Abstract
Background and Objetives: Currently, total knee arthroplasty is one of the most common surgeries, increasing with the increase in life expectancy. Whether or not to replace the patella has been a subject of debate over the years, remaining in controversy and without reaching a consensus. Over the years, different meta-analyses have been carried out in order to provide evidence on the subject, although, in recent times, there have not been many new studies in this regard. Therefore, it is considered necessary that the latest works form part of a new meta-analysis. Materials and Method: We searched the literature using PUBMED, SCOPUS, the Cochrane database and VHL from 2010 to 2020. The search terms used were “patellar” AND “resurfacing” OR “Replacement” and “no resurfacing” OR “no replacement”. A meta-analysis was performed with Stata software (Stata version 15.1). Forest plots were generated to illustrate the overall effect of knee arthroplasty interventions. Results: As a result, it was obtained that there is a significantly higher risk of suffering AKP in the non-resurfacing group, in addition to a significant increase in the risk of undergoing a reoperation in the non-resurfacing group. On the other hand, significant differences were obtained in favor of the resurfacing group in both the clinical and Feller KSS, with functional KSS being inconclusive. After analyzing different variables throughout the literature, it does seem clear that the non-resurfacing group may present a higher risk of reoperation than the resurfacing group. Conclusions: For all these reasons, we think that, although it does seem that not replacing the patella can precipitate a reoperation, it is not clear whether this reoperation is a direct consequence of not having replaced the patella. Therefore, in our opinion, the treatment must be individualized for each patient.
1. Introduction
Total knee arthroplasty is one of the most common surgeries of our time, being more and more frequent due to the increase in life expectancy and quality of life of patients [1]. There are many possibilities within this type of intervention (one-compartment, two-compartment or three-compartment prostheses). The decision to replace the patella or not has been the subject of debate over the years and remains controversial. On the one hand, the defenders of not replacing the patella or doing it only in selected cases argue that the replacement could increase the rate of patella fracture, rupture of the polyethylene or loosening of the latter, among other complications [2], while those who defend systematic replacement cite less anterior knee pain and a lower revision rate [3,4]. However, it is also indicated that the complications of replacing it may be more severe (fracture or avascular necrosis of the patella) [5,6].
Likewise, the functional results of the different options in terms of patella replacement in knee arthroplasty remain under debate [7,8]. All of this has led to the realization of randomized clinical trials to evaluate the efficacy of the different therapeutic options. Currently, it is still a matter of debate; some surgeons prefer patellaplasty over replacement [9,10], while others prefer selective replacement of the patella based on the state of the cartilage, bone stock or the shape of the patella, radiographic issues or individual characteristics of the patient, such as weight, height or personal preference [9,11].
Over the years, different meta-analyses have been carried out to provide evidence on the subject [8,9,10,11]. However, in recent times, there have not been many new studies in this regard, the last being published in 2019, based on the search criteria. Therefore, it is considered necessary that the latest works form part of a new meta-analysis.
For this reason, the present article includes five new randomized clinical trials of the ten selected in the systematic review, which are not included in previous meta-analyses. We also include some variables that are not very constant throughout the literature, such as the deep infection rate, or radiographic variables such as the Insall ratio or the congruence angle, among others, in addition to the most common variables, such as functional scales, the KSS being the most frequent.
2. Materials and Methods
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist and statement was followed for conducting this study [12,13].
2.1. Search Strategy
We searched the literature using PUBMED, SCOPUS, the Cochrane database and BVS from 1 January 2010 to 15 September 2020. The search terms used were “patellar” AND “resurfacing” OR “replacement” AND “non-resurfacing” OR “non-replacement”. The search was performed between 16 September and 20 September.
2.2. Inclusion Criteria
English- and Spanish-language literature, prospective randomized control trials (RCTs) performed in humans comparing total knee arthroplasty (TKA) with patellar resurfacing to TKAs without patellar resurfacing. Adults undergoing primary total knee arthroplasty. Data for at least one of the following outcomes: Visual Analog Scale (VAS), Knee Society Score (KSS), WOMAC score, KOOS, Feller score, postoperative outcomes (such as anterior knee pain or deep infection) and radiological outcomes (Insall ratio, congruence angle or patellar tilt).
2.3. Data Extraction
Two authors independently extracted data, using standardized data extraction forms, from studies and discrepancies were resolved by discussion and consensus with a third party. Extracted data included publication information, number of knees analyzed, general characteristics of the study (such as mean age, gender, BMI), type of implant, follow-up time and outcomes reported. The number of subjects, mean and SD of continuous outcomes were extracted.
2.4. Risk of Bias Assessment
Two of the authors independently assessed the methodological quality of each included study using the Cochrane Collaborations’ tool for assessing risk of bias, and discrepancies were resolved by discussion [14]. This checked for random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcomes assessors, incomplete outcome data and selective reporting [15].
2.5. Meta-Analysis
A meta-analysis was performed using the Stata Software for Statistics and Data Science (Stata version 15.1, College Station, TX, USA: StataCorp LLC) and was limited due to the clinical heterogeneity of the included studies. Forest plots were generated to illustrate the overall effect of knee arthroplasty interventions and funnel plots were produced to assess publication bias.
3. Results
The literature search yielded 345 potentially relevant papers (Figure 1). Following screening and the application of eligibility criteria, 61 relevant papers were identified based on title and abstract. These papers were subjected to screening of their full texts. Following application of the eligibility criteria to the full texts, we were able to identify 10 studies for inclusion (Table 1). The assessment of bias for these studies can be seen in Table 2.
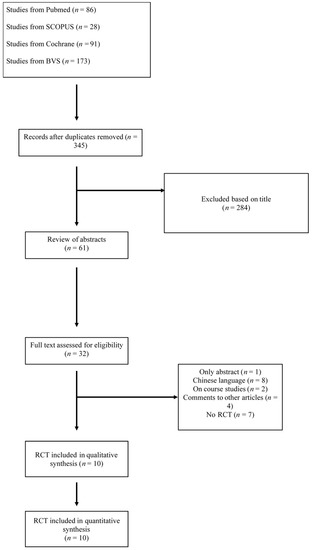
Figure 1.
Search flowchart.

Table 1.
Articles selected and included in the meta-analysis.

Table 2.
Assessment of study bias (red=high bias, yellow=intermediate bias, green=low bias.
It is essential to emphasize that all the exposed variables correspond to the results given after the surgical intervention at its maximum time of follow-up.
- Range of Motion (ROM)
There are three studies that provide data on ROM, observing that there are no significant differences between replacing and not replacing the patella, as seen in Figure 2.
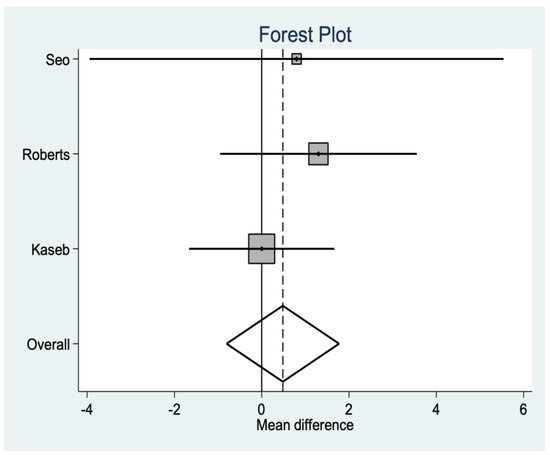
Figure 2.
Range of Motion (ROM) data.
- KSS clinical
This is the variable that is repeated the most throughout the studies, and statistically significant differences (p = 0.0007) are observed in favor of the resurfacing group (Figure 3).
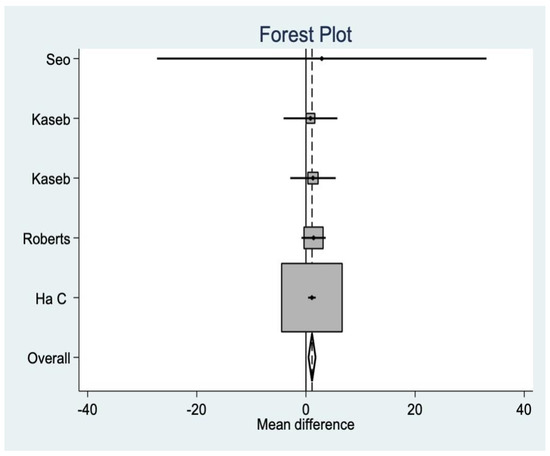
Figure 3.
KSS clinical data.
- KSS functional
This variable is also found quite consistently in the literature, but, in this case, we did not find significant differences (Figure 4
).
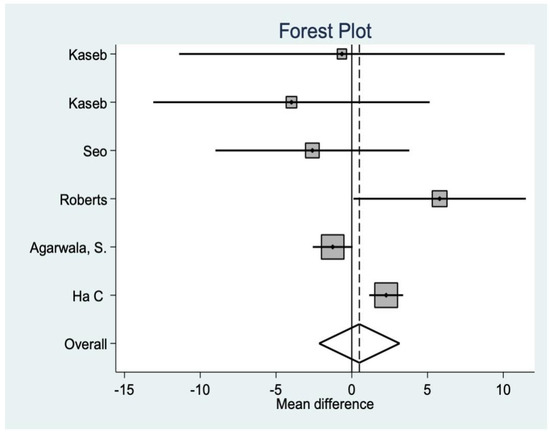
Figure 4.
KSS functional data.
- Feller Score
This is another variable that analyzes functionality after the intervention, finding, in this case, significant differences in favor of the resurfacing group (p = 0.001 (Figure 5).
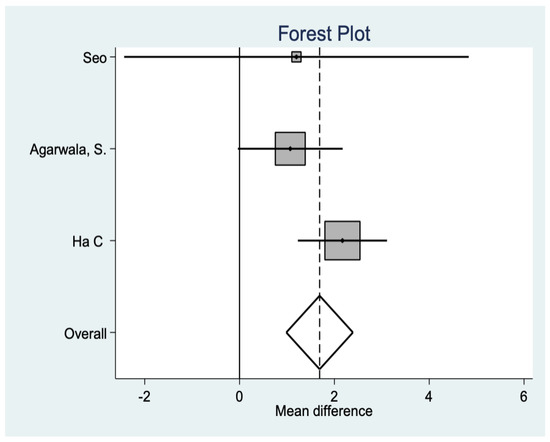
Figure 5.
Feller score data.
- Visual Analog Scale (VAS)
In three studies, the VAS was analyzed for postoperative pain, where no significant differences were found between groups (Figure 6).
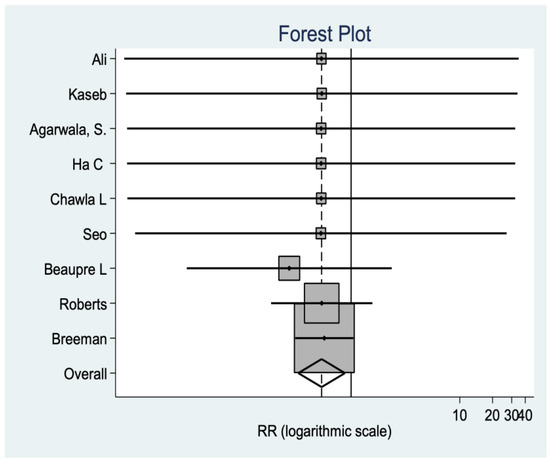
Figure 6.
Visual Analog Scale data.
- Review fee
Data are reported in this regard in nine studies, observing a significant difference in favor of the no-resurfacing group (p = 0.0137). In other words, this group has a higher risk of revision than the resurfacing group (Figure 7).
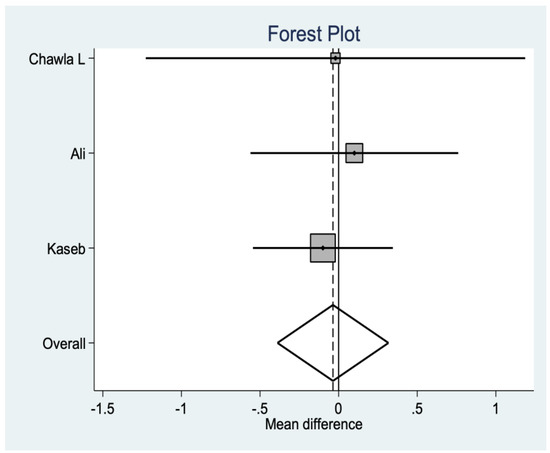
Figure 7.
Review fee data.
- Deep infection rate
Regarding the deep infection rate, a precise statistical analysis cannot be performed due to the few reported cases, since only one case of infection has been reported in the non-resurfacing group [19] and another case in the resurfacing group [18]. The rest of the studies that report data on this question did not find cases of infection in either of the two groups.
- Anterior Knee Pain (AKP)
There are results in three of the studies, which show statistically positive data in favor of no resurfacing (p = 0.012). In other words, in this group, there is a greater risk of suffering from AKP than in the resurfacing group (Figure 8).
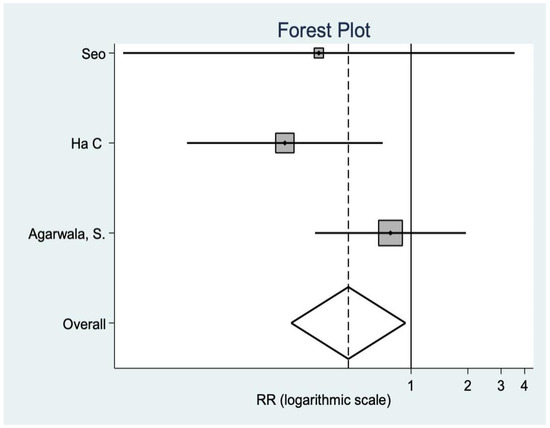
Figure 8.
Anterior knee pain data.
- Radiological variables
Radiological variables are not very constant throughout the literature. In this case, both the Insall ratio and the patellar tilt are found in three studies that show that there are no statistically significant differences between groups (Figure 9 and Figure 10).
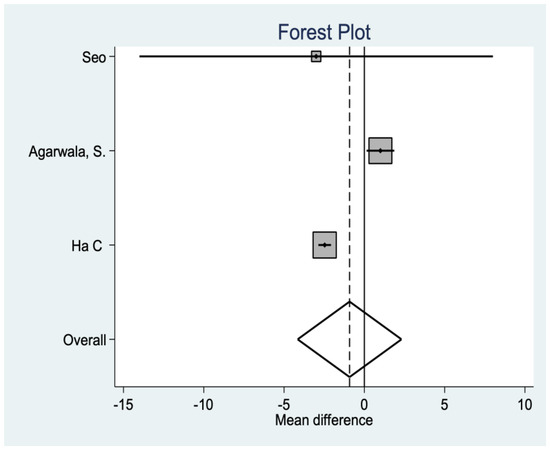
Figure 9.
Radiological variable data.
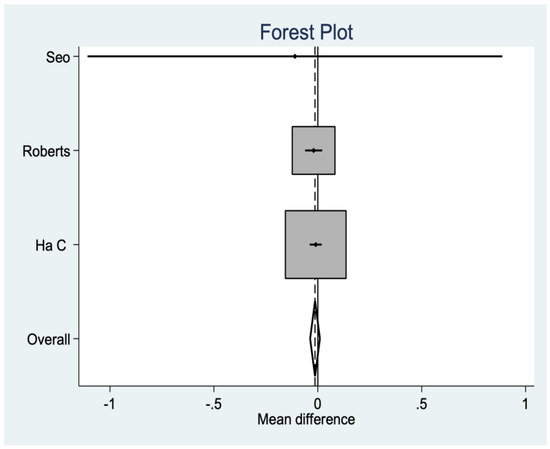
Figure 10.
Radiological variable data.
Although the clinical effect of each variable is not analyzed in any of the studies included in the meta-analysis, it seems reasonable to suggest that purely clinical variables such as ROM or functionality scales should have greater weight in daily clinical practice than, for example, the radiological variables studied, which have an application that is more academic than practical. This correlation between the variables is reflected in Table 3. The data obtained are summarized in Table 3.

Table 3.
Summary of results.
4. Discussion
The question of whether to replace the patella in a total knee replacement has been debated over the years. Several meta-analyses or systematic reviews of the literature have been conducted in an attempt to try to elucidate which is better. The most critical aspects seem to be the reduction of anterior knee pain and better functional outcomes in terms of the option to replace the patella, as opposed to complications such as patella fracture or loosening.
One of the most important variables is the revision rate, in which a greater tendency is observed in the non-resurfacing group, but, as has been postulated throughout the study, it does not seem clear that this higher revision rate could be attributable to patella replacement. In fact, this is the key point of the discussions in favor of one trend or another throughout the entire body of literature.
Regarding anterior knee pain, He et al. [26] reported a higher rate of AKP in the non-resurfacing group but without being statistically significant. Li et al. [27], in studies with more than 5 years of follow-up, did find significant differences, although the data were not consistent in the subgroup analysis. It seems that similar data were maintained throughout the literature [28,29,30], with varying degrees of statistical significance. Meanwhile, others, such as Arirachakaran et al. [31,32], observed that patellar denervation had a lower risk of AKP than patellar replacement, although these results were not statistically significant.
Longo et al. [33,34] more recently did observe significant differences in AKP as it was statistically higher in the non-resurfacing group, while other studies, such as Tang [35] or Teel [36], found no differences between groups.
In our study, we did find a significantly higher risk of AKP in the non-resurfacing group.
As we can see, it seems that, in the literature consulted, there are more studies that consider that anterior knee pain occurs more commonly in the non-resurfacing group than the other way around. Although we do not consider this to be critical in day-to-day clinical practice, the risk–benefit of systematically replacing the patella to avoid AKP, with the possible complications of AKP, should be studied.
The reoperation rate is another of the most studied variables in the literature. He [26] found a higher reoperation rate for patellofemoral problems in the non-resurfacing group. Li et al. [27] observed a higher reoperation rate, both absolute and due to femoropatellar problems, in the non-resurfacing group, with statistically significant results. Fu et al. [28] observed that the absolute risk of reoperation was reduced by 4% in the resurfacing group, meaning that approximately 25 patellae would need to be replaced to prevent one case of reoperation. Similar data were presented by Pavlou et al. [29], Chen et al. [31], and others [32,34,35,36,37,38].
In our case, a significantly higher risk of reintervention was observed in the non-resurfacing group.
On this point, it is true that most of the studies speak in favor of patellar replacement and we do consider in this case that it is something to be considered in clinical practice. We also believe that it should be studied in more depth because, although some studies do distinguish between cases due to the patella and those not due to the patella in their reoperation rates, others do not. The consequences and the magnitude of these consequences should also be considered.
The results of many meta-analyses consulted [26,27,28,29,31,33] showed no differences between groups. However, Pilling et al. [30] did observe differences in favor of the resurfacing group in KSS, and Teel [15] observed differences in both KSS and functional scores. Meanwhile, Aririchakaran [32] obtained worse results in the KSS functional score in the resurfacing group, but this was not significant. Longo et al. [34] did not observe differences in most of the functional tests but did find that the resurfacing group had statistically higher values in the HSS.
Likewise, Tang et al. [35] found no differences in the KSS, although, in the analysis by subgroups, they did observe that, in studies with 1–2-year follow-up, the resurfacing group presented significantly better data, which did not occur when the follow-up was longer than 2 years. In our case, we did find differences in favor of the resurfacing group in both KSS clinical and Feller, with KSS functional being inconclusive.
Here, again, there is a lack of consensus, with most studies finding a lack of differences between groups.
5. Conclusions
As stated in the Introduction, there are not many methodologically sound meta-analyses that include modern studies. In fact, this includes five modern clinical trials not found in other meta-analyses.
After analyzing different variables throughout the literature, it does seem clear that the non-resurfacing group may have a higher risk of reintervention than the resurfacing group. In terms of functional variables, we found some disparity. On some occasions, they seem to be in favor of the resurfacing group, as in our study, and others are not; thus, it seems sensible to suggest that these types of variables should not excessively condition the results regarding whether the patella is replaced or not replaced in a total knee prosthesis.
As for the radiological variables and the VAS of pain, no significant differences were observed, so they do not seem to have a great influence on the results either.
As a limitation, we note that the period of inclusion of the studies was limited to 10 years, with the possibility of omitting suitable studies carried out previously, although it is true that some of the meta-analyses consulted included previous studies.
One of the main strengths is the inclusion in the meta-analysis of the most recent clinical trials found on the subject, in addition to the analysis of variables not previously analyzed but which may be of great interest, such as the rate of deep infection, a serious clinical complication for both the patient and the surgeon. Since there are few studies that report this rate as such, which we consider to be of great clinical interest, we believe that our work indicates that it should be included in
future studies.
For all these reasons, we believe that, although it seems to have been demonstrated that not replacing the patella may precipitate a reintervention, we do not believe that it is necessary to replace the patella every time, because it is not clear whether this reintervention is a direct consequence of not replacing the patella or not, and doing it systematically may lead to greater consequences.
Therefore, in our opinion, treatment should be individualized for each patient.
Author Contributions
Conceptualization, A.D.-G., C.C.R., A.d.P.M.-R., S.C.S. and J.J.M.-V.; methodology, J.J.M.-V. and J.G.A.-H.; software G.C.-A. and L.M.D.; formal analysis, J.J.G.-B.; investigation, M.J., A.d.P.M.-R., S.C.S. and J.G.-S.; data curation, J.J.G.-B., M.J., J.G.-S. and A.D.-G. writing—original draft preparation, A.D.-G.; writing—review and editing, J.J.G.-B., M.J. and Á.L.-A.; visualization, Á.L.-A., A.D.-G., J.J.M.-V., J.G.A.-H., G.C.-A., L.M.D., J.J.G.-B., M.J. and J.G.-S.; supervision, J.J.G.-B. and M.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The study did not report any data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Schindler, O.S. The controversy of patellar resurfacing in total knee arthro- plasty: Ibisne in medio tutissimus? Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1227–1244. [Google Scholar] [CrossRef] [PubMed]
- Clements, W.J.; Miller, L.; Whitehouse, S.L.; Graves, S.E.; Ryan, P.; Crawford, R.W. Early outcomes of patella resurfacing in total knee arthroplasty. Acta Orthop. 2010, 81, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Helmy, N.; Anglin, C.; Greidanus, N.V.; Masri, B.A. To resurface or not to resurface the patella in total knee arthroplasty. Clin. Orthop. Relat. Res. 2008, 466, 2775–2778. [Google Scholar] [CrossRef][Green Version]
- Boyd, A.D., Jr.; Ewald, F.C.; Thomas, W.H.; Poss, R.; Sledge, C.B. Long-term complica- tions after total knee arthroplasty with or without resurfacing of the patella. J. Bone Jt. Surg. Am. 1993, 75, 674–681. [Google Scholar] [CrossRef] [PubMed]
- Park, B.K.; Paprosky, W.G. Patellar resurfacing in total knee arthroplasty. Semin. Arthroplast. 2015, 26, 232–235. [Google Scholar] [CrossRef]
- Schroeder-Boersch, H.; Scheller, G.; Fischer, J.; Jani, L. Advantages of patellar resurfacing in total knee arthroplasty. Two-year results of a prospective randomized study. Arch. Orthop. Trauma Surg. 1998, 117, 73–78. [Google Scholar] [CrossRef]
- Parvizi, J.; Rapuri, V.R.; Saleh, K.; Kuskowski, M.A.; Sharkey, P.F.; Mont, M.A. Failure to Resurface the Patella during Total Knee Arthroplasty May Result in More Knee Pain and Secondary Surgery. Clin. Orthop. Relat. Res. 2005, 438, 191–196. [Google Scholar] [CrossRef]
- Keblish, P.A.; Varma, A.K.; Greenwald, A.S. Patellar resurfacing or retention in total knee arthroplasty. A prospective study of patients with bilateral replacements. J. Bone Jt. Surg. Br. 1994, 76, 930–937. [Google Scholar] [CrossRef]
- Enis, J.E.; Gardner, R.; Robledo, M.A.; Latta, L.; Smith, R. Comparison of patellar resurfacing versus nonresurfacing in bilateral total knee arthroplasty. Clin. Orthop. Relat. Res. 1990, 260, 38–42. [Google Scholar] [CrossRef]
- Fern, E.D.; Winson, I.G.; Getty, C.J. Anterior knee pain in rheumatoid patients after total knee replacement. Possible selection criteria for patellar resurfacing. J. Bone Jt. Surg. Br. 1992, 74, 8. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Updated March 2011]; The Cochrane Collaboration: London, UK, 2011; Available online: www.handbook.cochra-ne.org (accessed on 12 January 2021).
- Teel, A.J.; Esposito, J.G.; Lanting, B.A.; Howard, J.L.; Schemitsch, E.H. Patellar Resurfacing in Primary Total Knee Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. J. Arthroplast. 2019, 34, 3124–3132. [Google Scholar] [CrossRef]
- Breeman, S.; Campbell, M.; Dakin, H.; Fiddian, N.; Fitzpatrick, R.; Grant, A.; Gray, A.; Johnston, L.; MacLennan, G.; Morris, R.; et al. Patellar resurfacing in total knee replacement: Five-year clinical and economic results of a large randomized controlled trial. J. Bone Jt. Surg. Ser. A 2011, 93, 1473–1481. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.S.; Kim, C.W.; Moon, S.W. A Comparison of Patella Retention versus Resurfacing for Moderate or Severe Patellar Articular Defects in Total Knee Arthroplasty: Minimum 5-year Follow-up Results. Knee Surg. Relat. Res. 2011, 23, 142–148. [Google Scholar] [CrossRef]
- Beaupre, L.; Secretan, C.; Johnston, D.; Lavoie, G. A Randomized controlled trial comparing patellar retention versus patellar resurfacing in primary total knee arthroplasty: 5–10 year follow-up. BMC Res. Notes 2012, 5, 273. [Google Scholar] [CrossRef]
- Roberts, D.W.; Hayes, T.D.; Tate, C.T.; Lesko, J.P. Selective patellar resurfacing in total knee arthroplasty: A prospective, randomized, double-blind study. J. Arthroplast. 2015, 30, 216–222. [Google Scholar] [CrossRef]
- Ali, A.; Lindstrand, A.; Nilsdotter, A.; Sundberg, M. Similar patient-reported outcomes and performance after total knee arthroplasty with or without patellar resurfacing: A randomized study of 74 patients with 6 years of follow-up. Acta Orthop. 2016, 87, 274–279. [Google Scholar] [CrossRef]
- Agarwala, S.; Shetty, V.; Karumuri, L.K.; Vijayvargiya, M. Patellar Resurfacing versus Nonresurfacing with Patellaplasty in Total Knee Arthroplasty. Indian J. Orthop. 2018, 52, 393–398. [Google Scholar]
- Kaseb, M.H.; Tahmasebi, M.N.; Mortazavi, S.M.J.; Sobhan, M.R.; Nabian, M.H. Comparison of clinical results between patellar resurfacing and non-resurfacing in total knee arthroplasty: A short term evaluation. Arch. Bone Jt. Surg. 2018, 6, 124–129. [Google Scholar] [PubMed]
- Kaseb, M.H.; Mortazavi SM, J.; Firoozabadi, M.A.; Toofan, H. Comparison between Patellar Resurfacing and Postoperative Satisfaction of Patients and Patellar. Arch. Bone Jt. Surg. 2019, 7, 441–444. [Google Scholar] [PubMed]
- Ha, C.; Wang, B.; Li, W.; Sun, K.; Wang, D.; Li, Q. Resurfacing versus not-resurfacing the patella in one-stage bilateral total knee arthroplasty: A prospective randomized clinical trial. Int. Orthop. 2019, 43, 2519–2527. [Google Scholar] [CrossRef] [PubMed]
- Chawla, L.; Bandekar, S.M.; Dixit, V.; Ambareesh, P.; Krishnamoorthi, A.; Mummigatti, S. Functional outcome of patellar resurfacing vs non resurfacing in Total Knee Arthoplasty in elderly: A prospective five year follow-up study. J. Arthrosc. Jt. Surg. 2018, 6, 65–69. [Google Scholar] [CrossRef]
- He, J.-Y.; Jiang, L.-S.; Dai, L.-Y. Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee 2011, 18, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Chen, Y.; Su, W.; Zhao, J.; He, S.; Luo, X. Systematic review of patellar resurfacing in total knee arthroplasty. Int. Orthop. 2010, 35, 305–316. [Google Scholar] [CrossRef]
- Fu, Y.; Wang, G.; Fu, Q. Patellar resurfacing in total knee arthroplasty for osteoarthritis: A meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1460–1466. [Google Scholar] [CrossRef]
- Pavlou, G.; Meyer, C.; Leonidou, A.; As-Sultany, M.; West, R.; Tsiridis, E. Patellar resurfacing in total knee arthroplasty: Does design matter? J. Bone Jt. Surg. Ser. A 2011, 93, 1301–1309. [Google Scholar] [CrossRef]
- Pilling, R.; Moulder, E.; Allgar, V.; Messner, J.; Sun, Z.; Mohsen, A. Patellar resurfacing in primary total knee replacement. J. Bone Jt. Surg. 2012, 94, 2270–2278. [Google Scholar] [CrossRef]
- Chen, K.; Li, G.; Fu, N.; Yuan, C.; Zhang, Q.; Cai, Z. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: A meta-analysis of randomised controlled trials. Int. Orthop. 2013, 37, 1075–1083. [Google Scholar] [CrossRef]
- Arirachakaran, A.; Sangkaew, C.; Kongtharvonskul, J. Patellofemoral resurfacing and patellar denervation in primary total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1770–1781. [Google Scholar] [CrossRef] [PubMed]
- Findlay, I.; Wong, F.; Smith, C.; Back, D.; Davies, A.; Ajuied, A. Non-resurfacing techniques in the management of the patella at total knee arthroplasty: A systematic review and meta-analysis. Knee 2016, 23, 191–197. [Google Scholar] [CrossRef]
- Longo, U.G.; Ciuffreda, M.; Mannering, N.; D’Andrea, V.; Cimmino, M.; Denaro, V. Patellar Resurfacing in Total Knee Arthroplasty: Systematic Review and Meta-Analysis. J. Arthroplast. 2018, 33, 620–632. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.-B.; Wang, J.; Dong, P.-L.; Zhou, R. A Meta-Analysis of Patellar Replacement in Total Knee Arthroplasty for Patients With Knee Osteoarthritis. J. Arthroplast. 2018, 33, 960–967. [Google Scholar] [CrossRef]
- Serbest, S.; Tiftikçi, U.; Karaaslan, F.; Tosun, H.B.; Sevinç, H.F.; Balci, M. A neglected case of giant synovial chondromatosis in knee joint. Pan Afr. Med. J. 2015, 22, 5. [Google Scholar] [CrossRef] [PubMed]
- Tiftikçi, U.; Serbest, S.; Burulday, V. Can Achilles tendon be used as a new distal landmark for coronal tibial component alignment in total knee replacement surgery? An observational MRI study. Ther. Clin. Risk Manag. 2017, 13, 81–86. [Google Scholar] [CrossRef]
- Oğurel, T.; Serbest, S.; Oğurel, R.; Tiftikçi, U.; Ölmez, Y. Blood chromium-cobalt levels in patients after total knee arthroplasty and their effect on the retinal nerve fiber layer and macular ganglion cell complex. Retina 2020, 40, 1200–1206. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).