Acute Eosinophilic Pneumonia after Combined Use of Conventional and Heat-Not-Burn Cigarettes: A Case Report
Abstract
1. Introduction
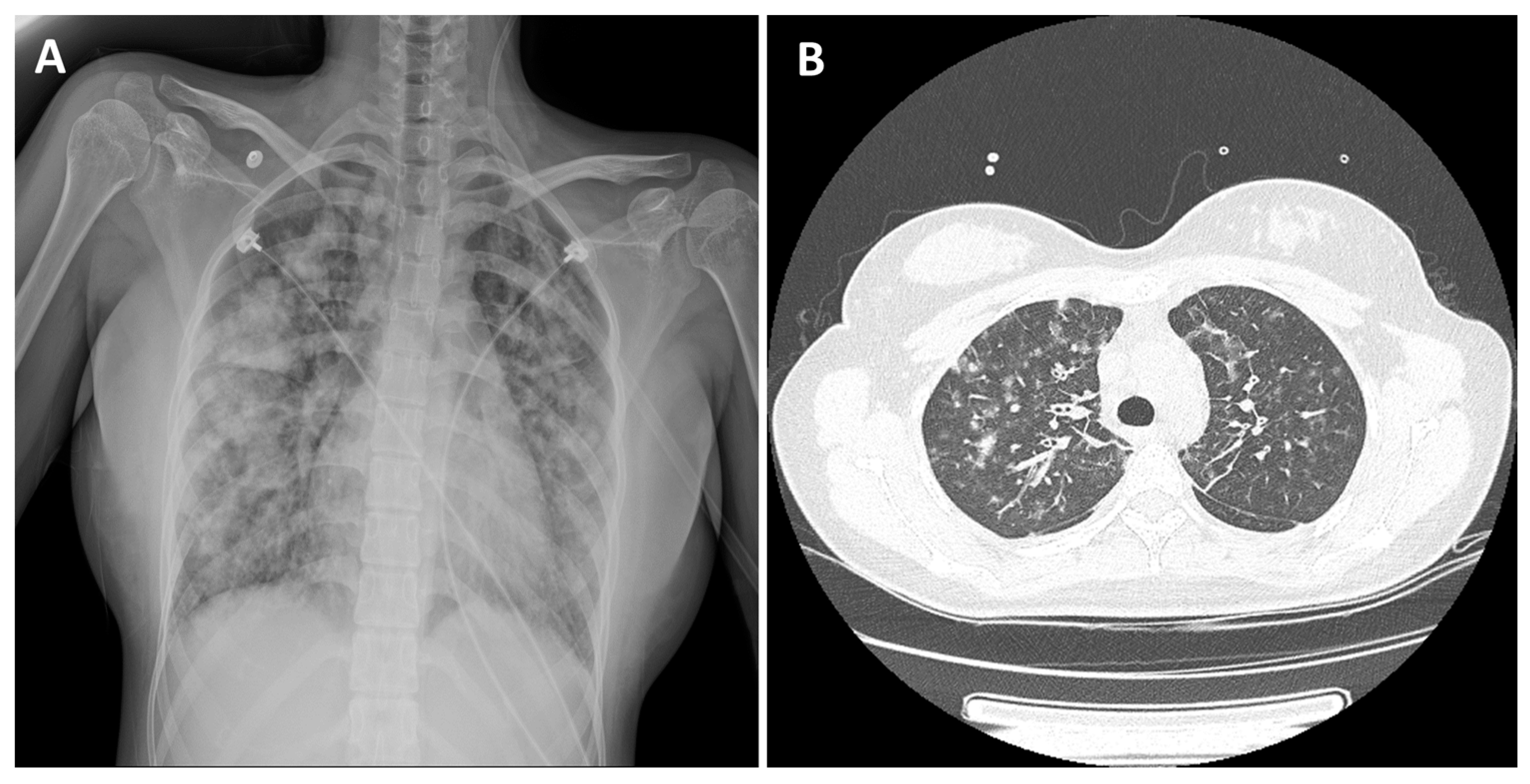
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giacomi, F.D.; Vassallo, R.; Yi, E.S.; Ryu, J.H. Acute Eosinophilic Pneumonia. Causes, Diagnosis, and Management. Am. J. Respir. Crit. Care Med. 2018, 197, 728–736. [Google Scholar] [CrossRef] [PubMed]
- Giacomi, F.D.; Decker, P.A.; Vassallo, R.; Ryu, J.H. Acute Eosinophilic Pneumonia: Correlation of Clinical Characteristics with Underlying Cause. Chest 2017, 152, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.K.; Min, K.H.; Yim, N.Y.; Lee, J.E.; Chung, M.P.; Jeon, K. Clinical characteristics and corticosteroid treatment of acute eosinophilic pneumonia. Eur. Respir. J. 2013, 41, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Pokhrel, P.; Herzog, T.A.; Kawamoto, C.T.; Fagan, P. Heat-not-burn Tobacco Products and the Increased Risk for Poly-tobacco Use. Am. J. Health Behav. 2021, 45, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.M. The Impact of Heated Tobacco Products on Smoking Cessation, Tobacco Use, and Tobacco Sales in South Korea. Korean J. Fam. Med. 2020, 41, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Auer, R.; Concha-Lozano, N.; Jacot-Sadowski, I.; Cornuz, J.; Berthet, A. Heat-Not-Burn Tobacco Cigarettes: Smoke by Any Other Name. JAMA Intern. Med. 2017, 177, 1050–1052. [Google Scholar] [CrossRef] [PubMed]
- Basaran, R.; Güven, N.M.; Eke, B.C. An Overview of iQOS® as a New Heat-Not-Burn Tobacco Product and Its Potential Effects on Human Health and the Environment. Turk. J. Pharm. Sci. 2019, 16, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Shorr, A.F.; Scoville, S.L.; Cersovsky, S.B.; Shanks, G.D.; Ockenhouse, C.F.; Smoak, B.L.; Carr, W.W.; Petruccelli, B.P. Acute eosinophilic pneumonia among US Military personnel deployed in or near Iraq. JAMA 2004, 292, 2997–3005. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Sun, W.; Meng, W.; Xiao, Y.; Feng, G.; Shi, B. Cigarette smoking-induced acute eosinophilic pneumonia: A case report. Medicine 2019, 98, e14704. [Google Scholar] [CrossRef] [PubMed]
- Tajiri, T.; Wada, C.; Ohkubo, H.; Takeda, N.; Fukumitsu, K.; Fukuda, S.; Kanemitsu, Y.; Uemura, T.; Takemura, M.; Maeno, K.; et al. Acute Eosinophilic Pneumonia Induced by Switching from Conventional Cigarette Smoking to Heated Tobacco Product Smoking. Intern. Med. 2020, 59, 2911–2914. [Google Scholar] [CrossRef] [PubMed]
- Peri, Y.; Shifman, O.T.; Hershko, A.Y. Eosinophilic pneumonia following occupational smoke exposure. Eur. J. Case Rep. Intern. Med. 2016, 3, 000494. [Google Scholar] [CrossRef] [PubMed]
- Chabot, C.; Gouat, F. Rare finding of acute eosinophilic pneumonia associated with heavy cannabis use: A case-report. Radiol. Case Rep. 2022, 17, 3040–3042. [Google Scholar] [CrossRef] [PubMed]
- LaMorte, D.; Desmond, D.; Ellis, J.; Lipkowitz, S. Acute eosinophilic pneumonia: A fatal reaction to ado-trastuzumab. BMJ Case Rep. 2021, 14, e243881. [Google Scholar] [CrossRef] [PubMed]
- Daimon, T.; Johkoh, T.; Sumikawa, H.; Honda, O.; Fujimoto, K.; Koga, T.; Arakawa, H.; Yanagawa, M.; Inoue, A.; Mihara, N.; et al. Acute eosinophilic pneumonia: Thin-section CT findings in 29 patients. Eur. J. Radiol. 2008, 65, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Suda, T. Eosinophilic pneumonia: A review of the previous literature, causes, diagnosis, and management. Allergol. Int. 2019, 68, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Grana, R.; Benowitz, N.; Glantz, S.A. E-cigarettes: A scientific review. Circulation 2014, 129, 1972–1986. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, B.H.; Lee, D.H.; Roh, M.S.; Um, S.-J.; Kim, I. Acute Eosinophilic Pneumonia after Combined Use of Conventional and Heat-Not-Burn Cigarettes: A Case Report. Medicina 2022, 58, 1527. https://doi.org/10.3390/medicina58111527
Kang BH, Lee DH, Roh MS, Um S-J, Kim I. Acute Eosinophilic Pneumonia after Combined Use of Conventional and Heat-Not-Burn Cigarettes: A Case Report. Medicina. 2022; 58(11):1527. https://doi.org/10.3390/medicina58111527
Chicago/Turabian StyleKang, Bo Hyoung, Dong Hyun Lee, Mee Sook Roh, Soo-Jung Um, and Insu Kim. 2022. "Acute Eosinophilic Pneumonia after Combined Use of Conventional and Heat-Not-Burn Cigarettes: A Case Report" Medicina 58, no. 11: 1527. https://doi.org/10.3390/medicina58111527
APA StyleKang, B. H., Lee, D. H., Roh, M. S., Um, S.-J., & Kim, I. (2022). Acute Eosinophilic Pneumonia after Combined Use of Conventional and Heat-Not-Burn Cigarettes: A Case Report. Medicina, 58(11), 1527. https://doi.org/10.3390/medicina58111527





