Transosseous Suturing for the Correction of Juvenile Hallux Valgus: A Preliminary Case Series Study
Abstract
1. Introduction
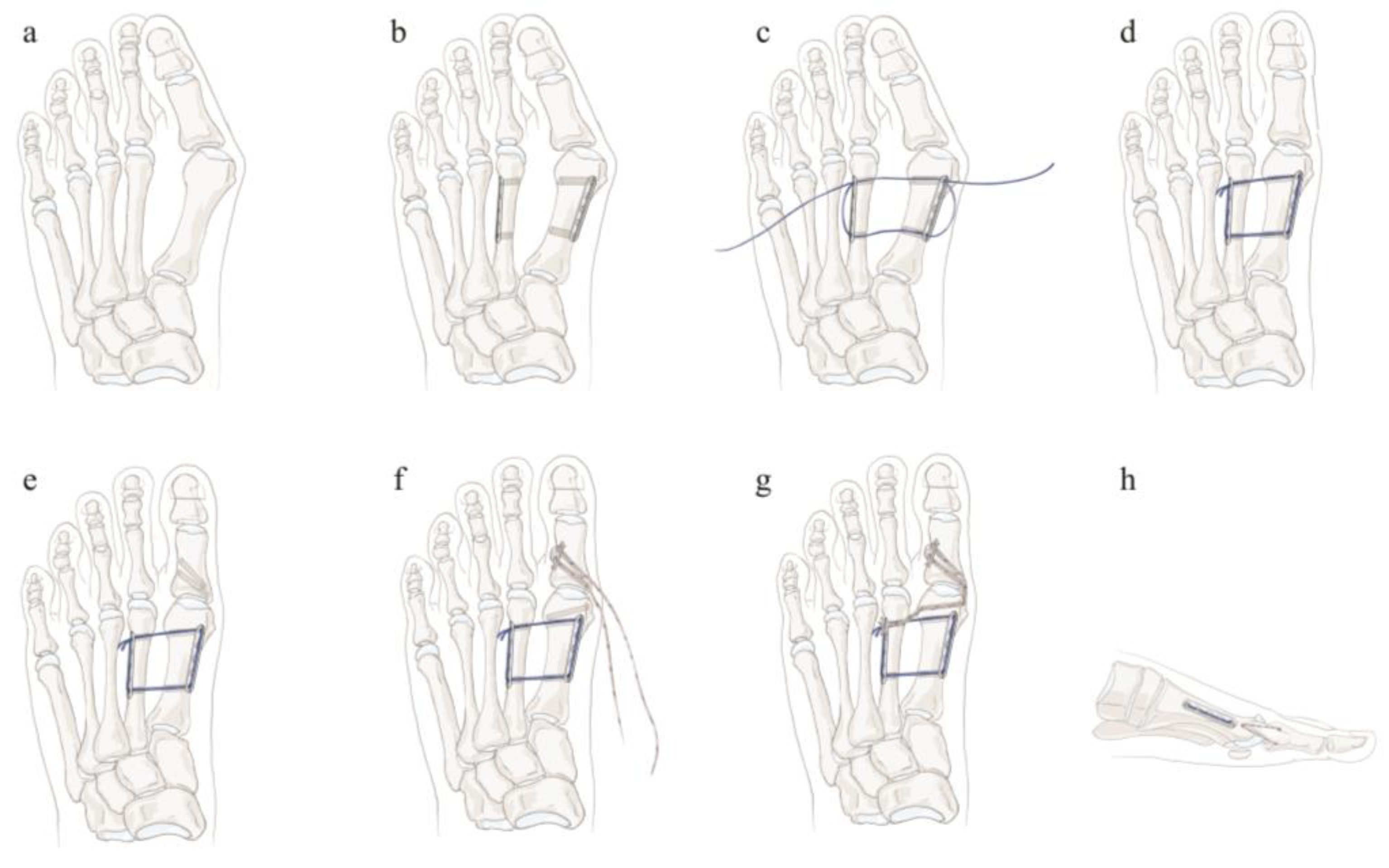
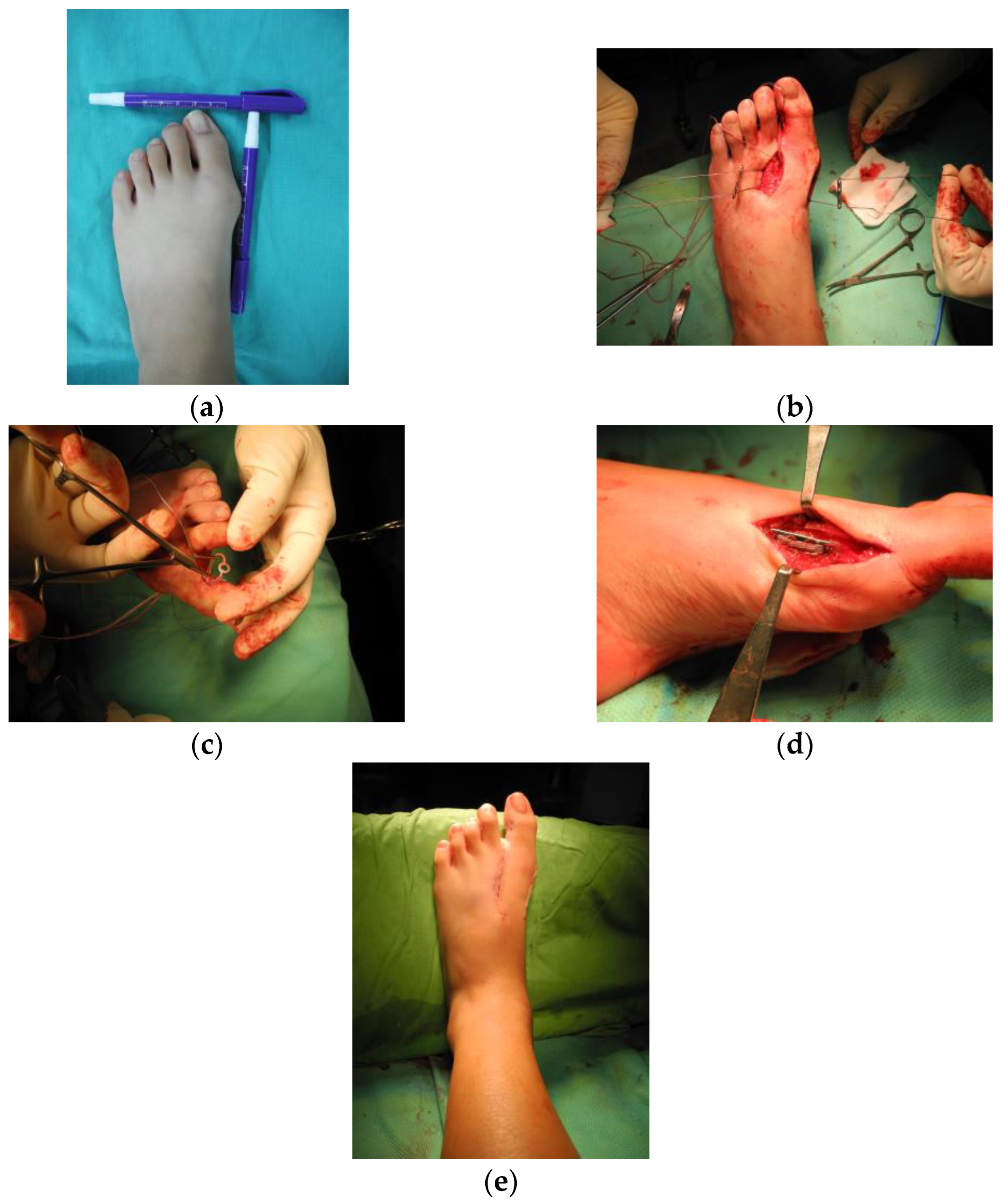
2. Materials and Methods
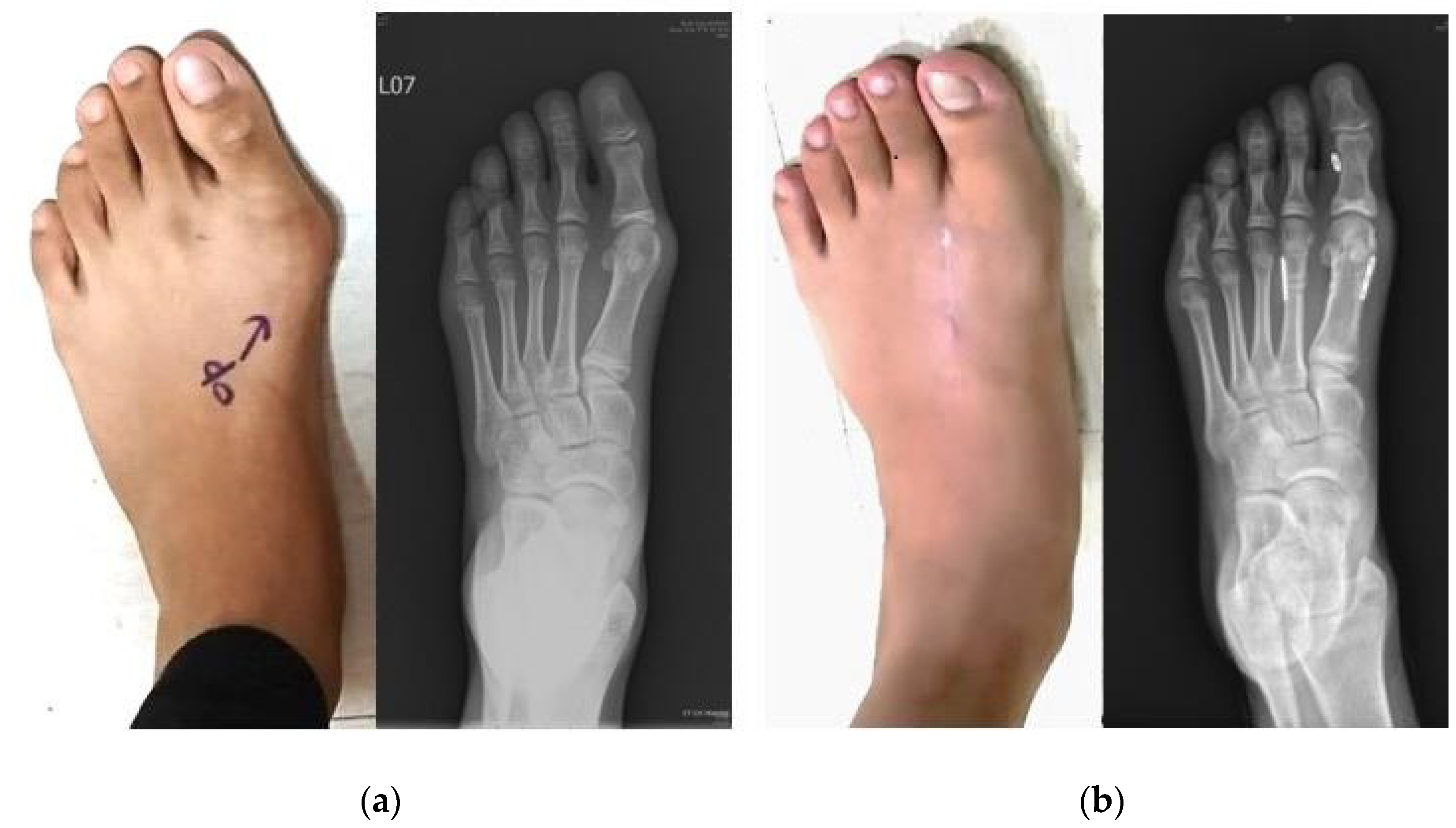
3. Results
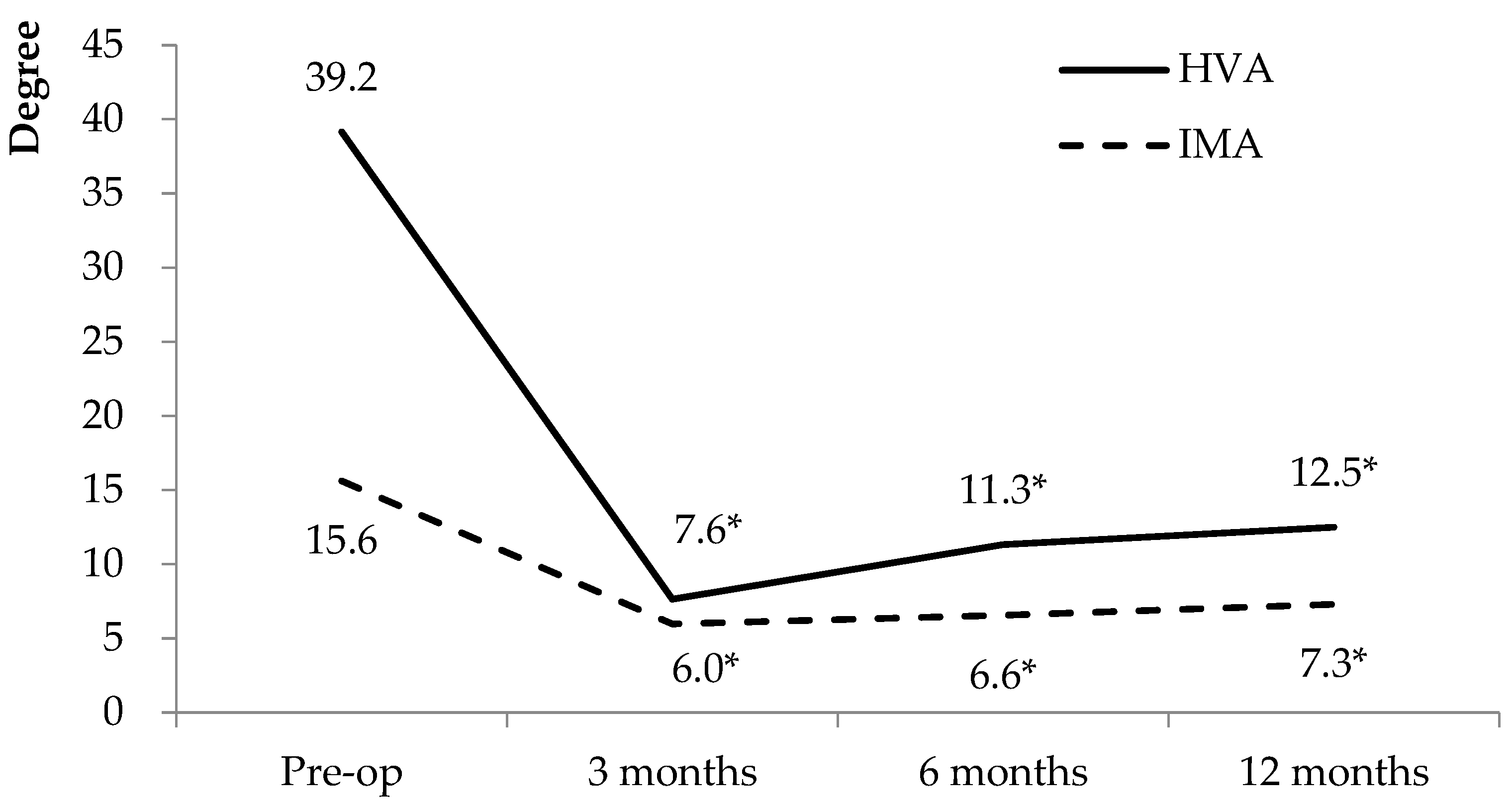
3.1. Radiographic Outcomes
3.2. Functional Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chell, J.; Dhar, S. Pediatric Hallux Valgus. Foot Ankle Clin. 2014, 19, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.W.; Park, K.B.; Kwak, Y.H.; Jin, S.; Park, H. Radiographic Assessment of Foot Alignment in Juvenile Hallux Valgus and Its Relationship to Flatfoot. Foot Ankle Int. 2019, 40, 1079–1086. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, P.; Livingston, K.; Miller, P.E.; May, C.; Mahan, S. Radiographic Evaluation of First Metatarsal and Medial Cuneiform Morphology in Juvenile Hallux Valgus. Foot Ankle Int. 2018, 39, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, M.J.; Michael, J. Juvenile Hallux Valgus: Etiology and Treatment. Foot Ankle Int. 1995, 16, 682–697. [Google Scholar] [CrossRef] [PubMed]
- Halebian, J.D.; Gaines, S.S. Juvenile hallux valgus. J. Foot Surg. 1983, 22, 290–293. [Google Scholar] [PubMed]
- Harb, Z.; Kokkinakis, M.; Ismail, H.; Spence, G. Adolescent hallux valgus: A systematic review of outcomes following surgery. J. Child. Orthop. 2015, 9, 105–112. [Google Scholar] [CrossRef]
- Kilmartin, T.E.; Barrington, R.L.; Wallace, W.A. A controlled prospective trial of a foot orthosis for juvenile hallux valgus. J. Bone Jt. Surg. Br. 1994, 76, 210–214. [Google Scholar] [CrossRef]
- Yucel, I.; Tenekecioglu, Y.; Ogut, T.; Kesmezacar, H. Treatment of hallux valgus by modified McBride procedure: A 6-year follow-up. J. Orthop. Traumatol. 2010, 11, 89–97. [Google Scholar] [CrossRef]
- Ball, J.; Sullivan, J.A. Treatment of the Juvenile Bunion by Mitchell Osteotomy. Orthopedics 1985, 8, 1249–1252. [Google Scholar] [CrossRef]
- Scranton, P.E., Jr.; Zuckerman, J.D. Bunion Surgery in Adolescents: Results of surgical treatment. J. Pediatr. Orthop. 1984, 4, 39–43. [Google Scholar] [CrossRef]
- George, H.L.; Casaletto, J.; Unnikrishnan, P.N.; Shivratri, D.; James, L.A.; Bass, A.; Bruce, C.E. Outcome of the scarf osteotomy in adolescent hallux valgus. J. Child. Orthop. 2009, 3, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, Y.; Bajaj, S.K.; Flowers, M.J. Scarf–Akin osteotomy for hallux valgus in juvenile and adolescent patients. J. Pediatr. Orthop. B 2015, 24, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Chiang, M.-H.; Wang, T.-M.; Kuo, K.N.; Huang, S.-C.; Wu, K.-W. Management of Juvenile Hallux Valgus Deformity: The role of combined Hemiepiphysiodesis. BMC Musculoskelet. Disord. 2019, 20, 472. [Google Scholar] [CrossRef] [PubMed]
- Herring, J.A. Tachdjian’s Pediatric Orthopaedics; Saunders/Elsevier: Philadelphia, PA, USA, 2020. [Google Scholar]
- Holmes, G.B., Jr.; Hsu, A.R. Correction of Intermetatarsal Angle in Hallux Valgus Using Small Suture Button Device. Foot Ankle Int. 2013, 34, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Dayton, P.; Sedberry, S.; Feilmeier, M. Complications of Metatarsal Suture Techniques for Bunion Correction: A Systematic Review of the Literature. J. Foot Ankle Surg. 2015, 54, 230–232. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical Rating Systems for the Ankle-Hindfoot, Midfoot, Hallux, and Lesser Toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef]
- Agnew, P. Pediatric First Ray Deformities. Clin. Podiatr. Med. Surg. 2013, 30, 491–501. [Google Scholar] [CrossRef]
- Johnson, J.E.; Clanton, T.O.; Baxter, D.E.; Gottlieb, M.S. Comparison of Chevron Osteotomy and Modified McBride Bunionectomy for Correction of Mild to Moderate Hallux Valgus Deformity. Foot Ankle 1991, 12, 61–68. [Google Scholar] [CrossRef]
- Choi, G.W.; Kim, H.J.; Kim, T.S.; Chun, S.K.; Kim, T.W.; Lee, Y.I.; Kim, K.H. Comparison of the Modified McBride Procedure and the Distal Chevron Osteotomy for Mild to Moderate Hallux Valgus. J. Foot Ankle Surg. 2016, 55, 808–811. [Google Scholar] [CrossRef]
- Filippi, J.; Briceno, J. Complications after Metatarsal Osteotomies for Hallux Valgus: Malunion, Nonunion, Avascular Necrosis, and Metatarsophalangeal Osteoarthritis. Foot Ankle Clin. 2019, 25, 169–182. [Google Scholar] [CrossRef]
- Barg, A.; Harmer, J.R.; Presson, A.P.; Zhang, C.; Lackey, M.; Saltzman, C.L. Unfavorable Outcomes Following Surgical Treatment of Hallux Valgus Deformity: A Systematic Literature Review. J. Bone Jt. Surg. 2018, 100, 1563–1573. [Google Scholar] [CrossRef] [PubMed]
- Kayiaros, S.; Blankenhorn, B.D.; Dehaven, J.; Van Lancker, H.; Sardella, P.; Pascalides, J.T.; DiGiovanni, C.W. Correction of Metatarsus Primus Varus Associated with Hallux Valgus Deformity Using the Arthrex Mini TightRope: A report of 44 cases. Foot Ankle Spéc. 2011, 4, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Weatherall, J.M.; Chapman, C.B.; Shapiro, S.L. Postoperative Second Metatarsal Fractures Associated with Suture-Button Implant in Hallux Valgus Surgery. Foot Ankle Int. 2013, 34, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Lui, T.H.; Chan, K.B. Technical tip: Reconstruction of medial collateral ligament in correction of hallux valgus deformity with primary medial collateral ligamentous insufficiency. Foot Ankle Surg. 2011, 18, 66–73. [Google Scholar] [CrossRef] [PubMed]

| Patient No. | Sex | Age (Years) | Side | Follow-Up (Months) | AOFAS (0–100) | |
|---|---|---|---|---|---|---|
| Pre-Op | Final Follow-Up | |||||
| 1 | F | 15 | L | 35.0 | 59 | 85 |
| 2 | F | 13 | L | 42.2 | 54 | 88 |
| 3 | F | 11 | L | 48.2 | 54 | 93 |
| 4 | F | 12 | L | 21.5 | 54 | 83 |
| 4 | F | 13 | R | 15.9 | 54 | 80 |
| 5 | F | 15 | L | 50.0 | 49 | 87 |
| 6 | F | 11 | L | 12.0 | 49 | 92 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, W.-C.; Yao, S.-H.; Wang, T.-M.; Chen, C.-H. Transosseous Suturing for the Correction of Juvenile Hallux Valgus: A Preliminary Case Series Study. Medicina 2022, 58, 1679. https://doi.org/10.3390/medicina58111679
Hung W-C, Yao S-H, Wang T-M, Chen C-H. Transosseous Suturing for the Correction of Juvenile Hallux Valgus: A Preliminary Case Series Study. Medicina. 2022; 58(11):1679. https://doi.org/10.3390/medicina58111679
Chicago/Turabian StyleHung, Wei-Chen, Shu-Hsin Yao, Ting-Ming Wang, and Chun-Ho Chen. 2022. "Transosseous Suturing for the Correction of Juvenile Hallux Valgus: A Preliminary Case Series Study" Medicina 58, no. 11: 1679. https://doi.org/10.3390/medicina58111679
APA StyleHung, W.-C., Yao, S.-H., Wang, T.-M., & Chen, C.-H. (2022). Transosseous Suturing for the Correction of Juvenile Hallux Valgus: A Preliminary Case Series Study. Medicina, 58(11), 1679. https://doi.org/10.3390/medicina58111679






