Treatment of Radial Nerve Palsy in Paediatric Humeral Shaft Fractures—STROBE-Compliant Investigation
Abstract
1. Introduction
2. Materials and Methods
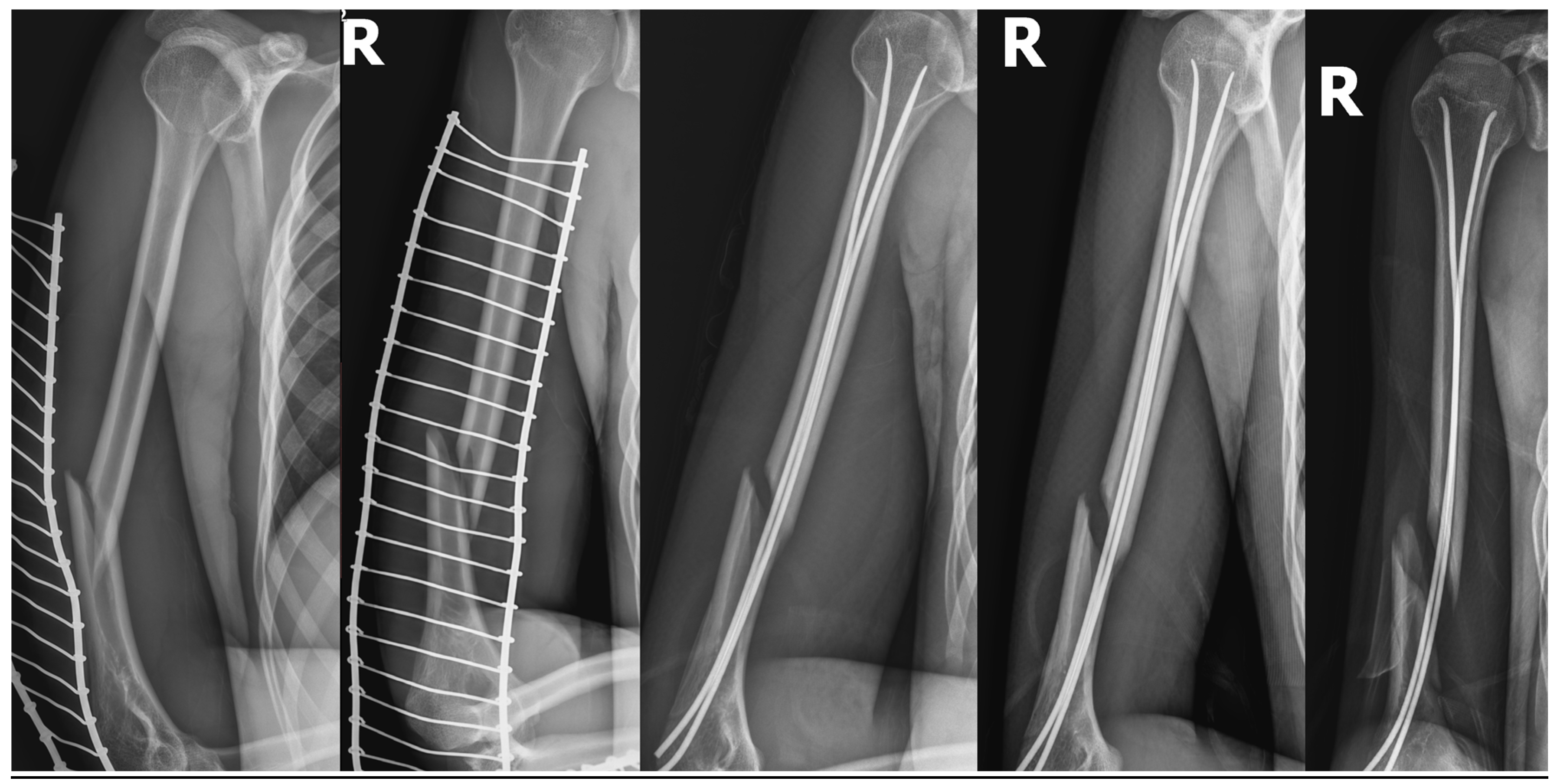
2.1. Case 1
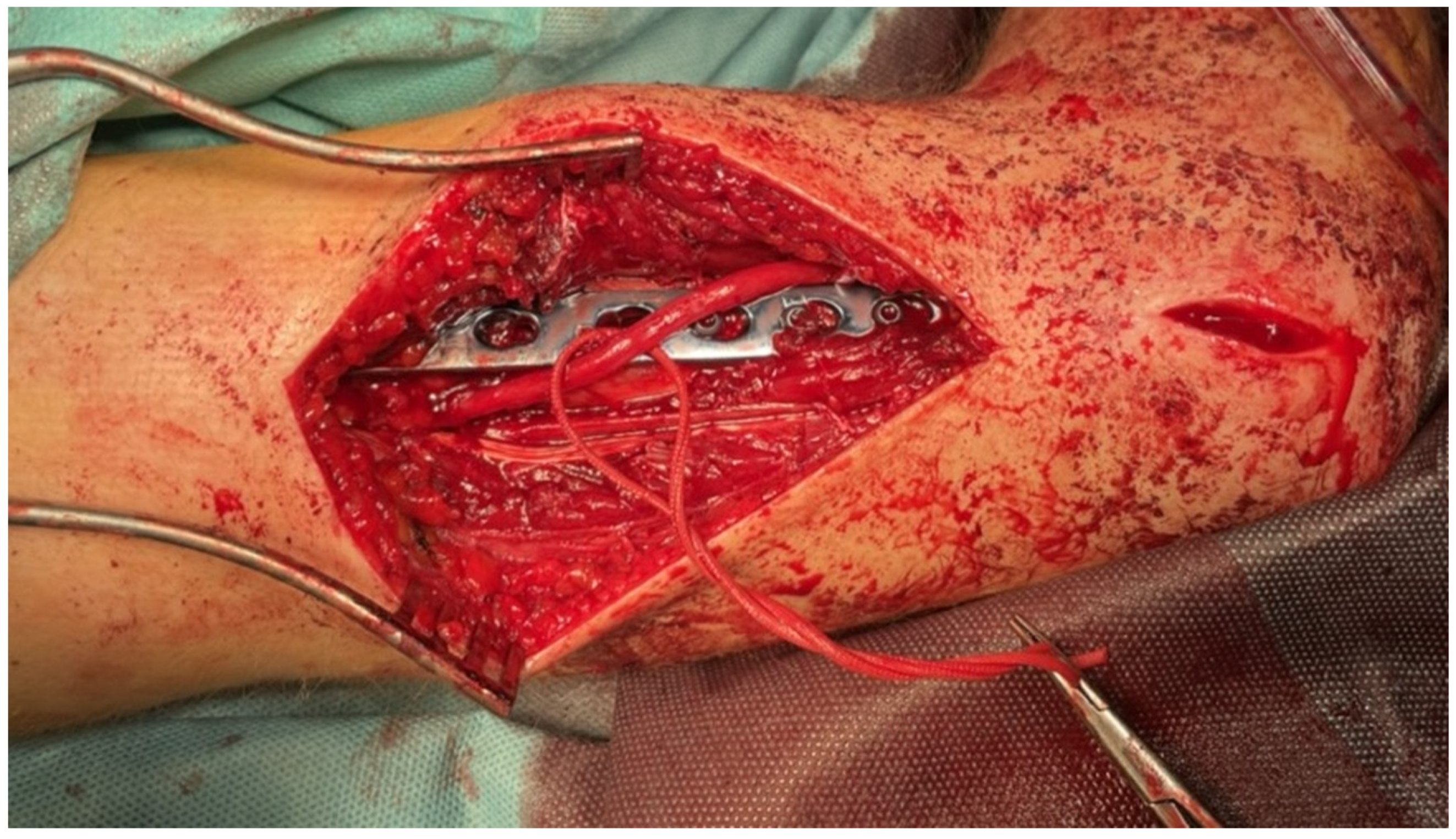
2.2. Case 2
2.3. Case 3
2.4. Case 4
2.5. Case 5
2.6. Case 6
3. Results
4. Discussion
4.1. Electrophysiological Studies
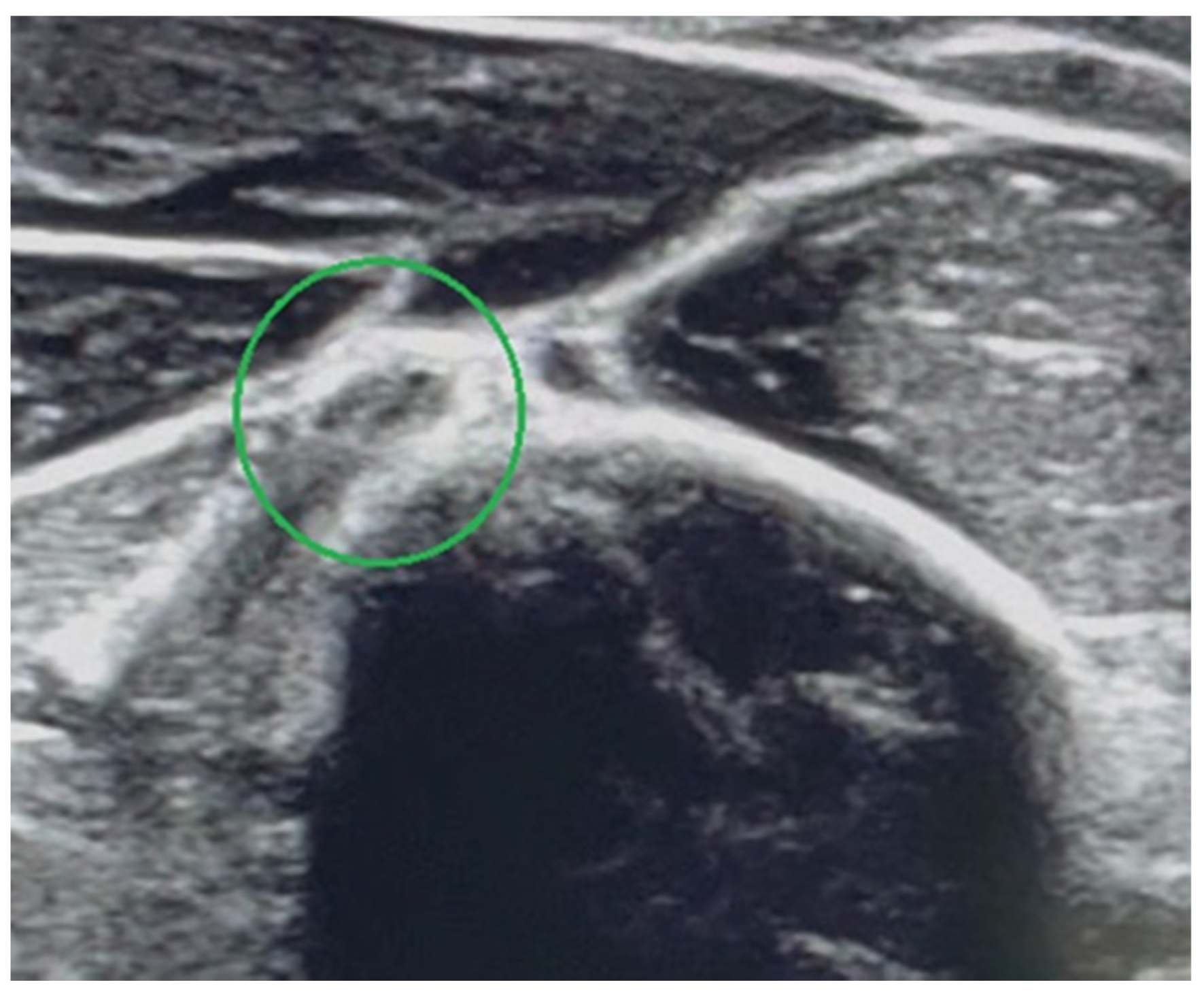
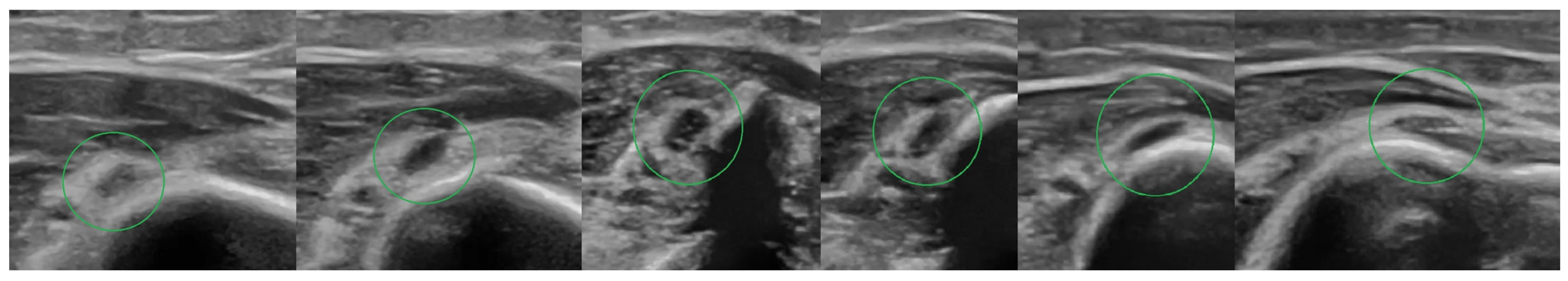
4.2. Ultrasound Examination
4.3. Relationship between the Level of Fracture and the Radial Nerve Damage
4.4. Patient Management and Treatment Options
4.5. Surgical Techniques
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology. |
| EMG | electromyography. |
| US | ultrasound. |
| BMRC | British Medical Research Council. |
| CRIF/FIN | close reduction and internal fixation/flexible intramedullary nailing. |
| ORIF | open reduction with internal fixation. |
| MCP | metacarpophalangeal joint. |
References
- Caviglia, H.; Garrido, C.P.; Palazzi, F.F.; Meana, N.V. Pediatric fractures of the humerus. Clin. Orthop. Relat. Res. 2005, 432, 49–56. [Google Scholar] [CrossRef]
- Rennie, L.; Court-Brown, C.M.; Mok, J.Y.; Beattie, T.F. The epidemiology of fractures in children. Injury 2007, 38, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Barr, L.V. Paediatric supracondylar humeral fractures: Epidemiology, mechanisms and incidence during school holidays. J. Child Orthop. 2014, 8, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Abrams, R.A.; Ziets, R.J.; Lieber, R.L.; Botte, M.J. Anatomy of the radial nerve motor branches in the forearm. J. Hand Surg. Am. 1997, 22, 232–237. [Google Scholar] [CrossRef]
- Bumbasirevic, M.; Palibrk, T.; Lesic, A.; Atkinson, H.D.E. Radial nerve palsy. EFORT Open Rev. 2017, 1, 286–294. [Google Scholar] [CrossRef]
- Shao, Y.C.; Harwood, P.; Grotz, M.R.; Limb, D.; Giannoudis, P.V. Radial nerve palsy associated with fractures of the shaft of the humerus: A systematic review. J. Bone Joint Surg. 2005, 87-B, 1647–1652. [Google Scholar] [CrossRef]
- Pollock, F.H.; Drake, D.; Bovill, E.G.; Day, L.; Trafton, P.G. Treatment of radial neuropathy associated with fractures of the humerus. J. Bone Joint Surg. 1981, 63-A, 239–243. [Google Scholar] [CrossRef]
- Larsen, L.B.; Barfred, T. Radial nerve palsy after simple fracture of the humerus. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2000, 34, 363–366. [Google Scholar] [PubMed]
- Chapman, J.R.; Henley, M.B.; Agel, J.; Benca, P.J. Randomized prospective study of humeral shaft fracture fixation: Intramedulllary nails versus plates. J. Orthop. Trauma. 2000, 14, 162–166. [Google Scholar] [CrossRef]
- Bumbaširević, M.; Lešić, A.; Bumbaširević, V.; Čobeljić, G.; Milošević, I.; Atkinson, H.D.E. The management of humerał shaft fractures with associated radial nerve palsy: A review of 117 cases. Arch. Orthop. Trauma. Surg. 2010, 130, 519–522. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Compston, A. Aids to the investigation of peripheral nerve injuries. Brain 2010, 133, 2838–2844. [Google Scholar] [CrossRef] [PubMed]
- O’Shaughnessy, M.A.; Parry, J.A.; Liu, H.; Stans, A.A.; Larson, A.N.; Milbrandt, T.A. Management of paediatric humeral shaft fractures and associated nerve palsy. J. Child Orthop. 2019, 13, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Karabay, N.; Toros, T.; Ademoğlu, Y.; Ada, S. Ultrasonographic evaluation of the iatrogenic peripheral nerve injuries in upper extremity. Eur. J. Radiol. 2010, 73, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Peer, S.; Bodner, G.; Meirer, R.; Willeit, J.; Piza-Katzer, H. Examination of postoperative peripheral nerve lesions with high-resolution sonography. AJR Am. J. Roentgenol. 2001, 177, 415–419. [Google Scholar] [CrossRef] [PubMed]
- DeFranco, M.J.; Lawton, J.N. Radial nerve injuries associated with humeral fractures. J. Hand Surg. Am. 2006, 31, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Ricci, F.P.F.M.; Barbosa, R.I.; Elui, V.M.C.; Barbieri, C.H.; Mazzer, N.; Fonseca, M.D.C.R. Radial nerve injury associated with humeral shaft fracture: A retrospective study. Acta. Ortop. Bras. 2015, 23, 19–21. [Google Scholar] [CrossRef]
- Payne, S.H., Jr. Nerve repair and grafting in the upper extremity. J. South Orthop. Assoc. 2001, 10, 173–189. [Google Scholar]
- Robinson, L.R. Traumatic injury to peripheral nerves. Muscle Nerve 2000, 23, 863–873. [Google Scholar] [CrossRef]
- Bertelli, J.; Soldado, F.; Ghizoni, M.F. Outcomes of Radial Nerve Grafting In Children after Distal Humerus Fracture. J. Hand Surg. Am. 2018, 43, 1140. [Google Scholar] [CrossRef]
- Bodner, G.; Buchberger, W.; Schocke, M.; Bale, R.; Huber, B.; Harpf, C.; Gassner, E.; Jaschke, W. Radial nerve palsy associated with humeral shaft fracture: Evaluation with USA—Initial experience. Radiology 2001, 219, 811–816. [Google Scholar] [CrossRef]
- Holstein, A.; Lewis, G.B. Fractures of the humerus with radial nerve paralysis. J. Bone Jt. Surg. 1963, 45, 1382–1388. [Google Scholar] [CrossRef]
- Ekholm, R.; Ponzer, S.; Törnkvist, H.; Adami, J.; Tidermark, J. Primary radial nerve palsy in patients with acute humeral shaft fractures. J. Orthop. Trauma. 2008, 22, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Ilyas, A.M.; Mangan, J.J.; Graham, J. Radial Nerve Palsy Recovery with Fractures of the Humerus: An Updated Systematic Review. J. Am. Acad. Orthop. Surg. 2020, 28, e263–e269. [Google Scholar] [CrossRef]
- Kim, D.H.; Kam, A.C.; Chandika, P.; Tiel, R.L.; Kline, D.G. Surgical management and outcome in patients with radial nerve lesions. J. Neurosurg. 2001, 95, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Lowe, J.B., 3rd; Sen, S.K.; Mackinnon, S.E. Current approach to radial nerve paralysis. Plast. Reconstr. Surg. 2002, 110, 1099–1113. [Google Scholar]
- Korompilias, A.V.; Lykissas, M.G.; Kostas-Agnantis, I.P.; Vekris, M.D.; Soucacos, P.N.; Beris, A.E. Approach to radial nerve palsy caused by humerus shaft fracture: Is primary exploration necessary? Injury 2013, 44, 323–326. [Google Scholar] [CrossRef]
| No. | Sex/Age | Fracture Type | Injury Mechanism | Accompanying Injuries | Type of Nerve Damage | Type of Intervention | Treatment Effect. | Follow -Up |
|---|---|---|---|---|---|---|---|---|
| 1. | Boy/8.6 years | Close/ Simple spiral/Middle thirds AO 12A1b | Low-energy trauma | Neuropraxia | CRIF/FIN expectant observation | spontaneous recovery after 2.5 months | 30 months | |
| 2. | Girl/16.3 years | Close/ Simple oblique/Distal thirds AO 12A2c | High-energy trauma/fall from 8 m | Lungs contusion. Bilateral pneumothorax. Fracture of the sacrum. | Neurotmesis | ORIF/titan plate + nerve reconstruction with a sural nerve cable graft. | recovery after 7.5 months | 20 months |
| 3. | Boy/13.5 years | Close/ Simple transverse/Distal thirds AO 12A3c | Low-energy trauma | Entrapment between bone fragments | ORIF/titan plate + nerve exploration 23 days after injury—2 days after nerve palsy. | recovery after 3.3 months | 8 months | |
| 4. | Boy/17.2 years | Open GA 1/ Intact wedge/Distal thirds AO 12B2c | High-energy trauma/fall from 6 m | Right scapula fracture. Multifragmentary fracture of the left distal forearm. Stable Th8 compression fracture. Left lateral mass fracture of the sacrum. Right iliac wing fracture. Right pubic bone fracture. Lungs contusion with a minor bilateral pneumothorax. | Entrapment between bone fragments | CRIF/external fixator ORIF/titan plate + nerve exploration 16 days after injury | recovery after 4.6 months | 16 months |
| 5. | Boy/12.3 years | Open GA 2/Simple transverse/Distal thirds AO 12A3c | High-energy trauma/hit by a car | Numerous wounds and bruises. Lung contusion. Right distal radius fracture. | Neurotmesis | ORIF/FIN with no nerve exploration due to wound contamination; implant removal + nerve reconstruction with a sural nerve cable graft 4.5 months after injury. | recovery 5.5 months after nerve reconstruction/15.5 months after injury! | 18 months |
| 6. | Boy/17.5 years | Close/ Simple spiral/Distal thirds AO 12A1c | Low-energy trauma | Stretching over the bone fragments | CRIF/FIN ORIF/titan plate + nerve exploration 56 days after injury—slowly progressive palsy. | recovery after 2 months | 5 months |
| Grade | Muscle Power |
|---|---|
| 0 | no contraction |
| 1 | flicker or trace of contraction |
| 2 | active movement, with gravity eliminated |
| 3 | active movement, against gravity |
| 4 | active movement, against gravity and resistance |
| 5 | normal power |
| No. | Wrist Extension | Fingers Extension | Thumb Extension | Active Wrist Extension Strength (BMRC) | Active Finger Extension (BMRC) | Active Thumb Extension (BMRC) | Skin Sensations Disturbances | Final Follow-Up (Months) |
|---|---|---|---|---|---|---|---|---|
| 1. | No deficit | No deficit | No deficit | M5 | M5 | M5 | No deficit | 6 |
| 2. | 10° deficit | No deficit | 10° deficit/MCP joint | M4 | M4 | M4 | Reduced skin sensation on radio-dorsal part of hand | 9 |
| 3. | 10° deficit | No deficit | No deficit | M4 | M4 | M4 | No deficit | 9 |
| 4. | 10° deficit | 10° deficit/MCP joint | No deficit | M4 | M4 | M4 | No deficit | 9 |
| 5. | 15° deficit | 10° deficit/MCP joint | 10° deficit/MCP joint | M4 | M4 | M4 | Reduced skin sensation on radio-dorsal part of hand | 18 |
| 6. | 10° deficit | 10° deficit/MCP joint | 10° deficit/MCP joint | M4 | M4 | M4 | Reduced skin sensation on radio-dorsal part of hand | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wiktor, Ł.; Tomaszewski, R. Treatment of Radial Nerve Palsy in Paediatric Humeral Shaft Fractures—STROBE-Compliant Investigation. Medicina 2022, 58, 1571. https://doi.org/10.3390/medicina58111571
Wiktor Ł, Tomaszewski R. Treatment of Radial Nerve Palsy in Paediatric Humeral Shaft Fractures—STROBE-Compliant Investigation. Medicina. 2022; 58(11):1571. https://doi.org/10.3390/medicina58111571
Chicago/Turabian StyleWiktor, Łukasz, and Ryszard Tomaszewski. 2022. "Treatment of Radial Nerve Palsy in Paediatric Humeral Shaft Fractures—STROBE-Compliant Investigation" Medicina 58, no. 11: 1571. https://doi.org/10.3390/medicina58111571
APA StyleWiktor, Ł., & Tomaszewski, R. (2022). Treatment of Radial Nerve Palsy in Paediatric Humeral Shaft Fractures—STROBE-Compliant Investigation. Medicina, 58(11), 1571. https://doi.org/10.3390/medicina58111571







