Benefits of Virtual Reality Program and Motor Imagery Training on Balance and Fall Efficacy in Isolated Older Adults: A Randomized Controlled Trial
Abstract
1. Introduction
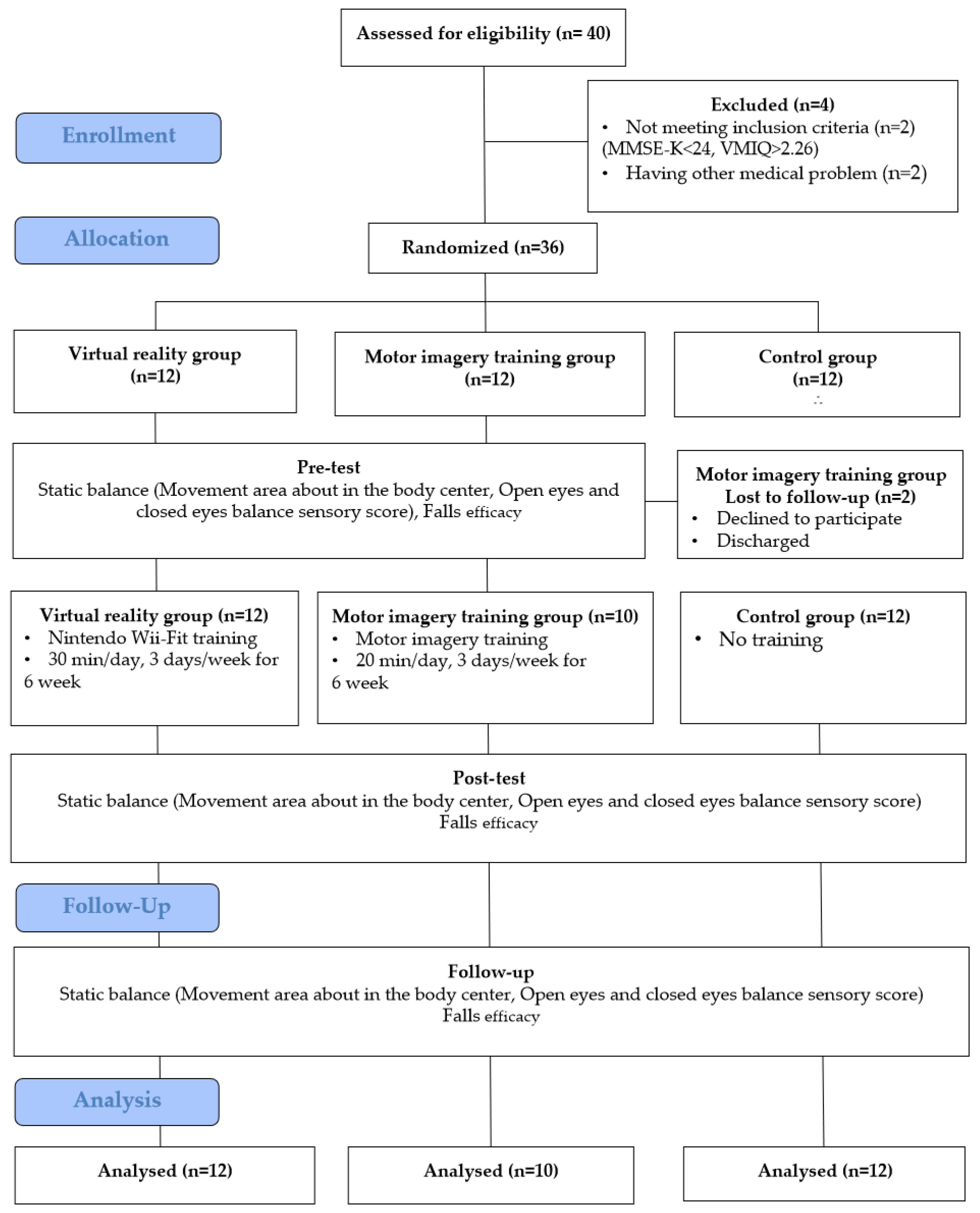
2. Materials and Methods
2.1. Design and Participants
2.2. Patient Safety Precautions and Compliance
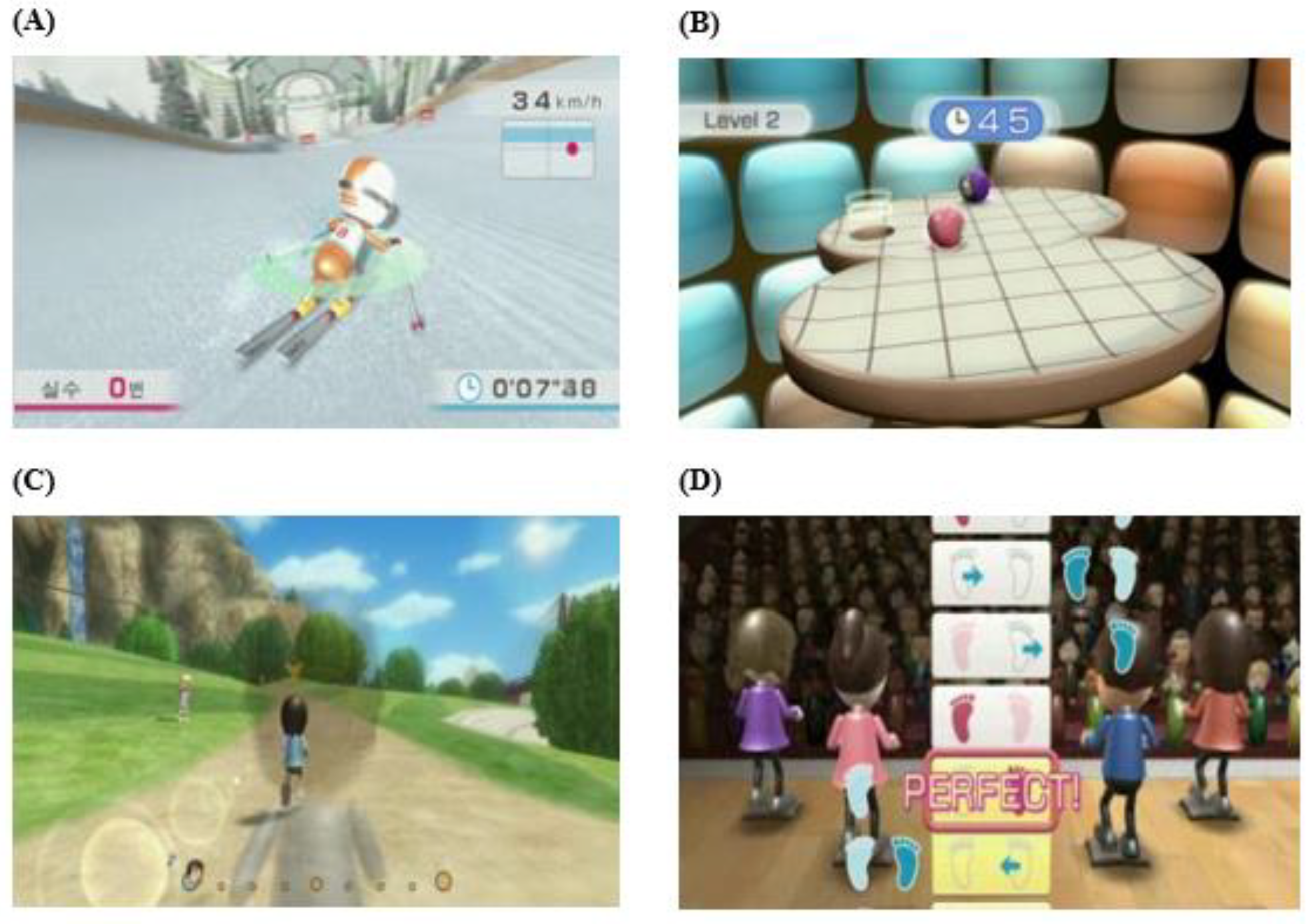
2.3. Intervention Method
2.4. Measurement
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Participants
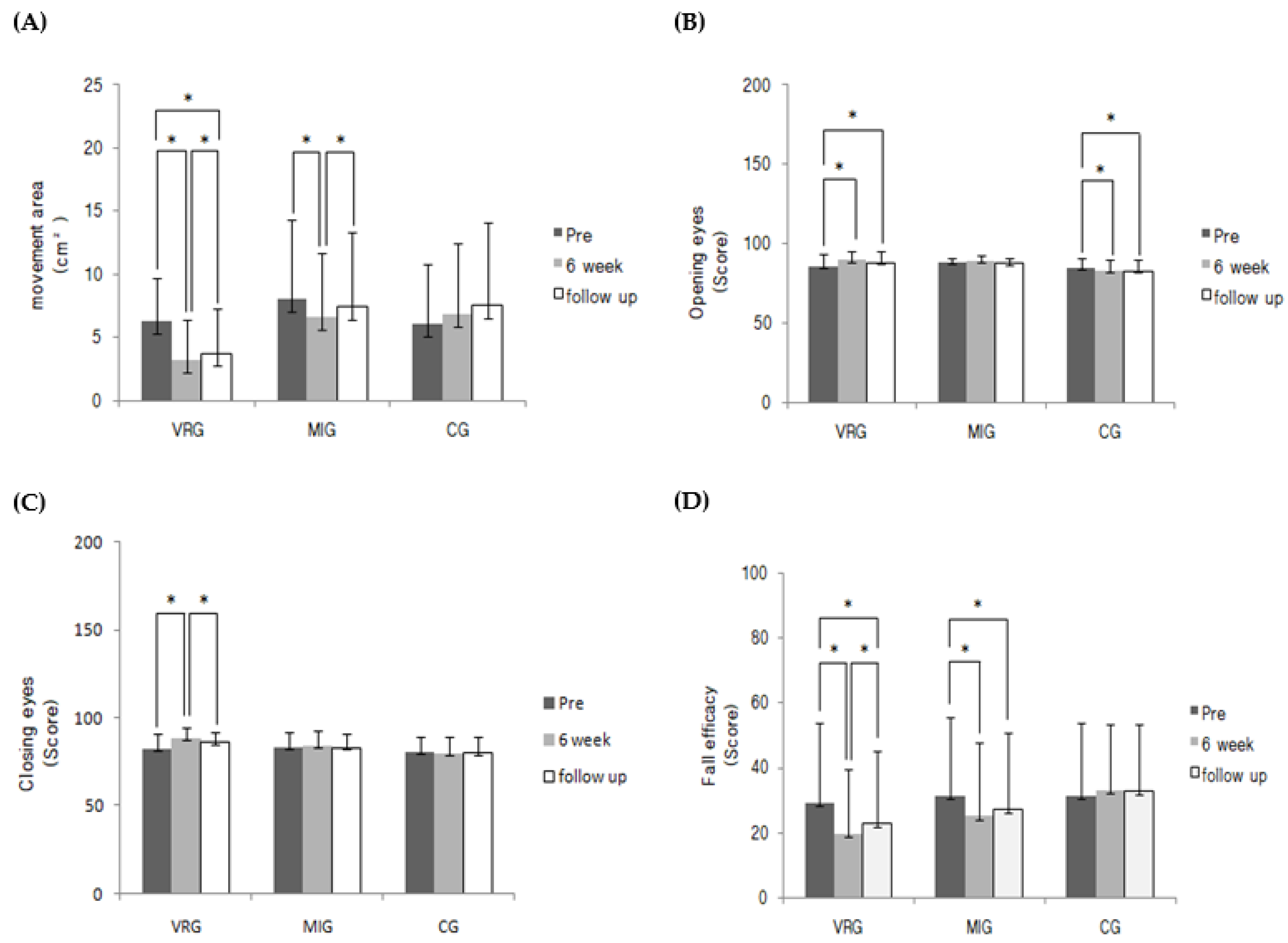
3.2. Comparison of Static Balance Ability of Each Group
3.3. Comparison of Changes in Fall Efficacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID–19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- De La Cámara, M.Á.; Jiménez–Fuente, A.; Pardos, A.I. Falls in older adults: The new pandemic in the post COVID–19 era? Med. Hypotheses 2020, 145, 110321. [Google Scholar] [CrossRef]
- Miciano, A.S.; Cross, C.L. Poster 9: The Body Function, Activity Limitation, and Participation Restrictions of clinically weak elderly individuals. PM&R 2018, 8, S13. [Google Scholar] [CrossRef]
- Seidler, R.D.; Bernard, J.A.; Burutolu, T.B.; Fling, B.W.; Gordon, M.T.; Gwin, J.T.; Kwak, Y.; Lipps, D.B. Motor control and aging: Links to age–related brain structural, functional, and biochemical effects. Neurosci. Biobehav. Rev. 2010, 34, 721–733. [Google Scholar] [CrossRef] [PubMed]
- Laurence, B.D.; Michel, L. The fall in older adults: Physical and cognitive problems. Curr. Aging Sci. 2017, 10, 185–200. [Google Scholar] [CrossRef] [PubMed]
- Resnick, B.; Galik, E.; Boltz, M.; Vigne, E.; Holmes, S.; Fix, S.; Zhu, S. The impact of physical activity and function on falls in assisted living residents. J. Aging Phys. Act. 2019, 27, 816–822. [Google Scholar] [CrossRef]
- Thomas, E.; Battaglia, G.; Patti, A.; Brusa, J.; Leonardi, V.; Palma, A.; Bellafiore, M. Physical activity programs for balance and fall prevention in elderly: A systematic review. Medicine 2019, 98, e16218. [Google Scholar] [CrossRef]
- Cheval, B.; Sivaramakrishnan, H.; Maltagliati, S.; Fessler, L.; Forestier, C.; Sarrazin, P.; Orsholits, D.; Chalabaev, A.; Sander, D.; Ntoumanis, N.; et al. Relationships between changes in self–Reported physical activity, sedentary behaviour and health during the coronavirus (COVID–19) pandemic in France and Switzerland. J. Sports Sci. 2021, 39, 699–704. [Google Scholar] [CrossRef]
- Audiffren, J.; Bargiotas, I.; Vayatis, N.; Vidal, P.P.; Ricard, D. A non linear scoring approach for evaluating balance: Classification of elderly as fallers and non–Fallers. PLoS ONE 2016, 11, e0167456. [Google Scholar] [CrossRef]
- Watt, A.A.; Clark, C.; Williams, J.M. Differences in sit–To–Stand, standing sway and stairs between community–dwelling fallers and non–fallers: A review of the literature. Phys. Ther. Rev. 2018, 23, 273–290. [Google Scholar] [CrossRef]
- Kozinc, Ž.; Löfler, S.; Hofer, C.; Carraro, U.; Šarabon, N. Diagnostic balance tests for assessing risk of falls and distinguishing older adult fallers and non–fallers: A systematic review with meta–Analysis. Diagnostics 2020, 10, 667. [Google Scholar] [CrossRef] [PubMed]
- Quijoux, F.; Vienne–Jumeau, A.; Bertin–Hugault, F.; Zawieja, P.; Lefèvre, M.; Vidal, P.P.; Ricard, D. Center of pressure displacement characteristics differentiate fall risk in older people: A systematic review with meta–Analysis. Ageing Res. Rev. 2020, 62, 101117. [Google Scholar] [CrossRef] [PubMed]
- Berglund, J. A balancing act: Scientists seek to reduce the risk of falls in the elderly. IEEE Pulse 2017, 8, 21–24. [Google Scholar] [CrossRef]
- Leightley, D.; Yap, M.H.; Coulson, J.; Piasecki, M.; Cameron, J.; Barnouin, Y.; Tobias, J.; McPhee, J.S. Postural stability during standing balance and sit–to–stand in master athlete runners compared with nonathletic old and young adults. J. Aging Phys. Act. 2017, 25, 345–350. [Google Scholar] [CrossRef]
- Hornyak, V.; Brach, J.S.; Wert, D.M.; Hile, E.; Studenski, S.; VanSwearingen, J.M. What is the relation between fear of falling and physical activity in older adults? Arch. Phys. Med. Rehabil. 2013, 94, 2529–2534. [Google Scholar] [CrossRef] [PubMed]
- Mora, J.C.; Valencia, W.M. Exercise and older adults. Clin. Geriatr. Med. 2018, 34, 145–162. [Google Scholar] [CrossRef] [PubMed]
- WHO. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak; Contract No.: WHO/2019–nCoV/MentalHealth/2020.1; World Health Organization: Geneva, Switzerland, 2020; pp. 1–5. [Google Scholar]
- Matias, T.; Dominski, F.H.; Marks, D.F. Human needs in COVID–19 isolation. J. Health Psychol. 2020, 25, 871–882. [Google Scholar] [CrossRef]
- Jiao, Y.; Lin, Y.; Zhang, X.; Wu, Y.; Wang, J.; Liang, Z. Evaluation of the effectiveness of immersive virtual reality–based exercise system for vestibular rehabilitation. J. Clin. Otorhinolaryngol. Head Neck Surg. 2020, 34, 447–451. [Google Scholar] [CrossRef]
- Nicholson, V.; Watts, N.; Chani, Y.; Keogh, J.W.L. Motor imagery training improves balance and mobility outcomes in older adults: A systematic review. J. Physiother. 2019, 65, 200–207. [Google Scholar] [CrossRef]
- Steinicke, F.; Visell, Y.; Campos, J.; Lécuyer, A. Human Walking in Virtual Environments; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Young, W.; Ferguson, S.; Brault, S.; Craig, C. Assessing and training standing balance in older adults: A novel approach using the ‘Nintendo Wii’ Balance Board. Gait Posture 2011, 33, 303–305. [Google Scholar] [CrossRef]
- Clark, R.A.; McGough, R.; Paterson, K. Reliability of an inexpensive and portable dynamic weight bearing asymmetry assessment system incorporating dual Nintendo Wii Balance Boards. Gait Posture 2011, 34, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Marivan, K.; Boully, C.; Benveniste, S.; Reingewirtz, S.; Rigaud, A.S.; Kemoun, G.; Bloch, F. Rehabilitation of the psychomotor consequences of falling in an elderly population: A pilot study to evaluate feasibility and tolerability of virtual reality training. Technol. Health Care 2016, 24, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Sultana, M.; Bryant, D.; Orange, J.B.; Beedie, T.; Montero–Odasso, M. Effect of Wii Fit© Exercise on Balance of Older Adults with Neurocognitive Disorders: A Meta–Analysis. J. Alzheimers Dis. 2020, 75, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Viana, R.B.; de Lira, C.A.B. Exergames as coping strategies for anxiety disorders during the COVID–19 quarantine period. Games Health J. 2020, 9, 147–149. [Google Scholar] [CrossRef]
- Kilteni, K.; Andersson, B.J.; Houborg, C.; Ehrsson, H.H. Motor imagery involves predicting the sensory consequences of the imagined movement. Nat. Commun. 2018, 9, 1617. [Google Scholar] [CrossRef]
- Lebon, F.; Horn, U.; Domin, M.; Lotze, M. Motor imagery training: Kinesthetic imagery strategy and inferior parietal fMRI activation. Hum. Brain Mapp. 2018, 39, 1805–1813. [Google Scholar] [CrossRef]
- Vasilyev, A.; Liburkina, S.; Yakovlev, L.; Perepelkina, O.; Kaplan, A. Assessing motor imagery in brain–computer interface training: Psychological and neurophysiological correlates. Neuropsychologia 2017, 97, 56–65. [Google Scholar] [CrossRef]
- Saimpont, A.; Malouin, F.; Tousignant, B.; Jackson, P.L. Assessing motor imagery ability in younger and older adults by combining measures of vividness, controllability and timing of motor imagery. Brain Res. 2015, 1597, 196–209. [Google Scholar] [CrossRef]
- Ruffino, C.; Bourrelier, J.; Papaxanthis, C.; Mourey, F.; Lebon, F. The use of motor imagery training to retain the performance improvement following physical practice in the elderly. Exp. Brain Res. 2019, 237, 1375–1382. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Liao, Y.Y.; Yang, Y.; Wu, Y.R.; Wang, R.Y. Virtual reality–based Wii Fit training in improving muscle strength, sensory integration ability, and walking abilities in patients with Parkinson’s disease: A randomized control trial. Int. J. Gerontol. 2015, 9, 190–195. [Google Scholar] [CrossRef]
- Nicholson, V.P.; Keogh, J.W.; Low Choy, N.L. Can a single session of motor imagery promote motor learning of locomotion in older adults? A randomized controlled trial. Clin. Interv. Aging 2018, 13, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Hovington, C.L.; Brouwer, B. Guided motor imagery in healthy adults and stroke: Does strategy matter? Neurorehabil. Neural. Repair. 2010, 24, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Dunsky, A.; Dickstein, R.; Marcovitz, E.; Levy, S.; Deutsch, J.E. Home–based motor imagery training for gait rehabilitation of people with chronic poststroke hemiparesis. Arch. Phys. Med. Rehabil. 2008, 89, 1580–1588. [Google Scholar] [CrossRef]
- Driskell, J.E.; Copper, C.; Moran, A. Does mental practice enhance performance? J. Appl. Psychol. 1994, 79, 481–492. [Google Scholar] [CrossRef]
- Kim, Y.T.; Lee, J.S. Normal pressures and reliability of the Gaitview® system in healthy adults. Prosthet. Orthot. Int. 2012, 36, 159–164. [Google Scholar] [CrossRef][Green Version]
- Tinetti, M.E.; Richman, D.; Powell, L. Falls efficacy as a measure of fear of falling. J. Gerontol. 1990, 45, P239–P243. [Google Scholar] [CrossRef]
- Buford, T.W.; Anton, S.D.; Clark, D.J.; Higgins, T.J.; Cooke, M.B. Optimizing the benefits of exercise on physical function in older adults. PM&R 2014, 6, 528–543. [Google Scholar] [CrossRef]
- Crocker, T.; Forster, A.; Young, J.; Brown, L.; Ozer, S.; Smith, J.; Green, J.; Hardy, J.; Burns, E.; Glidewell, E.; et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst. Rev. 2013, 2013, CD004294. [Google Scholar] [CrossRef]
- Chen, T.; Chang, C.C.; Chou, L.S. Sagittal plane center of mass movement strategy and joint kinetics during sit–to–walk in elderly fallers. Clin. Biomech. 2013, 28, 807–812. [Google Scholar] [CrossRef]
- Siriphorn, A.; Chamonchant, D. Wii balance board exercise improves balance and lower limb muscle strength of overweight young adults. J. Phys. Ther. Sci. 2015, 27, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Weaver, T.B.; Ma, C.; Laing, A.C. Use of the Nintendo Wii balance board for studying standing static balance control: Technical considerations, force–plate congruency, and the effect of battery life. J. Appl. Biomech. 2017, 33, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Park, E.C.; Kim, S.G.; Lee, C.W. The effects of virtual reality game exercise on balance and gait of the elderly. J. Phys. Ther. Sci. 2015, 27, 1157–1159. [Google Scholar] [CrossRef] [PubMed]
- Lamoth, C.; Alingh, R.; Caljouw, S. Exergaming for elderly: Effects of different types of game feedback on performance of a balance task. Stud. Health Technol. Inform. 2012, 181, 103–107. [Google Scholar] [CrossRef]
- Babadi, S.Y.; Daneshmandi, H. Effects of virtual reality versus conventional balance training on balance of the elderly. Exp. Gerontol. 2021, 153, 111498. [Google Scholar] [CrossRef]
- Hamel, M.F.; Lajoie, Y. Mental imagery. Effects on static balance and attentional demands of the elderly. Aging Clin. Exp. Res. 2005, 17, 223–228. [Google Scholar] [CrossRef]
- Moshref–Razavi, S.; Sohrabi, M.; Sotoodeh, M.S. Effect of Neurofeedback Interactions and Mental Imagery on the Elderly’s Balance. Iran. J. Ageing 2017, 12, 288–299. [Google Scholar] [CrossRef]
- Oh, D.S.; Choi, J.D. Effects of motor imagery training on balance and gait in older adults: A randomized controlled pilot study. Int. J. Environ. Res. Public Health 2021, 18, 650. [Google Scholar] [CrossRef]
- Mouthon, A.; Ruffieux, J.; Mouthon, M.; Hoogewoud, H.M.; Annoni, J.M.; Taube, W.J. Age–Related differences in cortical and subcortical activities during observation and motor imagery of dynamic postural tasks: An fMRI study. Neural. Plast. 2018, 2018, 1598178. [Google Scholar] [CrossRef]
- Maciaszek, J.; Osiński, W.; Szeklicki, R.; Salomon, A.; Stemplewski, R.; Maciaszek, J. Body balance parameters established with closed and open eyes in young and elderly men. Biol. Sport 2006, 23, 185–193. [Google Scholar]
- Turano, K.; Rubin, G.S.; Herdman, S.J.; Chee, E.; Fried, L.P. Visual stabilization of posture in the elderly: Fallers vs. nonfallers. Optom. Vis. Sci. 1994, 71, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Chiacchiero, M.; Cagliostro, P.; DeGenaro, J.; Giannina, C.; Rabinovich, Y. Motor imagery improves balance in older adults. Top. Geriatr. Rehabil. 2015, 31, 159–163. [Google Scholar] [CrossRef]
- Grenier, S.; Richard–Devantoy, S.; Nadeau, A.; Payette, M.C.; Benyebdri, F.; Duhaime, M.M.B.; Gunther, B.; Beauchet, O. The association between fear of falling and motor imagery abilities in older community–Dwelling individuals. Maturitas 2018, 110, 18–20. [Google Scholar] [CrossRef] [PubMed]
- Pua, Y.H.; Ong, P.H.; Clark, R.A.; Matcher, D.B.; Lim, E.C. Falls efficacy, postural balance, and risk for falls in older adults with falls–related emergency department visits: Prospective cohort study. BMC Geriatr. 2017, 17, 291. [Google Scholar] [CrossRef] [PubMed]
| Groups (n) | Age (Years) | Height (cm) | Weight (kg) | BMI (kg/m2) | MMSE–K | VMIQ | Sex (M/F) |
|---|---|---|---|---|---|---|---|
| VRG (12) | 75.75 ± 10.15 | 157.17 ± 9.48 | 58.67 ± 12.15 | 23.82 ± 5.23 | 26.17 ± 1.53 | 1.60 ± 0.33 | 5/7 |
| MIG (10) | 83.10 ± 5.24 | 156.20 ± 10.49 | 54.70 ± 9.15 | 21.88 ± 2.73 | 25.60 ± 1.90 | 1.89 ± 0.31 | 4/6 |
| CG (12) | 80.75 ± 6.03 | 157.33 ± 10.53 | 59.75 ± 9.98 | 24.90 ± 4.30 | 25.83 ± 1.59 | 1.76 ± 0.34 | 6/6 |
| F | 2.753 | 0.039 | 0.672 | 1.366 | 0.325 | 2.207 | |
| p | 0.079 | 0.962 | 0.518 | .270 | 0.725 | 0.127 |
| Variables | Group | Pre-Test (Week 0) | Post-Test (Week 6) | Follow-Up (Week 8) | Mean Difference (95% CI) Effect Size (d) | F (p) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | Pre-Test Compared with Post-Test | Pre-Test Compared with Follow-Up | Post-Test Compared with Follow-Up | Group | Time | Group × Time | ||
| Body center movement area | VRG | 6.3 ± 3.3 | 3.26 ± 3.13 | 3.76 ± 3.54 | 3.1 (1.0 to 5.1) 0.95 | 2.6 (0.5 to 4.6) 0.75 | −0.5 (−1.0 to −0.0) −0.15 | 1.205 (0.313) | 7.822 (0.002 *) | 3.627 (0.010 *) |
| MIG | 8.0 ± 6.3 | 6.63 ± 5.05 | 7.44 ± 5.85 | 1.4 (0.0 to 2.8) 0.25 | 0.6 (−0.6 to 1.8) 0.10 | −0.8 (−1.5 to −0.1) −0.15 | ||||
| CG | 6.1 ± 4.7 | 6.87 ± 5.54 | 7.54 ± 6.51 | −0.8 (−1.6 to 0.1) −0.15 | −1.4 (−3.6 to 0.7) −0.25 | −0.7 (−2.2 to 0.9) −0.11 | ||||
| Balance sensory with eyes kept open | VRG | 85.9 ± 7.9 | 89.6 ± 5.8 † | 88.1 ± 7.3 | −3.7 (−6.5 to −0.8) 0.53 | −2.2 (−3.6 to −0.8) 0.28 | 1.5 (−0.5 to 3.5) −0.23 | 2.483 (0.100) | 2.848 (0.066) | 6.122 (0.000 *) |
| MIG | 88.1 ± 2.5 | 89.2 ± 3.8 † | 87.3 ± 3.6 | −1.1 (−2.8 to 0.6) 0.34 | 0.8 (−1.9 to 3.5) −0.26 | 1.9 (−0.4 to 4.2) −0.51 | ||||
| CG | 84.8 ± 5.6 | 82.8 ± 6.8 | 82.8 ± 6.7 | 2.0 (0.3 to 3.7) −0.32 | 2.1 (0.5 to 3.7) −0.34 | 0.1 (−0.7 to 0.9) −0.01 | ||||
| Balance sensory with eyes kept closed | VRG | 82.7 ± 8.2 | 88.2 ± 6.6 | 86.3 ± 5.7 | −5.5 (−9.6 to −1.4) 0.74 | −3.6 (−7.7 to 0.5) 0.51 | 1.9 (0.9 to 2.9) 0.31 | 1.344 (0.276) | 5.860 (0.007 *) | 3.888 (0.007 *) |
| MIG | 83.3 ± 9.0 | 84.3 ± 8.8 | 83.1 ± 8.4 | −1.0 (−2.7 to 0.7) 0.11 | 0.2 (−0.6 to 1.0) −0.02 | 1.2 (−0.6 to 3.0) −0.14 | ||||
| CG | 80.8 ± 8.9 | 80.0 ± 9.6 | 80.2 ± 9.2 | 0.8 (−0.2 to 1.9) −0.09 | 0.7 (−0.3 to 1.7) −0.07 | −0.2 (−1.1 to 0.8) 0.02 | ||||
| Falls efficacy | VRG | 29.1 ± 24.8 | 19.7 ± 19.9 | 22.3 ± 22.0 | 9.4 (5.4 to 13.5) 0.42 | 6.2 (3.7 to 8.7) 0.26 | −3.3 (−5.1 to −1.4) −0.15 | 0.431 (0.653) | 15.724 (0.000 *) | 7.509 (0.000 *) |
| MIG | 31.2 ± 24.3 | 25.1 ± 22.4 | 27.2 ± 23.6 | 6.1 (3.9 to 8.3) 0.26 | 4.0 (2.0 to 6.0) 0.17 | −2.1 (−4.4 to 0.2) −0.09 | ||||
| CG | 31.2 ± 22.5 | 33.0 ± 20.2 | 32.7 ± 20.6 | −1.8 (−4.2 to 0.5) −0.09 | −1.5 (−3.3 to 0.3) −0.07 | 0.3 (−0.9 to 1.6) 0.02 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-H.; Cho, S.-H. Benefits of Virtual Reality Program and Motor Imagery Training on Balance and Fall Efficacy in Isolated Older Adults: A Randomized Controlled Trial. Medicina 2022, 58, 1545. https://doi.org/10.3390/medicina58111545
Kim S-H, Cho S-H. Benefits of Virtual Reality Program and Motor Imagery Training on Balance and Fall Efficacy in Isolated Older Adults: A Randomized Controlled Trial. Medicina. 2022; 58(11):1545. https://doi.org/10.3390/medicina58111545
Chicago/Turabian StyleKim, So-Hyun, and Sung-Hyoun Cho. 2022. "Benefits of Virtual Reality Program and Motor Imagery Training on Balance and Fall Efficacy in Isolated Older Adults: A Randomized Controlled Trial" Medicina 58, no. 11: 1545. https://doi.org/10.3390/medicina58111545
APA StyleKim, S.-H., & Cho, S.-H. (2022). Benefits of Virtual Reality Program and Motor Imagery Training on Balance and Fall Efficacy in Isolated Older Adults: A Randomized Controlled Trial. Medicina, 58(11), 1545. https://doi.org/10.3390/medicina58111545







