.25 | 0.6 | ||||||||
| Presence Percentage | Asymmetry | Symmetry |
|---|---|---|
| Pre- | 75% | 25% |
| Post- | 37.5% | 62.5% |
| Mean Pre- | Dev. Pre- | Mean Post- | Dev. Post- | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Cont. | Interv. | Cont. | Interv. | Cont. | Interv. | Cont. | Interv. | ||
| Mouth Opening | 44.92 | 7.36 | 51.75 | 51 | 2.36 | 2.64 | |||
| Facial Pain | 7.75 | 8.57 | 0.95 | 0.97 | 0.5 | 1.5 | 0.57 | 0.97 | |
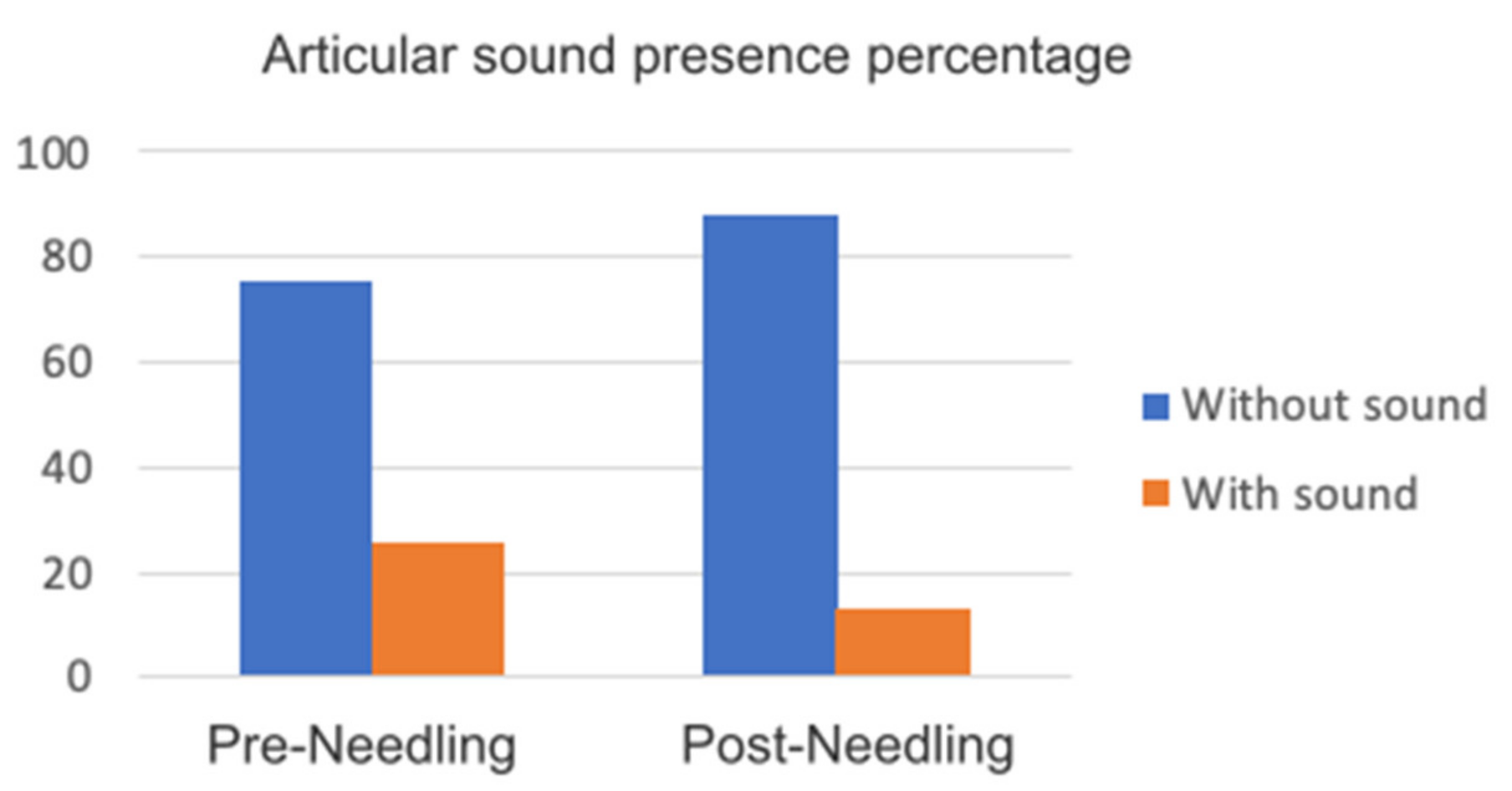
| Articular Sound | No | 75% | 75% | 100% | 87.5% | ||||
| Yes | 25% | 25% | 0 | 12.5% | |||||
| TMJ pain | 2.50 | 3 | 1.73 | 2.77 | 1 | 2.63 | 2 | 3.24 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dib-Zakkour, J.; Flores-Fraile, J.; Montero-Martin, J.; Dib-Zakkour, S.; Dib-Zaitun, I. Evaluation of the Effectiveness of Dry Needling in the Treatment of Myogenous Temporomandibular Joint Disorders. Medicina 2022, 58, 256. https://doi.org/10.3390/medicina58020256
Dib-Zakkour J, Flores-Fraile J, Montero-Martin J, Dib-Zakkour S, Dib-Zaitun I. Evaluation of the Effectiveness of Dry Needling in the Treatment of Myogenous Temporomandibular Joint Disorders. Medicina. 2022; 58(2):256. https://doi.org/10.3390/medicina58020256
Chicago/Turabian StyleDib-Zakkour, Juan, Javier Flores-Fraile, Javier Montero-Martin, Sara Dib-Zakkour, and Ibrahim Dib-Zaitun. 2022. "Evaluation of the Effectiveness of Dry Needling in the Treatment of Myogenous Temporomandibular Joint Disorders" Medicina 58, no. 2: 256. https://doi.org/10.3390/medicina58020256
APA StyleDib-Zakkour, J., Flores-Fraile, J., Montero-Martin, J., Dib-Zakkour, S., & Dib-Zaitun, I. (2022). Evaluation of the Effectiveness of Dry Needling in the Treatment of Myogenous Temporomandibular Joint Disorders. Medicina, 58(2), 256. https://doi.org/10.3390/medicina58020256








